Abstract
Background:
Open carpal tunnel release (OCTR) and endoscopic carpal tunnel release (ECTR) are the 2 operative approaches used to treat carpal tunnel syndrome (CTS). This study aims to identify whether differences between OCTR and ECTR rates exist, and, if so, are these differences associated with patient demographics or hospital characteristics.
Methods:
The 2018 Nationwide Ambulatory Surgery Sample (NASS) was filtered for patient encounters including either OCTR or ECTR operations. All patients undergoing either OCTR or ECTR were included, regardless of surgical specialty. Patient demographics and hospital characteristics data, provided and predefined by the NASS database, were collected and compared between the 2 treatment groups.
Results:
A total of 180 740 patient encounters were collected for both procedure types (OCTR: 62.4% women, mean age, 58 years; ECTR: 62.2% women, mean age, 58 years). Patients from lower income zip codes were more likely to undergo OCTR (P < .001). Patients either self-paying (P < .008) or covered by Medicare (P < .001) or Medicaid insurance (P < .001) were also more likely to undergo OCTR. In contrast, patients who received care at academic centers and centers with >300 beds were more likely to undergo ECTR (P < .001). Patients <65 years old were more likely to undergo ECTR (P < .001), and patients > 75 years old were more likely to undergo OCTR (P < .001). In addition, ECTR was found to be more expensive, with average total charges $1568 greater than charges for OCTR (P < .001).
Conclusions:
Significant differences exist in treatment strategies for CTS and are related to patient income, location, and primary payor status. Differences in OCTR and ECTR rates are also present, and are related to the size and academic status of hospitals.
Keywords: carpal tunnel syndrome, nerve, diagnosis, hand, anatomy, cost utilization, practice patterns, primary payor status
Introduction
Carpal tunnel syndrome (CTS) is the most common compressive neuropathy with a prevalence of 30 to 50 cases per 1000 patients per year.1,2 In the Medicare population alone, surgical treatment of CTS with carpal tunnel release (CTR) provides up to $1.6 billion in economic benefit annually. 3 The 2 techniques used for CTR are open carpal tunnel release (OCTR) and endoscopic carpal tunnel release (ECTR). These techniques have been compared extensively in the literature, with comparable results in treating compressive symptoms and functional improvement.4-6
Open CTR is associated with superior visualization of the transverse carpal ligament, which allows for certain complete ligament transection. 7 However, OCTR is linked to increased incision site pain, incision site infection and dehiscence, increased scar burden, and lower patient satisfaction.7-9 In contrast, ECTR offers a smaller incision that is associated with faster recovery times, decreased incision site–related morbidity, decreased pain, and decreased scar burden.5,10 The downsides of ECTR are most notably increased cost, risk for incomplete transection of the transverse carpal ligament, and transient median nerve injury.5,10,11 No strong evidence supports the superiority of one technique over the other.
Patient demographics have been shown to influence procedure rates across many surgical specialties. It is well known that Medicare- and Medicaid-based payors have decreased reimbursement rates for physicians when compared with private payors.12,13 One study identified significant disparities among Medicare and Medicaid compensation for common plastic surgery procedures within the United States. The authors postulated that these differences likely play a role in the surgeons’ decreased ability or willingness to provide care to these underserved populations. 12 Based on the high prevalence of CTS, our study aims to determine whether national trends or differences exist in the surgical management of CTS with respect to patient and hospital demographics.
Materials and Methods
Data were retrieved from the 2018 Health Care Utilization Project (HCUP) Nationwide Ambulatory Surgery Sample (NASS). The NASS is a database with a collection of more than 7 million ambulatory surgery encounters from 2699 hospital-owned facilities. 14 It contains information regarding encounter Current Procedural Terminology (CPT) codes and International Classification of Diseases, Tenth Revision (ICD-10) codes as well as predefined patient demographics and hospital categorical variables. The 2018 NASS database encompasses an estimated 72% of ambulatory surgery encounters in the United States. 14 The database was filtered for encounters in which the primary procedure was OCTR (CPT 64721) or ECTR (CPT 29848). No exclusions were made based on surgical specialty or training as this was not reported in the database. All surgeries performed by both fellowship-trained or non-fellowship-trained surgeons, regardless of plastic or orthopedic surgical training, were included if CPT criteria was met.
To evaluate demographic differences between patients who underwent OCTR and those who underwent ECTR, the following variables were collected: patient age, sex, patient residential location (large central metropolitan, large fringe metropolitan, medium metropolitan, micropolitan, not metropolitan or micropolitan), national median household income quartile for patient ZIP code, hospital location (rural, urban) according to National Center for Health Statistics (NCHS) urban-rural code, hospital teaching status (nonteaching, teaching), hospital US geographic region (Northeast, Midwest, South, West), hospital bed count (0-99, 100-299, 300+), expected primary payor (Medicare, Medicaid, private including HMO, self-pay, no charge, or other), and total charges for the encounter. The national median household income quartiles by zipcode were <$42 999 (first), $43 000 to $53 999 (second), $54 000 to $70 999 (third), and >$71 000 (fourth). These values are derived from ZIP code–demographic data obtained from Clarita.
Continuous variables (age, total charges) were reported as means with standard deviations, while categorical variables were reported as percentages and frequencies. Comparisons of proportions for each variable with respect to procedure type (OCTR vs ECTR) were done using chi-square tests with Bonferroni corrections. Differences in total charges based on patient demographics and hospital characteristics were assessed using 2-sided t tests, assuming equal variances with Bonferroni correction to protect from type 1 error. Multivariate logistic regression was then performed to elucidate the significant factors independently associated with the procedure type chosen. Data processing and statistical analysis were conducted using IBM SPSS Statistics software (version 25). Results were deemed statistically significant when P < .05.
Results
Querying of the 2018 NASS database resulted in 180 740 encounters for outpatient CTR. Open CTR consisted of 145 407 (80%) encounters, while the remaining 35 333 (20%) encounters were for ECTR. The mean age for all patients was 58.1 years (SD = 15.0). A more detailed breakdown of age categories can be found in Table 1.
Table 1.
Patient Demographics (%) for Each Carpal Tunnel Release Surgical Technique.
| Patient Demographics | n | % | |
|---|---|---|---|
| Total encounters | 180 740 | 100 | |
| OCTR | 145 407 | 80 | |
| ECTR | 35 333 | 20 | |
| Proportion of patients (%) | |||
| ECTR | OCTR | ||
| Sex | |||
| Male | 37.8 | 37.6 | |
| Female | 62.2 | 62.4 | |
| Age categories, y | |||
| <45 | 20.1* | 19.4 | |
| 45-54 | 21.6* | 21.1 | |
| 55-64 | 25.2* | 24.4 | |
| 65-74 | 19.2 | 19.3 | |
| ≥75 | 13.9 | 15.8* | |
| Median household income national quartile for patient ZIP code | |||
| ≤$42 999 | 21.5 | 26.0* | |
| $43 000-$53 999 | 28.7 | 33.2* | |
| $54 000-$70 999 | 27.8* | 25.4 | |
| ≥$71 000 | 22.0* | 15.4 | |
| Patient location: NCHS urban-rural code | |||
| Large central metro | 20.2* | 17.5 | |
| Large fringe metro | 26.7* | 20.7 | |
| Medium metro | 18.9 | 21.2* | |
| Small metro | 11.4 | 12.1* | |
| Micropolitan | 14.1 | 16.5* | |
| Other | 8.7 | 12.0* | |
| Primary expected payor (uniform) | |||
| Medicare | 34.2 | 37.1* | |
| Medicaid | 13.1 | 15.1* | |
| Private | 46.0* | 41.5 | |
| Self-pay | 0.9 | 1.0 | |
| No charge | 0.1 | 0.1 | |
| Other | 5.7* | 5.3 | |
| Hospital academic status | |||
| Nonacademic | 36.2 | 38.5* | |
| Academic | 63.8* | 61.5 | |
| Hospital bed count | |||
| 0-99 | 14.8 | 20.6* | |
| 100-299 | 36.5 | 38.2* | |
| 300+ | 48.7* | 41.2 | |
Note. ECTR = endoscopic carpal tunnel release, OCTR = open carpal tunnel release. NCHS = National Center for Health Statistics.
Results are based on 2-sided tests with Bonferroni correction. For each significant pair, the category with the larger column proportion is indicated with an asterisk (*), P < .001.
Bivariate Analysis
Patients <65 years old were more likely to undergo ECTR (P < .001), and patients >75 years old were more likely to undergo OCTR (P < .001). The proportion of female patients was similar between treatment groups at 62.2% for ECTR and 62.4% for OCTR (Table 1).
Analysis of patients based on median income revealed that those in the first or second income quartile zip codes (<$42 999 and $43 000-$53 999, respectively) are more likely to undergo OCTR (first quartile: 26% vs 21.5%, P < .001; second quartile: 33.2% vs 28.7%, P < .001) for the treatment of CTS (Table 1, Figure 1). Conversely, patients in higher income zip codes were more likely to receive ECTR (third quartile: 27.8% vs 25.4%, P < .001; fourth quartile: 22.0% vs 15.4%, P < .001).
Figure 1.

OCTR and ECTR proportion of patients (%) for each procedure type based on median household income quartile.
Note. OCTR = open carpal tunnel release; ECTR = endoscopic carpal tunnel release.
Analysis of patient location also revealed differences in the CTR technique performed. Patients from large metropolitan areas (population > 1 million, NCHS urban-rural codes 1 and 2) were more likely to undergo ECTR (0.2% vs 17.5%; 26.7% vs 20.7%, P < .001; Table 1, Figure 2). All other patient location subgroups were more likely to receive OCTR (P < .001).
Figure 2.
OCTR and ECTR proportion of patients (%) for each procedure type based on patient geographic location (NCHS urban-rural code).
Note. OCTR = open carpal tunnel release; ECTR = endoscopic carpal tunnel release; NCHS = National Center for Health Statistics.
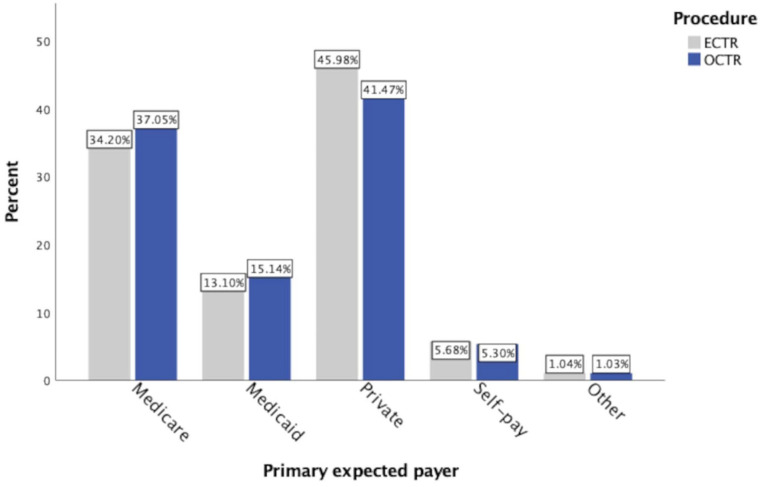
Patients were further grouped according to their expected primary payor. Patients whose primary payor was either Medicare or Medicaid were more likely to undergo OCTR (Medicare 37.1% vs 34.2%, P < .001; Medicaid 15.1% vs 13.1%, P < .001; Table 1, Figure 3). Conversely, patients with private payors, including HMOs, were more likely to receive ECTR (46.0% vs 41.5%, P < .001).
Figure 3.
OCTR and ECTR proportion of patients (%) for each procedure type based on expected primary payor.
Note. OCTR = open carpal tunnel release; ECTR = endoscopic carpal tunnel release.
Hospital surgery centers were then stratified by: (1) teaching status; and (2) hospital bed count. Patients who underwent CTR at academic hospitals were more likely to receive ECTR (64% vs 62%, P < .001). Furthermore, patients who underwent CTR at hospitals with 300+ beds were also more likely to receive ECTR (48.7% vs 41.2%, P < .001; Table 1).
The mean total charges was $9396.68 (SD = $7278.02). The average total charges for ECTR and OCTR were $10 656 (SD = $7602) and $9088 (SD = $7163), respectively (P < .001). Differences in total charges per encounter were analyzed based on patient income status, expected primary payor, and hospital teaching status. For both the ECTR and OCTR subgroups, average total charges were highest for patients with an income status in the first quartile (<$42 999, P < .001). Medicare ($10 938) and private payor ($10 724) patients both had higher total charges for ECTR when compared with Medicaid ($9818) patients (P < .001). Academic centers had higher total charges for both ECTR and OCTR when compared with nonacademic centers, and the mean differences were $333 and $728, respectively (P < .001; Table 2).
Table 2.
Total Charges for Carpal Tunnel Release Stratified by Surgical Technique, Patient Demographics, and Hospital Characteristics.
| Total charges (mean, $) | ||
|---|---|---|
| Patient Demographics | ECTR | OCTR |
| Sex | ||
| Male | 10 605* | 9084 |
| Female | 10 688* | 9091 |
| Age categories, y | ||
| <45 | 10 332* | 9157 |
| 45-54 | 10 766* | 9169 |
| 55-64 | 10 588* | 9159 |
| 65-74 | 10 943* | 9204 |
| ≥75 | 10 683* | 8647 |
| Median household income national quartile for patient ZIP code | ||
| ≤$42 999 | 11 390* | 9669 |
| $43 000-$53 999 | 10 259* | 8575 |
| $54 000-$70 999 | 10 579* | 8877 |
| ≥$71 000 | 10 480* | 9574 |
| Patient location: NCHS urban-rural code | ||
| Large central metro | 11 681* | 10 886 |
| Large fringe metro | 10 259* | 9564 |
| Medium metro | 12 201* | 9729 |
| Small metro | 10 590* | 8477 |
| Micropolitan | 9272* | 7850 |
| Other | 8864* | 7457 |
| Primary expected payor (uniform) | ||
| Medicare | 10 938* | 9089 |
| Medicaid | 9818* | 9227 |
| Private | 10 724* | 8972 |
| Self-pay | 11 780 | 10 145 |
| No charge | 8675 | 9661 |
| Other | 10 174* | 9451 |
| Hospital academic status | ||
| Nonacademic | 10 446* | 8645 |
| Academic | 10 779* | 9373 |
| Hospital bed count | ||
| 0-99 | 8854* | 7353 |
| 100-299 | 11 210* | 9336 |
| 300+ | 10 813* | 9782 |
Note. ECTR = endoscopic carpal tunnel release, OCTR = open carpal tunnel release, NCHS = National Center for Health Statistics.
Results are based on 2-sided tests with Bonferroni correction. For each significant pair, the category with the larger column proportion is indicated with an asterisk (*), P < .001.
Multivariate Analysis
On multivariate analysis, several factors were significantly associated with increased odds of undergoing OCTR, lower patient household median income quartile by zip code, patients with self-pay or using Medicare and Medicaid, and smaller hospital bed size. Patient’s were more likely to undergo OCTR if they fell within the first 3 national quartiles for median household income by zipcode by 57% for Q1 (P < .001), 42% for Q2 (P < .001), and 13% for Q3 (P < .001). In terms of primary expected payor, patients using Medicaid were 20% more likely (P < .001), those with self-pay status also were 20% more likely (P < .008), and those using Medicare were 9% more likely (P < .001) to be treated with the open technique. Private insurance (including HMO plans) was not a statistically significant factor (P = .673). Age was a statistically significant predictor (P < .001); however, it increased odds of open CTR treatment by only 0.4%. Patients treated in hospitals with 0 to 99 beds had 58% increased odds of OCTR treatment (P < .001), while those treated in hospitals with 100 to 299 beds had 24% increased odds of OCTR treatment (P < .001).
Conversely, several significant factors were associated with decreased odds of receiving OCTR. Patients residing in large central metropolitan (P < .001), large fringe metropolitan (P < .001), small metropolitan (P < .001), and micropolitan (P < .002) areas were associated with decreased odds of treatment with the open technique by 21%, 20%, 13%, and 8%, respectively. Geographically, the Northeast and the South were the only 2 regions that were statistically significant (both P < .001), and treatment in these locations were both associated with 31% decreased odds of receiving OCTR. Hospitals in an urban location were associated with 28% decreased odds of receiving the open technique (P > .001).
Discussion
In this analysis of the 2018 NASS, one of the largest, most recent databases for national ambulatory surgery rates, we revealed stark differences in the surgical management of CTS. Patients with Medicare/Medicaid insurance coverage, in the lowest income quartile (<$42 999), and located in rural areas are more likely to undergo OCTR. Conversely, patients in the highest income quartile (>$71 000) undergo ECTR at a rate 42.8% higher than OCTR. Furthermore, patients with private payor insurance are 10.8% more likely to receive ECTR than OCTR. Age was also correlated with differences in the CTR technique performed. Patients <65 years old are more likely to undergo ECTR, although the effect size is quite small (0.5%-0.8% increase). On multivariate analysis, age was a statistically significant predictor for OCTR; however, it increased odds of OCTR treatment by only 0.4%. Prior studies have similarly shown a lower average age for ECTR versus OCTR, 14 therefore supporting the similarity between our dataset and study populations reported in the literature.
The literature comparing ECTR with OCTR is dense and variable. Previous large database studies have shown that surgical site infection, wound dehiscence, and scar formation are all higher with OCTR when compared with ECTR.7-9,15 On the contrary, ECTR is associated with decreased postoperative pain and increased patient satisfaction, but has increased risk of transient nerve injuries and incomplete transection of the transverse carpal ligament.5,10,11 However, no major difference in operative duration is observed between ECTR and OCTR (mean difference 5.81 minutes). 16 Therefore, there is no clear evidence that either technique is superior.
Despite no clinical superiority between techniques, the higher costs associated with ECTR attract attention in the literature.15,16 A study by Zhang et al 17 using PearlDiver data from 2007 to 2014 identified that ECTR results in significantly higher physician fees ($555 vs $428). In our study, total charges for ECTR were 17% higher than OCTR ($10 656 vs $9088). Although the NASS database used in our study provides total charges as the only financial metric, we speculate the increased total charges associated with ECTR highlight the disadvantages of instrument start-up and maintenance costs associated with endoscopic techniques. However, this is counterbalanced by greater reimbursements when compared with OCTR. In the Medicare population specifically, total reimbursement for ECTR is greater than OCTR ($1643 vs $1312). 18 In the Medicaid population, reimbursement adjustments for ECTR and OCTR are similar at 77.7% and 78.2% of Medicare rates, respectively. 19 Thus, it appears reimbursement for ECTR remains greater than OCTR for Medicare/Medicaid populations, and these reimbursement rates are known to be much lower than those of private payors.13,15
Patient demographics and hospital characteristics associated with the 2 surgical techniques further elucidate the economic implications. Endoscopic carpal tunnel release is performed on higher income and privately insured patients, while OCTR is performed in lower income and Medicare/Medicaid-insured patients. However, this difference does not necessarily represent a difference in the quality of care. Both techniques are accepted as standard of care and no clear clinical advantage has been identified. The difference in patient selection for each technique may be economically motivated to receive greater reimbursements from patients perceived as able to sustain higher costs. This brings up an interesting question of cost-minimization in wealthier populations. The disproportionate use of a more expensive surgical technique when a cheaper alternative exists may have larger economic consequences. The burden of this practice on the economic system is unknown and should be further quantified. In other surgical specialties, the expense of minimally invasive techniques is offset by the decreased length of stays. 20 In this case, no clear financial trade-off exists. Some claim an earlier return to work is a cost-effective impact on society. 21 This is potentially concerning given the findings of this study, as this economic advantage would more likely benefit higher income individuals, thus furthering the socioeconomic gap.
Our data also revealed a preference for ECTR in academic centers, and more densely populated areas. Although the NASS database does not provide data on the fellowship-training status on the surgeons performing CTR procedures, we speculate that trends in surgical training may explain this difference. Hand fellowship–trained surgeons perform 4.5 times more ECTRs than non-fellowship-trained surgeons. 22 Academic training programs and hand surgeons are more likely located in larger cities and university hospitals. Hand surgeon density can be as much as 3 times higher in states such as Massachusetts when compared with Alabama. 23 In addition, a positive correlation exists between per capita income at the state level and density of subspecialist hand surgeons. 19
In our study, using a single year of NASS (2018) encounters, we found that the absolute difference between ECTR procedure rates in academic centers and nonacademic centers is modest (2.3%, P < .001). Although our data were limited to 1 year and thus a temporal trend could not be analyzed, previous studies analyzing CTR procedure rates reveal a 3 times increase in ECTR procedures from 2000 to 2014, while OCTR procedures have decreased since 2003. 24 These data are correlated with the greater than 20% increase in number of hand fellowship positions since 2010. 25 Although academic centers see higher proportions of Medicaid/Medicare patients, educational pressures such as teaching and meeting case requirements for trainees may exist. Other factors limiting the use of ECTR in rural areas are the start-up costs and sustainability of expensive surgical equipment. Smaller hospitals may not have the capital to invest in equipment that has not proven to be necessary to provide the standard of care. 26
Several limitations exist within our study and should be mentioned. First, large database studies such as ours are limited by an inherent risk of data entry/coding errors by the treating physicians. In addition, this database uses median income for zip codes in which the patient resides. This is a surrogate marker and can be influenced by areas with fluctuating levels of income. The NASS database has predefined groupings of all categorical; therefore, our analysis is limited to the information provided. The database also does not clarify information about the operating surgeon’s specialty. Therefore, we did not report differences related to orthopedic, plastic, and fellowship-trained hand surgeons. Furthermore, data related to charges for each procedure was only provided for “total charges” which can be influenced by many factors, including facility costs, anesthesia costs, and regional differences.
Conclusion
This study reveals that specific differences in patient demographics and hospital characteristics affect the surgical management of CTS. Medicare/Medicaid-insured patients, with low income, and located in rural populations are more likely to undergo OCTR. At first glance, it appears that surgeons tend to select the more costly alternative, ECTR, for higher income and privately insured patients. However, the NASS database only provides total charges associated with each procedure rather than actual costs and reimbursements, and thus, we are unable to confirm that opting for ECTR is reimbursement motivated and not patient requested. This may represent a financial incentive when higher reimbursements are seen as attainable based on demographic factors. Trends in academic training and costly equipment may explain the higher OCTR procedure rate in rural settings. Further quantification and characterization of the economic impact of over-using surgical resources in the treatment of CTS is warranted. More consideration for cost-minimization without compromising the quality of care is also needed, especially due to the increasing use of ECTR in wealthier populations, as demonstrated by this article.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Fernando A. Herrera  https://orcid.org/0000-0001-6957-0413
https://orcid.org/0000-0001-6957-0413
References
- 1. Foster BD, Sivasundaram L, Heckmann N, et al. Surgical approach and anesthetic modality for carpal tunnel release: a nationwide database study with health care cost implications. Hand (N Y). 2017;12(2):162-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rojo-Manaute JM, Capa-Grasa A, Chana- Rodríguez F, et al. Ultra-minimally invasive ultrasound-guided carpal tunnel release: a randomized clinical trial. J Ultrasound Med. 2016;35(6):1149-1157. [DOI] [PubMed] [Google Scholar]
- 3. Hubbard ZS, Law TY, Rosas S, et al. Economic benefit of carpal tunnel release in the Medicare patient population. Neurosurg Focus. 2018;44(5):E16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Michelotti B, Romanowsky D, Hauck RM. Prospective, randomized evaluation of endoscopic versus open carpal tunnel release in bilateral carpal tunnel syndrome: an interim analysis. Ann Plast Surg. 2014;73(Suppl. 2):S157-S160. [DOI] [PubMed] [Google Scholar]
- 5. Sayegh ET, Strauch RJ. Open versus endoscopic carpal tunnel release: a meta-analysis of randomized controlled trials. Clin Orthop Relat Res. 2015;473(3):1120-1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vasiliadis HS, Georgoulas P, Shrier I, et al. Endoscopic release for carpal tunnel syndrome. Cochrane Database Syst Rev. 2014;1:CD008265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hu K, Zhang T, Xu W. Intraindividual comparison between open and endoscopic release in bilateral carpal tunnel syndrome: a meta-analysis of randomized controlled trials. Brain Behav. 2016;6(3):439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Larsen MB, Sørensen AI, Crone KL, et al. Carpal tunnel release: a randomized comparison of three surgical methods. J Hand Surg Eur Vol. 2013;38(6):646-650. [DOI] [PubMed] [Google Scholar]
- 9. Zuo D, Zhou Z, Wang H, et al. Endoscopic versus open carpal tunnel release for idiopathic carpal tunnel syndrome: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2015;10:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen L, Duan X, Huang X, et al. Effectiveness and safety of endoscopic versus open carpal tunnel decompression. Arch Orthop Trauma Surg. 2014;134(4):585-593. [DOI] [PubMed] [Google Scholar]
- 11. Thoma A, Veltri K, Haines T, et al. A meta-analysis of randomized controlled trials comparing endoscopic and open carpal tunnel decompression. Plast Reconstr Surg. 2004;114(5):1137-1146. [DOI] [PubMed] [Google Scholar]
- 12. Kaura AS, Berlin NL, Momoh AO, et al. State variations in public payer reimbursement for common plastic surgery procedures. Plast Reconstr Surg. 2018;142(6):1653-1661. [DOI] [PubMed] [Google Scholar]
- 13. Firouzbakht PK, Shaum KM, Israel JS, et al. Medicaid for the plastic and reconstructive surgeon. Plast Reconstr Surg. 2020;145(3):637e-646e. [DOI] [PubMed] [Google Scholar]
- 14. HCUP Nationwide Ambulatory Surgery Sample (NASS). Healthcare Cost and Utilization Project (HCUP). 2016 and 2018. Rockville, MD: Agency for Healthcare Research and Quality. www.hcup-us.ahrq.gov/nassoverview.jsp [Google Scholar]
- 15. Devana SK, Jensen AR, Yamaguchi KT, et al. Trends and complications in open versus endoscopic carpal tunnel release in private payer and Medicare patient populations. Hand (N Y). 2019;14(4):455-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lorgelly PK, Dias JJ, Bradley MJ, et al. Carpal tunnel syndrome, the search for a cost-effective surgical intervention: a randomised controlled trial. Ann R Coll Surg Engl. 2005;87(1):36-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhang S, Vora M, Harris AH, et al. Cost-minimization analysis of open and endoscopic carpal tunnel release. J Bone Joint Surg Am. 2016;98(23):1970-1977. [DOI] [PubMed] [Google Scholar]
- 18. Law TY, Rosas S, Hubbard ZS, et al. Trends in open and endoscopic carpal tunnel release utilization in the Medicare patient population. J Surg Res. 2017;214:9-13. [DOI] [PubMed] [Google Scholar]
- 19. Baker W, Rivlin M, Sodha S, et al. Variability in Medicaid reimbursement in hand surgery may lead to inequality in access to patient care [published online ahead of print, 2020 Oct 27]. Hand (N Y). 2020. doi: 10.1177/1558944720964966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Janjua H, Cousin-Peterson E, Barry TM, et al. The paradox of the robotic approach to inguinal hernia repair in the inpatient setting. Am J Surg. 2020;219:497-501. [DOI] [PubMed] [Google Scholar]
- 21. Barnes JI, Paci G, Zhuang T, et al. Cost-effectiveness of open versus endoscopic carpal tunnel release. J Bone Joint Surg Am. 2021;103:343-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rios-Diaz AJ, Metcalfe D, Singh M, et al. Inequalities in specialist hand surgeon distribution across the United States. Plast Reconstr Surg. 2016;137(5):1516-1522. [DOI] [PubMed] [Google Scholar]
- 23. Smetana BS, Zhou X, Hurwitz S, et al. Effects of hand fellowship training on rates of endoscopic and open carpal tunnel release. J Hand Surg Am. 2016;41(4):e53-e58. [DOI] [PubMed] [Google Scholar]
- 24. Williamson ERC, Vasquez Montes D, Melamed E. Multistate comparison of cost, trends, and complications in open versus endoscopic carpal tunnel release. Hand (N Y). 2021;16(1):25-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ruddell JH, Eltorai AEM, DePasse JM, et al. Trends in the orthopaedic surgery subspecialty fellowship match: assessment of 2010 to 2017 applicant and program data. J Bone Joint Surg Am. 2018;100(21):e139. [DOI] [PubMed] [Google Scholar]
- 26. Zender J, Thell C. Developing a successful robotic surgery program in a rural hospital. AORN J. 2010;92(1):72-83; quiz 84. [DOI] [PubMed] [Google Scholar]