Sir,
Coexistence of both human immunodeficiency virus (HIV) and discoid lupus erythematosus (DLE) is rare with only few cases reported in the literature.[1,2,3,4] The exact prevalence has not been studied; however, one study from a medical center in the USA has found it to be around 0.02%.[5] HIV and DLE are both characterized by dysregulation of immune system. In HIV patients, the restoration of immunity with highly active antiretroviral therapy (HAART) may lead to the development of autoimmune disease due to increase in circulating CD4 number. This is a part of immune reconstitution syndrome.[5] We report the case of a HIV-infected individual who developed DLE during HAART and responded quickly to hydroxychloroquine.
A 61-year-old married heterosexual male, detected as HIV positive in 2019, (CD4 count 481 cells/mm,3 HIV RNA 9503 IU) on HAART regime of Tenofovir, Lamivudine and Efavirenz presented to our outpatient department with a history of red raised, asymptomatic skin lesions over the forehead, lips, ears, and upper chest for 2 months. Lesions started as small papule and gradually increased in size and number, to involve all sites, with dry scaly surface. He complained of similar lesions on the face few years back before being diagnosed with HIV which self-resolved within few months, without any treatment, after being diagnosed with HIV. He had not visited any dermatologist for the same as the lesions subsided on its own. On enquiry he revealed a history of multiple unprotected exposure 5 years back. There was no history of intravenous drug abuse or any blood transfusion. He had not presented with any other sexually transmitted infections.
His general physical examination and systemic examinations were normal. Cutaneous examination revealed multiple, erythematous to brown papules measuring 0.5 cm × 1 cm with dry surface covered with fine white adherent scales, distributed over the forehead, lips [Figure 1], chest and ear. The carpet tac sign was positive. On investigation, routine blood and urine investigations were within the normal limits. Antinuclear antibodies were positive (1:72) and ds DNA was negative. Currently, CD4 count was within normal limits (WNL) and HIV RNA was not detectable. Skin biopsy taken from the lesion was consistent with the diagnosis of DLE [Figure 2]. After complete ophthalmological examination, he was started on tablet hydroxychloroquine 200 mg twice daily. Within 4 weeks, all the lesions healed with postinflammatory hyperpigmentation [Figure 3]. He is on regular follow-up.
Figure 1.

Erythematous scaly plaques on the face
Figure 2.
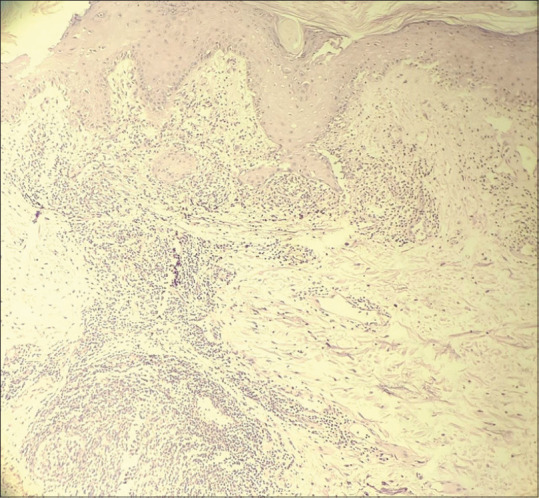
Hyperkeratosis and follicular plugging. Vacuolar degeneration of basement membrane. Dense superficial and deep lymphocytic infiltrate around adnexae and vessels. Dilated blood vessels in dermis (H and E, ×10)
Figure 3.

Healed lesions with postinflammatory hyperpigmentation
Few reasons which have been proposed for this rare co-occurrence of DLE with HIV are different demographic profile in both, with HIV commonly being seen in homosexual men and intravenous drug abusers, while DLE is commonly seen in adult women.[5] Another reason is that in HIV, may be due to depletion of CD4+ T-cells, lupus lesions tend to subside. As in our case, the lesions patient developed first subsided on being diagnosed with HIV. Later when the patient had undetectable HIV viral loads and normal CD4+ T-cell counts on HAART, he developed DLE lesions, suggesting how improved immunity played a role in the development of DLE lesions despite infection with HIV. In general, HIV-related immunosuppression improves systemic lupus erythematosus (SLE) symptoms and antiretroviral therapy may lead to an autoimmune disease flare subsequent to the increase of circulating CD4+ cell number.[3] There are many case reports of HIV patients diagnosed with SLE as part of an immune reconstitution syndrome that occurs after initiating HAART but very few with DLE.[2] SLE has been suggested to be protective against HIV because of lupus-related increased antibody production and possible anti-retroviral effect of immunosuppressive agents.[2] This particular coexistence of both the diseases is rare and peculiar. It can be considered as a new manifestation of immune reconstitution inflammatory syndrome. Further research needs to be done on the role of immunity in diagnosing and treating these patients. Patients of HIV presenting with DLE should be screened for the diagnosis of systemic autoimmune conditions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Montero A, Jorfen M, Arpini R. Chronic cutaneous lupus erythematosus and subsequent infection with HIV1. Mater Med Pol. 1992;24:21–3. [PubMed] [Google Scholar]
- 2.Calza L, Manfredi R, Colangeli V, D’Antuono A, Passarini B, Chiodo F. Systemic and discoid lupus erythematosus in HIV-infected patients treated with highly active antiretroviral therapy. Int J STD AIDS. 2003;14:356–9. doi: 10.1258/095646203321605585. [DOI] [PubMed] [Google Scholar]
- 3.Bhagwat PV, Kudligi C, Shashikumar BM, Thirunavukkarasu A, Shendre ME. Extensive discoid lupus erythematosus in a HIV patient responding to hydroxychloroquine monotherapy. Indian J Dermatol. 2012;57:326–7. doi: 10.4103/0019-5154.97687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soria A, Canestri A, Bournerias I, Le Pelletier F, Bricaire F, Caumes E. Cutaneous chronic lupus, a new cutaneous manifestation of the immune reconstitution in human immunodeficiency virus infection. Presse Med. 2009;38:1541–3. doi: 10.1016/j.lpm.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 5.Two A, So JK, Paravar T. Discoid lupus and human immunodeficiency virus: A retrospective chart review to determine the prevalence and progression of co-occurrence of these conditions at a single academic center. Indian J Dermatol. 2017;62:226. doi: 10.4103/0019-5154.201750. [DOI] [PMC free article] [PubMed] [Google Scholar]


