Abstract
This study explores the variability in nursing documentation patterns in acute care and ICU settings, focusing on vital signs and note documentation, and examines how these patterns vary across patients’ hospital stays, documentation types, and comorbidities. In both acute care and critical care settings, there was significant variability in nursing documentation patterns across hospital stays, by documentation type, and by patients’ comorbidities. The results suggest that nurses adapt their documentation practices in response to their patients’ fluctuating needs and conditions, highlighting the need to facilitate more individualized care and tailored documentation practices. The implications of these findings can inform decisions on nursing workload management, clinical decision support tools, and EHR optimizations.
Introduction
Nursing documentation in electronic health records (EHRs) is vital for clinical decision-making, communication among care teams, and legal recordkeeping. Variability in nursing documentation patterns refers to differences in how nurses document, such as the frequency and timing of documentation, and the types of data documented. The variability in nursing documentation patterns reflects the active decision-making and expertise that underlie the nursing process. Nurses draw on their observations and knowledge to make complex judgments that guide their patient care actions, with these patterns revealing important signals regarding nurses’ concerns for clinical deterioration and patients’ health status. Several studies have demonstrated variabilities in nursing documentation patterns based on the types of data and external factors such as nursing staff workload documentation burden, facility types, nursing practice standards, and unit culture1-3.
A number of studies have examined nursing documentation patterns and their associations with patient outcomes. For example, documenting vital signs more frequently than the minimum requirement is associated with higher mortality and cardiac arrest rates, suggesting that increased documentation frequency may reflect a nurse’s increased concern regarding a patient’s deteriorating health4,5. A recent study found that in ICUs, nursing documentation patterns such as increased documentation of heart rate and body temperature were significantly associated with a higher likelihood of patient mortality, while in acute care units, increased documentation of blood pressure, respiratory rate with comments, and withheld medications were associated with a higher likelihood of patient mortality6. Therefore, understanding nursing documentation patterns can reveal important signals that may not be evident from data values alone. These signals have been leveraged in the CONCERN (Communicating Narrative Concerns entered by RNs) predictive model and clinical decision support tool to identify early warning signs of patient deterioration. CONCERN uses real-time analytic approaches that account for the temporal signals of each data point of nursing documentation, such as an increased number of documentation entries during uncommon times and optional documentation, to predict patient deterioration7,8.
Despite the importance of nursing documentation patterns, as evidenced by the CONCERN study, there is a lack of research on how these patterns vary across the days of patients’ inpatient hospitalization. As patients’ conditions and needs evolve during their hospital stay, nursing documentation patterns may also change, with nurses adjusting the frequency and types of documentation based on their assessment of the patient’s condition. For example, during the initial days of hospitalization, nurses may document more frequently as they assess and monitor the patient’s condition. As the patient stabilizes, the frequency of documentation may decrease. On the other hand, if a patient’s condition worsens, the frequency of documentation may increase as nurses monitor the patient more closely. The types of documentation may also vary as the patient’s condition changes, with nurses focusing on different aspects of care or interventions as the patient progresses through their hospital stay. Overall, understanding how nursing documentation patterns change across patients’ hospital stay can provide valuable insights into how nurses are adapting their practices to address the changing needs of their patients. Establishing a baseline of nursing documentation patterns across hospital days can also be useful to identify when nurses change those patterns in response to varying patient states and conditions. These insights can inform decisions about nursing workload management, identify areas where documentation standards and practices may need to be revised, and facilitate efforts to streamline documentation processes, ultimately reducing documentation burden. Documentation burden is a critical problem impacting the health professional workforce and is prioritized by the Office of the Surgeon General, Centers for Medicare and Medicaid, and the National Academy 9-11. Interestingly, some of the strongest signals in the CONCERN model are nurse documentation patterns that are above and beyond the documentation requirements. A deeper understanding of the interplay between documentation requirements, documentation patterns, patient states, and statistical signals is needed to guide burden reduction efforts.
In this study, we explored how nursing documentation patterns vary across patients’ hospital stays. Specifically, we aimed to 1) describe the patterns of nursing documentation over the first 10 days of hospitalization, 2) examine whether there are significant variations in documentation frequency across days of hospital stays and the types of documentation, and 3) explore how nursing documentation patterns differ across patients’ hospital stays based on their levels of comorbidities.
Methods
We conducted a retrospective analysis of all vital signs and nursing notes entries documented in the Epic EHR system at a large academic hospital in New York City over 12 months from January 2022 to December 2022. Our study included all patients aged 18 years or older admitted to any of our 13 CONCERN study units, including 9 acute care units and 4 ICUs. Patients with a total duration of hospital stay less than 24 hours were excluded. For each data point entered, we collected data element name, unique patient encounter identifier, date and time of data entry, clinical unit type (acute vs. critical care), Charlson Comorbidity Index (CCI) category, admission date and time, and demographic characteristics for each patient, such as age at admission, gender, race, and ethnicity.
Our study focused on five vital signs commonly collected for routine clinical nursing practice in inpatient settings: body temperature, blood pressure, oxygen saturation, pulse rate, and respiration rate. Since we were interested in nursing documentation patterns, we only included vital sign entries in nursing flowsheets. To address the issue of reuse of data elements and different data element names for the same vital sign, if a patient had data entered for any of the different names for the same vital sign concept with the same time stamp, it was counted as one. In addition to vital signs, we also included nursing notes documented in the EHR. Nursing notes included the following note names from our EHR: note, nurse note, and progress notes authored by registered nurses. As a measure of patients’ complexities, we used the Charlson Comorbidity Index (CCI) scores that were available through our EHR system. The CCI is a widely used tool that categorizes the comorbidities of patients based on their medical history, using the International Classification of Diseases (ICD) codes. A score of zero indicates the absence of comorbidities, whereas higher scores indicate an increased likelihood of adverse outcomes such as mortality or increased resource consumption12. To classify the scores, we utilized the commonly used categorization of CCI into four categories: 0, 1-2, 3-4, and 5 or higher, which respectively represent none, low, moderate, and high comorbidities.
We calculated the number of days since admission (i.e., length of hospital stays in days) for each data entry by subtracting the date and time of the data point entered from the admission start date and time. To analyze the data, we grouped the data points entered by patient encounter IDs and documentation types (blood pressure, pulse, respiration, SpO2, temperature, notes), and counted the number of data points entered for each hospital day. We conducted a descriptive analysis of documentation counts per patient per hospital stay days for each documentation type. We performed a one-way analysis of variance (ANOVA) to test for significant differences in the mean counts of each documentation type per patient between the first 10 days of hospital stays. Next, we conducted ANOVA for each combination of CCI category and documentation type to examine the differences in mean counts. To test for independent and interaction effects of documentation type, length of stay, and CCI category on the mean counts of nursing documentation per patient, we performed a three-way ANOVA. All analyses were conducted separately for acute care units and ICUs.
Results
The data used for analysis in this study included 2741 patients in the acute care units and 391 patients in ICUs. For acute care units, the mean age at admission was 62.85 years (SD=17.47), and the mean CCI was 2.52 (SD=2.69). 33.6% of patients had a CCI score of 1or 2, 28.53% had CCI score of 0 (28.53%), 19.85% had CCI scores 5 or higher (19.85%), and 18.02% had CCI scores of 3 or 4 (18.02%). About half of the patients were female (50.86%), and the most common race was unknown (32.98%), followed by White (33.38%), Black or African American (20.57%), and Other (10.98%). The majority of patients were not Hispanic or Latino (63.33%). For patients in ICUs, the mean age at admission was 62.82 years (SD=17.39), mean CCI was 2.85 (SD=2.76). 37.85% of patients had CCI scores of 1 or 2, 22.76% had CCI scores 3 or 4 (22.76%), 20.46% had CCI scores 5 or higher (20.46%), 18.93% had CCI score 0 (18.93%). 52.4% were male, and the most common race was White (39.89%), followed by Unknown (35.29%), Black or African American (15.6%), other race (7.16%) and Asian (2.04%). 64.45% were not Hispanic or Latino.
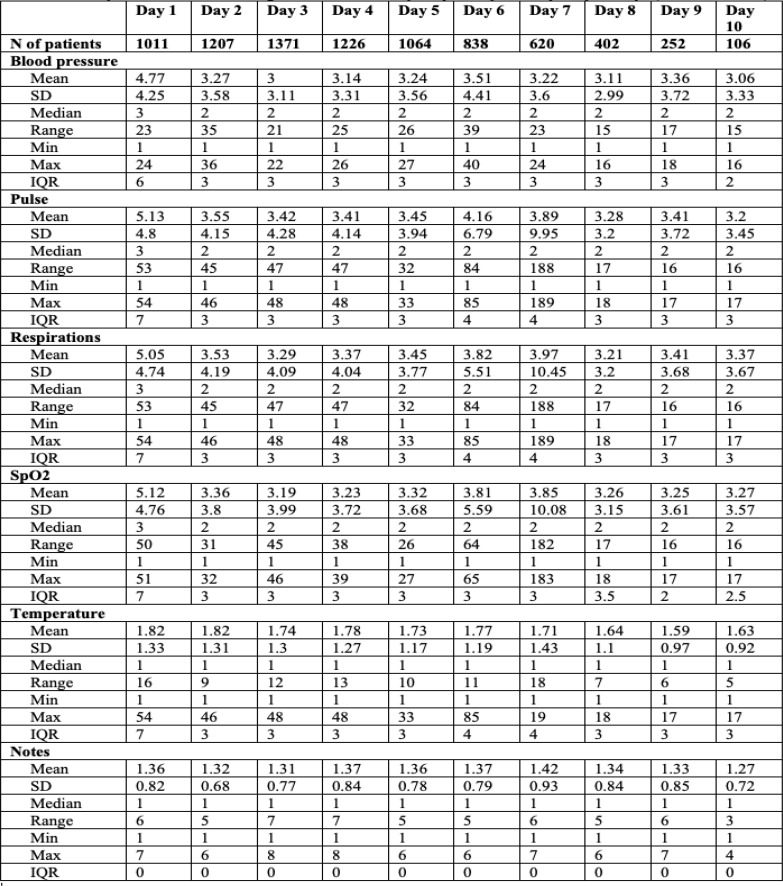
Table 1 shows the descriptive statistics of mean counts of documentation per patient by each hospital day for the first 10 days in acute care units. The average frequency of blood pressure, pulse, respiration, and SpO2 documentation decreased over time, while the frequency of note documentation increased slightly. The range of documentation frequency for all assessment types was quite wide, with some patients having very few assessments documented and others having many. The interquartile range of documentation frequencies was relatively consistent across assessment types, ranging from 2-4 for most types.
Table 1.
Descriptive statistics of nursing documentation frequency for a patient by hospital days (acute care units).
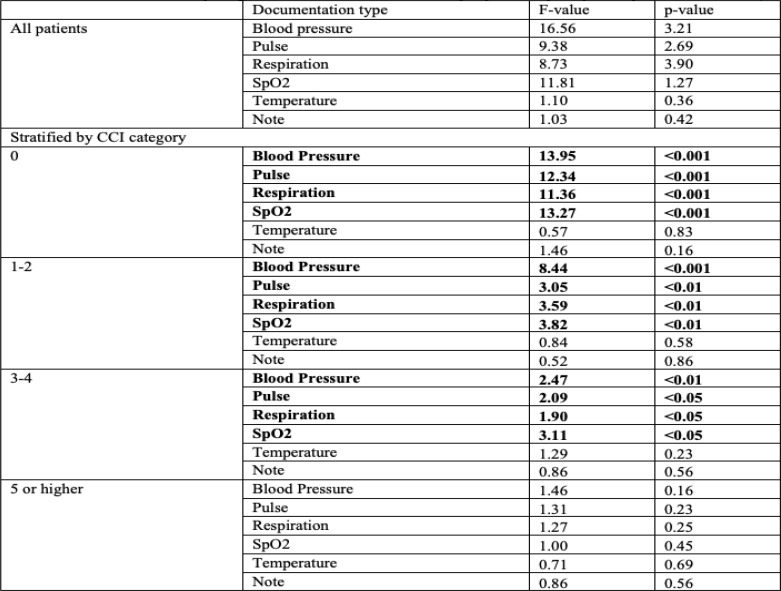
Table 2 presents the results of a one-way ANOVA for acute care patients comparing the mean counts of documentation per patient per hospital day stratified by CCI categories, in acute care units. Although there were no statistically significant differences in the mean counts of documentation by hospital days when analyzed with all patients, there were statistically significant differences between hospital days for when the analysis was conducted stratified by CCI categories. The mean counts of blood pressure, pulse, respiration, and SpO2 documentation types were significantly different between hospital days across all CCI categories except for CCI scores 5 or higher.
Table 2.
ANOVA results comparing mean counts of documentation per patient by hospital days (acute care units).
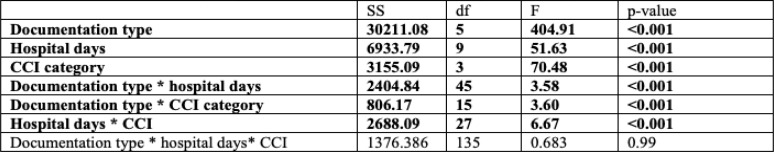
Table 3 presents the results of the ANOVA analysis that compared mean counts of documentation per patient by hospital days in acute care units. The analysis included documentation type, hospital days, and CCI category as independent variables. The main effects of documentation type, hospital days, and CCI category were all significant indicating that there is significant variability in documentation frequency by the types of documentation, hospital stay days, and CCI categories. The results also showed significant interaction effects between documentation type and hospital days and between documentation type and CCI category. These findings suggest that the relationship between documentation type and mean documentation frequency varied depending on the hospital days and the patients’ level of comorbidity. There was also a significant interaction effect between hospital days and CCI category, indicating that the effect of hospital days on mean counts of documentation per patient depended on the patient’s level of comorbidity.
Table 3.
ANOVA results comparing mean counts of documentation per patient by hospital days (acute care units).
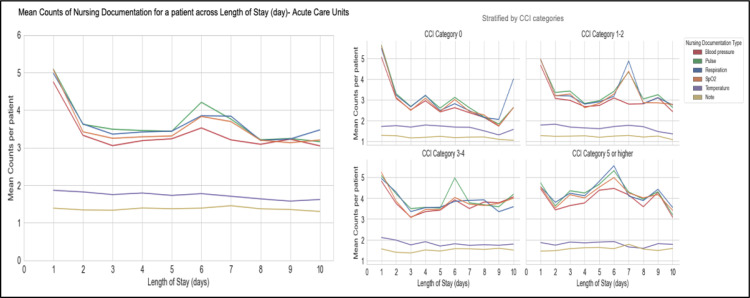
Figure 1 displays the mean counts of nursing documentation for a patient across the length of stay in the acute care units. Overall, there were similar trends across documentation types, with blood pressure, pulse, respiration, and SpO2 following similar patterns, while not many variabilities are evident for temperature and note documentation. Notably, the frequency of temperature documentation was lower compared to other vital signs. Additionally, the frequency of note documentation was low across days and CCI categories. The highest overall frequencies of documentation were observed on Day 1, which slowly decreased over time with some peaks at day 6-8 for most documentation types. However, the patterns differed for patients with different comorbidity levels. For patients with greater comorbidities, there were greater variability across hospital days. In contrast, for patients with lower comorbidities (CCI=0), there is a gradual decreased in documentation frequency over time, with an increase observed at day 10.
Figure 1.
Mean Counts of Nursing Documentation for a patient across Length of Stay (day)- Acute Care Units
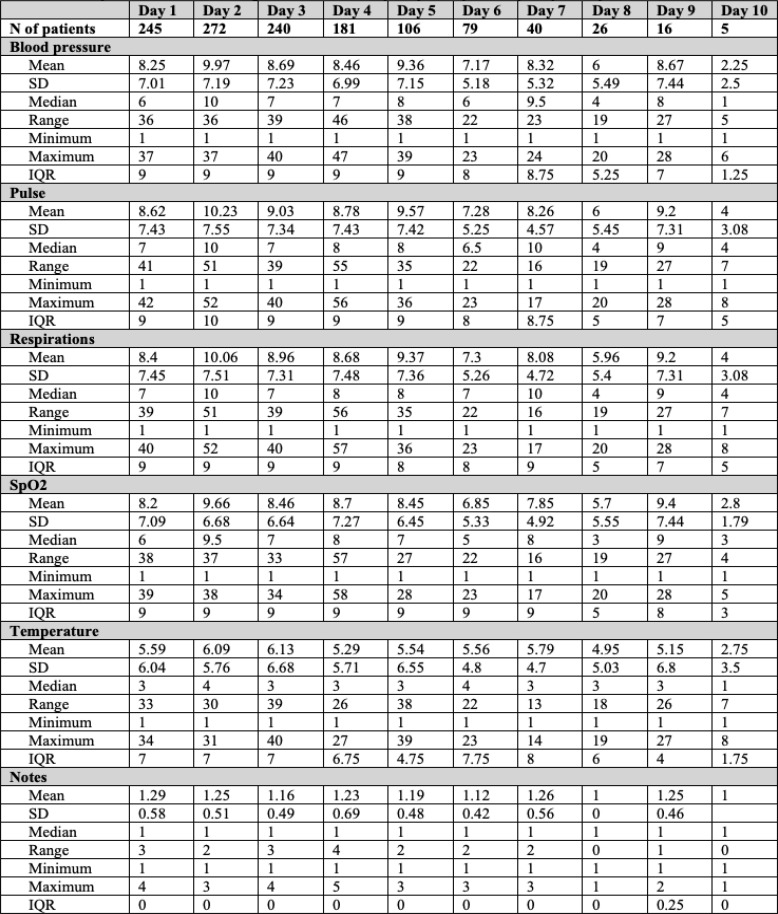
Table 4 shows the descriptive statistics of mean counts of documentation per patient by each hospital day for the first 10 days in ICUs. Similar to the results from acute care units, blood pressure, pulse, respiration, and SpO2 had higher means compared to temperature and notes. Additionally, the IQR for most documentation types was consistent and similar (between 8-10) across hospital days, except for temperature and notes.
Table 4.
Descriptive statistics of nursing documentation frequency for a patient by hospital days-ICUs
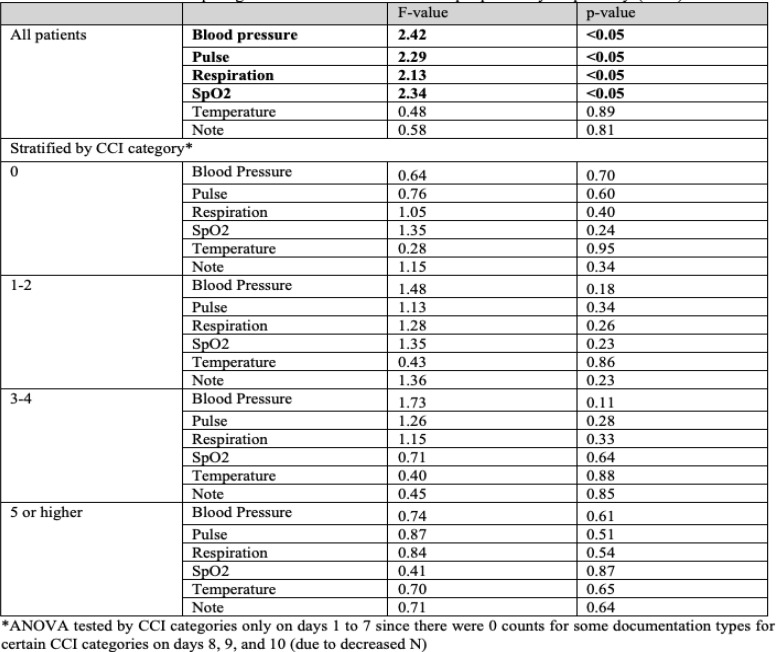
Table 5 presents the ANOVA results comparing the mean counts of documentation per patient by hospital days in the ICUs for all patients and stratified by CCI categories. The results show that for all documentation types, the F- values were relatively low, indicating lower variability between days. When mean counts of documentation per patient were compared between hospital days for all patients in ICUs, blood pressure, pulse, respiration, and SpO2 showed statistically significant differences. However, when the means were compared within each CCI category, there were no statistically significant differences between hospital days.
Table 5.
ANOVA results comparing mean counts of documentation per patient by hospital days(ICUs)
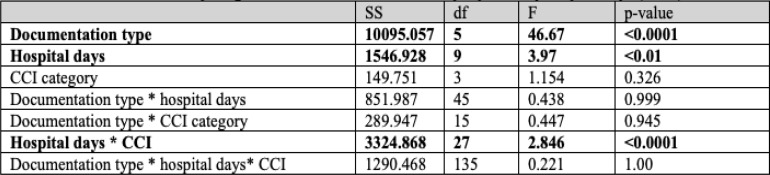
Table 6 displays the two-way ANOVA results comparing mean counts of documentation per patient by hospital days in ICUs. Significant differences in the mean counts of each documentation type and hospital days were observed, indicating that both factors play a role in the observed mean counts. However, there was no significant variability by CCI category in ICUs. Interestingly, the interaction between hospital days and CCI category was significant, suggesting that the relationship between hospital days and mean counts depends on the CCI category. In contrast, the non-significant three-way interaction suggests that the interaction between documentation type and hospital days remains consistent across different CCI categories.
Table 6.
ANOVA results comparing mean counts of documentation per patient by hospital days(ICUs)
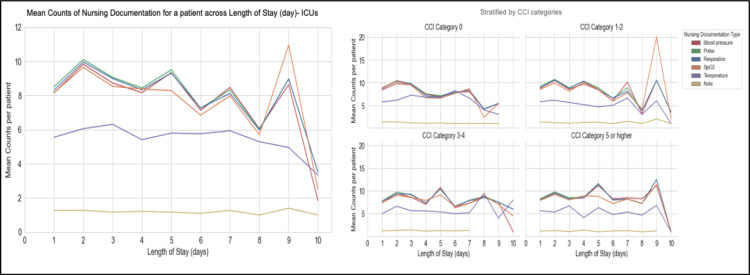
Figure 2 displays the mean counts of nursing documentation for a patient across the length of stay in the ICUs. The frequency of documentation was consistently high in the ICU setting, with some drops observed at around day 8 and on. This drop may be related to the significant drop in the number of patients included in the analysis at day 7, 8, 9, and 10. The highest frequency of documentation was observed on day 1 and 2, with peaks at day 7 for patients in CCI category 1-2. Blood pressure, pulse, respiration, and SpO2 followed similar patterns for the first 6 days for patients in all CCI categories.
Figure 2.
Mean Counts of Nursing Documentation for a patient across Length of Stay (day)- ICUs
Discussion and Conclusions
In this study, we investigated nursing documentation patterns in both acute care and ICU settings with a focus on vital signs and note documentation. Our first aim was to describe the nursing documentation patterns across patients’ hospital stays. In acute care units, nursing documentation frequency was the highest in the first few days and gradually decreased over time. The increased frequency of vital sign documentation on day 1 may indicate the need for baseline assessments or the instability of patient states or conditions. The spike in vital sign documentation on days 6-7 across all CCI categories, with some vital signs being documented more frequently than others, may also reflect a change in the patient’s condition. The ranges of documentation frequency for all assessment types were quite wide, which may suggest variability in how nurses prioritize and document assessments across patients. In contrast, we found lower variability in documentation across hospital days in ICUs suggesting that nurses in ICUs documented at more similar rates across patients’ hospital stays than in acute care units. In ICUs, there were also less variability in the first few days with some spikes in the frequency around day 8 and on. This may indicate that those patients who stay in the ICUs longer may have deteriorating conditions requiring nurses to increase their surveillance and document more frequently. Lower variability in ICUs may also be explained by the differences in baseline documentation frequency between acute and critical care settings. In the ICUs, nurses are typically required to document patient information every hour, as opposed to every 4-6 hours in the acute care settings. Our studies have demonstrated that nurses tend to increase their surveillance frequency in response to changes in patient states7. This suggests that for the sickest patients in the ICU, the hourly documentation requirement may already be high enough, so that nurses do not need to further increase their surveillance frequency. On the other hand, in the acute care setting, there may be a wider range of patient surveillance needs and a lower baseline for surveillance frequency. Finally, we found that, in both acute and ICU settings, blood pressure, respirations, pulse, and SpO2 were most frequently documented, while temperature was least frequently documented, consistent with a previous study.13 Temperature may be less frequently monitored because it requires a more intrusive method requiring more hands-on interaction with patients, particularly in the acute care setting, compared to parameters like blood pressure, pulse, and SpO2, which can be monitored continuously using devices. In the ICUs, temperature probes may be included on some continuous monitoring devices for some patient conditions, but this is not the case in acute care settings. This is an important area for further exploration, particularly given the importance of temperature assessments for sepsis risk assessment and identification. The frequency of note documentation was also very low but consistent across hospital days. The infrequent documentation of clinical notes may also reflect the current documentation practices and expectations of the healthcare system. Nurses may feel pressured to focus more on objective data, like vital signs, instead of subjective observations to make sure they are meeting documentation requirements and reducing legal risks. In addition, nurses may not have sufficient time to complete note documentation, as they may be preoccupied with the documentation they are required to complete, as well as non- EHR patient care activities.
The second aim of this study was to investigate if there is significant variability in nursing documentation frequency across patients’ hospital stays and by the types of documentation. In acute care units, we found significant variability in documentation frequency by documentation type and hospital days. Additionally, there was a significant interaction effect between documentation type and hospital days, indicating that the effects of documentation type on documentation frequency may change depending on the number of hospital days. For example, some documentation types may be more critical in the early days of hospitalization, while others may become more important later on. This finding highlights the importance of considering the duration of hospitalization when designing documentation protocols and analyzing nurse documentation patterns. In the ICUs, we also found significant variability in documentation frequency by documentation type and hospital days. In contrast to the acute care units, there was no significant interaction between documentation type and hospital days in the ICUs, suggesting that the variations of how each documentation types were entered did not significantly vary on different hospital stay days meaning that documentation patterns were more consistent across patients’ hospital stays. While nursing orders often group vital signs together, our findings suggest that nurses selectively document some vital signs more frequently than others.
The third aim of this study was to investigate how nursing documentation patterns across patients’ hospital stays differ by patients’ comorbidities as measured by CCI. In acute care units, there were significant differences in nursing documentation patterns across hospital stays in acute care units by patients’ CCI categories. The results show that patients with lower comorbidities (CCI category 0) had the greatest variability in the frequency of documentation between hospital days for all types of documentation. However, as comorbidity scores increased, the variability decreased. Specifically, for CCI category 0, 1-2, and 3-4, all documentation types except for temperature and note showed significant differences in mean counts per patient by hospital days. For CCI category 5 or higher, none of the differences in means by documentation types were significant. These findings suggest that patients with higher comorbidity scores may require more consistent monitoring across hospital days. In addition, there was a smaller level of variability in the frequency of temperature and note documentation across all CCI categories, suggesting that these types of documentation may not require the same frequency of monitoring as other vital signs and may be more appropriate for intermittent or periodic documentation. Moreover, this result may suggest that temperature and notes documentation may follow similar patterns of nursing surveillance regardless of patient state while the surveillance patterns for other types of vital signs may depend on patient state. Interestingly, in the ICU setting, CCI categories alone did not significantly impact nursing documentation patterns. However, there was a significant interaction between hospital days and CCI categories. It is interesting that the mean counts of documentation did not have statistically significant differences between patients’ CCI categories in the ICUs, but there were significant differences by CCI categories in acute care units. This finding may reflect greater variability in patient acuity and conditions in acute care units and that nurses change their documentation practice in response. In contrast, the hourly documentation standard in the ICUs may be already at a high level of nursing surveillance that there is not as much opportunity for variability in documentation frequency. The significant interaction between hospital days and CCI category in both acute care units and ICUs suggests that the relationship between hospital days and mean counts of nursing documentation varies depending on the patients’ comorbidities. This finding highlights the importance of considering patients’ comorbidities, or patient conditions in general, when designing nursing documentation protocols and analyzing nursing documentation patterns. It also suggests that nurses tailor their documentation practices to meet the needs and complexity of their patients’ conditions. Overall, our findings indicate that nursing documentation practices are adaptive and responsive to patients’ needs and conditions, and that understanding the relationship between comorbidities and nursing documentation patterns can inform efforts to redesign and optimize our EHR to reduce documentation burden.
Although this study provides important insights into nursing documentation patterns in acute care and ICU settings, several limitations should be noted. First, this study analyzed data from our CONCERN study units, which may limit the generalizability of the findings to other units and hospitals. Additionally, the study did not consider factors like workload, nursing experience, and EHR usability, all of which could significantly influence nurses’ documentation patterns. Future studies should consider accounting for these factors. It is also important to note that we did not conduct post-hoc analysis to further examine specific differences between groups, as this was not the primary focus of our study. Moreover, our analysis included patients with daytime discharges and transfers, which may have lowered average documentation frequency.
In conclusion, our results suggest that nursing documentation patterns vary significantly across hospital stays, by documentation type, and by patients’ comorbidities. These variations may reflect the changing needs and conditions of patients as well as the decision-making processes of nurses. Our findings suggest that nurses adapt their documentation practices based on patients’ conditions and comorbidities, highlighting the importance of individualized care and tailored documentation practices. These patterns of documentation can also be leveraged to inform the development of more precise and effective models for patient risk prediction as our team has done7.
Finally, based on these findings and our prior work, as EHRs are being redesigned and re-visioned to decrease documentation burden, we see an opportunity to capture and use nursing surveillance decision-making data to evaluate quality and safety rather than relying on “one size fits all” documentation requirements for patients in the hospital setting.
Acknowledgments
This work was supported by the National Institute for Nursing Research (NINR) CONCERN Study #1R01NR016941-01. JW is a postdoctoral research fellow supported by the Reducing Health Disparities through Informatics training grant (T32NR007969).
Figures & Tables
References
- 1.Collins S, Couture B, Kang MJ, Dykes P, Schnock K, Knaplund C, et al. Quantifying and visualizing nursing flowsheet documentation burden in acute and critical care. AMIA Annu Symp Proc. 2018 Dec 5;2018:348–57. [PMC free article] [PubMed] [Google Scholar]
- 2.Kang M-J, Rossetti SC, Knaplund C, Chang FY, Schnock KO, Whalen K, et al. Nursing documentation variation across different medical facilities within an integrated healthcare system. Comput Inform Nurs. 2021 May 3;39(12):845–50. doi: 10.1097/CIN.0000000000000736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stevenson JE, Israelsson J, Petersson G, Bath PA. Factors influencing the quality of vital sign data in electronic health records: A qualitative study. J Clin Nurs. 2018 Mar;27(5-6):1276–86. doi: 10.1111/jocn.14174. [DOI] [PubMed] [Google Scholar]
- 4.Collins SA, Vawdrey DK. “Reading between the lines” of flow sheet data: nurses’ optional documentation associated with cardiac arrest outcomes. Appl Nurs Res. 2012 Nov;25(4):251–7. doi: 10.1016/j.apnr.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collins SA, Cato K, Albers D, Scott K, Stetson PD, Bakken S, et al. Relationship between nursing documentation and patients’ mortality. Am J Crit Care. 2013 Jul;22(4):306–13. doi: 10.4037/ajcc2013426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schnock KO, Kang M-J, Rossetti SC, Garcia J, Lowenthal G, Knaplund C, et al. Identifying nursing documentation patterns associated with patient deterioration and recovery from deterioration in critical and acute care settings. Int J Med Inform. 2021 Sep;153:104525. doi: 10.1016/j.ijmedinf.2021.104525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rossetti SC, Knaplund C, Albers D, Dykes PC, Kang MJ, Korach TZ, et al. Healthcare Process Modeling to Phenotype Clinician Behaviors for Exploiting the Signal Gain of Clinical Expertise (HPM-ExpertSignals): Development and evaluation of a conceptual framework. J Am Med Inform Assoc. 2021 Jun 12;28(6):1242–51. doi: 10.1093/jamia/ocab006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rossetti SC, Dykes PC, Knaplund C, Kang M-J, Schnock K, Garcia JP, et al. The communicating narrative concerns entered by registered nurses (CONCERN) clinical decision support early warning system: protocol for a cluster randomized pragmatic clinical trial. JMIR Res Protoc. 2021 Dec 10;10(12):e30238. doi: 10.2196/30238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Office of Burden Reduction & Health Informatics | CMS [Internet]. [cited 2023 Mar 21] Available from: https://www.cms.gov/about-cms/obrhi.
- 10.National Academies of Sciences, Engineering, and Medicine, National Academy of Medicine, Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being. Taking action against clinician burnout: A systems approach to professional well-being. Washington (DC): National Academies Press (US); 2019. [PubMed] [Google Scholar]
- 11.New Surgeon General Advisory Sounds Alarm on Health Worker Burnout and Resignation | HHS.gov [Internet]. [cited 2023 Mar 21] Available from: https://www.hhs.gov/about/news/2022/05/23/new-surgeon-general-advisory-sounds-alarm-on-health-worker-burnout-and-resignation.html.
- 12.Beyrer J, Manjelievskaia J, Bonafede M, Lenhart G, Nolot S, Haldane D, et al. Validation of an International Classification of Disease, 10th revision coding adaptation for the Charlson Comorbidity Index in United States healthcare claims data. Pharmacoepidemiol Drug Saf. 2021 May;30(5):582–93. doi: 10.1002/pds.5204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Considine J, Trotter C, Currey J. Nurses’ documentation of physiological observations in three acute care settings. J Clin Nurs. 2016 Jan;25(1-2):134–43. doi: 10.1111/jocn.13010. [DOI] [PubMed] [Google Scholar]