Abstract
Documentation burden is experienced by clinical end-users of the electronic health record. Flowsheet measure reuse and clinical concept redundancy are two contributors to documentation burden. In this paper, we described nursing flowsheet documentation hierarchy and frequency of use for one month from two hospitals in our health system. We examined respiratory care management documentation in greater detail. We found 59 instances of reuse of respiratory care flowsheet measure fields over two or more templates and groups, and 5 instances of clinical concept redundancy. Flowsheet measure fields for physical assessment observations and measurements were the most frequently documented and most reused, whereas respiratory intervention documentation was less frequently reused. Further research should investigate the relationship between flowsheet measure reuse and redundancy and EHR information overload and documentation burden.
Introduction
Documentation burden is an ongoing challenge in healthcare. It can affect clinicians and patients by contributing to healthcare professional burnout, and negatively impacting patient safety and outcomes. The universal adoption of electronic medical records in healthcare, ongoing federal policy changes (i.e., 21st Century Cures Act and Open Notes, electronic prior authorization), and individual health system requirements, necessitate that defining, measuring, and addressing documentation burden for clinical end-users become a top priority. Robust and ongoing efforts are underway at the local, national, and international levels to address documentation burden in the near and longer terms. Two recent examples include the American Medical Informatics Association (AMIA) 25x5 Taskforce)1 to reduce documentation burden to 25% of its current state by 2026 and the US Surgeon General’s taskforce on clinician wellbeing,2 which highlights addressing documentation burden as one element of the proposed action plan.
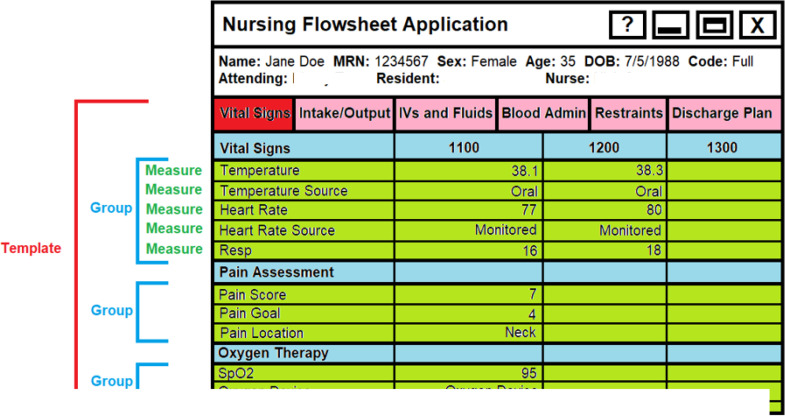
Registered nurses (RNs) spend nearly 25% of their shift interacting with the electronic health record (EHR).3 These activities include entering, locating, viewing, and synthesizing data. Also associated with these workflows include the cognitive load associated with switching between these documentation tasks.4 The largest volume of nursing data is captured in structured flowsheets (Figure 1). This figure illustrates the hierarchical presentation of flowsheet documentation to nurses and other clinician end-users in the EHR. The templates, noted in red in Figure 1, are the broadest categories for organizing patient care observations. In this figure, the templates which include Vital Signs, Intake/Output, IV and Fluids, Blood Administration, etc. provide a framework for increasingly granular groups and flowsheet measure fields to systematically document individual patient care activities and clinical findings. Groups, noted in blue in Figure 1, are collections of flowsheet measure fields. In this example, the Vital Sign template contains three groups (vital signs, pain assessment, and oxygen therapy). Finally, flowsheet measure fields, found in green, are the areas in the EHR where clinicians document individual patient-level observation (discrete) and measurement (numeric) values. In this example, Pain Score is a flowsheet measure field, which contains a patient’s reported value of 7 (out of 0-10 pain scale) which was recorded at 11am. Narrative notes and other data entry formats are also used by nurses in the EHR, but typically with less volume and less frequency than flowsheets. Nursing practice standards for documentation are informed by compliance, regulatory, and clinical guidelines, and are set by individual institutions. At our study site, the documentation that registered nurses (RNs) working on an inpatient acute care unit (i.e., non-intensive care units) are required to complete each shift includes Pain Assessment, Fall Assessment, Skin Assessment, Patient Positioning, Laboratory Tasks, Patient Education, Care Plan, and Physical Assessment. Additional documentation that might occur during the shift can include more frequent flowsheet entries of patient-level data that are reflective of clinical changes, or documentation of escalation communication to the care team around significant clinical events and subsequent interventions or assessments.
Figure 1.
Hierarchy of flowsheet documentation
Identifying the structure and content of nursing documentation templates, groups, and flowsheet measure fields is elemental to understanding the breadth and depth of documentation requirements and information overload, including instances of documentation reuse versus instances of redundant documentation, to inform documentation burden reduction efforts. In this study, we define flowsheet documentation as reuse when a unique flowsheet measure field is found in more than one template or group. We define flowsheet documentation redundancy as when more than one unique flowsheet measure field is used to capture the same clinical concept. For example, there may be a flowsheet measurement field to capture Respiratory (WDL) and another flowsheet measurement field to capture Respiratory WDL, each with slightly different names and different database IDs. The purpose of this work is to 1) analyze and describe the flowsheet content hierarchy for intensive care units (ICU) and acute care units (i.e., non-intensive care units), and 2) identify flowsheet instances of documentation reuse and redundancies related to the respiratory care management domain.
Methods
Dataset preparation
Flowsheet data were extracted from Epic for the most recent month of August 2022 to analyze nursing documentation burden. Given the large volume of flowsheet documentation generated daily, one month of data was determined to be sufficient for this analysis. The extracted data set of flowsheet data included patient encounter identifier or contact serial number (CSN), medical record number (MRN), flowsheet measure identifier, flowsheet measure display name, flowsheet group identifier, flowsheet group display name, flowsheet template identifier, flowsheet template display name, recorded date and time for captured measurements, data entry date and time by registered nurses, registered nurse user identifier, registered nurse user name, provider type, provider degree, and captured measurement values. Additionally, the role type ‘RN’ for registered nurse was used to filter for data entered by registered nurses only. Finally, these data were filtered to include documentation for inpatient encounters only. The dataset was exported to Excel.
Analysis and description of the flowsheet content hierarchy for both intensive care units (ICU) and acute care units (i.e., non-intensive care units).
To begin the descriptive analysis, the dataset was manually reviewed for null or retired entries, which were removed. We then were able to determine the total number of template, groups, and flowsheet measure fields that existed. Next, duplicate entries for template IDs, group IDs, and flowsheet measure field IDs were then evaluated to obtain the total number of unique templates, groups, and flowsheet measure fields. Averages and ranges were reported for groups and flowsheet measures. These findings were calculated manually, and then verified by the data engineer through back-end database queries.
Parsing of respiratory documentation
We then chose a portion of the dataset to explore in greater detail to identify potential redundancies and instances of reuse in acute care nursing documentation for respiratory care management. To identify all flowsheet content related to respiratory care management, we performed a multi-stage review of flowsheet content that included: 1) term matching, 2) subject matter expert iterative reviews and face validity. First, we removed any documentation that was used in the ICU setting only, and we accomplished this by reviewing the usage and the names of the templates that would include critical care documentation. Then we identified flowsheet templates, groups, and flowsheet measures that would likely be used to document nursing assessment and care for the respiratory system specifically (e.g., Respiratory Assessment), as well as those that would likely include documentation pertaining to the respiratory system (e.g., Patient Controlled Analgesia template). Key terms and concepts of interest included: lung, breathing, cough, inspiration, ventilation, respiration, inhalation, exhalation, inspiratory, and oxygenation or/and conveyed clinical concepts related to respiratory care management. The primary author initiated this step by manually looking at the template display names, group display names, and flowsheet measure field names. This initial review resulted in a dataset of 47 flowsheet templates and their associated groups and flowsheet measure field names. This respiratory-focused subset was iteratively reviewed and subsequently validated by the primary author and a clinical subject matter expert (BS), who is a practicing registered professional nurse at the study site and is well acquainted with its EHR and the documentation standards for the acute care (i.e., non-ICU) setting. An additional validation step included cross walking the template names with the nursing documentation standard for acute care of the organization. Once the respiratory documentation hierarchy was determined, the number of instances of reuse for each unique flowsheet measure field ID across groups and templates was tallied. Finally, a manual review was conducted to determine instances of redundancy.
Results
The overall EHR documentation content for both ICU and acute care settings was analyzed descriptively and included unique counts, ranges, and averages (Table 1a, 1b).
Table 1a.
Total Number of Unique Templates, Groups, Flowsheet Measure Fields
| Documentation Type | Unique Counts |
|---|---|
| Templates | 292 |
| Groups | 777 |
| Flowsheet Measures | 3272 |
Table 1b.
Counts of Flowsheet Structures within Flowsheet Hierarchy
| Parent Flowsheet Structure | Children Flowsheet Structures = Average (Range) | |
|---|---|---|
| Templates | group IDs = 43 (1-115) | flowsheet measure field IDs = 203 (1-658) |
| Groups | flowsheet measure field IDs = 12 (1-49) |
The respiratory-specific documentation dataset, a subset of the original dataset, is described in Table 2a. There were 167 unique flowsheet measures which included 59 instances of reuse noted across several flowsheet templates. These are noted in Table 2b.
Table 2a.
Respiratory Documentation Hierarchy in Acute Care Settings
| Documentation Type | Unique Counts | Instances of Flowsheet Measure Field Reuse Across Templates or Groups: Total, (Average, Range) | |
|---|---|---|---|
| Templates | 16 | ||
| Groups | 24 | ||
| Flowsheet Measures | 167 | Field only used once | 108 |
| Field used more than once | 59 (3.75, 2-7) | ||
Table 2b.
Flowsheet Measure Fields Reused Across Template or Groups (n=59)
| Flowsheet Measure Field Names | |
|---|---|
| Resp Rate | Retraction Location |
| SpO2 | Suction Device |
| Respiratory Rate Source | Trigger Sensitivity Pressure (cmH2O) |
| Oximetry Probe Site | Waveform |
| O2 Flow Rate | Trigger Sensitivity Flow |
| FiO2 (%) | Humidification |
| Resp Rate (Set) | Disconnect Sensitivity (%) |
| Vt (Set, mL) | Heater Temperature |
| Pressure Support Set (above PEEP) (cmH2O) | Vent Mode |
| Bilateral Breath Sounds | Respiratory Interventions |
| Right Breath Sounds | Cough and Deep Breathe |
| Left Breath Sounds | Airway LDA |
| Respiratory Pattern | Respiratory Additional Assessments |
| Chest Assessment | Oximetry Probe Site Changed |
| Cough | Pulse Oximetry Type |
| Respiratory WDL | Suction Type |
| $ Delivery Source | Airway Suction Tolerance |
| $ Suction | Suctioning Adverse Effects |
| PIP Set (Above PEEP) (cmH2O) | $ Oxygen Therapy |
| Insp Time Measured (sec) | O2 Delivery Method 1 |
| Insp Flow (L/sec) | Respiratory Effort |
| Duration (Minutes) | Respiratory Effort Characteristics |
| Breath Sounds Pre-Treatment Right | Respiratory Depth/Rhythm |
| Breath Sounds Post-Treatment Right | Airway Clearance Treatment Tolerance |
| Breath Sounds Pre-Treatment Left | Secretion Amount |
| Breath Sounds Post-Treatment Left | Secretion Color |
| Position | Secretion Consistency |
| Dyspnea Occurrence | Airway Suction Count per Hour (RN only) |
Table 3 provides counts of the top 15 most frequently documented respiratory care management flowsheet measure fields out of 167 total, and the number of templates or groups they were reused in, if applicable.
Table 3.
Top 15 Most Frequent Respiratory Care Management Flowsheet Measure Fields in Acute Care Documentation
| Flowsheet Measure Field Display Name | Number of Patient Data Points Recorded in each Flowsheet Measure Field in one month of EHR Data | Reused? If, yes, the number of instances | Purpose of Flowsheet Measure – Assessment, Intervention, or Outcome |
|---|---|---|---|
| Resp Rate | 1,668,622 | Yes, 7 | Assessment |
| Respiratory Rate Source | 1,402,257 | Yes, 6 | Assessment |
| FiO2 % | 190,990 | Yes, 4 | Intervention |
| Respiratory Interventions | 147,724 | Yes, 2 | Intervention |
| SpO2 | 146,525 | Yes, 3 | Assessment |
| O2 Flow Rate | 146,283 | Yes, 2 | Intervention |
| Oximetry Probe Site | 144,794 | Yes, 2 | Assessment |
| Oximetry Probe Site Changed | 144,737 | Yes, 2 | Intervention |
| Right Breath Sounds | 98,870 | Yes, 5 | Assessment |
| Left Breath Sounds | 98,870 | Yes, 5 | Assessment |
| Respiratory Pattern | 98,870 | Yes, 5 | Assessment |
| Chest Assessment | 98,870 | Yes, 5 | Assessment |
| Cough | 98,675 | Yes, 7 | Assessment |
| Bilateral Breath Sounds | 97,139 | Yes, 4 | Assessment |
| Respiratory – WDL | 42,993 | No | Assessment |
Finally, instances of flowsheet measure field reuse were more prevalent with 59, as compared to the five instances of redundancies, listed in Table 4.
Table 4.
Flowsheet Field Measure Redundancies Across Template or Groups (n=5)
| Flowsheet Field Measure Name | Flowsheet Measure Field ID | Number of times Flowsheet Field reused in EHR |
|---|---|---|
| Cough | 302590 | 7 |
| Cough Present | 5203025902 | 2 |
| O2 Delivery Method 1 | 3040109305 | 2 |
| O2 Delivery Method 2 | 3040920211 | 1 |
| Obstructed | 160237701 | 1 |
| Obstructed by | 160237901 | 1 |
| Respiratory (WDL) | 305410 | 2 |
| Respiratory WDL | 302380 | 1 |
| Respiratory (WDL) | 5203054101 | 1 |
| Breathing (WDL) | 1010010014 | 1 |
| Suction Device | 3040100614 | 5 |
| Suction Type | 3040103233 | 5 |
Discussion
Nurses primarily use flowsheets to document patient care measurements and observations. Collins and colleagues used nursing flowsheet data to quantify the volume of documentation that nurses are generating within a 12-hour shift.5 Administrative documentation burden, in addition to the patient data documentation required for clinical care, can contribute to an increased workload for nurses.6 Previous literature has focused on making nursing flowsheet data stored in the clinical data warehouse more useable for research and quality improvement initiatives by hierarchically organizing the data through clustering and reducing clinical concept redundancy.7-10
In this work, we found 59 instances of reuse of respiratory care flowsheet measure fields over two or more templates and groups, and 5 instances of clinical concept redundancy. While there can be some advantages to reusing data fields in the EHR, overall flowsheet measure reuse and/or redundancy contribute to a bloated EHR and can result in information overload and difficulties with information retrieval. The reuse of the flowsheet measures fields was noted most often with assessment documentation rather than intervention documentation. Assessment documentation is a record of the RN’s clinical observations and measurements of individual patients at a fixed point in time. Intervention documentation involves the recording of the actions an RN takes to implement the patient’s plan of care. One possible explanation that the reuse of flowsheet measures was highest for assessment information could be that assessment documentation is inextricably tied to other physiological systems and may be included across many flowsheet templates and groups with the goal of minimizing nurses having to switch screens while documenting on related clinical information.
The use of best practices for controlled terminologies in the creation of flowsheet data elements would minimize the redundancies observed. For example, some of the redundancies were due to spelling or character errors (Respiratory (WDL)) and others were due to a lack of standard naming conventions (cough vs cough present). Finally, others reflect a limitation of EHR data structures inability to handle multiple instances of the same concepts (O2 Delivery Method 1 and O2 Delivery Method 2).
Future research will focus on understanding the nurses’ documentation practices when faced with clinically redundant fields (as noted in Table 4). We hypothesize that there are workflow differences, unit culture differences, or clinician characteristics and preferences may be possible contributors. We will also investigate from the perspective of the end user whether EHR configuration is a factor driving redundancy. Featuring the voices of nurses and other healthcare professionals in documentation burden mitigation efforts will be essential to ensure that there are not unintended consequences, such as clinician frustration, or workarounds, as examples.
Limitations
There were several limitations to this analysis. The first is that we only examined one month of nursing flowsheet documentation for two campuses and two care settings (acute care and ICU) of one hospital system. The second limitation is that the respiratory care management was conducted for acute care (e.g., non-critical care, ICU patients) only. Critical care and ICU settings have additional and different templates, groups, and flowsheet measure fields than acute care settings. This work will need to be expanded to other inpatient settings to understand the full breadth of EHR content and nursing flowsheet documentation. The dataset used in our study was not mapped to a standard terminology, but this is part of our current work to align the flowsheet content across our study sites for analyses of documentation patterns.
Conclusion
Documentation burden is experienced by clinical end-users of the electronic health record, including RNs, providers, and other healthcare professionals. In this paper, we described nursing documentation, specifically structured flowsheet documentation, to illustrate the hierarchy and frequency of use for one month of data generated from two hospitals in our health system. We also explored the respiratory documentation domain in greater detail to identify instances of flowsheet measure fields reuse and template, group, and flowsheet measure field redundancies, laying the groundwork for a broader analysis across other physiological domains in flowsheets. Further research should investigate the relationship between flowsheet measure reuse and redundancy and EHR information overload and documentation burden.
Acknowledgements:
This work was funded by AHRQ 1R01HS028454-01A1. JW is a postdoctoral research fellow supported by the Reducing Health Disparities through Informatics training grant (T32NR007969). AM was supported by the U.S. National Library of Medicine training fellowship (5T15LM007079), the Agency for Healthcare Research and Quality (R01HS028454), and the National Institute for Nursing Research (1R01NR016941-01). RL is a postdoctoral research scientist supported through the Communicating Narrative Concerns Entered by RNs grant through the National Institute for Nursing Research (NR016941-01).
Figures & Tables
References
- 1.AMIA 25x5: Reducing Documentation Burden to 25% of Current State in Five Years. Accessed on March 20, 2023. https://amia.org/about-amia/amia-25x5.
- 2.Murthy VH. Confronting health worker burnout and well-being. New England Journal of Medicine. 2022 Aug 18;387(7):577–9. doi: 10.1056/NEJMp2207252. [DOI] [PubMed] [Google Scholar]
- 3.Pinevich Y, Clark KJ, Harrison AM, Pickering BW, Herasevich V. Interaction time with electronic health records: a systematic review. Applied clinical informatics. 2021 Aug;12(04):788–99. doi: 10.1055/s-0041-1733909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moy AJ, Aaron L, Cato KD, et al. Characterizing Multitasking and Workflow Fragmentation in Electronic Health Records among Emergency Department Clinicians: Using Time-Motion Data to Understand Documentation Burden. Appl Clin Inform. 2021;12(5):1002–1013. doi: 10.1055/s-0041-1736625. doi:10.1055/s-0041-1736625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collins S, Couture B, Kang MJ, Dykes P, Schnock K, Knaplund C, Chang F, Cato K. Quantifying and visualizing nursing flowsheet documentation burden in acute and critical care. AMIA Annual Symposium Proceedings. 2018;Vol. 2018:p. 348. American Medical Informatics Association. [PMC free article] [PubMed] [Google Scholar]
- 6.De Groot K., De Veer A. J., Munster A. M., Francke A. L., Paans W. Nursing documentation and its relationship with perceived nursing workload: a mixed-methods study among community nurses. BMC nursing. 2022;21(1):1–12. doi: 10.1186/s12912-022-00811-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Westra BL, Christie B, Johnson SG, Pruinelli L, LaFlamme A, Sherman SG, Park JI, Delaney CW, Gao G, Speedie S. Modeling flowsheet data to support secondary use. Computers, informatics, nursing: CIN. 2017 Sep;35(9):452. doi: 10.1097/CIN.0000000000000350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sutton D. E., Fogel J. R., Giard A. S., Gulker L. A., Ivory C. H., Rosa A. M. Defining an essential clinical dataset for admission patient history to reduce nursing documentation burden. Applied Clinical Informatics. 2020;11(03):464–473. doi: 10.1055/s-0040-1713634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Westra BL, Lytle KS, Whittenburg L, Adams M, Ali S, Furukawa M, Hartleben S, Hook M, Johnson S, Collins Rossetti S, Settergren T. A refined methodology for validation of information models derived from flowsheet data and applied to a genitourinary case. Journal of the American Medical Informatics Association. 2020 Nov;27(11):1732–40. doi: 10.1093/jamia/ocaa166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lytle KS, Westra BL, Whittenburg L, Adams M, Akre M, Ali S, Furukawa M, Hartleben S, Hook M, Johnson SG, Settergren T. Information models offer value to standardize electronic health record flowsheet data: A fall prevention exemplar. Journal of nursing scholarship. 2021 May;53(3):306–14. doi: 10.1111/jnu.12646. [DOI] [PubMed] [Google Scholar]