Abstract
Background
The Genetic Frontotemporal Initiative Staging Group has proposed clinical criteria for the diagnosis of prodromal frontotemporal dementia (FTD), termed mild cognitive and/or behavioral and/or motor impairment (MCBMI). The objective of the study was to validate the proposed research criteria for MCBMI-FTD in a cohort of genetically confirmed FTD cases against healthy controls.
Methods
A total of 398 participants were enrolled, 117 of whom were carriers of an FTD pathogenic variant with mild clinical symptoms, while 281 were non-carrier family members (healthy controls (HC)). A subgroup of patients underwent blood neurofilament light (NfL) levels and anterior cingulate atrophy assessment.
Results
The core clinical criteria correctly classified MCBMI vs HC with an AUC of 0.79 (p < 0.001), while the addition of either blood NfL or anterior cingulate atrophy significantly increased the AUC to 0.84 and 0.82, respectively (p < 0.001). The addition of both markers further increased the AUC to 0.90 (p < 0.001).
Conclusions
The proposed MCBMI criteria showed very good classification accuracy for identifying the prodromal stage of FTD.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13195-024-01383-1.
Keywords: Prodromal, MCBMI, Frontotemporal dementia, Diagnostic criteria, Diagnostic accuracy
Introduction
Frontotemporal dementia (FTD) encompasses a clinically, genetically, and pathologically heterogeneous group of neurodegenerative disorders characterized by predominant degeneration of the frontal and/or temporal lobes. The clinical criteria have been defined based on presenting clinical symptoms, i.e., the behavioral variant of FTD (bvFTD) [1], which is associated with early behavioral and executive deficits; the agrammatic variant of primary progressive aphasia (avPPA), with progressive deficits in speech, grammar, and word output; and the semantic variant of PPA (svPPA), which is a progressive disorder of semantic knowledge and naming [2]. During the course of the disease, these phenotypes may change or overlap [3] and are often associated with motor features, including extrapyramidal symptoms, as in progressive supranuclear palsy (PSP) and corticobasal syndrome (CBS), or motor neuron disease (FTD-MND) [4, 5].
The initial phases of FTD, preceding overt dementia, are characterized by a potentially extended period during which biological (preclinical) and subsequently clinical (prodromal) alterations progressively accumulate, yet these stages remain inadequately delineated [6].
Recent advances in therapeutic strategies, particularly for monogenic disease, and the need for accurate counseling and guidance make the proper definition of these stages more compelling. In particular, several approaches have now been operationalized to define the prodromal stages of FTD, and it has been reported that biological markers, such as neurofilament light (NfL) or brain magnetic resonance imaging (MRI), are already altered in these early stages [7, 8].
The Genetic Frontotemporal Initiative (GENFI) Staging Group has recently proposed clinical criteria for the diagnosis of prodromal FTD, termed “mild cognitive and/or behavioral and/or motor impairment” (MCBMI) [6] to capture the entire disease complexity at presentation. The proposed MCBMI criteria include gradual and progressive cognitive and/or behavioral and/or motor changes compared to prior functioning and reported by the patient or informant, with preservation of independence in functional abilities of daily living, occurring along with one or more of the following symptoms: (a) objective evidence of a dysexecutive syndrome, occurring in isolation or associated with other cognitive changes, such as impaired social cognition; (b) language deficits; (c) behavioral changes including apathy, disinhibition, loss of empathy, compulsive behavior, and change in appetite; and (d) signs and symptoms of parkinsonism or motor neuron disease [6]. The validity of this set of symptoms in defining MCBMI-FTD needs to be further explored.
A genetically inherited disorder, most frequently due to variants in the microtubule-associated protein tau (MAPT), progranulin (GRN), or chromosome 9 open reading frame72 (C9orf72) genes [9, 10], may represent a privileged scenario to assess the MCBMI criteria accuracy.
These observations prompted the present study, aimed at validating the proposed set of criteria for MCBMI in the GENFI cohort, considering subjects carrying pathogenic FTD variants with mild clinical symptoms compared to a healthy control group composed of non-carrier family members. Moreover, we wanted to assess whether blood NfL levels or MRI data could improve diagnostic accuracy.
Materials and methods
Participants
From the GENFI cohort study, subjects carrying a pathogenetic FTD variant and non-carrier family members were recruited from research centers across Europe and Canada (www.genfi.org.uk).
All participants underwent the GENFI standardized assessment [11]. During the first visit, demographic characteristics of all participants were collected, as well as information regarding clinical background. As previously published, the years to expected onset were calculated as the difference between age at assessment and mean age at onset within the family [11, 12]. Despite the variability in correlation strength across genetic groups, with the strongest observed for MAPT and the weakest for GRN, this approach remains one of the most dependable methods currently available for estimating age at disease onset in mutation carriers [11–13]. A subgroup of patients nearing their estimated disease onset was identified as those with an estimated years to onset of < 5 years. While recognizing that the variability in estimating disease onset may condition this time frame, within our cohort, particularly among patients who transitioned to a fully symptomatic status at follow-up, this cutoff demonstrated that the majority of those who converted (77.8%) had an estimated disease onset of < 5 years. It is noteworthy that predicting precise conversion timelines in FTD is inherently challenging, as previously highlighted [14].
For the purpose of the present study, we included a consecutive sample of participants, carriers of an FTD pathogenic variant (MAPT, GRN, or C9orf72) with mild clinical symptoms and non-carriers as healthy controls (HC). In keeping with current literature and the aim of the present study, mild clinical symptoms were defined as a global CDR® Dementia Staging Instrument plus National Alzheimer’s Coordinating Centre (NACC) behavior and language domains [15, 16] (CDR plus NACC FTLD) of 0.5 or a CDR plus NACC FTLD of 0 along with mild but significant motor symptoms. Unlike the global CDR score for which the memory domain is regarded as the primary domain and the others secondary, all eight domains of the CDR plus NACC FTLD are equally weighted in calculating the global CDR plus NACC FTLD score, and if any domain has a rating of 0.5 or if the maximum domain score is 1 and all other domains are 0, the global CDR plus NACC FTLD score is equal to 0.5 [17]. We did not include patients with a full FTD phenotype, thus with a global CDR plus NACC FLTD score of ≥ 1, according to the following scoring, as previously published by Miyagawa et al.: “If the maximum domain score is 2 or 3 and all other domains are 0, the global score is 1; if the maximum domain score occurs only once, and there is another rating besides 0, the global score is one level lower than the level corresponding to maximum impairment; if the maximum domain score occurs more than once, then the global score is that maximum domain score” [17].
Local ethics committees approved the study at each site, and all participants provided written informed consent. The study was conducted according to the Declaration of Helsinki.
Assessment of MCBMI
MCBMI was assessed by the following: (a) trial making test [18], semantic (animals) and phonemic fluencies (letters FAS) [19] scores to assess executive functions; (b) the mini-social cognition and emotional assessment (mini-SEA), which is composed from a reduced and modified version of the Faux-Pas test, and a facial emotions recognition test [20] scores to assess social cognition; (c) Boston Naming [21] and modified Camel and Cactus test (mCCT) [22] scores to test language; (d) presence of apathy, disinhibition, loss of empathy, compulsive behavior, and change in appetite, as reported by caregiver (which were rated on a 5-point scale: 0 = absent, 0.5 = questionable/very mild, 1 = mild, 2 = moderate, and 3 = severe) to assess behavioral disturbances; and (e) presence of signs of parkinsonism or motor neuron disease as referred by caregiver, including dysarthria, dysphagia, tremor, slowness, weakness, gait disorder, falls, and functional difficulties using hands (which were rated on a 5-point scale: 0 = absent, 0.5 = questionable/very mild, 1 = mild, 2 = moderate, and 3 = severe) to assess extrapyramidal and motor neuron signs and symptoms. For further details and practical examples for each symptom and level of severity, we refer readers to Table S1 of Samra et al. [23].
Neurofilament light quantification
In a subset of participants (n = 173), plasma was collected by venipuncture and centrifuged (2000g, 10 min, at room temperature). The serum was frozen at − 80 °C within 3 h after collection, shipped, and analyzed without any previous thaw–freeze cycle. We measured NfL levels in duplicates by single molecule array (Simoa) technique on the Simoa HD-X Analyzer (Quanterix, Lexington, MA, USA), using the NF-light Advantage kit for NfL [24] according to the manufacturer’s instructions (dilution: 1/4). All measurements had a coefficient of variation (CV) below 20%. Technicians were blinded to the genotypic and clinical status of the samples.
MRI visual rating
A subset of participants (n = 297) underwent MRI at their local site. The protocol, designed to match across scanners as much as possible, included a volumetric T1-weighted scan, as previously published [11]. Visual rating of cerebral atrophy of the complete imaging dataset of all participants was performed, blind to all clinical and genetic information, by two trained raters (A.B. and E.P.). We adopted the 4-point scale evaluating both left and right anterior cingulate atrophy, evaluated on the first anterior slice where the corpus callosum becomes visible, which has been shown to be specific for FTD [25]. The selection of the anterior cingulate atrophy visual rating scale was grounded in its demonstrated efficacy and validation in discriminating FTD from Alzheimer’s disease, as well as its applicability across pathologically confirmed FTLD subtypes [26]. While data-driven approaches like voxel-based morphometry (VBM) can provide comprehensive insights into patterns of atrophy, the practical applicability of such methods in routine clinical practice can be limited due to the requirement of specialized software and expertise. Moreover, Harper et al. [25] demonstrated significant correlations between the visual rating scales and objective measurements of atrophy in the corresponding brain regions, including smaller frontal regions like the anterior cingulate, ensuring the reliability and validity of these scales in assessing regional brain atrophy. In contrast, visual rating scales, particularly those that are validated and recognized for their utility in distinguishing between neurodegenerative disorders, provide an accessible and applicable tool for clinicians, ensuring that the criteria can be readily implemented in patient assessments and diagnoses.
Images were rated in native space, in keeping with standard clinical reads. To aid rating consistency, reference images for the rating scale were provided to raters [25]. The mean values obtained by both raters were considered for analyses. Inter-rater reliability was determined using the intraclass correlation coefficient (ICC) (two-way random, absolute ICC), which was equal to 0.78, comparable to previous studies [25].
Statistical analysis
Baseline demographic and clinical variables were compared across the groups using the Mann-Whitney U test for continuous variables or Fisher’s exact test for categorical variables. Considering that neuropsychological tests have substantial variability in performance below the normal range, tests were coded as “normal” or “abnormal” based on age-, sex-, and education-adjusted z-scores, with an impairment defined as z ≤ − 1.5, obtained from the healthy control group. Binomial logistic regressions were used to evaluate the predictive models and receiver-operating characteristic (ROC) curves constructed from the logistic scores. Areas under the curves (AUCs), including 95% confidence interval (CI) values, are reported. Sensitivities and specificities were computed at Youden’s J index thresholds. Positive predictive values (PPV) and negative predictive values (NPV) were computed; PPV was defined as the number of true positives/(number of true positives + number of false positives) while NPV was defined as the number or true negatives/(number of true negatives + number of false negatives). Given the multivariable nature of the model, specific cutoff values for individual measures are not obtainable, as changes in one predictor are considered in the context of all other variables in the model.
Statistical significance was assumed at p < 0.05, and p values were two-sided. Data analyses were carried out using SPSS, version 25.0 (IBM Corp).
Data availability
All study data, including raw and analyzed data, and materials will be available upon reasonable request.
Results
Participant characteristics
A total of 398 participants were enrolled, 117 of whom were carriers of an FTD pathogenic variant (51 C9orf72, 44 GRN, 22 MAPT) in the MCBMI phase, while 281 were familial non-carriers. Demographic characteristics for both carriers and non-carriers are reported in Table 1. The groups appeared similarly distributed in sex, education, and handedness. The prodromal FTD group appeared slightly older (p = 0.016), but this difference of ~ 5 years (50 vs 45) was not considered clinically meaningful. Carriers showed significantly higher levels of plasma NfL (p < 0.001). Anterior cingulate cortex atrophy was significantly different between carriers and non-carriers (p < 0.001).
Table 1.
Demographic and clinical characteristics of the prodromal FTD group and healthy control group
| Prodromal carriers (n = 117) | Healthy non-carriers (n = 281) | p value | |
|---|---|---|---|
| Age, years | 50.1 (39.4–56.9) | 44.7 (37.8–56.6) | 0.016 |
| Sex, n female (%) | 70 (59.8) | 158 (56.2) | 0.578 |
| Education, years | 15 (12–16) | 15 (12–16) | 0.858 |
| Handedness (R:L:A) | 105:10:2 | 258:19:4 | 0.702 |
| CDR plus NACC - SOB | 0.5 (0.5–1.5) | 0.0 (0.0–0.0) | |
| Genetic status, n (%)b | 0.189 | ||
| GRN | 44 (37.6) | 99 (35.2) | |
| C9orf72 | 51 (43.6) | 116 (41.3) | |
| MAPT | 22 (18.8) | 59 (21.0) | |
| Neuropsychological tests | |||
| TMT-A | 25.0 (19.0–33.0) | 24.9 (19.0–31.0) | 0.468 |
| TMT-B | 61.0 (45.0–80.0) | 57.1 (47.0–72.8) | 0.437 |
| Semantic fluencies | 23.0 (20.0–28.0) | 24.0 (20.0–27.0) | 0.784 |
| Phonemic fluencies | 40.0 (30.0–49.8) | 41.0 (31.0–50.0) | 0.581 |
| Mini-SEA | 25.6 (24.0–27.0) | 26.0 (24.0–27.0) | 0.444 |
| Boston naming | 28.0 (26.0–29.0) | 28.0 (27.0–29.0) | 0.097 |
| Modified camel and cactus test | 30.4 (29.0–31.0) | 30.4 (29.2–31.0) | 0.953 |
| Plasma NfL, pg/mL | 9.7 (6.7–15.9) | 7.4 (5.0–10.6) | < 0.001 |
| Anterior cingulate cortexa | 0.75 (0.25–1.25) | 0.50 (0.00–0.50) | < 0.001 |
Data are median (interquartile range (IQR)) or n (%). p values were calculated by the Mann-Whitney U test, χ2 test, or Fisher’s exact test, as appropriate
R right-handed, L left-handed, A ambidextrous, CDR plus NACC – SOB CDR® Dementia Staging Instrument plus National Alzheimer’s Coordinating Centre behavior and language domains sum of boxes, NfL neurofilament light
aSee text for details
bFor healthy non-carriers, the number of participants in each genetic group represents healthy participants with a family member with that particular genetic variant
Behavioral features
Behavioral symptoms for each group are reported in Table 2. The most frequently rated symptoms in the prodromal FTD group were apathy (21.4%), followed by disinhibition (17.9%), loss of empathy (14.5%), compulsive behavior (13.7%), and change in appetite (10.3%). All behavioral features were significantly different between the groups (all p < 0.001).
Table 2.
Behavioral and motor features of the prodromal FTD group and healthy control group
| Prodromal carriers (n = 117) | Healthy non-carriers (n = 281) | p value | |
|---|---|---|---|
| Behavior | |||
| Disinhibition | 21 (17.9%) | 4 (1.4%) | < 0.001 |
| Apathy | 25 (21.4%) | 11 (3.9%) | < 0.001 |
| Loss of empathy | 17 (14.5%) | 2 (0.7%) | < 0.001 |
| Compulsive behavior | 16 (13.7%) | 3 (1.1%) | < 0.001 |
| Change in appetite | 12 (10.3%) | 4 (1.4%) | < 0.001 |
| ≥ 1 behavioral symptom | 51 (43.6%) | 19 (6.8%) | < 0.001 |
| Cognitive | |||
| Camel and Cactus | 20 (17.4%) | 20 (7.2%) | 0.005 |
| TMT A | 52 (44.8%) | 18 (6.5%) | < 0.001 |
| TMT B | 18 (15.5%) | 24 (8.6%) | 0.049 |
| Boston Naming | 77 (66.4%) | 21 (7.5%) | < 0.001 |
| Semantic fluencies | 21 (18.1%) | 15 (5.4%) | < 0.001 |
| Phonemic fluencies | 21 (18.1%) | 20 (7.2%) | < 0.001 |
| Mini-SEA | 15 (13.0%) | 16 (5.8%) | 0.022 |
| ≥ 1 cognitive impairment | 85 (72.6%) | 47 (16.8%) | < 0.001 |
| Motor | |||
| Dysarthria | 6 (5.1%) | 3 (1.1%) | 0.022 |
| Dysphagia | 7 (6.0%) | 2 (0.7%) | 0.003 |
| Tremor | 7 (6.0%) | 11 (3.9%) | 0.428 |
| Slowness | 7 (6.0%) | 3 (1.1%) | 0.009 |
| Weakness | 16 (13.7%) | 1 (0.4%) | < 0.001 |
| Gait disorder | 9 (7.7%) | 5 (1.8%) | 0.006 |
| Falls | 7 (6.0%) | 1 (0.4%) | 0.001 |
| Difficulties using hands | 9 (7.7 %) | 0 (0.0%) | < 0.001 |
| ≥ 1 motor symptom | 30 (25.6%) | 15 (5.3%) | < 0.001 |
Data are n (%). p values were calculated by the χ2 test or Fisher’s exact test
We observed that nearly half (43.6%) of prodromal FTD presented with at least one behavioral symptom while only 6.8% of the control group did (p < 0.001).
Neuropsychological assessment
The frequency of impairment at formal neuropsychological testing is reported in Table 2. We observed significantly more impaired scores in the prodromal FTD group compared to the healthy control group in nearly all neuropsychological tests. In particular, the Boston Naming Test was impaired in 66.4% of prodromal FTD patients, followed by the Trail Making Test Part A (44.8%). Semantic and phonemic fluencies were similarly altered in 18.1% of prodromal FTD patients. We observed that at least one cognitive test was impaired in up to 72.6% of prodromal FTD, compared to just 16.8% of healthy controls.
Motor features
Motor symptoms for each group are reported in Table 2. The most frequently rated symptoms in the prodromal FTD group were weakness (13.7%), followed by gait disorder (7.7%), functional difficulties using hands (7.7%), dysphagia (6.0%), tremor (6.0%), slowness (6.0%), falls (6.0%), and dysarthria (5.0%). Of all motor symptoms, only tremor was not significantly different between the groups. We observed that one quarter (25.6%) of prodromal FTD presented with at least one motor symptom while only 5.3% of the control group did (p < 0.001).
Classification accuracy of proposed criteria
We tested the diagnostic accuracy of the proposed criteria in discriminating prodromal FTD from healthy controls and subsequently adding information on plasma NfL and/or anterior cingulate cortex atrophy evaluated by visual rating scale.
Considering the whole group, as shown in Fig. 1A and Table 3, the MCBMI criteria showed an AUC of 0.79 (95% CI 0.73–0.84), with a sensitivity of 56.5% and specificity of 93.4%. Diagnostic accuracy of behavioral, cognitive, and motor symptoms core features is reported separately in Additional file 1: Table S1.
Fig. 1.
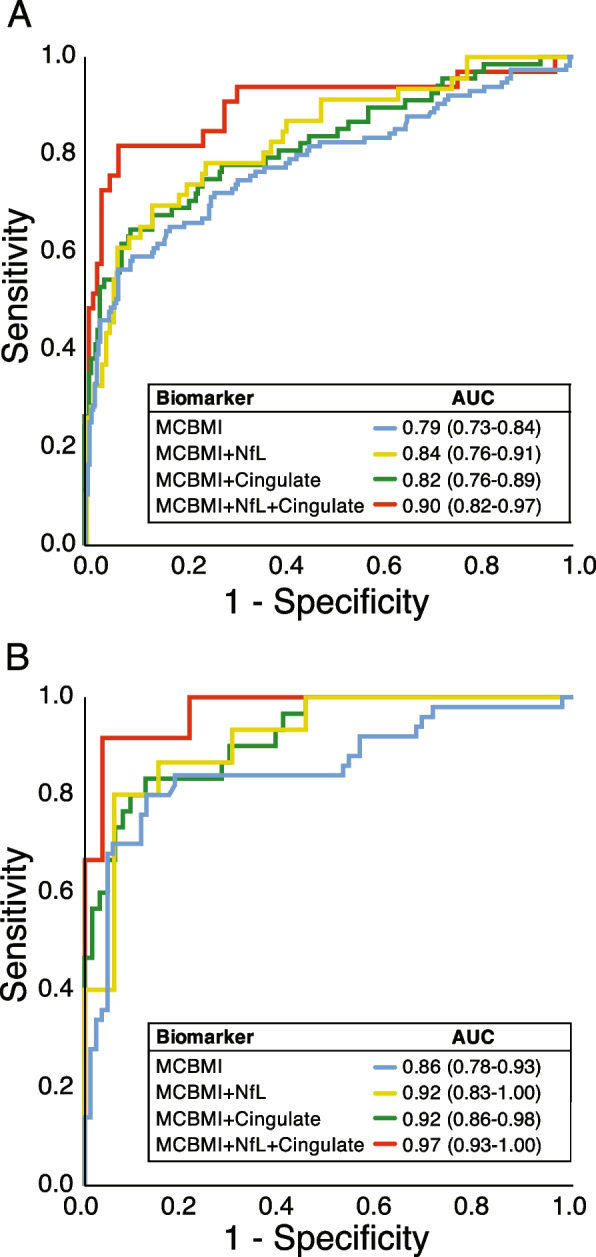
ROC curve analysis for differentiating prodromal FTD from healthy controls in A the whole group and in B participants with an estimated years to onset > − 5 years. ROC, receiver operating characteristics; AUC, area under the curve; NfL, neurofilament light; Cingulate, average left and right anterior cingulate cortex atrophy evaluated by visual rating scales
Table 3.
Diagnostic accuracy of the proposed criteria in classifying prodromal FTD from healthy controls
| AUC (95% CI) | Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|---|
| Whole group (n = 398) | |||||
| Core criteria | 0.79 (0.73–0.84) | 56.5% | 92.8% | 76.5% | 83.8% |
| Plasma NfLa | 0.68 (0.59–0.77) | 63.0% | 66.1% | 40.3% | 83.2% |
| Anterior cingulateb | 0.69 (0.62–0.77) | 55.1% | 77.6% | 42.7% | 85.1% |
| Core criteria + NfLa | 0.84 (0.76–0.91) | 69.6% | 86.4% | 65.3% | 88.5% |
| Core criteria + anterior cingulateb | 0.82 (0.76–0.89) | 64.7% | 90.6% | 67.7% | 89.4% |
| Core criteria + NfL + anterior cingulatea | 0.90 (0.82–0.97) | 81.8% | 93.0% | 77.1% | 94.7% |
| EYO < 5 years (n = 139) | |||||
| Core criteria | 0.85 (0.78–0.93) | 80.0% | 87.4% | 78.4% | 88.4% |
| Plasma NfLc | 0.65 (0.49–0.81) | 60.0% | 69.7% | 47.4% | 79.3% |
| Anterior cingulated | 0.72 (0.61–0.83) | 45.2% | 89.2% | 66.7% | 77.3% |
| Core criteria + NfLc | 0.92 (0.83–1.00) | 80.0% | 93.9% | 85.7% | 91.2% |
| Core criteria + anterior cingulated | 0.92 (0.86–0.98) | 83.3% | 87.5% | 75.8% | 91.8% |
| Core criteria + NfL + anterior cingulatec | 0.97 (0.93–1.00) | 91.7% | 96.4% | 91.7% | 96.4% |
MCBMI Mild cognitive and/or behavior and/or motor impairment, AUC Area under the curve, PPV Positive predictive value, NPV Negative predictive value, NfL Neurofilament light, EYO Estimated years to onset
an = 173
bn = 297
cn = 48
dn = 96
Taken singularly, plasma NfL and anterior cingulate cortex atrophy showed similar accuracies (AUC of 0.68 [95% CI 0.59–0.77] with a cutoff of 8.53 pg/mL and 0.69 [95% CI 0.62–0.77], respectively). The addition of plasma NfL or anterior cingulate cortex atrophy to core clinical criteria similarly increased diagnostic accuracy (AUC of 0.84 [95% CI 0.76–0.91] and 0.82 [95% CI 0.76–0.89], respectively). The inclusion of both plasma NfL and anterior cingulate cortex atrophy to core clinical criteria showed the highest diagnostic accuracy, with an AUC of 0.90 (0.82–0.97), with a sensitivity of 81.8% and a specificity of 93.0% (see Fig. 1A and Table 3).
If we considered only participants approaching estimated disease onset (with estimated years to onset < 5 years, n = 139), the proposed MCBMI criteria showed higher accuracies, as reported in Fig. 1B and Table 3. The MCBMI criteria showed an AUC of 0.85 (95% CI 0.78–0.93), with a sensitivity of 80.0% and a specificity of 87.4%. Diagnostic accuracy of behavioral, cognitive, and motor symptoms core features in this group are reported separately in Additional file 1: Table S1.
The addition of plasma NfL or anterior cingulate cortex atrophy to the MCBMI criteria similarly increased diagnostic accuracy (AUC of 0.92 [95% CI 0.83–1.00] and of 0.92 [95% CI 0.86–0.98], respectively). The inclusion of both plasma NfL and anterior cingulate cortex atrophy to the MCBMI criteria showed the highest diagnostic accuracy, with an AUC of 0.97 (0.93–1.00), with a sensitivity of 91.7% and a specificity of 96.4%.
If we considered single genes separately, we observed comparable results (see Additional file 1: Table S2). In the C9orf72 group, the MCBMI criteria added to plasma NfL and anterior cingulate cortex atrophy showed an AUC of 0.91 (0.82–0.99), with a sensitivity of 75.0% and a specificity of 95.5%. For GRN, we observed an AUC of 0.98 (0.94–1.00), with a sensitivity of 100.0% and a specificity of 85.0%, while for MAPT, we observed an AUC of 1.00 (1.00–1.00), with sensitivity and specificity of 100.0%.
Single ROC curves and cutoff values for each measure that was employed are reported in Additional file 1: Table S3.
Discussion
In this study, we tested the proposed set of diagnostic criteria for mild cognitive and/or behavioral and/or motor impairment (MCBMI), which represents the prodromal stage of FTD. These criteria have shown good diagnostic accuracy in classifying MCBMI versus a group of non-carrier family members, with better specificity and negative predictive values than sensitivity.
The decision to include cognitive, behavioral, and motor symptoms in the definition of prodromal FTD stemmed from the evidence that all these symptoms, alone or in combination, may be observed in the prodromal stages [4, 11, 27–31]. Moreover, during the course of the disease, cognitive, behavioral, and motor symptoms may change or overlap [3], making the classification of a particular clinical syndrome particularly problematic in its infancy. Indeed, when we considered these items separately, we found that both behavior abnormalities, cognitive deficits, and even motor symptoms contributed to the definition of MCBMI. It is however true that additional cognitive tests and clinical features may allow to better refine classification accuracy and sensitivity of MCBMI-FTD. In the same view, considering neuropsychiatric symptoms in the framework of MCBMI [32] may possibly further improve its operational definition and neuropathological correlations.
As already reported in other prodromal neurodegenerative dementias [33, 34], we also aimed at assessing the add-on value of potential biological or imaging diagnostic markers. To this, we considered blood NfL measurements, already shown to be increased in both sporadic and genetic FTD, particularly during the conversion from the presymptomatic to symptomatic phase, even if not specific for the disease [7, 35, 36], and anterior cingulate cortex atrophy, which is scored easily by visual rating scales at single subject level and has been shown to be specific for FTD [25, 37, 38].
Interestingly, we observed that plasma NfL and anterior cingulate scores, taken singularly, have only modest accuracy in identifying prodromal FTD; however, when added to the MCBMI clinical criteria, both markers significantly increased diagnostic accuracy, and the highest classification was achieved when both markers were incorporated.
We also assessed the diagnostic accuracy in patients who were predicted to be approaching disease onset (with an estimated symptom onset < 5 years). In this case, nearly all classification models showed higher levels of diagnostic accuracy, possibly identifying participants approaching disease conversion.
In interpreting the ROC curves and the diagnostic accuracy when adding biomarkers, it is crucial to proceed with caution due to the potential for overfitting, especially given the specificity and rarity of our sample.
We observed similar results between different genetic groups (C9orf72, GRN, MAPT), thus possibly suggesting that these criteria could be accurate also in the sporadic presentations of disease. While there are documented similarities between familial and sporadic FTD [39–41], it is pivotal to acknowledge the existing literature that points to crucial differences in the underlying biology and pathology between these forms. Notable distinctions such as dipeptide repeats (DPR) pathology [42, 43] and increased tau co-pathology in C9orf72 [44], lipofuscin presence in the retina of GRN carriers [45], and the heterogeneity of tau inclusion morphologies in MAPT versus sporadic tauopathies [46], as well as variations in biomarkers, including white matter hyperintensities in GRN FTD [47, 48] and altered CSF biomarker values in familial versus sporadic FTD [49], underscore the complexity and heterogeneity inherent in FTD. These differences necessitate a cautious approach in defining and understanding the prodromal state in both familial and sporadic FTD.
The MCBMI criteria, while conceptual, encompass a broad spectrum of symptoms and changes, including the vital consideration of gradual and progressive cognitive, behavioral, and motor changes compared to prior functioning, providing a subtle and dynamic characterization of early FTD. In contrast, the operationalization of these criteria, utilizing a CDR plus NACC FTLD score of 0.5, offers a standardized, quantifiable method for implementing the MCBMI criteria in practical settings. However, it is pivotal to note that the global CDR plus NACC FTLD, while instrumental in defining a stage of the disorder, does not inherently provide the tools to discriminate between early-stage FTD patients and healthy controls, underscoring the necessity of comprehensive, multidimensional criteria like MCBMI to accurately identify and characterize prodromal FTD.
This study brings further insights into the earliest phases of genetic FTD, joining the effort of other slightly different endeavors. Recently, the ALLFTD Consortium has operationalized the criteria for the prodromal behavioral variant of FTD (bvFTD), opting to use the term “mild behavioral and/or cognitive impairment in bvFTD (MBCI),” to acknowledge that both behavioral symptoms and cognitive impairment might be present during the disease prodrome [50], extending the previously published Rosovsky criteria to the earliest phases of the disease [1]. The bvFTD-MBCI and the MCBMI criteria address two key elements in the FTD field; the first with the attempt to capture a specific disease phenotype, while the second tries to identify the earliest phases of the global FTD spectrum. Both are reasonable and potentially useful depending on the clinical question, whether in relation to early-stage treatments, particularly for monogenic disease, that target the pathogenetic mechanisms of the disease regardless of the clinical phenotype. However, both approaches comply with a diagnostic tool rather than a screening test, reporting greater specificity than sensitivity.
We acknowledge that the present study entails several limitations. First, we did not include a control group with other neurodegenerative diseases, such as prodromal Alzheimer’s disease or non-neurodegenerative psychiatric disorders. This will be mandatory to confirm the validity of these criteria in real-world situations. Second, we did not perform a validation of the MCBMI criteria against a cohort that includes full phenotypes of FTD, as well as sporadic cases. While the criteria demonstrated validity in our specific cohort, further validation in cohorts encompassing a broader spectrum of FTD phenotypes and sporadic cases is crucial to ensure its applicability and validity in various clinical contexts. Third, while the scales used have shown good validity, it will be important in future studies to formally assess both intra- and inter-rater variabilities. Fourth, we acknowledge the limitation of not including premanifest disease carriers and not evaluating the stability of the prodromal status and phenoconversion to symptomatic syndromes which should be further assessed in future longitudinal studies.
The MCBMI criteria have demonstrated potential validity in identifying prodromal FTD within the confines of the present study, though further validation in diverse cohorts is essential to fully establish their validity and utility in clinical settings.
Supplementary Information
Additional file 1: Table S1. Diagnostic accuracy of each domain of proposed MCBMI criteria in classifying prodromal FTD from healthy controls. Table S2. Diagnostic accuracy of proposed criteria in classifying prodromal FTD from healthy controls for each genetic group. Table S3. Diagnostic accuracy of each subdomain of proposed MCBMI criteria in classifying prodromal FTD from healthy controls.
Acknowledgements
We thank the research participants and their families for their contribution to the study.
List of collaborators in the GENFI consortium:
•Annabel Nelson: Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UK
• Martina Bocchetta: Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UK
• David Cash: Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UK
• David L. Thomas: Neuroimaging Analysis Centre, Department of Brain Repair and Rehabilitation, UCL Institute of Neurology, Queen Square, London, UK
• Emily Todd: Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UK
• Hanya Benotmane: UK Dementia Research Institute at University College London, UCL Queen Square Institute of Neurology, London, UK
• Jennifer Nicholas: Department of Medical Statistics, London School of Hygiene and Tropical Medicine, London, UK
• Kiran Samra: Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UK
• Rachelle Shafei: Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UK
• Carolyn Timberlake: Department of Clinical Neurosciences, University of Cambridge, Cambridge, UK
• Thomas Cope: Department of Clinical Neuroscience, University of Cambridge, Cambridge, UK
• Timothy Rittman: Department of Clinical Neurosciences, University of Cambridge, Cambridge, UK
• Andrea Arighi: Fondazione IRCCS Ca′ Granda Ospedale Maggiore Policlinico, Neurodegenerative Diseases Unit, Milan, Italy; University of Milan, Centro Dino Ferrari, Milan, Italy
• Chiara Fenoglio: Fondazione IRCCS Ca′ Granda Ospedale Maggiore Policlinico, Neurodegenerative Diseases Unit, Milan, Italy; University of Milan, Centro Dino Ferrari, Milan, Italy
• Elio Scarpini: Fondazione IRCCS Ca′ Granda Ospedale Maggiore Policlinico, Neurodegenerative Diseases Unit, Milan, Italy; University of Milan, Centro Dino Ferrari, Milan, Italy
• Vittoria Borracci: Fondazione IRCCS Ca′ Granda Ospedale Maggiore Policlinico, Neurodegenerative Diseases Unit, Milan, Italy; University of Milan, Centro Dino Ferrari, Milan, Italy
• Giacomina Rossi: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, Italy
• Giorgio Giaccone: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, Italy
• Giuseppe Di Fede: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, Italy
• Paola Caroppo: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, Italy
• Pietro Tiraboschi: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, Italy
• Sara Prioni: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, Italy
• Veronica Redaelli: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, Italy
• David Tang-Wai: The University Health Network, Krembil Research Institute, Toronto, Canada
• Ekaterina Rogaeva: Tanz Centre for Research in Neurodegenerative Diseases, University of Toronto, Toronto, Canada
• Miguel Castelo-Branco: Faculty of Medicine, University of Coimbra, Coimbra, Portugal
• Morris Freedman: Baycrest Health Sciences, Rotman Research Institute, University of Toronto, Toronto, Canada
• Ron Keren: The University Health Network, Toronto Rehabilitation Institute, Toronto, Canada
• Sandra Black: Sunnybrook Health Sciences Centre, Sunnybrook Research Institute, University of Toronto, Toronto, Canada
• Sara Mitchell: Sunnybrook Health Sciences Centre, Sunnybrook Research Institute, University of Toronto, Toronto, Canada
• Christen Shoesmith: Department of Clinical Neurological Sciences, University of Western Ontario, London, Ontario, Canada
• Robart Bartha: Department of Medical Biophysics, The University of Western Ontario, London, Ontario, Canada; Centre for Functional and Metabolic Mapping, Robarts Research Institute, The University of Western Ontario, London, Ontario, Canada
• Rosa Rademakers: Center for Molecular Neurology, University of Antwerp
• Jackie Poos: Department of Neurology, Erasmus Medical Center, Rotterdam, Netherlands
• Janne M. Papma: Department of Neurology, Erasmus Medical Center, Rotterdam, Netherlands
• Lucia Giannini: Department of Neurology, Erasmus Medical Center, Rotterdam, Netherlands
• Rick van Minkelen: Department of Clinical Genetics, Erasmus Medical Center, Rotterdam, Netherlands
• Yolande Pijnenburg: Amsterdam University Medical Centre, Amsterdam VUmc, Amsterdam, Netherlands
• Benedetta Nacmias: Department of Neuroscience, Psychology, Drug Research and Child Health, University of Florence, Florence, Italy
• Camilla Ferrari: Department of Neuroscience, Psychology, Drug Research and Child Health, University of Florence, Florence, Italy
• Cristina Polito: Department of Biomedical, Experimental and Clinical Sciences “Mario Serio”, Nuclear Medicine Unit, University of Florence, Florence, Italy
• Gemma Lombardi: Department of Neuroscience, Psychology, Drug Research and Child Health, University of Florence, Florence, Italy
• Valentina Bessi: Department of Neuroscience, Psychology, Drug Research and Child Health, University of Florence, Florence, Italy
• Michele Veldsman: Nuffield Department of Clinical Neurosciences, Medical Sciences Division, University of Oxford, Oxford, UK
• Christin Andersson: Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden
• Hakan Thonberg: Center for Alzheimer Research, Division of Neurogeriatrics, Karolinska Institutet, Stockholm, Sweden
• Linn Öijerstedt: Center for Alzheimer Research, Division of Neurogeriatrics, Department of Neurobiology, Care Sciences and Society, Bioclinicum, Karolinska Institutet, Solna, Sweden; Unit for Hereditary Dementias, Theme Aging, Karolinska University Hospital, Solna, Sweden
• Vesna Jelic: Division of Clinical Geriatrics, Karolinska Institutet, Stockholm, Sweden
• Paul Thompson: Division of Neuroscience and Experimental Psychology, Wolfson Molecular Imaging Centre, University of Manchester, Manchester, UK
• Tobias Langheinrich: Division of Neuroscience and Experimental Psychology, Wolfson Molecular Imaging Centre, University of Manchester, Manchester, UK; Manchester Centre for Clinical Neurosciences, Department of Neurology, Salford Royal NHS Foundation Trust, Manchester, UK
• Albert Lladó: Alzheimer’s Disease and Other Cognitive Disorders Unit, Neurology Service, Hospital Clínic, Barcelona, Spain
• Anna Antonell: Alzheimer’s Disease and Other Cognitive Disorders Unit, Neurology Service, Hospital Clínic, Barcelona, Spain
• Jaume Olives: Alzheimer’s Disease and Other Cognitive Disorders Unit, Neurology Service, Hospital Clínic, Barcelona, Spain
• Mircea Balasa: Alzheimer’s Disease and Other Cognitive Disorders Unit, Neurology Service, Hospital Clínic, Barcelona, Spain
• Nuria Bargalló: Imaging Diagnostic Center, Hospital Clínic, Barcelona, Spain
• Sergi Borrego-Ecija: Alzheimer’s Disease and Other Cognitive Disorders Unit, Neurology Service, Hospital Clínic, Barcelona, Spain
• Ana Verdelho: Department of Neurosciences and Mental Health, Centro Hospitalar Lisboa Norte – Hospital de Santa Maria & Faculty of Medicine, University of Lisbon, Lisbon, Portugal
• Carolina Maruta: Laboratory of Language Research, Centro de Estudos Egas Moniz, Faculty of Medicine, University of Lisbon, Lisbon, Portugal
• Catarina B. Ferreira: Laboratory of Neurosciences, Faculty of Medicine, University of Lisbon, Lisbon, Portugal
• Gabriel Miltenberger: Faculty of Medicine, University of Lisbon, Lisbon, Portugal
• Frederico Simões do Couto: Faculdade de Medicina, Universidade Católica Portuguesa
• Alazne Gabilondo: Cognitive Disorders Unit, Department of Neurology, Donostia University Hospital, San Sebastian, Gipuzkoa, Spain; Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, Spain
• Ana Gorostidi: Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, Spain
• Jorge Villanua: OSATEK, University of Donostia, San Sebastian, Gipuzkoa, Spain
• Marta Cañada: CITA Alzheimer, San Sebastian, Gipuzkoa, Spain
• Mikel Tainta: Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, Spain
• Miren Zulaica: Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, Spain
• Myriam Barandiaran: Cognitive Disorders Unit, Department of Neurology, Donostia University Hospital, San Sebastian, Gipuzkoa, Spain; Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, Spain
• Patricia Alves: Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, Spain; Department of Educational Psychology and Psychobiology, Faculty of Education, International University of La Rioja, Logroño, Spain
• Benjamin Bender: Department of Diagnostic and Interventional Neuroradiology, University of Tübingen, Tübingen, Germany
• Carlo Wilke: Department of Neurodegenerative Diseases, Hertie-Institute for Clinical Brain Research and Center of Neurology, University of Tübingen, Tübingen, Germany; Center for Neurodegenerative Diseases (DZNE), Tübingen, Germany
• Lisa Graf: Department of Neurodegenerative Diseases, Hertie-Institute for Clinical Brain Research and Center of Neurology, University of Tübingen, Tübingen, Germany
• Annick Vogels: Department of Human Genetics, KU Leuven, Leuven, Belgium
• Mathieu Vandenbulcke: Geriatric Psychiatry Service, University Hospitals Leuven, Belgium; Neuropsychiatry, Department of Neurosciences, KU Leuven, Leuven, Belgium
• Philip Van Damme: Neurology Service, University Hospitals Leuven, Belgium; Laboratory for Neurobiology, VIB-KU Leuven Centre for Brain Research, Leuven, Belgium
• Rose Bruffaerts: Department of Biomedical Sciences, University of Antwerp, Antwerp, Belgium; Biomedical Research Institute, Hasselt University, 3500 Hasselt, Belgium
• Koen Poesen: Laboratory for Molecular Neurobiomarker Research, KU Leuven, Leuven, Belgium
• Pedro Rosa-Neto: Translational Neuroimaging Laboratory, McGill Centre for Studies in Aging, McGill University, Montreal, Québec, Canada
• Serge Gauthier: Alzheimer Disease Research Unit, McGill Centre for Studies in Aging, Department of Neurology & Neurosurgery, McGill University, Montreal, Québec, Canada
• Agnès Camuzat: Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France
• Alexis Brice: Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France; Reference Network for Rare Neurological Diseases (ERN-RND)
• Anne Bertrand: Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France; Inria, Aramis project-team, F-75013, Paris, France; Centre pour l’Acquisition et le Traitement des Images, Institut du Cerveau et la Moelle, Paris, France
• Aurélie Funkiewiez: Centre de référence des démences rares ou précoces, IM2A, Département de Neurologie, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France; Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France
• Daisy Rinaldi: Centre de référence des démences rares ou précoces, IM2A, Département de Neurologie, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France; Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France; Département de Neurologie, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France
• Dario Saracino: Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France; Inria, Aramis project-team, F-75013, Paris, France; Centre de référence des démences rares ou précoces, IM2A, Département de Neurologie, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France
• Olivier Colliot: Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France; Inria, Aramis project-team, F-75013, Paris, France; Centre pour l’Acquisition et le Traitement des Images, Institut du Cerveau et la Moelle, Paris, France
• Sabrina Sayah: Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP – Hôpital Pitié-Salpêtrière, Paris, France
• Catharina Prix: Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, Germany
• Elisabeth Wlasich: Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, Germany
• Olivia Wagemann: Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, Germany
• Sandra Loosli: Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, Germany
• Sonja Schönecker: Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, Germany
• Tobias Hoegen: Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, Germany
• Jolina Lombardi: Department of Neurology, University of Ulm, Ulm, Germany
• Sarah Anderl-Straub: Department of Neurology, University of Ulm, Ulm, Germany
• Adeline Rollin: CHU, CNR-MAJ, Labex Distalz, LiCEND Lille, France
• Gregory Kuchcinski: Univ Lille, France; Inserm 1172, Lille, France; CHU, CNR-MAJ, Labex Distalz, LiCEND Lille, France
• Maxime Bertoux: Inserm 1172, Lille, France; CHU, CNR-MAJ, Labex Distalz, LiCEND Lille, France
• Thibaud Lebouvier: Univ Lille, France; Inserm 1172, Lille, France; CHU, CNR-MAJ, Labex Distalz, LiCEND Lille, France
• Vincent Deramecourt: Univ Lille, France; Inserm 1172, Lille, France; CHU, CNR-MAJ, Labex Distalz, LiCEND Lille, France
• Beatriz Santiago: Neurology Department, Centro Hospitalar e Universitario de Coimbra, Coimbra, Portugal
• Diana Duro: Faculty of Medicine, University of Coimbra, Coimbra, Portugal
• Maria João Leitão: Centre of Neurosciences and Cell Biology, Universidade de Coimbra, Coimbra, Portugal
• Maria Rosario Almeida: Faculty of Medicine, University of Coimbra, Coimbra, Portugal
• Miguel Tábuas-Pereira: Neurology Department, Centro Hospitalar e Universitario de Coimbra, Coimbra, Portugal
• Sónia Afonso: Instituto Ciencias Nucleares Aplicadas a Saude, Universidade de Coimbra, Coimbra, Portugal
Abbreviations
- AUC
Area under the curve
- avPPA
Agrammatic variant of primary progressive aphasia
- bvFTD
Behavioral variant frontotemporal dementia
- C9orf72
Chromosome 9 open reading frame 72
- CBS
Corticobasal syndrome
- CI
Confidence interval
- CDR plus NACC FTLD
CDR® Dementia Staging Instrument plus National Alzheimer’s Coordinating Centre behavior and language domains
- GENFI
Genetic Frontotemporal Initiative
- GRN
Progranulin
- HC
Healthy controls
- FTD
Frontotemporal dementia
- MAPT
Microtubule-associated protein tau
- MCBMI
Mild cognitive and/or behavioral and/or motor impairment
- MRI
Magnetic resonance imaging
- NfL
Neurofilament light
- PSP
Progressive supranuclear palsy
- ROC
Receiver operating characteristic
- svPPA
Semantic variant of primary progressive aphasia
Authors’ contributions
AB, BB, and JDR contributed to the conception and design of the work and the analysis of the data. AB and BB drafted the original work. All authors contributed to the acquisition and interpretation of the data and revised the work. All authors read and approved the final manuscript.
Funding
This work was supported by the MRC UK GENFI grant (MR/M023664/1), the Bluefield Project, and the JPND GENFI-PROX grant (2019-02248). Several authors of this publication are members of the European Reference Network for Rare Neurological Diseases – Project ID No 739510. AB was supported by the Airalzh-AGYR2020, by Fondazione Cariplo (grant n° 2021-1516), and by the Fondation pour la Recherche sur Alzheimer. JCVS was supported by the Dioraphte Foundation grant 09-02-03-00, the Association for Frontotemporal Dementias Research Grant 2009, the Netherlands Organisation for Scientific Research (NWO) grant HCMI 056-13-018, ZonMw Memorabel (Deltaplan Dementie, project number 733 051 042), Alzheimer Nederland, and the Bluefield project. FM received funding from the Tau Consortium and the Center for Networked Biomedical Research on Neurodegenerative Disease (CIBERNED). RS-V has received funding from Fundació Marató de TV3, Spain (grant no. 20143810). CG received funding from JPND-Prefrontals VR Dnr 529-2014-7504, VR 2015-02926, and 2018-02754; the Swedish FTD Inititative-Schörling Foundation; Alzheimer Foundation; Brain Foundation; and Stockholm County Council ALF. MM has received funding from a Canadian Institute of Health Research operating grant and the Weston Brain Institute and Ontario Brain Institute. JBR has received funding from the Welcome Trust (220258), the Cambridge University Centre for Frontotemporal Dementia, the Medical Research Council (SUAG/051 G101400), and the National Institute for Health Research (NIHR) Cambridge Biomedical Research Centre (BRC-1215-20014). EF has received funding from a CIHR grant #327387. DG received support from the EU Joint Programme – Neurodegenerative Disease Research (JPND) and the Italian Ministry of Health (PreFrontALS) grant 733051042. RV has received funding from the Mady Browaeys Fund for Research into Frontotemporal Dementia. MO has received funding from BMBF (FTLDc). HZ is a Wallenberg Scholar supported by grants from the Swedish Research Council (#2018-02532); the European Research Council (#681712), Swedish State Support for Clinical Research (#ALFGBG-720931); the Alzheimer Drug Discovery Foundation (ADDF), USA (#201809-2016862); the AD Strategic Fund and the Alzheimer’s Association (#ADSF-21-831376-C, #ADSF-21-831381-C, and #ADSF-21-831377-C); the Olav Thon Foundation; the Erling-Persson Family Foundation, Stiftelsen för Gamla Tjänarinnor, Hjärnfonden, Sweden (#FO2019-0228); the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement No. 860197 (MIRIADE); the European Union Joint Program for Neurodegenerative Disorders (JPND2021-00694); and the UK Dementia Research Institute at UCL. JL received funding for this work from the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) under Germany’s Excellence Strategy within the framework of the Munich Cluster for Systems Neurology (EXC 2145 SyNergy – ID 390857198). JDR is supported by the Miriam Marks Brain Research UK Senior Fellowship and has received funding from an MRC Clinician Scientist Fellowship (MR/M008525/1) and the NIHR Rare Disease Translational Research Collaboration (BRC149/NS/MH).
Availability of data and materials
All study data, including raw and analyzed data, and materials will be available from the corresponding author, B.B., upon reasonable request.
Declarations
Ethics approval and consent to participate
Local ethics committees approved the study at each site, and all participants provided written informed consent. The study was conducted according to the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jonathan D. Rohrer and Barbara Borroni contributed equally to the present study.
Contributor Information
Barbara Borroni, Email: bborroni@inwind.it.
Genetic Frontotemporal dementia Initiative (GENFI):
Annabel Nelson, Martina Bocchetta, David L. Thomas, Hanya Benotmane, Jennifer Nicholas, Rachelle Shafei, Carolyn Timberlake, Thomas Cope, Timothy Rittman, Andrea Arighi, Chiara Fenoglio, Elio Scarpini, Vittoria Borracci, Giacomina Rossi, Giorgio Giaccone, Giuseppe Di Fede, Paola Caroppo, Sara Prioni, Veronica Redaelli, David Tang-Wai, Ekaterina Rogaeva, Miguel Castelo-Branco, Morris Freedman, Ron Keren, Sandra Black, Sara Mitchell, Christen Shoesmith, Robart Bartha, Rosa Rademakers, Jackie Poos, Janne M. Papma, Lucia Giannini, Rick van Minkelen, Yolande Pijnenburg, Benedetta Nacmias, Camilla Ferrari, Cristina Polito, Gemma Lombardi, Valentina Bessi, Michele Veldsman, Christin Andersson, Hakan Thonberg, Linn Öijerstedt, Vesna Jelic, Paul Thompson, Tobias Langheinrich, Albert Lladó, Anna Antonell, Jaume Olives, Mircea Balasa, Nuria Bargalló, Sergi Borrego-Ecija, Ana Verdelho, Carolina Maruta, Catarina B. Ferreira, Gabriel Miltenberger, Frederico Simões do Couto, Alazne Gabilondo, Ana Gorostidi, Jorge Villanua, Marta Cañada, Mikel Tainta, Miren Zulaica, Myriam Barandiaran, Patricia Alves, Benjamin Bender, Carlo Wilke, Lisa Graf, Annick Vogels, Mathieu Vandenbulcke, Philip Van Damme, Rose Bruffaerts, Koen Poesen, Pedro Rosa-Neto, Serge Gauthier, Agnès Camuzat, Alexis Brice, Anne Bertrand, Aurélie Funkiewiez, Daisy Rinaldi, Dario Saracino, Olivier Colliot, Sabrina Sayah, Catharina Prix, Elisabeth Wlasich, Olivia Wagemann, Sandra Loosli, Sonja Schönecker, Tobias Hoegen, Jolina Lombardi, Sarah Anderl-Straub, Adeline Rollin, Gregory Kuchcinski, Maxime Bertoux, Thibaud Lebouvier, Vincent Deramecourt, Beatriz Santiago, Diana Duro, Maria João Leitão, Maria Rosario Almeida, Miguel Tábuas-Pereira, and Sónia Afonso
References
- 1.Rascovsky K, Hodges JR, Knopman D, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134:2456–77. doi: 10.1093/brain/awr179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gorno-Tempini ML, Hillis AE, Weintraub S, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76:1006–14. doi: 10.1212/WNL.0b013e31821103e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kertesz A, McMonagle P, Blair M, et al. The evolution and pathology of frontotemporal dementia. Brain. 2005;128:1996–2005. doi: 10.1093/brain/awh598. [DOI] [PubMed] [Google Scholar]
- 4.Carneiro F, Saracino D, Huin V, et al. Isolated parkinsonism is an atypical presentation of GRN and C9orf72 gene mutations. Parkinsonism Relat Disord. 2020;80:73–81. doi: 10.1016/j.parkreldis.2020.09.019. [DOI] [PubMed] [Google Scholar]
- 5.Gasca-Salas C, Masellis M, Khoo E, et al. Characterization of movement disorder phenomenology in genetically proven, familial frontotemporal lobar degeneration: a systematic review and meta-analysis. PLoS One. 2016;11:1–20. doi: 10.1371/journal.pone.0153852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benussi A, Alberici A, Samra K, et al. Conceptual framework for the definition of preclinical and prodromal frontotemporal dementia. Alzheimer’s Dement. 2022;18:1408–23. doi: 10.1002/alz.12485. [DOI] [PubMed] [Google Scholar]
- 7.van der Ende EL, Meeter LH, Poos JM, et al. Serum neurofilament light chain in genetic frontotemporal dementia: a longitudinal, multicentre cohort study. Lancet Neurol. 2019;18:1103–11. doi: 10.1016/S1474-4422(19)30354-0. [DOI] [PubMed] [Google Scholar]
- 8.McCarthy J, Borroni B, Sanchez-Valle R, et al. Data-driven staging of genetic frontotemporal dementia using multi-modal MRI. Hum Brain Mapp. 2022;43:1821–35. doi: 10.1002/hbm.25727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Borroni B, Padovani A. Dementia: a new algorithm for molecular diagnostics in FTLD. Nat Rev Neurol. 2013;9:241–2. doi: 10.1038/nrneurol.2013.72. [DOI] [PubMed] [Google Scholar]
- 10.Greaves CV, Rohrer JD. An update on genetic frontotemporal dementia. J Neurol. 2019;266:2075–86. doi: 10.1007/s00415-019-09363-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rohrer JD, Nicholas JM, Cash DM, et al. Presymptomatic cognitive and neuroanatomical changes in genetic frontotemporal dementia in the Genetic Frontotemporal dementia Initiative (GENFI) study: a cross-sectional analysis. Lancet Neurol. 2015;14:253–62. doi: 10.1016/S1474-4422(14)70324-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore KM, Nicholas J, Grossman M, et al. Age at symptom onset and death and disease duration in genetic frontotemporal dementia: an international retrospective cohort study. Lancet Neurol. 2020;19:145–56. doi: 10.1016/S1474-4422(19)30394-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Staffaroni AM, Quintana M, Wendelberger B, et al. Temporal order of clinical and biomarker changes in familial frontotemporal dementia. Nat Med. 2022;28:2194–206. doi: 10.1038/s41591-022-01942-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poos JM, Moore KM, Nicholas J, et al. Cognitive composites for genetic frontotemporal dementia: GENFI-Cog. Alzheimers Res Ther. 2022;14:1–12. doi: 10.1186/s13195-022-00958-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hughes CP, Berg L, Danziger WL, et al. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–72. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- 16.Knopman DS, Kramer JH, Boeve BF, et al. Development of methodology for conducting clinical trials in frontotemporal lobar degeneration. Brain. 2008;131:2957–68. doi: 10.1093/brain/awn234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miyagawa T, Brushaber D, Syrjanen J, et al. Utility of the global CDR ® plus NACC FTLD rating and development of scoring rules: data from the ARTFL/LEFFTDS Consortium. Alzheimer’s Dement. 2020;16:106–17. doi: 10.1002/alz.12033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Corrigan JD, Hinkeldey NS. Relationships between parts A and B of the Trail Making Test. J Clin Psychol. 1987;43:402–9. doi: 10.1002/1097-4679(198707)43:4<402::AID-JCLP2270430411>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 19.Lezak MD, Howieson D, Bigler E, et al. Neuropsychological assessment. (5th ed.). Oxford University Press; 2012.
- 20.Bertoux M, Delavest M, De Souza LC, et al. Social cognition and emotional assessment differentiates frontotemporal dementia from depression. J Neurol Neurosurg Psychiatry. 2012;83:411–6. doi: 10.1136/jnnp-2011-301849. [DOI] [PubMed] [Google Scholar]
- 21.Morris JC, Weintraub S, Chui HC, et al. The Uniform Data Set (UDS): clinical and cognitive variables and descriptive data from Alzheimer disease centers. Alzheimer Dis Assoc Disord. 2006;20:210–6. doi: 10.1097/01.wad.0000213865.09806.92. [DOI] [PubMed] [Google Scholar]
- 22.Moore K, Convery R, Bocchetta M, et al. A modified Camel and Cactus Test detects presymptomatic semantic impairment in genetic frontotemporal dementia within the GENFI cohort. Applied Neuropsychology Adult. 2020;29:1–8. doi: 10.1080/23279095.2020.1716357. [DOI] [PubMed] [Google Scholar]
- 23.Samra K, MacDougall AM, Peakman G, et al. Motor symptoms in genetic frontotemporal dementia: developing a new module for clinical rating scales. J Neurol. 2023;270:1466–77. doi: 10.1007/s00415-022-11442-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuhle J, Barro C, Andreasson U, et al. Comparison of three analytical platforms for quantification of the neurofilament light chain in blood samples: ELISA, electrochemiluminescence immunoassay and Simoa. Clin Chem Lab Med. 2016;54:1655–61. doi: 10.1515/cclm-2015-1195. [DOI] [PubMed] [Google Scholar]
- 25.Harper L, Fumagalli GG, Barkhof F, et al. MRI visual rating scales in the diagnosis of dementia: evaluation in 184 post-mortem confirmed cases. Brain. 2016;139:1211–25. doi: 10.1093/brain/aww005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chu M, Liu L, Wang J, et al. Investigating the roles of anterior cingulate in behavioral variant frontotemporal dementia: a PET/MRI study. J Alzheimer’s Dis. 2021;84:1771–9. doi: 10.3233/JAD-215127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barker MS, Manoochehri M, Rizer SJ, et al. Recognition memory and divergent cognitive profiles in prodromal genetic frontotemporal dementia. Cortex. 2021;139:99–115. doi: 10.1016/j.cortex.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Staffaroni AM, Bajorek L, Casaletto KB, et al. Assessment of executive function declines in presymptomatic and mildly symptomatic familial frontotemporal dementia: NIH-EXAMINER as a potential clinical trial endpoint. Alzheimer’s Dement. 2020;16:11–21. doi: 10.1016/j.jalz.2019.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Malpetti M, Jones PS, Tsvetanov KA, et al. Apathy in presymptomatic genetic frontotemporal dementia predicts cognitive decline and is driven by structural brain changes. Alzheimer’s Dement. 2020;17:969–83. [DOI] [PMC free article] [PubMed]
- 30.Tavares TP, Mitchell DGV, Coleman KKL, et al. Early symptoms in symptomatic and preclinical genetic frontotemporal lobar degeneration. J Neurol Neurosurg Psychiatry. 2020;91:975–84. doi: 10.1136/jnnp-2020-322987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Benussi A, Premi E, Gazzina S, et al. Progression of behavioral disturbances and neuropsychiatric symptoms in patients with genetic frontotemporal dementia. JAMA Netw Open. 2021;4:1–17. doi: 10.1001/jamanetworkopen.2020.30194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ducharme S, Dols A, Laforce R, et al. Recommendations to distinguish behavioural variant frontotemporal dementia from psychiatric disorders. Brain. 2020;143:1632–50. doi: 10.1093/brain/awaa018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jack CR, Bennett DA, Blennow K, et al. NIA-AA Research Framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14:535–62. doi: 10.1016/j.jalz.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McKeith IG, Ferman TJ, Thomas AJ, et al. Research criteria for the diagnosis of prodromal dementia with Lewy bodies. Neurology. 2020;94:743–55. doi: 10.1212/WNL.0000000000009323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Benussi A, Ashton NJ, Karikari TK, et al. Prodromal frontotemporal dementia: clinical features and predictors of progression. Alzheimers Res Ther. 2021;13:188. doi: 10.1186/s13195-021-00932-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Benussi A, Cantoni V, Rivolta J, et al. Classification accuracy of blood-based and neurophysiological markers in the differential diagnosis of Alzheimer’s disease and frontotemporal lobar degeneration. Alzheimers Res Ther. 2022;14:155. doi: 10.1186/s13195-022-01094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gami-Patel P, Scarioni M, Bouwman FH, et al. The severity of behavioural symptoms in FTD is linked to the loss of GABRQ-expressing VENs and pyramidal neurons. Neuropathol Appl Neurobiol. 2022;48. 10.1111/nan.12798. [DOI] [PMC free article] [PubMed]
- 38.Rus T, Perovnik M, Vo A, et al. Disease specific and nonspecific metabolic brain networks in behavioral variant of frontotemporal dementia. Hum Brain Mapp. Published Online First: 5 November 2022. 10.1002/hbm.26140. [DOI] [PMC free article] [PubMed]
- 39.Heuer HW, Wang P, Rascovsky K, et al. Comparison of sporadic and familial behavioral variant frontotemporal dementia (FTD) in a North American cohort. Alzheimer’s Dement. 2020;16:60–70. doi: 10.1002/alz.12046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Capozzo R, Sassi C, Hammer MB, et al. Clinical and genetic analyses of familial and sporadic frontotemporal dementia patients in Southern Italy. Alzheimer’s Dement. 2017;13:858–69. doi: 10.1016/j.jalz.2017.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Benussi A, Libri I, Premi E, et al. Differences and similarities between familial and sporadic frontotemporal dementia: an Italian single‐center cohort study. Alzheimer’s Dement. 2022;8. 10.1002/trc2.12326. [DOI] [PMC free article] [PubMed]
- 42.Mori K, Arzberger T, Grässer FA, et al. Bidirectional transcripts of the expanded C9orf72 hexanucleotide repeat are translated into aggregating dipeptide repeat proteins. Acta Neuropathol. 2013;126:881–93. doi: 10.1007/s00401-013-1189-3. [DOI] [PubMed] [Google Scholar]
- 43.Zu T, Gibbens B, Doty NS, et al. Non-ATG-initiated translation directed by microsatellite expansions. Proc Natl Acad Sci U S A. 2011;108:260–5. doi: 10.1073/pnas.1013343108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bieniek KF, Murray ME, Rutherford NJ, et al. Tau pathology in frontotemporal lobar degeneration with C9ORF72 hexanucleotide repeat expansion. Acta Neuropathol. 2013;125:289–302. doi: 10.1007/s00401-012-1048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ward ME, Chen R, Huang H-Y, et al. Individuals with progranulin haploinsufficiency exhibit features of neuronal ceroid lipofuscinosis. https://www.science.org. [DOI] [PMC free article] [PubMed]
- 46.Giannini LAA, Ohm DT, Rozemuller AJM, et al. Isoform-specific patterns of tau burden and neuronal degeneration in MAPT-associated frontotemporal lobar degeneration. Acta Neuropathol. 2022;144:1065–84. doi: 10.1007/s00401-022-02487-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Paternicò D, Premi E, Gazzina S, et al. White matter hyperintensities characterize monogenic frontotemporal dementia with granulin mutations. Neurobiol Aging. 2016;38:176–80. doi: 10.1016/j.neurobiolaging.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 48.Sudre CH, Bocchetta M, Cash D, et al. White matter hyperintensities are seen only in GRN mutation carriers in the GENFI cohort. Neuroimage Clin. 2017;15:171–80. doi: 10.1016/j.nicl.2017.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Swift IJ, Sogorb-Esteve A, Heller C, et al. Fluid biomarkers in frontotemporal dementia: past, present and future. J Neurol Neurosurg Psychiatry. 2020;92:204–15 [DOI] [PubMed]
- 50.Barker MS, Gottesman RT, Manoochehri M, et al. Proposed research criteria for prodromal behavioural variant frontotemporal dementia. Brain. 2022;145:1079–97. doi: 10.1093/brain/awab365. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Diagnostic accuracy of each domain of proposed MCBMI criteria in classifying prodromal FTD from healthy controls. Table S2. Diagnostic accuracy of proposed criteria in classifying prodromal FTD from healthy controls for each genetic group. Table S3. Diagnostic accuracy of each subdomain of proposed MCBMI criteria in classifying prodromal FTD from healthy controls.
Data Availability Statement
All study data, including raw and analyzed data, and materials will be available upon reasonable request.
All study data, including raw and analyzed data, and materials will be available from the corresponding author, B.B., upon reasonable request.


