Abstract
Background
Somalia has long been in a state of humanitarian crisis; trauma-related mental health needs are extremely high. Access to state-of-the-art mental health care is limited. Islamic Trauma Healing (ITH) is a manualized mosque-based, lay-led group intervention aimed at healing the individual and communal mental wounds of war and refugee trauma. The 6-session intervention combines Islamic principles with empirically-supported exposure and cognitive restructuring principles for posttraumatic stress disorder (PTSD). ITH reduces training time, uses a train the trainers (TTT) model, and relies on local partnerships embedded within the strong communal mosque infrastructure.
Methods
We will conduct a hybrid effectiveness-implementation randomized control trial (RCT) in the Somaliland, with implementation in the cities of Hargeisa, Borama, and Burao. In this study, a lay-led, mosque-based intervention, Islamic Trauma Healing (ITH), to promote mental health and reconciliation will be examined in 200 participants, randomizing mosques to either immediate ITH or a delayed (waitlist; WL) ITH conditions. Participants will be assessed by assessors masked to condition at pre, 3 weeks, 6 weeks, and 3-month follow-up. Primary outcome will be assessor-rated posttraumatic stress symptoms (PTSD), with secondary outcomes of depression, somatic symptoms, and well-being. A TTT model will be tested, examining the implementation outcomes. Additional measures include potential mechanisms of change and cost effectiveness.
Conclusion
This trial has the potential to provide effectiveness and implementation data for an empirically-based principle trauma healing program for the larger Islamic community who may not seek mental health care or does not have access to such care.
Clinical trial registration number
ClinicalTrials.gov NCT05890482.
World health organization trial registration data set information
See Supplemental Appendix 1.
Keywords: Trauma, Posttraumatic stress disorder, Lay leaders, Islam, Cognitive behavioral therapy, Psychotherapy
Highlights
-
•
Islam-focused, lay-led program addresses mental health impact of trauma.
-
•
Uses a train the trainers model and relies on local partnerships with mosques.
-
•
Effectiveness-implementation randomized controlled trial of ITH versus delayed ITH.
-
•
Trauma-related mental health, implementation, and cost effectiveness examined.
-
•
Provides scalability data for mental health response in humanitarian crisis settings.
1. Background
According the United Nations High Commissioner for Refugees [1], 89.3 million people worldwide are forcibly displaced due to various forms of trauma exposure including war, conflicts, fear of persecution, and human rights violations. Despite decades of advancement, evidence-based mental health and psychosocial support interventions (MHPSS) have failed to permeate many low- and middle-income countries (LMICs [2]). In Somalia, there is limited community mental health care and there have been no documented in-country mental health trials of any evidence-based MHPSS interventions [1,3]. Muslims in, and displaced peoples from, war-torn regions like Somalia experience a high trauma burden and are at a substantially increased risk for posttraumatic stress disorder (PTSD; [4,5]). Thus, the international community faces a dilemma in addressing the mental health needs of those from humanitarian crisis effected LMICs and resultant refugee populations.
A radical shift in mental health care delivery is needed [6]. In many countries, expert human resources are virtually non-existent [7], stigma about mental illness persists, and many Muslims rely on private prayer and would not consider Western-based interventions [8]. Islamic Trauma Healing (ITH) is unique in incorporating faith practices and evidence-based approaches to trauma intervention [9]. See Fig. 1. This low-cost, easily scalable, faith-based intervention is consistent with the WHO's mental health action plan to develop novel approaches to address unmet clinical needs [10].
Fig. 1.
Overview of Islamic Trauma Healing Program
Visual abstract was designed by Ifrah Shiekh and previously published in Bentley, J. A., Feeny, N. C., Dolezal, M. L., Klein, A., Marks, L. H., Graham, B., & Zoellner, L. A [9]. Islamic trauma healing: integrating faith and empirically supported principles in a community-based program. Cognitive and Behavioral Practice, 28, 167–192.
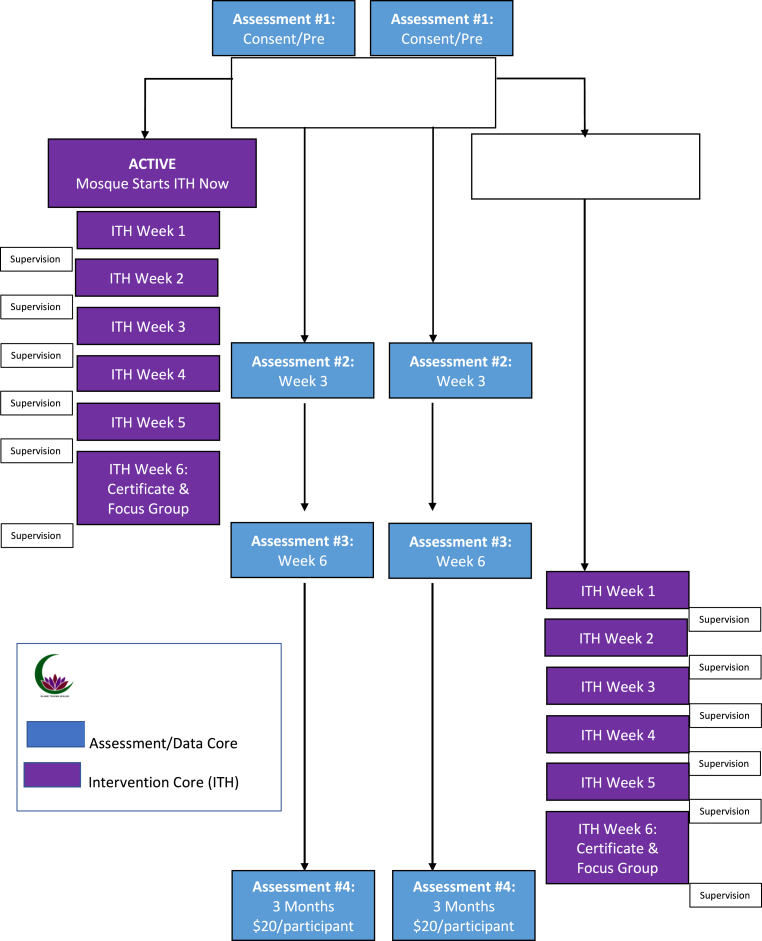
We will conduct a hybrid effectiveness-implementation randomized controlled trial (RCT) in Somaliland, with implementation sites in the cities of Hargeisa, Borama, and Burao across nine mosques. In this study, a lay-led, mosque-based intervention, ITH, to promote mental health and reconciliation will be examined in 200 participants, randomizing mosques to either immediate ITH or a delayed (waitlist; WL) conditions. Participants will be assessed by interviewers masked to condition at pre, 3 weeks, 6 weeks, and 3-month follow-up. A train-the-trainer (TTT) model will be tested, examining the implementation and outcomes for leaders trained by lay leaders. See Fig. 2. Primary outcome will be masked interviewer-rated posttraumatic stress disorder (PTSD), with secondary outcomes of depression, somatic symptoms, and well-being. Additional measures include potential mechanisms of change, implementation, and cost effectiveness outcomes.
Fig. 2.
Trial design diagram.
2. Methods
2.1. Research design
This is a single-masked (i.e., assessor-masked), prospective, cluster randomized hybrid type 1 effectiveness-implementation controlled trial designed to assess the mental health and implementation outcomes in trauma-exposed individuals with re-experiencing and or avoidance symptoms of PTSD. Randomization to active or delayed ITH will occur based on mosque. Assessments occur at baseline, mid-intervention, post-intervention, and at three-month follow-up. See Fig. 1.
2.2. Participants
We will enroll 200 individuals with Criterion A trauma exposure according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition [11], and related PTSD reexperiencing or avoidance symptoms, across three cities in Somaliland: Borama, Burao, and Hargeisa.
2.2.1. Inclusion criteria
-
1.
Experienced a DSM-5 Criterion A trauma at least 12 weeks ago
-
2.
Report current re-experiencing or avoidance PTSD symptoms
-
3.
Islamic faith
-
4.
18–70 years of age
2.2.2. Exclusion criteria
-
1.
Immediate suicide risk, with intent or plan
-
2.
Cannot understand consent/visible cognitive impairment
Criteria were carefully selected to facilitate lay leader and self-referral. Two behavioral symptoms of PTSD were chosen, specifically avoidance and re-experiencing symptoms, that are common, easily recognized, directly linked to trauma exposure; and accordingly, easy for lay individuals to identify. A diagnosis of PTSD or severity cut-off was not required, allowing for a range of sub-clinical to clinical levels of symptoms. This approach is consistent with posttraumatic stress symptoms being transdiagnostic [12,13], and may reduce stigma of joining a trauma-healing group. Further, subthreshold PTSD symptoms are also common, often unremitting, and impairing and warrant intervention [14]. Individuals with current suicidal intent will be excluded and provided referrals.
2.3. Randomization
The data analyst generated the random allocation sequence based one maximally-tolerated-imbalance (MTI) randomization using the Clinical Trials Randomization Tool, with 1:1 allocation of mosques balanced between conditions and stratified across the three cities and men's/women's groups within a mosque considered a block. A cluster randomized design, as opposed to individual participant randomization, was necessary to avoid contamination between intervention arms (i.e., intervention participants coming into direct contact with controls and sharing the intervention, maintaining masking of assessors). Assignments by cluster will be concealed by the data analyst and revealed to the intervention core team after consent and baseline assessments for a particular mosque. Assessment investigators will be masked to intervention assignment; they will not be included in any study meetings that include discussion of intervention-related matters. The team will remind participants at every assessment not to disclose whether they received the ITH intervention or not.
2.4. Procedures
The study procedures were reviewed and approved by the University of Washington Institutional Review Board (IRB). Letters of study approval from the Somaliland Ministry of Endowment and Islamic Affairs, Somaliland Ministry of Health Development, and the University of Burao were obtained.
2.4.1. Recruitment
Participants will be recruited from the community by word of mouth, lay leader and Imam recommendation, and through community contacts. Lay leaders and clinical supervisors will work with local contacts to create a list of referrals for those not eligible.
2.4.2. Assessments procedures and masking of intervention condition
Prior to randomization, consented participants will be interviewed by an independent assessor to determine eligibility and collect baseline measures. Eligible participants will then be randomized as part of their respective cluster to study condition. Participants will be assessed at baseline (Time 1), at 3 weeks (Time 2), at 6 weeks (Time 3), and at 3-month follow-up (Time 4). Those who discontinue the intervention will be invited to continue study assessments. Participants will receive up to $20 USD at the three-month follow up, prorated at $5 per assessment.
Eligible assessors will be computer literate, reliable, compassionate, and respected in their communities. Assessor training will include two, 4-h didactic trainings on the PTSD measure (PSS–I-5), role-play administrations, scoring mock assessments to fidelity, and routine reliability meetings focusing on the PSS-I-5 every six months where reliability data will be obtained across interviewers using audio recordings of assessments. All study personnel will receive training on the importance of confidentiality, protection of human subjects, and methods to ensure data safety. Staff will sign confidentiality statements.
2.5. Measures
Interviews and questionnaires will be completed electronically (e.g., tablet, smartphone) using Qualtrics, when possible. All measures have been translated and back translated from English to Somali. See Table 1. Participant assessments will be tracked with multiple follow-up attempts to ensure retention and complete data.
Table 1.
Timing of assessment Measures.
1 For the first 6 months after training of new lay leaders, 50 % of group sessions will be observed. For the next 6 months, 30 % will be observed.
Confidentiality of the material will be preserved, including no subject-identifying features on entered data using an identification number.
2.5.1. Main outcome measures
Consistent with transdiagnostic approach [15], psychopathology following trauma exposure is assessed as dimensional and multifaceted, examining not only PTSD, but also depression, well-being, and somatic symptoms. A somatic symptom measure was included to examine indicators of distress potentially associated with reactions to trauma more common in the population of interest relative to samples collected in Westernized contexts [16,17].
PTSD Scale – Interview for DSM-5 (PSS–I-5; [18]) [primary outcome]. This measure provides a trauma screen and rates DSM-5 symptoms for the past week, ranging from 0 to 4 with higher scoring indicating more severe posttraumatic stress. Total PTSD severity will be the main outcome, with PTSD diagnostic status also derived.
Patient Health Questionnaire-9 for Depression Symptoms (PHQ-9; [19]) [secondary outcome]. The PHQ-9 is a self-report measure of depression symptoms with each question rated from 0 to 3, for the past week.
Somatic Symptom Scale-8 [20] [secondary outcome]. This eight-item measure assesses somatic symptoms (e.g., stomach ache, headaches) in the past week.
WHO-5 Wellbeing Index (WHO-5; [21]) [secondary outcome]. This five-item measure assesses emotional well-being on a 0–5 scale over the past week, with higher scores indicating better wellbeing.
2.5.2. Mechanism and other measures
These measures are included to understand underlying mechanism driving symptom change and assessment of other potentially relevant constructs.
Posttraumatic Cognitions Inventory (PTCI; [22]). This self-report measure assesses maladaptive trauma-related beliefs about self, the world, and self-blame. Twelve items were selected based on factor analytic work and focus group feedback with Somali Muslims; rated from totally agree to totally disagree.
Daily Spiritual Experience Scale (DSES; [23]). The DSES measures daily spiritual experiences and rated from never to many times a day, with higher scores indicating more daily spiritual experiences. A 6-item short-form, with a seventh global item, of the scale adapted for Islam is utilized.
Social Connectedness Scale [24]. A 7-item version of the social connectedness scale will be used to assess connection to one's community, rating from strongly agree to strongly disagree with higher scores indicating lack of belonging.
Transgression-Related Interpersonal Motivations (TRIM-R; [25]). This measure assesses forgiveness, particularly desire for retribution, rating items from strongly disagree to strongly agree, with lower scores reflecting higher forgiveness.
Trauma Stigma and Help Seeking Scale. This 9-item developed measure assesses stigma associated with trauma and seeking help for emotional distress. Items include willingness to acknowledge to others and seek help (e.g., family, elder, religious leader, healthcare worker), ranging from strongly disagree to strongly agree.
WHO Disability Assessment Schedule 2.0 (WHODAS; [26]). The WHODAS 2.0 is a 12-item self-report assessing functioning across cognition, mobility, self-care, getting along, life activities, and participation and rated from no problems to severe or cannot do.
Local Measure of Functioning (LocF). Based on Bolton and Tang [27], functioning for oneself, family, community, and faith were generated by community members. Common items were combined and feedback solicited. Eleven items are rated from no/not at all to very much/a lot, with three specific to men or women.
2.5.3. Implementation outcomes
Implementation measures will be completed by trainers, lay leaders, or participants.
Fidelity Checklists. Following each session, fidelity checklists will assess whether critical elements were completed (yes/no), duration of time (min) to complete the element, including amount of imaginal exposure, and quality of the group discussion rated from very poor to excellent.
“Buddy System” Adherence. New lay leaders will be paired with a trainer of the same sex. This “buddy” will observe 50 % of sessions in leaders’ first 6 months of provision, and 30 % in the second 6 months, rating adherence to essential components and competence.
Implementation Outcome Measures (IOM; [28]). This 6-item, adapted measure assesses acceptability, appropriateness, and feasibility of ITH. Rated from completely disagree to completely agree, lay leaders will completed before and after the six sessions of ITH groups.
Client Services Satisfaction Questionnaire [29]. This measure is included to assess acceptability of content and delivery of ITH. The questionnaire was modified to contain 5 items, scored from poor to excellent. It will be completed by study participants after completion of the six sessions of ITH.
Focus Group Feedback. Focus groups at post will consist of qualitative interviews focusing on the experience of participating, what was liked most, where ITH needs improvement, barriers to involvement, how to reduce help-seeking stigma, and lessons learned. Focus groups for study participants will be recorded and translated.
2.5.4. Direct and indirect cost analysis measures
We will assess financial and economic total incremental and unit costs associated with trauma and the proposed intervention to improve PTSD severity and well-being. These include: (1) an estimate intervention costs; and (2) an estimate cost savings because of the improved functionality and participation in social and economic activities. For estimating intervention costs, we will use a mixed methods approach based on project expenditures and micro costing to capture all resources used to delivery of the intervention. We will capture both financial and economic costs, where the latter will estimate the value of all donated goods and services, specifically, venue and internet access, and lay leader time, as well as participant time and resources expended to receive the intervention. We will obtain financial expenses records to capture personnel, supplies, transport, equipment, overhead/indirect costs. We will capture the economic or opportunity cost of participant time and include questions on time allocation and out-of-pocket expenses, as part of the scheduled follow-up assessments.
Participant Time and Unaccounted Expenses. An accounting of participant time will be captured. Additional expenses such as transportation will also be queried.
Time and Unaccounted Leader Expenses. An accounting of lay leader time, including training, practice, group leading, and supervision will be captured. Additional expenses such as transportation to and from the mosque will also be queried.
Potential Cost Savings. We will ask questions to assess potential cost savings from medical costs averted, or increases in person or household income, capturing: household demographics; education and literacy; health seeking behavior; use and costs of health and social services related to trauma-related symptoms; and impact on childcare, household and employment activities, time and earnings.
2.5.5. Exploratory moderators
Demographic variables of sex, age, primary traumatic event, and education will be examined.
2.6. Treatment conditions
2.6.1. Islamic trauma healing (ITH)
The program was designed for groups of 5–7 members, with two lay leaders of the same gender. Sessions run once a week for 90–120 min for six weeks. The manual [30] contains an introduction to trauma healing, including a description of types of trauma exposure and common reactions, as well as Islamic principles related to trauma healing. Each session includes time for community building rituals (e.g., sharing tea or snacks), spiritual preparation using a brief supplication, prophet narratives relevant to trauma healing, and a closing supplication. In the first session, the rationale for the program, common reactions to trauma, and a breathing relaxation exercise are described. Starting in the second session, turning individually to Allah in dua about the trauma is conducted. The last session has a closing event at which certificates are given. See Table 2 and Bentley et al. [9] for a description and Zoellner et al. [31,32] for pilot studies. Participants who experienced substantial worsening of their symptoms or an acute mental health crisis (e.g., actively suicidal) would be removed from the study and provided appropriate referrals for more intensive care.
Table 2.
Synopsis of ITH intervention.
|
Islamic Trauma Healing Session Structure: Session 1: Faith During Hard Times Prophet Job (Ayyub) Session 2: Trials Build Strength Prophet Joseph (Yusuf) Session 3: Overcoming Fear Prophet Moses (Musa) Session 4: Redemption of Self and Others Prophet Jonah (Yoonus) Session 5: Faith, Courage, and Hope for the Future Prophet Abraham (Ibraheem); Session 6: Reconciliation Prophet Muhammad [صلى الله عليه وسلم]. Prophet Narratives and Group Discussion: Prophet narratives are brief synopses of a particular prophet's life, including verses from the Qur'an, who has gone through some form of difficult or traumatic life events. Cognitive restructuring-related group questions follow the narrative, mirroring the theme for the session. Prophet narrative content and questions shift from the presence and purpose of suffering to healing and reconciliation for oneself, others, and the larger community. Prophet narratives are read aloud (5–10 min) by the group leaders. Following each narrative are questions to facilitate a group discussion related to the theme. The themes form an arch, moving from suffering to healing to growth following trauma. Turning to Allah in Dua and Group Discussion: From sessions 2–6, participants are asked to spend time in individual dua (i.e., informal prayer), turning to Allah about their trauma. In the first session, group leaders provide a rationale for turning to Allah. In the second session, this rationale is repeated, including instructions about how to select a trauma memory, and an example dua provided. Turning to Allah is conducted individually for approximately 15–20 min. Content shifts from what happened, turning to Allah about feelings and thoughts experienced during the trauma, to turning to Allah about the hardest parts, to finally thanking and praising Allah for the experience of what he or she has learned through the trauma and through turning to Allah about it. Following individual dua are questions to facilitate a group discussion related to the theme. Participants are encouraged to talk in the group about their experience while turning to Allah but not to directly share their traumatic experiences with the group. Similarly, the content of the turning to Allah forms an arch from initially approaching the trauma memory to approaching the hardest parts of the memory to at the end shifting the meaning of the memory to have positive or growth elements to it. |
2.6.2. Delayed ITH waitlist control condition
Mosques randomized delayed ITH will wait six weeks and start ITH after the week 6 (post-intervention) assessment.
2.7. Intervention training and fidelity
Male and female leaders (n = 12+) will be selected based on being a community leader, a heart for healing and reconciliation, and willingness to later train additional group leaders. Lay leaders will sign consent forms for implementation and leader cost data. They will be trained via remote, two 4-h training sessions. Training will include psychoeducation, discussion leading skills, role plays, and videos. Lay leaders will lead groups based on the manual [30] and receive remote weekly clinical supervision by Zoellner, Feeny, or Bentley. These leaders will then train as trainers, training new lay leaders (n = 24+) and provide weekly supervision. Drs. Zoellner, Feeny, or Bentley will supervise the trainers’ supervision.
2.8. Data analysis
2.8.1. Main analytic plan
Data will be nested within the clusters of city, mosque, group, and within the individual. Mosques will be randomized into ITH and Waitlist groups. Further, each group represents a cluster that have within group dependence, as individual response within a group can be related. Since we will be using dependent clustered data, random effects models will be utilized. These models will help to address issues with longitudinal data, including missingness, clustering, serial correlation, and time-varying covariates [33]. Effect size estimates will be provided by scaling the unstandardized model coefficient using the pooled baseline standard deviation of the outcome measure in the observed data [34,35].
Data will be screened for accuracy, missing values, and fit between the data and the assumptions of the general linear and linear mixed-model analysis. Data transformations or model re-specifications will be performed for any violated assumptions. Missing data will be handled using full maximum likelihood estimation or multiply imputed and data recombined using Rubin's rules [36].
To test the main hypothesis that ITH will show a greater reduction in PTSD (PSS–I-5) and related psychopathology and well-being (PHQ-9, SSS-8, WHO-5) than WL at post, we will use repeated measures mixed models, accounting for the presence of clustering in the data from pre-, 3-week, to 6-week (post). Additionally, we will examine if gains from the ITH are maintained from post to 3 months follow-up, in the initial active ITH condition only. Care needs to be taken as any comparison across conditions from 6 week [post] and 3 month-follow-up is contaminated by the provision of ITH in the WL condition. As a post hoc analysis, we will also examine the role of baseline PTSD severity across observed outcomes to examine the potential impact of including sub-clinical participants in the trial.
To examine potential mechanisms of ITH and test the hypothesis that, for those with elevated levels of the mechanism, ITH will show a greater reduction of negative beliefs (PTCI), social connectedness (SCS), daily spiritual experiences (DSES), and desire for retribution (TRIM-R) than those in the waitlist condition (WL), we will conduct similar analyses to above. The baseline by intervention interaction will be used to predict post-treatment levels and change over time in the dependent variables, to estimate how groups differ in their rate of symptom reduction over the course of the intervention.
Further, as an exploratory mediation hypothesis, we will examine whether changes in negative beliefs (PTCI), connectedness (SCS), daily spiritual experiences (DSES), and retribution (TRIM-R) will mediate the relationship between treatment condition and changes in PTSD symptoms (PSS–I-5). We will predict week 3 mediators from treatment (a path) and post-treatment outcome from the mediator (b path) controlling for treatment and baseline levels. Mediation will be tested using the product of coefficients method with bootstrapped standard errors [37].
Results will only be reported on aggregate without identifiable information.
2.8.2. Implementation outcomes
Noninferiority analyses [38] will allow us to examine whether implementation outcomes were clinically noninferior (not worse) for new lay leaders trained by the trainers compared to the original trainers trained by the investigational team. Noninferiority margins [39] will be determined a priori [40], based on one standard deviation of the measure for groups led by the trainers. Accordingly, one-sided confidence intervals (CIs), α = 0.05, for lay leaders trained by the trainers will be calculated for main implementation outcomes: overall fidelity checklist adherence and total score across the six sessions of quality of group discussion, implementation outcomes measures (IOM) of acceptability (2 items), appropriateness (2 items), and feasibility (2 items), and client service satisfaction (CSS).
To test whether the main clinical outcome of PTSD severity (PSS–I-5) are not inferior for participants who are in groups led by new lay leaders compared to trainers, three-month follow-up PTSD severity will be examined. Given the lack of validation of the PSS-I-5 in the present sample and no previously calculated non-inferiority margin for the measure, a reliable change index score [41] will be calculated using the pooled standard deviation from baseline and the published test-retest reliability (r = 0.87 [18]). Accordingly, the non-inferiority range will reflect 2 × SE of the measure in this sample. Any difference greater on PTSD severity total for participants on the trainer led groups compared to the lay leader led groups at the three-month follow-up (TP4) will be considered statistically significant and not a result of measurement error.
Descriptive data will be reported on the fidelity checklists, “buddy system” adherence, examining adherence and competence, and differential intervention attendance using session attendance and intervention dropout (<4 sessions). For focus group feedback, we will utilize thematic analysis for qualitative interviews, allowing coding for a priori (e.g., importance of Islam [32]) and emergent themes.
2.8.3. Economic evaluation of ITH
We will first estimate costs using data extracted from financial expense reports and from follow up assessments. All data will be analyzed in Excel. We will estimate the opportunity cost of time as the average quantity of time for lay leader and participants multiplied by the relevant local wage rate. We will match relevant wage rates using information on: (1) gender; (2) whether the lay leader is employed or not; and (3) if employed, type of employment, to apply the relevant wage, accounting for urban and rural locations and accounting for differences in male and female wage rates. For unemployed, we will apply the daily wage rate in the informal sector. In order to assess the impact of uncertainty in specific wage rates, we will conduct sensitivity analysis to account for variations in that wage rate, accounting for gender and occupations in the formal and informal sector. The value of time and out of pocket expenses will be combined and added to financial costs to estimate the total intervention costs. We will estimate the following cost metrics for the full project period, across the three phases of the intervention roll out (Phase 1: trainers lead groups [3 mosques], Phase 2: trainers train new lay leaders to lead groups [3 new mosques]; Phase 3: trainers train new lay leaders to lead groups [3 new mosques] and continuing to provide supervision for previous leaders [3 previous Phase 2 mosques]). Metrics will include.
-
•
The total intervention costs
-
•The unit cost, defined as the total cost divided by project outputs for
-
oCost per beneficiary reached, i.e. total intervention cost divided by the number of beneficiaries (N = 200)
-
oCost per participating mosque, (i.e., N = 9)
-
oCost per lay volunteers trained (i.e., N = 36)
-
o
We will explore cost profiles for inputs and the timing of costs (i.e., one-time startup costs (materials development, training) and recurrent costs of operating the program at each mosque).
Cost-effectiveness analysis. Once impact estimates are available, we will estimate the incremental cost effectiveness ratio (ICER) defined as the net costs of the program per PTSD symptom averted. The net costs of the program are equal to the total intervention costs, minus health costs averted plus net change in earnings due to participation in the project. If it is not possible to estimate health costs averted or net changes in earnings due to the project, the net cost will be equal to the intervention cost. ICER is a ratio, where the numerator is net economic costs, and the denominator is net benefits. Benefits will be measured using net changes in one or more of the outcome measures for PTSD, depression, somatic symptoms, well-being, functioning, and local measure of functioning.
2.8.4. Sample size determination
Calculations are based on the primary aim of comparing the primary outcome measure of PTSD severity between ITH and WL at post-intervention and on Somaliland pilot data [32]. Power was determined using an estimated sample size of N = 192, including city (3, n = 64 per city), mosque (9, n = 21 per mosque), intervention (2, n = 96 per ITH/delayed), and group (32, 16 groups per ITH/delayed, n = 6 per group). Assuming an ICC <0.3, cluster-level temporal autocorrelation <0.2, and individual-level temporal autocorrelation <0.4, with 16 clusters/arm and 10 % dropout, we are 80 % powered to detect a d of 0.51.
2.8.5. Data monitoring and interim analyses
There is no expectation of unanticipated problems or adverse events. The Data Safety and Monitoring Board (DSMB) will be provided information on adverse events and study outcome data as requested. The DSMB will convene annually and will produce recommendations related to the continuation or possible modification to the trial. Data generated by the trial will be made available to credible researchers upon request. The trial will be registered at ClinicalTrials.gov, where additional documents related to the protocol can be found (e.g., informed consent forms). No interim analyses will be conducted.
3. Conclusions
If effective, the ITH program could impact thousands of people in the next five years in Somalia, Muslim refugee camps, and other war-torn countries. Open access to materials will broaden reach and allow for outside mental health providers, Islamic leaders, and NGOs to easily adapt this program; ultimately expanding its reach.
Using a TTT model provides an exponential growth-like model of uptake. One remote expert can supervise multiple trainers. One trainer can train and supervise multiple new leaders.
Moreover, project results and their dissemination could impact humanitarian mental health policies. Our main outcome paper and policy brief will be distributed widely, and we aim to collaboratively present the results internationally. A cost effective, faith based, scalable mental health program with little need for expert involvement could be adapted broadly. Critically, this work builds on existing community mosque infrastructure and integrates faith with healing, further supporting the use of lay leaders [42]. The use of remote WhatsApp supervision allows team members to stay connected without travel, regardless of the situation on the ground and avoids technology costs and concerns.
Taken together, a lay-lead, manual-based intervention for war and refugee-related trauma has the potential to be easily taken, adapted, and implemented in a wide variety of contexts, not only in mosques but in community centers, health care/primary care centers, and by mental health professionals themselves.
Funding
This work is supported by Elrha through the Research for Health in Humanitarian Crises (R2HC) mechanism, grant #70165.
Role of the funding source
Elrha had no involvement in the study design and will have no role in data collection, analysis, interpretation, or publication of the study findings. They were not involved in the development or submission of this manuscript.
Authorship eligibility guidelines
Author eligibility guidelines included being substantively involved in the conceptualization, implementation, and/or analysis/interpretation of this project. No professional writers or artificial intelligence will be used.
CRediT Authorship:
Lori A. Zoellner: conceptualization, methodology, formal analysis, investigation, data curation, writing original, writing review, supervision, project administration, funding acquisition; Norah C. Feeny: conceptualization, methodology, formal analysis, investigation, data curation, writing original, writing review, supervision, project administration, funding acquisition; Dega A. Angula: conceptualization, methodology, investigation, data curation, writing original, writing review, supervision, project administration, funding acquisition; Mohamed H. Aideed: conceptualization, methodology, writing original, writing review, supervision, project administration, funding acquisition; Essa N. Liban: conceptualization, methodology, writing original, writing review, supervision, project administration, funding acquisition; Muumin H. Egeh: conceptualization, methodology, investigation, data curation, writing original, writing review, supervision, project administration, funding acquisition; Abdisalan I. Awke: methodology, investigation, data curation, writing review, supervision, project administration; Ahmed S. Ismail: methodology, formal analysis, investigation, data curation, writing review, supervision, project administration; Mohamed A. Kunle: methodology, formal analysis, investigation, data curation, writing review, supervision, project administration; Eesha Ali: investigation, data curation, writing review; Carol E. Levin: conceptualization, methodology, formal analysis, writing original, writing review, project administration, funding acquisition; Christopher J. Burant: conceptualization, methodology, formal analysis, writing original, writing review, project administration, funding acquisition; Jacob A. Bentley: conceptualization, methodology, formal analysis, investigation, data curation, writing original, writing review, supervision, project administration, funding acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This work is only possible through an ongoing partnership among the Somaliland Youth Development and Voluntary Organization (SOYDAVO), the University of Burao, Case Western Reserve University, and the University of Washington. We would like to thank the Somaliland Ministry of Endowment and Islamic Affairs and Ministry of Health Development who provided approval to complete this work in Somaliland. We would also like to thank the following mosques who are providing support and space for this work: in Borama: Mosque Abubakar Siddiq, Mosque Imam Shafici, Al Raxma; Hargeisa: Ma'alin Haruon, AliAbi Talib, Al Bukhari; and Burao: Taqwa, Dacwa, Al Nafic.
This work is also not possible without the leadership of the intervention trainers: in Hargeisa, Somaliland: Mohamed Ahmed Abdi, Zeinab Aden Abdilahi, Ayan Abdilahi Ali, and Khadar Hindi Botan; in Borama, Somaliland: Kawsar Saad Ahmed, Sh. Aden Mohamed Ali, Salma Hassan Ibrahim, and Abdirahman Muse Tubeec; and in Burao, Somaliland: Hodan Ali, Mohamed Yonis Ibrahim, Hafsa Jama, and Mohamed Ahmed Yusuf.
Lay leaders for trauma healing groups include the following in Hargeisa: Cisman Cabdi Cabdillahi, Cabdulqadir Ciise Cali, Axmed Cabdi Dubad, Zeynab Hassan Ibrahim, Asiya Maxamed Maxamud, Nimco Xuseen Muxumad, Anda Cumer Siciid, Xuseen Cabdillahi Warsame; Borama: Hanna Jamac Cabdilahi, Cabdillahi Cabdi Cali, Yusuf Cabdi Cali, Cabdirashi Axmed Caynan, Douale Ahmed Douale, Kaltuum Jamac Qalinle, Hodan Qasim Siciid, Ayaan Maxamad Tallan; and Burao: Abdiqani Farax Abokor, Nacima Cali Axmed, Axmed Jamac X. Diriye, Xamda Farax Ibrahim, Muna Maxamad Ismacil, Muna Abdillahi Ismail, Xasan Maxamed Qasaal, Maxamad Ibrahim Shukri.
This work is also not possible without key assessors monitoring outcomes in: Hargeisa: Khalid Abdi Ibrahim, Aziza Ahmed Mohmed, Liban Nagib Mohamed, Muhiyadin Awil Mohamoud, Abdillahi Hassan Osman, Mumtaz Mohamed Saed, Hoodo Abdirahman Yusuf; Borama: Hafsa Ali Abdillahi, Awaleh Jama Abdillahi, Faadumo Maxamed Ducale, Mustafe Diriye Idiris, Xafsa Abdulqadir Geedi, and Mohamed Dahir Jama; and Burao: Abdurahman Mostafe Ahmed, Halimo Ahmed Hassan, Ayan Farah Abdillahi, Khaliif Hassan Mohamed, Mohamed Ahmed Hassan, and Rahma Ibrahim Ahmed.
Finally, we would also like to Debra Kaysen, PhD, Michele Bedard-Gilligan, PhD, Shannon Dorsey, PhD, and Hamza Zafer, PhD, who served as Co-Investigators on the initial University of Washington Population Health Initiative Grant that provided pilot data to conduct this larger study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.conctc.2023.101237.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.United Nations High Commissioner for Refugees Global trends. UNHCR. 2022. https://www.unhcr.org/globaltrends Retrieved February 21, 2023.
- 2.Cole T.B., Flanagin A. Recovery after violence and human rights abuses. JAMA. 2013;310(5):486–487. doi: 10.1001/jama.2013.218058. [DOI] [PubMed] [Google Scholar]
- 3.Cavallera V., Reggi M., Abdi S., Jinnah Z., Kivelenge J., Warsame A.M.…Ventevogel P. United Nations High Commissioner for Refugees; Geneva: 2016. Culture, Context and Mental Health of Somali Refugees: A Primer for Staff Working in Mental Health and Psychosocial Support Programmes.https://www.unhcr.org/5bbb73b14.pdf [Google Scholar]
- 4.Johnson K., Scott J., Rughita B., Kisielewski M., Asher J., Ong R., Lawry L. Association of sexual violence and human rights violations with physical and mental health in territories of the Eastern Democratic Republic of the Congo. JAMA. 2010;304(5):553–562. doi: 10.1001/jama.2010.1086. [DOI] [PubMed] [Google Scholar]
- 5.Karam E.G., Friedman M.J., Hill E.D., Kessler R.C., McLaughlin K.A., Petukhova M.…Koenen K.C. Cumulative traumas and risk thresholds: 12‐month PTSD in the World Mental Health (WMH) surveys. Depress. Anxiety. 2014;31(2):130–142. doi: 10.1002/da.22169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Becker A.E., Kleinman A. Mental health and the global agenda. N. Engl. J. Med. 2013;369(1):66–73. doi: 10.1056/NEJMra1110827. [DOI] [PubMed] [Google Scholar]
- 7.Who . 2010. A Situation Analysis of Mental Health in Somalia.https://www.mhinnovation.net/sites/default/files/downloads/innovation/reports/A-SA-of-MH-in-Somalia.pdf October). Retrieved February 21, 2023. [Google Scholar]
- 8.Ai A.L., Tice T.N., Huang B., Ishisaka A. Wartime faith-based reactions among traumatized Kosovar and Bosnian refugees in the United States. Ment. Health Relig. Cult. 2005;8(4):291–308. https://doi:10.1080/13674670412331304357 [Google Scholar]
- 9.Bentley J.A., Feeny N.C., Dolezal M.L., Klein A., Marks L.H., Graham B., Zoellner L.A. Islamic trauma healing: integrating faith and empirically supported principles in a community-based program. Cognit. Behav. Pract. 2021;28(2):167–192. doi: 10.1016/j.cbpra.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pincus H.A., England M.J. Improving the quality of psychosocial interventions for mental and substance use disorders: a report from the IOM. JAMA. 2015;314(12):1227–1228. doi: 10.1001/jama.2015.9212. [DOI] [PubMed] [Google Scholar]
- 11.American Psychiatric Association, DSM-5 Task Force . fifth ed. American Psychiatric Publishing, Inc.; 2013. Diagnostic and Statistical Manual of Mental Disorders: DSM-5™. [DOI] [Google Scholar]
- 12.Broman-Fulks J.J., Ruggiero K.J., Green B.A., Kilpatrick D.G., Danielson C.K., Resnick H.S., Saunders B.E. Taxometric investigation of PTSD: data from two nationally representative samples. Behav. Ther. 2006;37(4):364–380. doi: 10.1016/j.beth.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Kozak M.J., Cuthbert B.N. The NIMH research domain criteria initiative: background, issues, and pragmatics. Psychophysiology. 2016;53(3):286–297. doi: 10.1111/psyp.12518. [DOI] [PubMed] [Google Scholar]
- 14.Bergman H.E., Przeworski A., Feeny N.C. Rates of subthreshold PTSD among US military veterans and service members: a literature review. Mil. Psychol. 2017;29(2):117–127. doi: 10.1037/mil0000154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cuthbert B.N. The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatr. 2014;13(1):28–35. doi: 10.1002/wps.20087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bentley J.A., Thoburn J.W., Stewart D.G., Boynton L.D. The indirect effect of somatic complaints on report of posttraumatic psychological symptomatology among Somali refugees. J. Trauma Stress. 2011;24(4):479–482. doi: 10.1002/jts.20651. [DOI] [PubMed] [Google Scholar]
- 17.Im H., Ferguson A., Hunter M. Cultural translation of refugee trauma: cultural idioms of distress among Somali refugees in displacement. Transcult. Psychiatr. 2017;54(5–6):626–652. doi: 10.1177/1363461517744989. 2017. [DOI] [PubMed] [Google Scholar]
- 18.Foa E.B., McLean C.P., Zang Y., Zhong J., Rauch S., Porter K., Kauffman B.Y. Psychometric properties of the posttraumatic stress disorder symptom scale interview for DSM–5 (PSSI–5) Psychol. Assess. 2016;28(10):1159. doi: 10.1037/pas0000259. [DOI] [PubMed] [Google Scholar]
- 19.Kroenke K., Spitzer R.L., Williams J.B. The PHQ‐9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gierk B., Kohlmann S., Kroenke K., Spangenberg L., Zenger M., Brähler E., Löwe B. The somatic symptom scale–8 (SSS-8): a brief measure of somatic symptom burden. JAMA Intern. Med. 2014;174(3):399–407. doi: 10.1001/jamainternmed.2013.12179. [DOI] [PubMed] [Google Scholar]
- 21.Bech P., Olsen L.R., Kjoller M., Rasmussen N.K. Measuring well‐being rather than the absence of distress symptoms: a comparison of the SF‐36 Mental Health subscale and the WHO‐Five well‐being scale. Int. J. Methods Psychiatr. Res. 2003;12(2):85–91. doi: 10.1002/mpr.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Foa E.B., Ehlers A., Clark D.M., Tolin D.F., Orsillo S.M. The posttraumatic cognitions inventory (PTCI): development and validation. Psychol. Assess. 1999;11(3):303. doi: 10.1037/1040-3590.11.3.303. [DOI] [Google Scholar]
- 23.Underwood L.G., Teresi J.A. The daily spiritual experience scale: development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data. Ann. Behav. Med. 2002;24(1):22–33. doi: 10.1207/S15324796ABM2401_04. [DOI] [PubMed] [Google Scholar]
- 24.Lee R.M., Robbins S.B. Measuring belongingness: the social connectedness and the social assurance scales. J. Counsel. Psychol. 1995;42(2):232. doi: 10.1037/0022-0167.42.2.232. [DOI] [Google Scholar]
- 25.McCullough M.E., Rachal K.C., Sandage S.J., Worthington E.L., Jr., Brown S.W., Hight T.L. Interpersonal forgiving in close relationships: II. Theoretical elaboration and measurement. J. Pers. Soc. Psychol. 1998;75(6):1586. doi: 10.1037/0022-3514.75.6.1586. [DOI] [PubMed] [Google Scholar]
- 26.Üstün T.B., Kostanjsek N., Chatterji S., Rehm J., editors. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule WHODAS 2.0. World Health Organization; 2010. https://apps.who.int/iris/handle/10665/43974 [Google Scholar]
- 27.Bolton P., Tang A.M. An alternative approach to cross-cultural function assessment. Soc. Psychiatr. Psychiatr. Epidemiol. 2002;37:537–554. doi: 10.1007/s00127-002-0580-5. [DOI] [PubMed] [Google Scholar]
- 28.Weiner B.J., Lewis C.C., Stanick C., Powell B.J., Dorsey C.N., Clary A.S.…Halko H. Psychometric assessment of three newly developed implementation outcome measures. Implement. Sci. 2017;12:1–12. doi: 10.1186/s13012-017-0635-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Larsen D.L., Attkisson C.C., Hargreaves W.A., Nguyen T.D. Assessment of client/patient satisfaction: development of a general scale. Eval. Progr. Plann. 1979;2(3):197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 30.Lang D., Zoellner L., Graham B., Marks L.H., Feeny N.C. 2016. Islahul Qulub: Islamic Trauma Healing. Published Manual. [Google Scholar]
- 31.Zoellner L., Graham B., Marks E., Feeny N., Bentley J., Franklin A., Lang D. Islamic trauma healing: initial feasibility and pilot data. Societies. 2018;8(3):47. doi: 10.3390/soc8030047. [DOI] [Google Scholar]
- 32.Zoellner L.A., Bentley J.A., Feeny N.C., Klein A.B., Dolezal M.L., Angula D.A., Egeh M.H. Reaching the unreached: bridging Islam and science to treat the mental wounds of war. Front. Psychiatr. 2021;12 doi: 10.3389/fpsyt.2021.599293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tasca G.A., Gallop R. Multilevel modeling of longitudinal data for psychotherapy researchers: I. The basics. Psychother. Res. 2009;19(4–5):429–437. doi: 10.1080/10503300802641444. [DOI] [PubMed] [Google Scholar]
- 34.Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychol. Methods. 2009;14(1):43. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feingold A. New approaches for estimation of effect sizes and their confidence intervals for treatment effects from randomized controlled trials. The Quantitative Methods for Psychology. 2019;15(2):96. doi: 10.20982/tqmp.15.2.p096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rubin D.B. vol. 79. Citeseer; Princeton, NJ, USA: 1988, August. An overview of multiple imputation; p. 84.https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=bc4b17922d8c5d5c8ff41c61c53ec2fa3de9c310 (Proceedings of the Survey Research Methods Section of the American Statistical Association). [Google Scholar]
- 37.MacKinnon D.P., Fairchild A.J. Current directions in mediation analysis. Curr. Dir. Psychol. Sci. 2009;18(1):16–20. doi: 10.1111/j.1467-8721.2009.01598.x. PMCID: PMC2821103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pocock S.J. The pros and cons of noninferiority trials. Fund. Clin. Pharmacol. 2003;17:483–490. doi: 10.1046/j.1472-8206.2003.00162.x. [DOI] [PubMed] [Google Scholar]
- 39.Wellek S. second ed. Chapman and Hall/CRC; Boca Raton, FL: 2010. Testing Statistical Hypotheses of Equivalence and Non- Inferiority. [DOI] [Google Scholar]
- 40.Kaul S., Diamond G.A. Good enough: a primer on the analysis and interpretation of noninferiority trials. Ann. Intern. Med. 2006;145:62–69. doi: 10.7326/0003-4819-145-1-200607040-00011. [DOI] [PubMed] [Google Scholar]
- 41.Jacobson N.S., Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991;59(1):12–19. doi: 10.1037/10109-042. [DOI] [PubMed] [Google Scholar]
- 42.Cohen F., Yaeger L. Task-shifting for refugee mental health and psychosocial support: a scoping review of services in humanitarian settings through the lens of RE-AIM. Implementation Research and Practice. 2021;2 doi: 10.1177/2633489521998790. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.