Abstract
Background
Pediatric myelodysplastic syndrome (pMDS) is a group of rare clonal neoplasms with a difficult diagnosis and risk of progression to acute myeloid leukemia (AML). The early stratification in risk groups is essential to choose the treatment and indication for allogeneic hematopoietic stem cell transplantation (HSCT). According to the Revised International Prognostic Scoring System, cytogenetic analysis has demonstrated an essential role in diagnosis and prognosis. In pMDS, abnormal karyotypes are present in 30–50% of the cases. Monosomy 7 is the most common chromosomal alteration associated with poor prognosis. However, the rarity of specific cytogenetic alterations makes its prognosis uncertain. Thus, this study aimed to describe uncommon cytogenetic alterations in a cohort of 200 pMDS patients and their association with evolution to AML.
Methods
The cytogenetic analysis was performed in 200 pMDS patients by G-banding and fluorescence in situ hybridization between 2000 to 2022.
Results
Rare chromosome alterations were observed in 7.5% (15/200) of the cases. These chromosome alterations were divided into four cytogenetic groups: hyperdiploidy, biclonal chromosomal alterations, translocations, and uncommon deletions representing 33.3%, 33.3%, 20%, and 13.3%, respectively. Most of these patients (10/15) were classified with advanced MDS (MDS-EB and MDS/AML) and the initial subtype was present in five patients (RCC). The leukemic evolution was observed in 66.66% (10/15) of the patients. Most patients had poor clinical outcomes and they were indicated for HSCT.
Conclusion
The study of uncommon cytogenetic alterations in pMDS is important to improve the prognosis and guide early indication of HSCT.
Keywords: Pediatric myelodysplastic syndrome, Uncommon chromosomal abnormalities, Leukemia evolution, Prognosis
Introduction
In recent years, significant advances in understanding myelodysplastic syndrome (MDS) pathology allowed a new classification.1 MDS is a heterogeneous group of clonal stem cell diseases with a risk of evolution to acute myeloid leukemia (AML). Pediatric MDS (pMDS) is a rare disease with a difficult diagnosis and variable clinical course, and it is biologically distinct from adult MDS.2 The Revised International Prognostic Scoring System (IPSS-R) has been used to stratify risk groups in pMDS. Thus, the cytogenetic analysis for these patients is essential since the karyotypic pattern is one of the pillars of IPSS-R.3
The incidence of cytogenetic alterations in pMDS ranges from 30 to 50%, being more frequent in advanced subtypes such as pMDS with excess blasts, MDS-EB (5–19% of blasts), and MDS/AML (20–29% of blasts). The most frequent cytogenetic alteration in pMDS is monosomy 7 (−7), which is associated with a poor prognosis, followed by trisomy 8 (+8), and trisomy 21 (+21) which have an intermediate prognosis and complex karyotypes with very poor prognosis.3,4 Rare chromosomal alterations such as del(13q), −21, +11, +13, +14, +14q, and 11q23 translocations were described in adult patients with MDS. These chromosomal alterations do not have their real prognosis determined due to the low number of cases described.5,6 So, these uncommon chromosomal alterations are classified mainly as an intermediate cytogenetic risk group according to the IPSS-R.3
The importance of refining the cytogenetic classification to determine the prognostic significance of rare chromosomal abnormalities has been pointed out in other diseases such as AML.7 Since the cytogenetic findings were the first diagnostic tool to stratify patients and their prognosis, accurate stratification is essential to choose the therapy and to indicate the hematopoietic stem cell transplantation (HSCT), which is the only curative treatment for MDS patients. 8,9 Nevertheless, to the best of our knowledge, studies focusing on the frequency of uncommon chromosomal alterations have not been previously performed in pMDS. Thus, the aim of this study was to analyze the frequency of specific uncommon chromosomal abnormalities in pMDS and their associations with the clinical features, evolution from MDS to AML, and prognostic significance.
Methods
Patients
Cytogenetic and clinical studies were performed on 200 pediatric patients with MDS between 2000 and 2022. Patients were diagnosed at Instituto Nacional de Câncer, Instituto de Puericultura e Pediatria Martagão Gesteira, and Hospital Universitário Oswaldo Cruz. Uncommon chromosome alterations were present in 15 patients. These patients were distributed according to sex as nine females and six males. The mean age among these patients was five years old (ranging from 1 to 18 years). Most of the patients had pancytopenia with hypocellular bone marrow (BM) showing dysplastic hematopoietic precursors and increased blasts. None of these patients was previously treated for malignancy nor had a previous diagnosis of genetic syndromes. The diagnosis and classification were done according to the criteria proposed by the International Consensus Classification of Myeloid Neoplasms and Acute Leukemias1. The pediatric MDS patients were classified as refractory cytopenia of childhood, RCC (5 patients), MDS-EB (6 patients), and MDS/AML (4 patients).
Conventional and Molecular Cytogenetic Analyses
The cytogenetic analysis from bone marrow cells was performed by G-banding as previously described by De Souza et al., 2014.10 Chromosomes were identified and arranged according to the International System for Cytogenomic Nomenclature, 2020.11 Fluorescence in situ hybridization (FISH) analyses were done to confirm the chromosome alterations using the following probes: D7S486 spectrum orange/CEP7 spectrum Green, LSI MLL dual-color break-apart rearrangement probe, LSI p53 spectrum orange, LSI EGR1 Spectrum Orange/ LSI D5S23, D5S721 Spectrum Green, LSI PML Spectrum Orange/ LSI RARA Spectrum Green and LSI RUNX1T1 Spectrum Orange Probe/ RUNX1 Spectrum Green Probe. The probes were from Vysis, Abbott Laboratories, USA. The slides preparation was done according to manufacturer protocols.
Results
Uncommon chromosome alterations were observed in 15 patients (7.5%) from 200 pMDS cases analyzed cytogenetically. These chromosome alterations were divided into four cytogenetic groups: hyperdiploidy, uncommon deletions, biclonal chromosomal alterations, and translocations, which represented 33.3% (5/15), 13.3% (2/15), 33.3% (5/15), and 20% (3/15), respectively. Of these patients, ten had disease progression before HSCT, among them one received the HSCT and nine patients died during disease evolution. Concerning the five patients who did not show disease evolution, four underwent HSCT. Nowadays, only three patients are still alive after HSCT. There is also a patient who remains stable in the clinical course of MDS (Table 1).
Table 1.
Pediatric MDS patients with uncommon cytogenetic alterations.
| Nº | Sex | Age (years) | Subtype | Karyotype | Cellularity | Blasts (%) | Cytopenias | Evolution to AML | HSCT |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 4 | MDS/AML | 49,XX,dup(1)(q21q32),+6,+8,+mar[4]/46,XX[16] | hypocellular | 23% | pancytopenia | Yes | No/ died |
| 2# | F | 16 | RCC | 51,XX,+4,+6,+8,+14,+20[3]/46,XX[41] | hypocellular | 3% | pancytopenia | No | Yes/ alive |
| 3 | F | 6 | MDS-EB | 58,XX,+X,+3,+5,+6,+8,+10,+11,+12,+13, +18,+20,+21[5]/58,XX,idem,dup(1) (q21q31)[14]/46,XX[21] | hypocellular | 16% | pancytopenia | Yes | No/ died |
| 4 | M | 5 | MDS-EB | 52,XY,+6,+8,+14,+16,+19,+22[3]/46,XY[19] | hypocellular | 5.8% | pancytopenia | Yes | No/ died |
| 5 | M | 3 | MDS-EB | 49,XY,del(3)(q21), del(6)(q21),+der(6)del(6)(q21),+8, +der(12)del(12)(p11)[21] | hypocellular | 16% | bicytopenia | Yes | Yes/died |
| 6 | M | 1 | RCC | 45,XY,−7 [15]/46,XY,del(7)(q22q32)[5] | hypocellular | 2% | pancytopenia | No | Yes/died |
| 7# | M | 13 | RCC | 46,XY,del(17)(p12)[9]/46,XY, del(17)(p12), del(12)(p13)[5]/46,XY, del(11)(q23)[3]/46,XY[34] | hypocellular | 1% | pancytopenia | No | Yes/ alive |
| 8 | F | 12 | MDS-EB | 47,XX,+8[4]/47,XX,+21[3]/46,XX[13] | hypocellular | 10% | bicytopenia | No | No |
| 9 | M | 5 | MDS/AML | 48,XY,+X,+8[6]/46,XY,add(7)(p22)[9]/46,XY[9] | hypocellular | 25% | bicytopenia | Yes | No/ died |
| 10 | F | 4 | MDS-EB | 47,XX,+21[5]/47,XX,+8[3]/46,XX[20] | normocelular | 15% | pancytopenia | Yes | No/died |
| 11 | M | 5 | MDS/AML | 46,XY,t(5;8)(q32;q22)[23]/46,XY[8] | hypocellular | 28% | pancytopenia | Yes | No/ died |
| 12 | F | 2 | MDS/AML | 46,XX,t(4;7)(p16;p15)[6]/46,XX[23] | hypocellular | 24% | bicytopenia | Yes | No/ died |
| 13 | F | 12 | MDS-EB | 46,XX,der(2)t(2;15)(q37;q21)[25] | normocelular | 16% | bicytopenia | Yes | No/ died |
| 14# | F | 11 | RCC | 46,XX,del(5)(q15q35)[15]/46,XX[28 ] | hypocellular | 3% | pancytopenia | No | Yes/ alive |
| 15 | F | 18 | RCC | 46,XX, del(5)(q12q33), del(13)(q14q12)[17]/46,XX[3] | normocelular | 4.5% | pancytopenia | Yes | No/ died |
The hyperdiploid karyotype represented 2.5% of all cases (5/200). Hyperdiploidy was subdivided into two subgroups: patients who only had chromosome gains (3/5) (Figure 1A) and patients who also had structural alteration (2/5). The structural alterations associated with hyperdiploid karyotype were: dup(1q); der(6)del(6)(q21); der(12)del(12)(p11). Most of these patients had advanced subtypes with severe pancytopenia and hypocellular BM. Three patients had MDS-EB, one MDS/AML, and one with RCC. All these patients were indicated for HSCT, but four had evolution to AML and three died before the HSCT. Only two patients actually underwent HSCT, the patient with RCC responded well to HSCT and is still alive. The patient with hyperdiploid and structural alteration presented post-HSCT cytogenetic and clinical relapse and died.
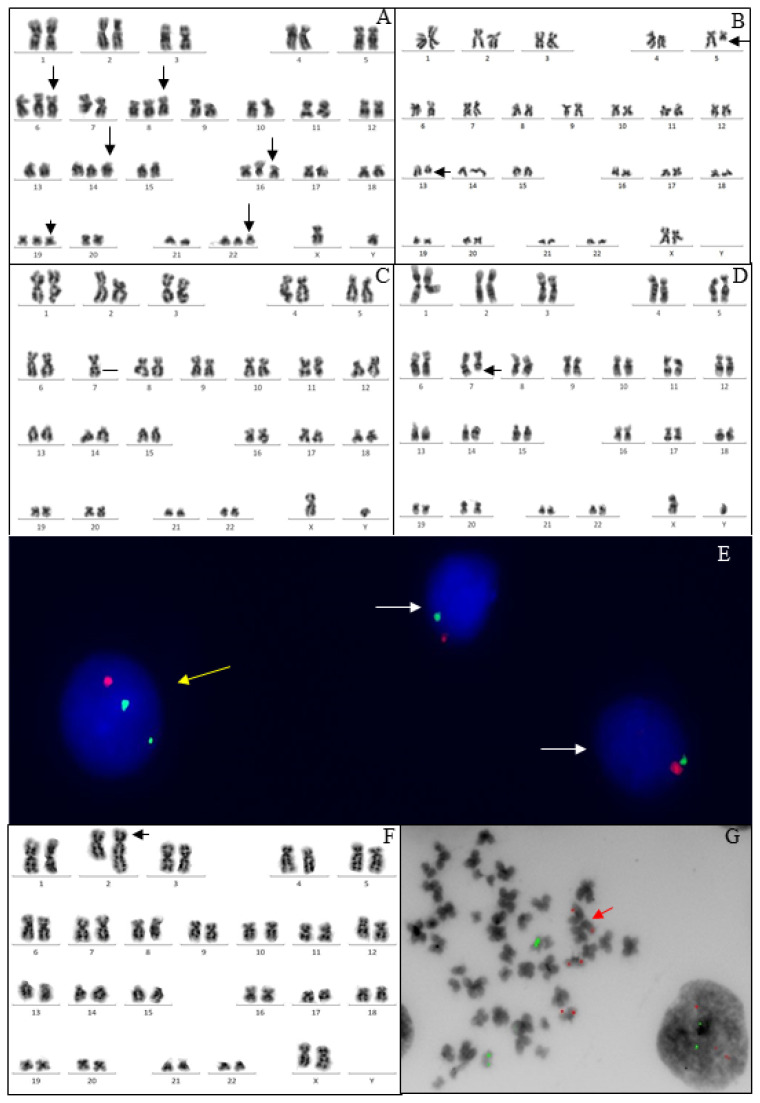
FIGURE 1.
Conventional and molecular cytogenetics of uncommon chromosomal alterations in pMDS patients. (A) Hyperdiploid karyotype; (B) Deletion of the long arm of chromosome 5 and deletion of the long arm of chromosome 13; Biclonal alteration: (C) Clone showing monosomy of chromosome 7, (D) Clone showing deletion of the long arm of chromosome 7 and (E) FISH using the D7S486 spectrum orange/CEP7 spectrum green probe identifying the two altered clones. The yellow arrow points to nuclei with a deletion of the long arm of chromosome monosomy 7 and the white arrow indicates a nucleus with monosomy of 7 ; (F) Unbalanced translocation between chromosomes 2 and 5 (G) FISH analysis of metaphase using the LSI PML/RARA Dual Color Single Fusion Probe that hybridizes with chromosome 15q22–24 (PML SpectrumOrange) and chromosome 17q21 (RARA SpectrumGreen ) showing two signals in chromosome 15 and one signal of chromosome 15 translocated to chromosome 2 and two green signals for chromosome 17.
Deletions of the long arm of chromosome 5 were observed in two patients, one of them had also del(13q) (Figure 1B). Both patients had pancytopenia and low blast count, being classified as RCC and both were indicated for HSCT. Nevertheless, only one received HSCT and this patient is still alive. The other patient did not have a compatible donor and was treated with azacytidine, but unfortunately died.
Biclonal karyotype was present in five patients, representing 2.5% of all cases (5/200). In two patients, independent clones, one with +8 and another with +21, were observed. Alterations involving chromosome 7 were present in two patients: one patient with a −7 clone and with a del(7q) clone (Figure 1 C–E). The second patient had an add(7p) clone and +X and +8 clone. The other patient had one clone with del(11)(q23) and another clone with del(17)(p12), which evolved by acquiring a second alteration generating a subclone del(17)(p12), del(12)(p13). Of patients with biclonal chromosomal alterations, two had RCC, two had MDSEB, and the other had MDS/AML. All patients had severe pancytopenia and BM dysplasias. Four patients were indicated for HSCT. However, two had disease progression before HSCT and died. The follow-up post-HSCT showed disease relapse in one patient who evolved to death, and the other patient is alive without disease. The two patients with +8 and +21 are still waiting for HSCT.
Chromosomal translocations were identified in three patients, representing 1.5% of all cases (3/200). Two patients with MDS/AML had balanced translocations, t(4;7)(p16;p15) and t(5;8)(q32;q22). The t(4;7)(p16;p15) patient had pancytopenia whereas the t(5;8)(q32;q22) patient had bicytopenia. In our study, unbalanced translocation, der(2)t(2;15)(q37;q21), was also observed in one patient with MDS-EB and normal cellularity. This patient also had three copies of chromosome 15, two normal and one translocated to chromosome 2 (Figure 1 F, G). All patients had a progression to AML and died before the HSCT.
Discussion
Pediatric MDS is characterized cytogenetically by clones containing alterations that involve mainly chromosomal partial losses (deletions) or chromosomal total losses (monosomies). These MDS cytogenetic patterns suggest that this disease is associated mainly with the inactivation or loss of tumor suppressor genes. 5,10
Pediatric patients with acute lymphoblastic leukemia (ALL) present hyperdyploidy as a frequent cytogenetic abnormality.12,13 Hyperdiploidy can be divided into two main subtypes: high hyperdiploidy (51–65 chromosomes) associated with favorable prognosis, and low hyperdiploidy (47–50 chromosomes) related with unfavorable prognosis.12,13 In MDS, the hyperdiploid karyotype is rare. However, patients with MDS may have complex karyotypes, with three or more chromosomal alterations, and are classified as very poor prognosis according to the IPSS-R.3 So, it is important to note the presence of hyperdiploidy in these cases.
Previously, our group reported the first case of high hyperdiploid karyotype in pMDS.14 In this study, we describe more four cases of hyperdiploid karyotype. However, these patients showed low hyperdiploidy. Three patients presented structural alterations such as deletions and duplications, which is uncommon in hyperdiploid karyotypes.13 The hyperdiploid was observed in the initial subtype and advanced subtypes. However, the HSCT was successful only in the initial subtype, highlighting the importance of an early diagnosis and indication for this treatment.
The most frequent cytogenetic alterations in adult MDS is del(5q), which is associated generally with a favorable prognosis and defines a unique MDS subcategory. 1,15 Nevertheless, del(5q) is extremely rare in children, and it seems to be associated with poor outcomes.16 In our study, the del(5q) was observed isolated, as previously published 17 and with del(13q). Both patients were indicated for HSCT. The patient with del(5q) as sole chromosomal abnormality had a good outcome post-transplant. Nevertheless, the other patient did not have a compatible donor. This patient was treated with azacytidine but showed disease evolution and died. Although it has been demonstrated that azacitidine is an efficient and safe MDS therapy for adult patients, data for this treatment in children is still lacking. In children, there is no established treatment to prevent or delay progression to leukemia before HSCT. However, some studies have shown that azacitidine is effective in some children with MDS and appears to be a non-toxic option in palliative situations to prolong survival. 18,19
Another uncommon finding in our study was unrelated clones, also known as biclonal chromosomal alterations, detected in one sample simultaneously by G-banding analysis. There are different hypotheses about the mechanisms that lead to these alterations. However, the actual mechanism is still unknown. Some authors believe those unrelated clones have the same founding molecular mutation and acquire different alterations over evolution, thus giving rise to unrelated cytogenetic clones.20–23 Nevertheless, nowadays there are molecular models of MDS development showing that distinct stem cells had different genetic variants at the same time.1
In adult patients, biclonal chromosomal alterations are also categorized as rare chromosomal abnormalities, representing 4.3–6.7% of the cases and being associated with disease relapse. These studies showed that the most recurrent chromosome alterations in unrelated clones were del(5q), +8, del(20q), del(7q), +11, +21, and −22.20,21 Previously, our group reported the first case of biclonal chromosomal alteration in a pMDS.22 The present study observed a frequency of biclonal chromosomal abnormalities of 2.5% (5/200), involving +8 and +21 as the most recurrent alterations. The leukemic evolution was observed in two patients (2/5), but it is important to note that the others were treated with HSCT. Furthermore, two patients after HSCT had cytogenetic relapse and death, showing how difficult it is to treat patients with such chromosomal instability.
In pMDS, chromosomal translocations are uncommon findings and associated with unfavorable prognosis.24 In this study, two patients had balanced chromosomal translocation: t(5;8)(q32;q22), t(4;7)(p16;p15), and one patient showed unbalanced translocation der(2)t(2;15)(q37;q21). These alterations were not previously reported in hematological neoplasm according to the Atlas of Genetics and Cytogenetics in Oncology and Haematology, 2022.15 The patients with balanced and unbalanced translocations were diagnosed with MDS/AML, showed disease progression to AML and died. The unfavorable outcome of our patients suggests that the chromosomal translocations are associated with an adverse prognosis.
Chromosomal abnormalities play an essential role in the diagnosis and prognosis of patients with MDS, but approximately 50% of patients have a normal karyotype observed by G-banding analysis. In these cases, complementary molecular methodologies may provide relevant prognostic information, such as the analysis using next-generation sequencing (NGS).25 Identification of genetic variants through the NGS opens new opportunities to characterize the genomic architecture of patients with MDS and contributes to the establishment of prognostic biomarkers.25–28 In this sense, it was developed the Molecular-IPSS for adult patients, which integrates the cytogenetic, molecular, and hematological features.28 In our study, although the focus was on cytogenetics, the analysis using NGS with a customized panel could provide complementary information associated with the prognosis reinforcing our findings. However, due to the high cost of NGS tests, these are not yet a reality globally used, mainly in developing countries. So, cytogenetics continues to play an important role for patients with hematologic malignancies, mainly for pMDS where yet little is known about the predictive value for molecular alterations due to the rarity of this disease. Since this study was the first with a large cohort of patients with pMDS focusing on rare chromosomal alterations and their impact on prognosis, it is necessary to confirm our results in other cohorts to provide a better understanding and to determine the true prognostic value of these uncommon chromosomal alterations in pMDS.
Conclusions
In summary, in our study, the uncommon chromosomal alterations in pMDS were associated with unfavorable prognosis. The study of uncommon cytogenetic alterations in pMDS is extremely important to contribute to the stratification of cytogenetic risk groups and early indication of HSCT.
Acknowledgements
This study was supported by Fundação Carlos Chagas Filho de Amaro à Pesquisa do Estado do Rio de Janeiro (FAPERJ) (FAPERJ/E-26/201.2018/2022) and the Brazilian Ministry of Health (Instituto Nacional de Câncer/INCA, Brazil).
Footnotes
Competing interests: The authors declare no conflict of Interest.
Author Contributions.: VLL, BFS, and TSF wrote the manuscript. TSF designed the study. VLL, BFS, EFR, MLRRB, and TJMS performed the cytogenetic and FISH analysis. RCBT, APB, and ESC analyzed the clinical data. TSF and TJMS reviewed critically the manuscript for important intellectual content. All authors have read and approved the manuscript.
Ethics Approval and Consent to Participate.: This study was approved by the Ethics and Research Committee of the National Cancer Institute (reference number # 3401739) in accordance with the Declaration of Helsinki. Informed consent was obtained from the children’s parents.
Funding Statement.: This study was supported by Fundação Carlos Chagas Filho de Amaro à Pesquisa do Estado do Rio de Janeiro (FAPERJ) (FAPERJ/E-26/201.2018/2022) and the Brazilian Ministry of Health (Instituto Nacional de Câncer/INCA, Brazil).
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Arber DA, Orazi A, Hasserjian RP, et al. International Consensus Classification of Myeloid Neoplasms and Acute Leukemias: integrating morphologic, clinical, and genomic data. Blood. 2022;140(11):1200–1228. doi: 10.1182/blood.2022015850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hasle H. Myelodysplastic and myeloproliferative disorders of childhood. Hematology Am Soc Hematol Educ Program. 2016;2016(1):598–604. doi: 10.1182/asheducation-2016.1.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greenberg PL, Tuechler H, Schanz J, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120(12):2454–65. doi: 10.1182/blood-2012-03-420489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moriwaki K, Manabe A, Taketani T, et al. Cytogenetics and clinical features of pediatric myelodysplastic syndrome in Japan. Int J Hematol. 2014;100(5):478–84. doi: 10.1007/s12185-014-1674-z. [DOI] [PubMed] [Google Scholar]
- 5.Bacher U, Schanz J, Braulke F, Haase D. Rare cytogenetic abnormalities in myelodysplastic syndromes. Mediterr J Hematol Infect Dis. 2015;7:e2015034. doi: 10.4084/mjhid.2015.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lamim Lovatel V, Otero L, Orlando EP, et al. Clinical and Prognostic Features in a Young Adult Patient with de novo Myelodysplastic Syndrome Presenting t(11;16)(q23;q24) Mediterr J Hematol Infect Dis. 2022;14(1):e2022013. doi: 10.4084/MJHID.2022.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grimwade D, Hills RK, Moorman AV, et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116(3):354–65. doi: 10.1182/blood-2009-11-254441. [DOI] [PubMed] [Google Scholar]
- 8.Mrózek K, Kohlschmidt J, Blachly JS, et al. Outcome prediction by the 2022 European LeukemiaNet genetic-risk classification for adults with acute myeloid leukemia: An Alliance study. Leukemia. 2023;37(4):788–798. doi: 10.1038/s41375-023-01846-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Platte V, Bergmann A, Hildebrandt B, et al. Clinical and Cytogenetic Characterization of Early and Late Relapses in Patients Allografted for Myeloid Neoplasms with a Myelodysplastic Component. Cancers. 2022;14(24):6244. doi: 10.3390/cancers14246244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Souza DC, de Fernandez CS, Camargo A, et al. Cytogenetic as an important tool for diagnosis and prognosis for patients with hypocellular primary myelodysplastic syndrome. Biomed Res Int. 2014;2014:542395. doi: 10.1155/2014/542395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McGowan-Jordan J, Hastings RJ, Moore S. Karger SAG, editor. ISCN 2020 an International System for Human Cytogenomic Nomenclature. 2020 doi: 10.1159/isbn.978-3-318-06867-2. [DOI] [PubMed] [Google Scholar]
- 12.Enshaei A, Vora A, Harrison CJ, et al. Defining low-risk high hyperdiploidy in patients with pediatric acute lymphoblastic leukaemia: a retrospective analysis of data from the UKALL97/99 and UKALL2003 clinical trials. Lancet Haematol. 2021;8(11):e828–e839. doi: 10.1016/S2352-3026(21)00304-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lejman M, Chałupnik A, Chilimoniuk Z, Dobosz M. Genetic Biomarkers and Their Clinical Implications in B-Cell Acute Lymphoblastic Leukemia in Children. Int J Mol Sci. 2022;23(5):2755. doi: 10.3390/ijms23052755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Souza Fernandez T, Ornellas MH, de Tavares RC, et al. Hyperdiploid karyotype in a child with hypocellular primary myelodysplastic syndrome. Eur J Haematol. 2003;71(5):399–401. doi: 10.1034/j.1600-0609.2003.00150.x. [DOI] [PubMed] [Google Scholar]
- 15.Atlas of Genetics and Cytogenetics in Oncology and Haematology in 2013. Huret JL, Ahmad M, Arsaban M, et al. Nucleic Acids Res. 2013 Jan;41(Database issue):D920–4. doi: 10.1093/nar/gks1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gurnari C, Piciocchi A, Soddu S, et al. Myelodysplastic syndromes with del(5q): A real-life study of determinants of long-term outcomes and response to lenalidomide. Blood Cancer J. 2022;12(9):132. doi: 10.1038/s41408-022-00724-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Souza DC, Otero L, Tavares R, de C, et al. An uncommon case of a child with del(5q) and hypocellular myelodysplastic syndrome. Pediatr Blood Cancer. 2010;55(4):767. doi: 10.1002/pbc.22633. [DOI] [PubMed] [Google Scholar]
- 18.Cseh AM, Niemeyer CM, Yoshimi A, et al. Therapy with low-dose azacitidine for MDS in children and young adults: a retrospective analysis of the EWOG-MDS study group. Br J Haematol. 2016;172(6):930–936. doi: 10.1111/bjh.13915. [DOI] [PubMed] [Google Scholar]
- 19.Waespe N, Van Den Akker M, Klaassen RJ, et al. Response to treatment with azacitidine in children with advanced myelodysplastic syndrome prior to hematopoietic stem cell transplantation. Haematologica. 2016;101(12):1508–1515. doi: 10.3324/haematol.2016.145821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han JY, Theil KS, Hoeltge G. Frequencies and characterization of cytogenetically unrelated clones in various hematologic malignancies: seven years of experiences in a single institution. Cancer Genet Cytogenet. 2006;164(2):128–32. doi: 10.1016/j.cancergencyto.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 21.Han JY, Kim KH, Kwon HC, et al. Unrelated clonal chromosome abnormalities in myelodysplastic syndromes and acute myeloid leukemias. Cancer Genet Cytogenet. 2002;132(2):156–8. doi: 10.1016/S0165-4608(01)00549-0. [DOI] [PubMed] [Google Scholar]
- 22.Rodrigues EF, de Souza DC, Camargo A, et al. Cytogenetic biclonality in a child with hypocellular primary myelodysplastic syndrome. Cancer Genet Cytogenet. 2007;178(1):70–2. doi: 10.1016/j.cancergencyto.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 23.Chen J, Kao YR, Sun D, et al. Myelodysplastic syndrome progression to acute myeloid leukemia at the stem cell level. Nat Med. 2019;25(1):103–110. doi: 10.1038/s41591-018-0267-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koppalkar RK, Rao PS, Sandhya I, Pai Muktha R. A Rare Translocation in a Paediatric Myelodysplastic Syndrome. Journal of Clinical and Diagnostic Research. 2018;12(12):ED07–ED09. doi: 10.7860/JCDR/2018/37527.12330. [DOI] [Google Scholar]
- 25.Zeng X, Zhang Y, Zhao K, et al. Somatic mutations predict prognosis in myelodysplastic syndrome patients with normal karyotypes. Signal Transduct Target Ther. 2021;6(1):274. doi: 10.1038/s41392-021-00606-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu L, Gu ZH, Li Y, et al. Genomic landscape of CD34+ hematopoietic cells in myelodysplastic syndrome and gene mutation profiles as prognostic markers. Proc Natl Acad Sci U S A. 2014;111(23):8589–94. doi: 10.1073/pnas.1407688111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schwartz JR, Ma J, Lamprecht T, et al. The genomic landscape of pediatric myelodysplastic syndromes. Nat Commun. 2017;8(1):1557. doi: 10.1038/s41467-017-01590-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernard E, Tuechler H, Greenberg PL, et al. Molecular international prognostic scoring system for myelodysplastic syndromes. NEJM evidence. 2022;1(7):EVIDoa 2200008. doi: 10.1056/EVIDoa2200008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.