Abstract
Backgrounds
Cutaneous T cell lymphoma (CTCL) is a non-Hodgkin lymphoma characterized by skin infiltration of malignant T cells. The biological overlap between malignant T cells and their normal counterparts has brought obstacles in identifying tumor-specific features and mechanisms, limiting current knowledge of CTCL pathogenesis. Transcriptional dysregulation leading to abnormal gene expression profiles contributes to the initiation, progression and drug resistance of cancer. Therefore, we aimed to identify tumor-specific transcription factor underlying CTCL pathology.
Methods
We analyzed and validated the differentially expressed genes (DEGs) in malignant T cells based on single-cell sequencing data. Clinical relevance was evaluated based on progression-free survival and time to next treatment. To determine the functional importance, lentivirus-mediated gene knockdown was conducted in two CTCL cell lines Myla and H9. Cell survival was assessed by examining cell viability, colony-forming ability, in-vivo tumor growth in xenograft models, apoptosis rate and cell-cycle distribution. RNA sequencing was employed to investigate the underlying mechanisms.
Results
Activating transcription factor 5 (ATF5) was overexpressed in malignant T cells and positively correlated with poor treatment responses in CTCL patients. Mechanistically, ATF5 promoted the survival of malignant T cells partially through the PI3K/AKT/mTOR pathway, and imparted resistance to endoplasmic reticulum (ER) stress-induced apoptosis.
Conclusions
These findings revealed the tumor-specific overexpression of the transcription factor ATF5 with its underlying mechanisms in promoting tumor survival in CTCL, providing new insight into the understanding of CTCL’s pathology.
Keywords: cancer pathogenesis, transcription factor, malignant T cell, phosphoinositide 3-kinase, endoplasmic reticulum stress
1. Introduction
Cutaneous T cell lymphomas (CTCLs) are a heterogeneous group of non-Hodgkin lymphomas, including mycosis fungoides (MF), Sézary syndrome (SS), and primary cutaneous CD30-positive lymphoproliferative disorders (CD30+LPDs) (1). Despite evident heterogeneity and interconnections among its subtypes, the mechanisms driving the development and progression of CTCL have not been fully elucidated. CTCL is characterized by cutaneous infiltration of monoclonally proliferative skin-homing T cells, alongside polyclonal reactive T cells triggered by inflammation and malignancy (2). The biological overlap between malignant T cells and normal T cells within cutaneous lesions presents challenges in unraveling the tumor-specific pathogenesis.
Efforts in recent decades have aimed to discover molecular markers that are specifically expressed in malignant T cells, as opposed to benign T cells. Loss of pan-T antigens, such as CD7 (3) and CD26 (4) was observed in circulating CD4+ T cells with morphological aberrance and has been applied in clinical diagnosis (5). The functional importance of these biomarkers to CTCL development, however, has rarely been depicted in previous studies. Immunostaining of thymocyte selection-associated high-mobility group box (TOX) was proposed to distinguish between CTCL, especially early-stage MF, and benign inflammatory dermatosis (BID) (6). However, the reactive T cells in BID commonly express TOX, limiting the development of targeted therapy (7). Other malignant T cell-specific molecular markers, such as KIR3DL2 (CD158k), have shown promising efficacy as therapeutic targets, tending to be expressed in Sézary cells or in patients with late-stage MF (8, 9).
Transcription factors bind to specific DNA sequences in the enhancers and promoters to regulate transcription, a process converting genetic information from DNA to mRNA (10). The well-organized expression of genes, under the proper regulation of transcription factors, is crucial for maintaining normal cellular structure and function (11). On the other hand, dysregulated transcription factors result in abnormal gene expression and disrupted cellular homeostasis, representing a key characteristic in the development of cancer (12). The aberrant gene expression pattern led by transcriptional dysregulation contributes to tumor initiation, progression and drug resistance (13–18). Therefore, understanding dysregulated transcription factors in cancer provides valuable insights into the mechanisms driving tumorigenesis and helps develop efficient treatment strategies (19, 20). In recent years, single-cell-based transcriptome sequencing combined with TCR sequencing has enabled the identification of malignant T cells at the single-cell level, offering a new perspective into the heterogeneous dysregulation of transcription within CTCL skin lesions. Based on previously reported single-cell RNA sequencing (scRNA-seq) data from our group (21), we identified ATF5 as a prosurvival transcription factor specifically expressed in malignant T cells in CTCL and unraveled its underlying mechanism.
2. Materials and methods
2.1. Identification for differentially upregulated genes in malignant T cells
Single-cell RNA sequencing, cell type identification and gene expression comparison were conducted as described in our previous research (21). Specifically, data from 10× Genomics RNA and TCR sequencing of 13 samples were reanalyzed. Large-scale CNVs were inferred using the infercnv package. Malignant T cells were differentiated from normal T cells based on CNVs and TCR clonotype. Differential RNA expression was determined between malignant T cells and their respective normal CD4+ T cells or CD8+ T cells from each sample. For the 11 samples of CD4+ CTCL, normal CD4+ T cells were referred to as the normal T and compared with their malignant T cells. Similarly, for the 2 samples of CD8+ CTCL, normal CD8+ T cells were referred to as normal T and compared with malignant T cells. Differentially upregulated genes were defined by a fold change>1.5 and adjusted p value<0.05.
2.2. CTCL cell lines and primary cells
Human CTCL cell lines H9, Myla, HH, Hut78, Mac1, Mac2A, PB2B, and Sz4 and the acute T-cell leukemia cell line Jurkat were cultured in RPMI-1640 medium with 10% fetal bovine serum, 100 U/ml penicillin, and 0.1 mg/ml streptomycin. Human CTCL cell line MJ was cultured in IMDM with 20% fetal bovine serum, 100 U/ml penicillin, and 0.1 mg/ml streptomycin.
Peripheral blood mononuclear cells (PBMCs) were obtained from 2 healthy donors by Ficoll-Paque PLUS (GE Healthcare). Peripheral blood CD4+ T cells were purified from PBMCs with a CD4+ T cell isolation kit (Biolegend).
2.3. Cell treatment
Cells were seeded in 12-well plates at a density of 1×10^5/ml. Hypoxia was induced by adding liquid paraffin on top to seal the culture medium. Drug concentrations were labeled in graphs or as follows: hydrogen peroxide (H2O2), 200 μM; low glucose, 1 mM; low serum, 1% fetal bovine serum; paraquat, 100 μM; thapsigargin, 5 nM for H9, 200 nM for Myla; tunicamycin, 0.5 μM for H9, 1 μM for Myla.
2.4. Lentivirus-mediated gene knockdown and overexpression
Two lentivirus short hairpin RNA (shRNA) vectors were constructed using the GV644 vector (GeneChem) and two independently designed oligonucleotides encoding shRNAs against ATF5. Control vectors were constructed with oligonucleotides encoding scrambled shRNA. The ATF5 lentivirus overexpression vector was constructed by ligating full-length human ATF5 (NM_001193646) cDNA into the GV643 vector (GeneChem). Cells were transfected according to the manufacturer’s instructions. shRNA oligonucleotide sequences are listed in Supplementary Table S1 .
2.5. Cell viability and apoptosis assays
For cell viability in normal culture, cells were cultured for 96h, and MTS-based cell viability was measured at 0h, 24h, 48h, 72h, and 96h using Cell Viability Colorimetric Assay Kit (Promega). Relative cell viability at each time point was normalized by reads at 0h. For LY294002 treatment, cells of shATF5 and shNC groups were treated and cultured for 48h. For each group, cell viability value after drug treatment (OD) was normalized by the cell viability value of the counterpart untreated cells (OD0μM), calculated as OD/OD0μM. This calculation obtains the relative cell viability, as shown in the bar graph.
For apoptosis, cells were stained with Annexin V-APC (BD Pharmingen) and apoptosis rates were quantified by flow cytometry. For drug-induced specific apoptosis, cells of shATF5 and shNC groups were treated as indicated. For each group, apoptosis rates with and without drug treatment were measured. Specific apoptosis was calculated using the formula: (percentage of apoptosis in treated cells - percentage of spontaneous apoptosis in untreated cells)/(100 - percentage of spontaneous apoptosis in untreated cells) (22, 23).
2.6. Lactate production assays
Lactate production assays were conducted using a lactate assay kit (Yuanye) and measured by absorbance (OD) at 540 nm. Cells of shATF5 and shNC groups were seeded at a density of 2×105/ml. The lactate concentration (mmol/L) in the cell culture supernatant was calculated as [OD-OD(culture medium without cells)]/[OD-OD(standard)] × standard concentration × dilution ratio. Lactate production at 48 h was calculated as (lactate concentration of cell supernatant) – (lactate concentration of culture medium without cells).
2.7. Bioinformatic analysis
Functional annotation was conducted on DAVID (https://david.ncifcrf.gov/). Enriched pathways are listed in Supplementary Table S2 . The promoter sequence from -2 kb to +100 bp of the PIK3AP1 transcription start site was obtained from NCBI and was subjected to Jaspar (https://jaspar.genereg.net) for motif searching. The retrieved results are listed in Supplementary Table S3 .
2.8. Statistics
Statistics were analyzed with GraphPad Prism (version 8.4.3) and R (version 4.0.3). Significant differences between two independent groups were analyzed by Student’s two-tailed t test. The correlation between the expression levels of two genes was determined by Spearman analysis. Kaplan−Meier analysis was performed and plotted using the survminer package (https://CRAN.R-project.org/package=survminer). A p value<0.05 was considered statistically significant.
3. Results
3.1. ATF5 is overexpressed in malignant T cells and is associated with unfavorable treatment responses in CTCL
To identify dysregulated transcription factors in malignant T cells in cutaneous T-cell lymphoma (CTCL), we conducted an analysis on the differentially expressed genes (DEGs) between malignant T cells and benign reactive T cells based on a single-cell RNA sequencing (scRNA-seq) dataset from our previous study (21). Within this dataset, the differentially upregulated genes (fold change>1.48, adjusted p value<0.05) were sorted based on the frequency of occurrence across the samples. The transcription regulator TOX, which has previously been reported as a marker for differential diagnosis between CTCL and benign inflammatory dermatoses (6), was found to be specifically upregulated in the malignant T cells in 4 out of 13 samples. Therefore, genes upregulated in 5 samples or more were defined as frequently recurrent DEGs in malignant T cells and are listed in Table 1 . Among these genes, transcription factors ATF5 and BHLHE40 were identified. Other frequently recurrent DEGs were involved in various cellular processes, including cellular interactions (LGALS1, LGALS3, SPINT2, CXCL13, LAIR2, ITM2A, CLU), cell metabolism (GAPDH, TPI1, SMS), signal transduction (S100A6, S100A11, S100A10, S100A4, ANXA2), cytoskeleton (LMNA, TUBA1B, TAGLN2), mitosis (STMN1, PTTG1), cellular transportation (MFSD10), cancer-testis antigens (PAGE5, CST7), redox reaction (PRDX1), protein folding (PPIA) and lncRNA (AC006129.4).
Table 1.
Frequently recurrent DEGs from scRNA-seq.
| Functional classification | Gene symble | Number of samples* | Average fold change# |
|---|---|---|---|
| Transcription factor | ATF5 | 6 | 1.81 |
| BHLHE40 | 5 | 1.77 | |
| Cellular interaction | LGALS1 | 9 | 2.93 |
| LGALS3 | 6 | 2.20 | |
| SPINT2 | 6 | 1.99 | |
| CXCL13 | 5 | 4.42 | |
| LAIR2 | 5 | 1.77 | |
| ITM2A | 5 | 1.63 | |
| CLU | 5 | 1.48 | |
| Cell metabolism | GAPDH | 7 | 2.33 |
| TPI1 | 7 | 2.09 | |
| SMS | 5 | 1.79 | |
| signal transduction | S100A6 | 8 | 1.78 |
| S100A11 | 8 | 1.48 | |
| S100A10 | 6 | 1.56 | |
| S100A4 | 5 | 1.68 | |
| ANXA2 | 5 | 1.64 | |
| cytoskeleton | LMNA | 6 | 2.04 |
| TUBA1B | 5 | 1.96 | |
| TAGLN2 | 5 | 1.51 | |
| mitosis | STMN1 | 5 | 1.90 |
| PTTG1 | 5 | 1.84 | |
| cellular transportation | MFSD10 | 5 | 1.59 |
| cancer-testis antigen | PAGE5 | 5 | 1.89 |
| CST7 | 5 | 1.60 | |
| redox reaction | PRDX1 | 5 | 1.92 |
| Protein folding | PPIA | 6 | 1.49 |
| IncRNA | AC006129.4 | 5 | 1.76 |
*the number of samples where this gene differentially upregulated in malignant T cells (fold change>1.48 and p.adj<0.05). #Average fold change was determined between all the malignant T cells and normal T cells from 13 samples.
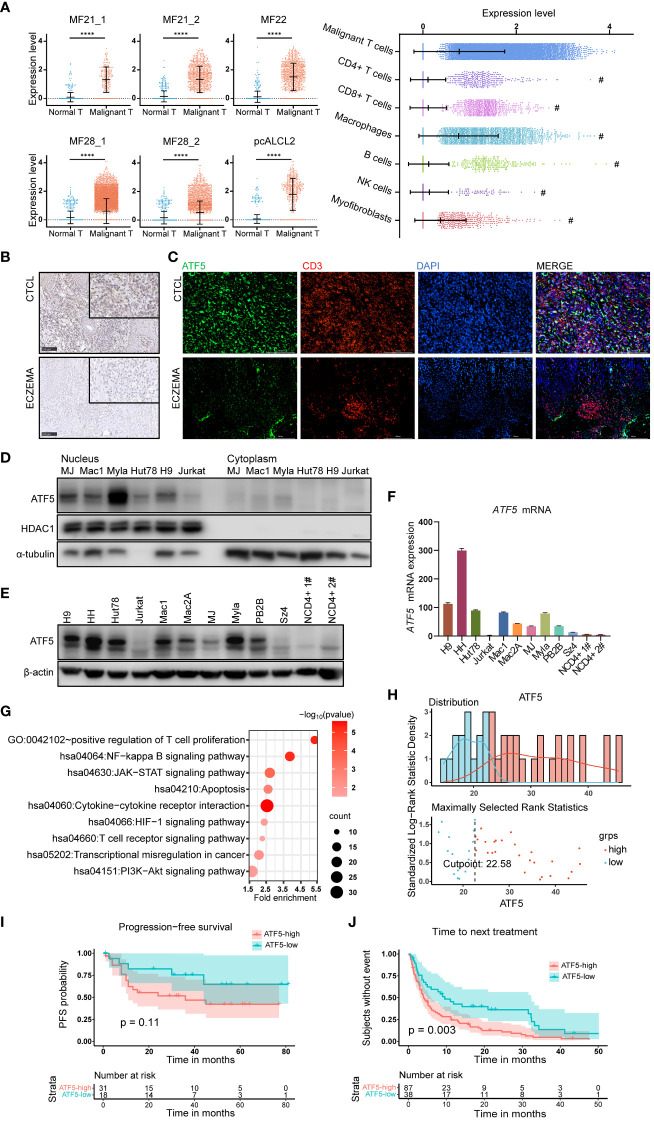
Notably, ATF5, a member of the basic leucine zipper (bZip) family (24), was the most consistently upregulated transcription factor across multiple samples. ATF5 was upregulated in malignant T cells from 6 lesions in 4 patients, while its expression remained low in normal T cells ( Figure 1A ). We also compared the expression levels of ATF5 across different cell types in the tumor microenvironment (25–27). We found that malignant T cells exhibit the highest expression of ATF5 compared to other cell types, while macrophages also demonstrate significant levels of ATF5 expression, the clinical significance of which is yet to be determined ( Figure 1A ). In the cases where more than one biopsy was taken (MF21 and MF28) (21), the expression levels of ATF5 in malignant T cells from different skin lesions were similar, regardless of biopsy site or lesion duration ( Figure 1A ). This observation, consistent with a previous study (28), indicated that the overexpression of ATF5 was more likely due to intrinsic malignant traits rather than a lesion-specific environment. Immunohistochemical staining of ATF5 ( Figure 1B ) and immunofluorescent co-staining with CD3 ( Figure 1C ) on lesional biopsies confirmed the increased expression of ATF5 protein in atypical CD3+ T cells from CTCL patients compared to normal CD3+ T cells from benign inflammatory dermatoses patients. Consistent with its main role as a transcription factor, ATF5 protein was predominantly detected in the nuclear component of patient samples ( Figures 1B, C ; Supplementary Figure 1 ) and CTCL cell lines ( Figure 1D ). Furthermore, CTCL cell lines showed heterogeneous, yet consistently higher, expression of ATF5 at both the mRNA and protein levels, compared to peripheral blood CD4+ T cells from healthy donors and the non-CTCL T-cell leukemic cell line Jurkat ( Figures 1E, F ).
Figure 1.
ATF5 is highly expressed in cutaneous T cell lymphoma and associates with poor treatment response. (A) Normalized ATF5 expression in various cell types in 6 samples from 4 CTCL patients who have higher ATF5 expression in malignant T cells. Malignant T: malignant T cells, Normal T: normal T cells (B) Representative images of immunohistochemical staining of ATF5 in paraffin-embedded tissues from CTCL patients and eczema patients. Original magnification ×200, insets ×400, scale bar=50 μm. (C) Representative images of immunofluorescence costaining of ATF5 (green) and CD3 (red) in paraffin-embedded tissues from CTCL patients and eczema patients. DAPI (blue) was used to visualize cell nuclei. Original magnification ×200, scale bar=200 μm. (D) ATF5 protein expression in nuclear and cytoplasmic lysates of CTCL cell lines and Jurkat cells. (E, F) Expression levels of ATF5 protein (E) and mRNA (F) in 9 CTCL cell lines, Jurkat cells, and CD4+ T cells from 2 normal controls (NCD4+ 1#, NCD4+ 2#). ATF5 mRNA expression levels were normalized to GAPDH. (G) Annotated pathways from genes (n=873, p<0.05) positively correlated with ATF5 expression in our previously reported CTCL cohort with RNA sequencing (FDR<0.25, p<0.05). (H) ATF5 expression distribution and cut point for prognosis and treatment analysis in the CTCL cohort. A total of 49 patients with regular follow-up were recruited from March 2010 to December 2018. The median (range) follow-up duration was 32 (1–81) months. (I) Kaplan−Meier survival analysis of PFS (n=49 patients). Progression-free survival information was collected for each patient from the time of biopsy to the time of disease progression. (J) Kaplan−Meier survival analysis of TTNT (n=125 treatment episodes). Data are shown as mean ± SD and representative of at least three independent experiments. ****P<0.0001.
Considering the relatively specific expression of ATF5 in malignant T cells, we evaluated the clinical relevance of ATF5 expression in a cohort of 49 tumor-stage CTCL patients with bulk RNA sequencing data which was published by our group previously (29). Genes positively correlated with ATF5 expression (n=873 genes with r>0, p<0.05) were enriched in pathways (FDR<0.25, p value<0.05) associated with CTCL development, including positive regulation of T cell proliferation, NF-kappa B signaling pathway, T cell receptor signaling pathway, JAK/STAT signaling pathway and PI3K/AKT pathway ( Figure 1G ; Table S2 ). These findings indicated that the upregulation of ATF5 in malignant T cells was implicated in the pathogenesis of CTCL. Patient prognosis was assessed through progression-free survival (PFS), while treatment response was evaluated by time to next treatment (TTNT). In this cohort, the median (range) follow-up duration was 32 (1–81) months. A total of 125 treatment episodes were administered during follow-up and were included in our analysis. Patients were divided into ATF5-high or ATF5-low group based on the transcriptional ATF5 levels. The cutoff value was determined by the surveminer package according to ATF5 expressions and the PFS data ( Figure 1H ). Patients in the ATF5-high group exhibited a tendency towards shorter progression-free survival, although the difference was not statistically significant ( Figure 1I ), which could be attributed to the fact that all the patients from this cohort were in the tumor stage. Notably, patients in the ATF5-high group experienced shorter durations in different lines of therapy ( Figure 1J ). Given the requirement for long-term medical treatment in CTCL patients, this rapid transition to subsequent therapeutic regimen indicated that patients with high ATF5 expression benefited less from current treatments, mainly due to unsatisfactory therapeutic effects (30).
Collectively, these results indicated the specific overexpression of the transcription factor ATF5 in malignant T cells among CTCL patients, which were associated with inferior therapeutic outcomes.
3.2. ATF5 knockdown hinders tumor survival by promoting cell apoptosis in CTCL lines
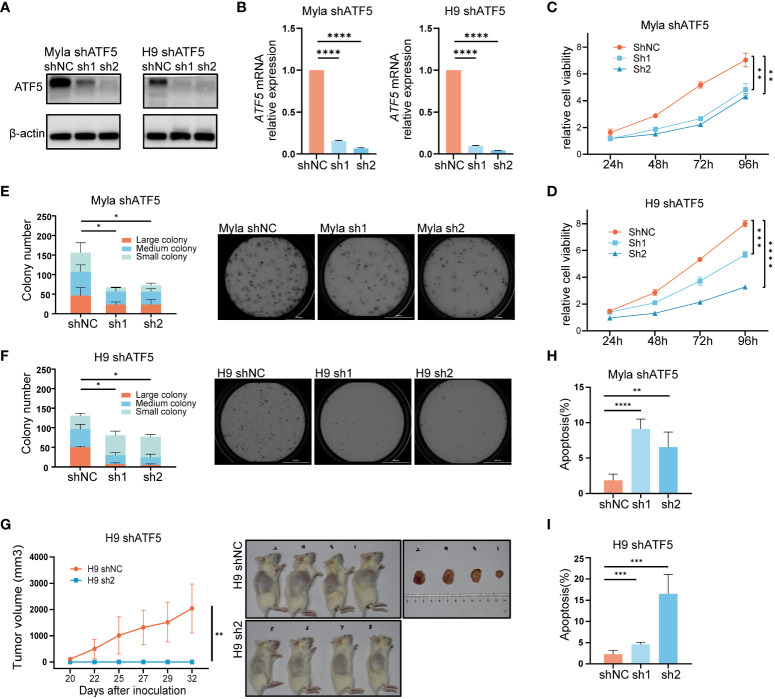
Given its specific overexpression in malignant T cells, we sought to investigate whether ATF5 contributed to malignant behaviors in CTCL. To understand the role of ATF5 in CTCL, we employed lentivirus-mediated shRNA transduction to suppress ATF5 expression in CTCL cell lines Myla and H9, with scrambled shRNA as a control. The suppression of ATF5 expression was confirmed at both the protein and mRNA levels ( Figures 2A, B ). MTS-based viability assays demonstrated reduced expansion rate in ATF5-knockdown (ATF5-KD) Myla and H9 cells ( Figures 2C, D ). In the colony-forming cell (CFC) assays, ATF5-KD Myla and H9 cells showed decreased colony number and size in semisolid cultures, indicating an impaired colony-forming ability ( Figures 2E, F ). Furthermore, ATF5 knockdown significantly impeded tumor growth in a xenograft model using H9 cells. ATF5-KD H9 cells failed to form subcutaneous tumors in the grafted sites, while control cells formed considerable tumors ( Figure 2G ). Therefore, ATF5 knockdown inhibited the survival of malignant T cells, prompting a further investigation of apoptosis and proliferation characteristics. Apoptosis rates were significantly increased in ATF5-KD Myla and H9 cells ( Figures 2H, I ), while cell cycle distributions were not remarkably affected by ATF5 suppression ( Supplementary Figure 2 ). Thus, the inhibition of tumor survival following ATF5 knockdown was primarily due to increased apoptosis rate.
Figure 2.
Interference with ATF5 expression inhibits CTCL cell growth. (A, B) Suppression of ATF5 protein (A) and mRNA (B) expression in Myla and H9 cell lines by lentivirus (shATF5) with two independent shRNA sequences (sh1, sh2). Cells transfected with scramble RNA were used as a control (shNC). Relative ATF5 mRNA expression was normalized to GAPDH and shNC. (C, D) Relative cell viability of control (shNC) and ATF5-KD (sh1, sh2) Myla and H9 cells normalized to 0 h. Student’s t-test was used to compare the relative cell viability of shNC vs. sh1 and shNC vs. sh2 at 96h. (E, F) Number of colonies of different sizes formed by control (shNC) and ATF5-KD (sh1, sh2) Myla (E) and H9 (F) cells in CFC assays. Representative pictures taken under microscope are shown on the right. Large colony: diameter > 60μm; medium colony: diameter between 30-60 μm; small colony: diameter < 30μm (G) Tumor sizes of xenograft models injected with control (shNC) and ATF5-KD (sh1, sh2) H9 cells. Tumor sizes were measured at the times indicated. Images of xenograft mice and tumors taken at the end of the experiment are shown on the right. (H, I) Apoptosis rate of control (shNC) and ATF5-KD (sh1, sh2) Myla (H) and H9 (I) cells. Data are shown as mean ± SD and representative of at least three independent experiments. *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001.
These results confirmed that ATF5 promoted tumor survival and contributed to the tumor progression of CTCL.
3.3. ATF5 protects malignant T cells against endoplasmic reticulum stress-induced apoptosis
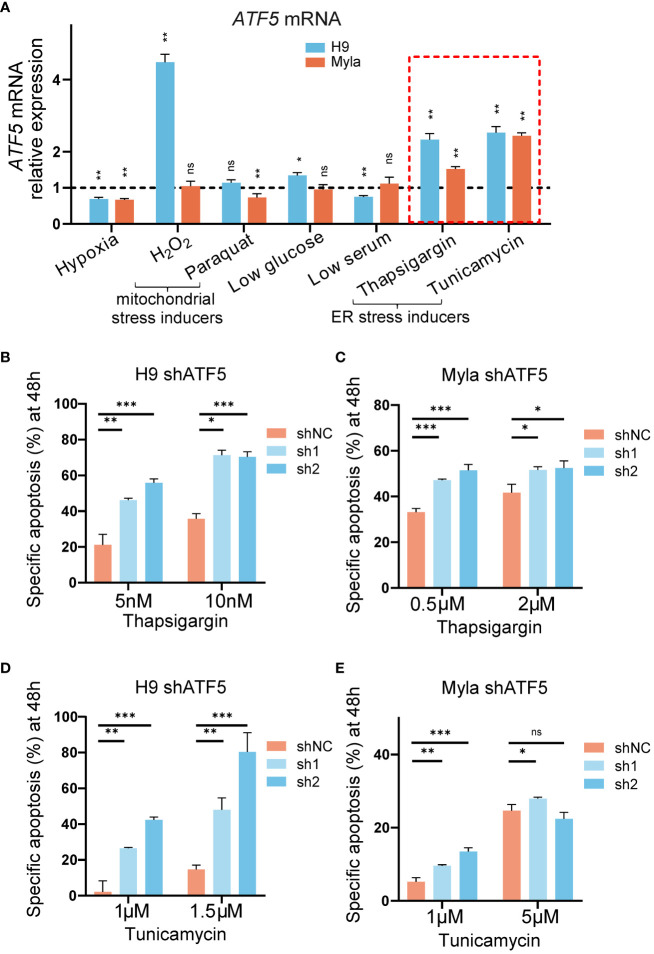
We noticed that the suppression of tumor survival induced by ATF5 knockdown was more prominent in semisolid cultures and xenograft models than in liquid cultures. Liquid-cultured cells are provided with moderate culture density, sufficient nutrients, and a suitable environment, whereas tumor cells face monoclonal expansion pressures in semisolid cultures and experience nutrient deficiency and hypoxia in xenograft models. Accumulating evidence suggests that ATF5 acts as a prosurvival factor under cellular stress (31–33). To assess the involvement of ATF5 in the stress response in CTCL, we exposed the liquid-cultured CTCL cell lines Myla and H9 to various stress-inducing conditions and assessed their impact on ATF5 expression. Both Myla and H9 cells were treated with various stressors, including hypoxia, mitochondrial stress inducers (H2O2, paraquat), low glucose, low serum and ER stress inducers (thapsigargin, tunicamycin). ATF5 expression showed a slight decline under hypoxia, while changes in expression were inconsistent between Myla and H9 cells under mitochondrial stress, low glucose, and low serum ( Figure 3A ). Notably, ATF5 consistently upregulated when treated with the ER stressors thapsigargin and tunicamycin in both cell lines (highlighted by the red dashed box in Figure 3A ). We further treated control and ATF5-KD cells with or without ER stress inducers and calculated ER stress-induced specific apoptosis (22). Notably, ATF5-KD Myla and H9 cells showed a marked increase in specific apoptosis induced by thapsigargin and tunicamycin ( Figures 3B–E ), indicating that ATF5 protects malignant T cells against ER stress-induced apoptosis in CTCL.
Figure 3.
ATF5 is upregulated under ER stress and protects cells from ER stress-induced apoptosis. (A) Relative ATF5 mRNA expression in Myla and H9 cells treated for 24h. Relative expression was normalized to GAPDH and vehicle. Relative ATF5 expressions of vehicle groups were normalized as 1 and indicated by the black dashed line. The red dashed box highlights ER stress inducers treatment. (B, C) Specific apoptosis of control (shNC) and ATF5-KD (sh1, sh2) H9 (B) and Myla (C) cells treated with thapsigargin for 48 h. (D, E) Specific apoptosis of control (shNC) and ATF5-KD (sh1, sh2) H9 (D) and Myla (E) cells treated with tunicamycin for 48 h. Data are presented as mean ± SD and representative of at least three independent experiments. ns, no significance, *P<0.05, **P<0.01, ***P<0.001.
Together, these results demonstrated that ATF5 protected against ER stress-induced apoptosis in CTCL.
3.4. ATF5 promotes CTCL partially through the PI3K/AKT/mTOR pathway
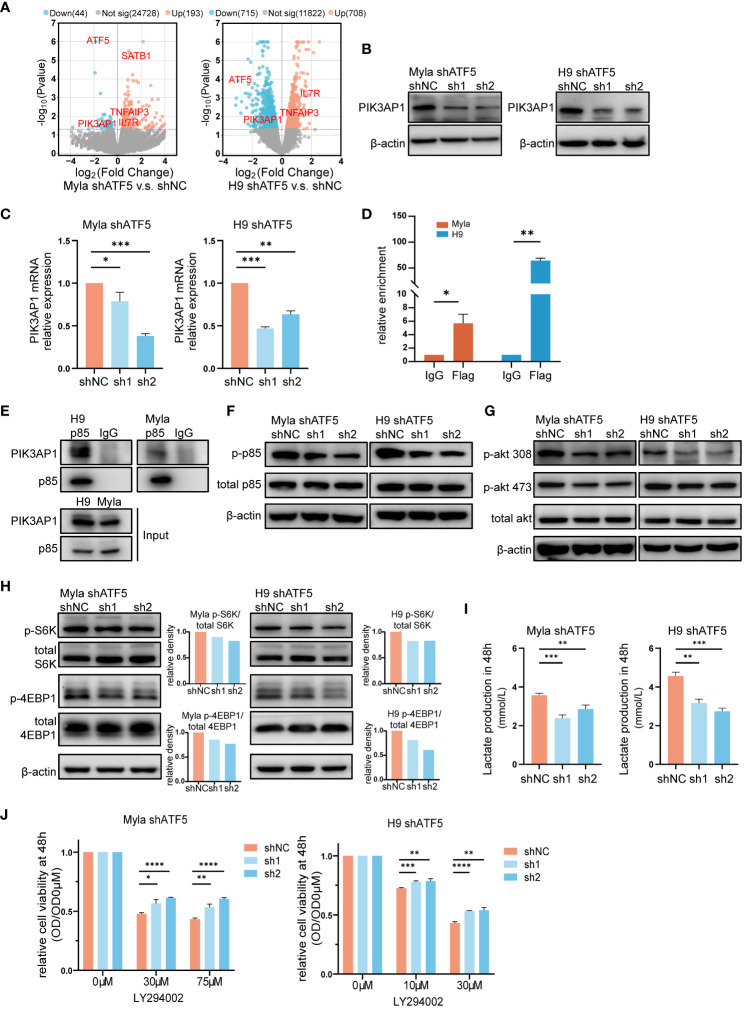
To investigate the mechanisms underlying the effects of ATF5 on CTCL cells, we performed transcriptome sequencing and identified differentially expressed genes (DEGs) between control and ATF5-KD Myla and H9 cells ( Figure 4A ). Since ATF5 primarily functions as a transcription factor, we focused on genes that were downregulated in both Myla and H9 cells upon ATF5 knockdown. Among these genes, PIK3AP1 exhibited the most significant reduction in expression ( Figures 4A–C ). PIK3AP1 is an adaptor protein required for the activation of PI3K/AKT signaling (34). PIK3AP1 promotes PI3K activity by directly binding to p85, enabling the phosphorylation of p85 by the intracellular segment of tyrosine receptor, and subsequently activates downstream PI3K/AKT pathway (34–36). PI3K phosphorylates AKT at Thr308 and Ser473, subsequently activating mTORC1 (37). The PI3K/AKT/mTOR activity, under the regulation of PIK3AP1, regulates T-cell homeostasis (35, 36), as well as tumor survival and metabolic adaptation (37, 38). Genes positively correlated with ATF5 in CTCL patients were enriched in the PI3K/AKT pathway ( Figure 1G ), which was essential for CTCL survival (39).
Figure 4.
The PI3K/AKT/mTOR pathway partially accounts for ATF5-promoted CTCL survival. (A) Volcano plot of upregulated (red) and downregulated (blue) DEGs (|fold change|>0 and P<0.05) between control (shNC) and ATF5-KD (shATF5) H9 and Myla cells. RNA was prepared 72 hours after transduction, following the validation of ATF5 knockdown. (B, C) Downregulation of PIK3AP1 protein (B) and mRNA (C) levels in control (shNC) and ATF5-KD (sh1, sh2) Myla and H9 cells. Relative PIK3AP1 mRNA expression was normalized to GAPDH and shNC. (D) Enrichment of ATF5 protein at the PIK3AP1 promoter in Myla and H9 cell lines stably expressing Flag-ATF5. (E) Immunoprecipitation in Myla and H9 cells using a p85 antibody or normal rabbit IgG with protein A/G agarose. PIK3AP1 and p85 were identified. (F-H) Phosphorylated p85, Akt, S6K and 4EBP1 in control (shNC) and ATF5-KD (sh1, sh2) Myla and H9 cells. The relative density of phosphorylated protein was normalized to total protein and control (shNC). Protein was prepared 72 hours after transduction, following the validation of ATF5 knockdown. (I) Lactate production at 48 h in control (shNC) and ATF5-KD (sh1, sh2) Myla and H9 cells. (J) Relative cell viability of control (shNC) and ATF5-KD (sh1, sh2) Myla and H9 cells after LY294002 treatment. Cell viability of the treated cells was normalized to that of the untreated cells at 48 h. Data are presented as mean ± SD and representative of at least three independent experiments. *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001.
Therefore, we investigated whether the overexpressed ATF5 activated the PI3K/AKT/mTOR pathway by upregulating PIK3AP1 transcription in CTCL. We analyzed the promoter region of PIK3AP1. The ATF/cAMP-responsive element binding protein (CREB) family, to which ATF5 belongs, share consensus binding sequences (40). Bioinformatic analysis of the PIK3AP1 promoter revealed the presence of several ATF/CREB transcription factor motifs within the region spanning -664 to -527 bp upstream of the transcription start site ( Table S3 ). Chromatin immunoprecipitation (ChIP) assays confirmed the direct binding of ATF5 to this region in Myla and H9 cells ( Figure 4D ), supporting the role of ATF5 in regulating PIK3AP1 expression. As an adaptor protein, PIK3AP1 recruits the p85 subunit of PI3K and enhances p85 phosphorylation, leading to activation of PI3K/AKT/mTOR pathway activity (34–36). Immunoprecipitation confirmed interaction between PIK3AP1 and p85 in Myla and H9 cells ( Figure 4E ). In addition to the downregulation of PIK3AP1 ( Figures 4B, C ), decreased phosphorylation of p85 was observed in ATF5-KD Myla and H9 cells ( Figure 4F ), as well as decreased phosphorylation of AKT at both Thr308 and Ser473 ( Figure 4G ), confirming reduced PI3K/AKT signaling activity regulated by ATF5. Downstream of the PI3K/AKT cascade, mTORC1 promotes protein synthesis by two critical effectors, p70S6 kinase (S6K) and 4EBP1 (41, 42). Phosphorylation of both S6K at Thr389 and 4EBP1 at Thr37/46 was suppressed in ATF5-KD Myla and H9, indicating decreased mTORC1 activity ( Figure 4H ). Apart from protein synthesis, mTORC1 also facilitates a shift from OXPHOS to glycolysis, which favors macromolecular synthesis to support rapid tumor growth (43). We found that the production of lactate, an end product of glycolysis, was decreased after ATF5 knockdown ( Figure 4I ), suggesting a reduced rate of glycolysis and consistent with the decreased activity of mTORC1.
To investigate the relationship between impaired survival and decreased PI3K/AKT/mTOR activity, we treated control and ATF5-KD Myla and H9 cells with the PI3K inhibitor LY294002. PI3K inhibition remarkably impaired cell survival in both cell lines, as reported previously (44, 45). The cell viability of treated cells (OD) was normalized by the viability of the corresponding untreated cells (OD0μM). ATF5-KD Myla and H9 cells showed less pronounced decreases in cell viability (higher relative cell viability) ( Figure 4J ). This indicates that cells with ATF5-KD and decreased PI3K activation are less vulnerable to further exogeneous PI3K inhibition, compared to cells with intact PI3K activity, suggesting that ATF5 promoted CTCL survival, at least in part, by enhancing PI3K/AKT/mTOR pathway activity.
Collectively, these results showed that ATF5 transcriptionally upregulated PIK3AP1 and enhanced the PI3K/AKT/mTOR pathway to promote the survival of CTCL.
4. Discussion
CTCL is a malignancy arising from mature skin-homing T cells, which provides adaptive defense and participates in skin inflammation (46–48). Identifying specific molecules and mechanisms in malignant T cells enhances our understanding of their aggressive behaviors. Hyperactivation of STAT3 and STAT5 has been shown to promote the survival of malignant T cells by transcribing oncogenic cytokines and microRNAs (49–51). Advanced-stage CTCL has been associated with a skewed T helper 2 phenotype driven by GATA3 (52, 53). These findings highlight the importance of transcriptional dysregulation in CTCL, while malignant T cell-specific transcription factors in CTCL were still lacking. In our study, we identified overexpression of the transcription factor ATF5 in malignant T cells and further elucidated its role in promoting CTCL. ATF5 belongs to the ATF/cAMP response element binding (CREB) protein family, a group of basic-region leucine zipper (bZIP) transcription factors (40, 54) that play crucial roles in regulating cell differentiation and survival (55, 56). Increased ATF5 expression has been reported in aggressive chronic lymphocytic leukemia (57), follicular lymphoma (58), and childhood acute lymphoblastic leukemia (59), implying potential involvement of ATF5 in the tumorigenesis and progression of these hematopoietic malignancies. Our study not only demonstrated the specific overexpression of ATF5 on malignant T cells, but also uncovered its functional significance in CTCL. Hence, our findings established ATF5 as a tumor-specific prosurvival transcription factor, contributing to the current understanding of transcriptional dysregulation in CTCL.
ATF5 has been implicated in tumor development by transcriptional regulation of downstream genes (60–63). We found that ATF5 enhanced the survival of malignant T cells partially through the PI3K/AKT/mTOR pathway downstream of PIK3AP1. Hyperactivation of the PI3K/AKT/mTOR pathway has been reported to promote CTCL (39). Treating CTCL by targeting the PI3K/AKT/mTOR pathway has been proven effective alone (64–67) or in combination with other strategies (45, 68), whereas the treatment responses vary among individuals. Multiple factors contributed to the regulation of PI3K/AKT/mTOR pathway. Our results showed that ATF5 promotes the activation of the PI3K/AKT/mTOR axis by regulating PIK3AP1, adding to the understanding of the regulation of this pathway in CTCL. Consequently, the expression levels of ATF5 in CTCL may serve as a molecular marker indicating the effectiveness of PI3K inhibition, thereby warranting further investigation.
Cellular ER stress can be triggered by intrinsic oncogenic signals, metabolic alterations, exposure to cytotoxic drugs, and changes in the microenvironment (69, 70). Tumor cells develop tolerance to ER stress as a survival strategy against these triggering conditions (71). Although ATF5 is not an established participant in the ER stress signaling, it has been reported to affect the tolerance to ER stress through diverse mechanisms (31, 72, 73). In our study, we have observed that ATF5 protected against ER stress-induced apoptosis. However, the mechanism through which ATF5 provides this protection is yet to be fully understood, and further investigation is required to elucidate this mechanism. Several studies have highlighted the link between the PI3K/AKT/mTOR pathway and ER stress. Activation of the PI3K/AKT pathway by PIK3AP1 mediates resistance to apoptosis under ER stress (74). And drug-induced ER stress leads to apoptosis by suppressing the PI3K/AKT/mTOR pathway (75, 76). These findings support the PI3K/AKT/mTOR pathway as a pro-survival factor under ER stress, which is consistent with our results. However, other studies have proposed that aberrantly activated mTORC1 lead to the accumulation of misfolded or unfolded proteins in the ER, thereby inducing ER stress (77, 78). Therefore, the interaction between the PI3K/AKT/mTOR pathway and ER stress remains controversial in different cellular contexts (79). Crosstalk between the mTOR pathway and ER stress is involved in cancer drug resistance (80, 81). Our results suggested a positive correlation between poor treatment response, increased PI3K/AKT/mTORC1 activity and ER stress resistance mediated by ATF5. Therefore, it remains to be elucidated whether the PI3K/AKT/mTOR activity and ER stress resistance enhanced by ATF5 are related and how they might contribute to the survival of malignant T cells during anticancer treatment.
In accordance with previous studies showing that ATF5 participates in the stress response (82, 83), we have demonstrated that ER stress inducers promote ATF5 expression in CTCL cell lines, but the specific mechanisms responsible are not fully understood. One possible explanation is the involvement of the unfolded protein response (UPR), which is activated in response to ER stress to restore ER homeostasis (84). Notably, activating transcription factor 4 (ATF4), a transcription factor downstream of UPR, has been reported to directly induce ATF5 expression in response to ER stress (31, 85). However, the complexity of ER stress signaling pathways leave open the possibility of additional mechanisms contributing to ATF5 upregulation, which should be investigated in future studies.
We found than ATF5 exhibited the highest expression in malignant T cells, while it was also prominently detected in macrophages in CTCL microenvironment, whose clinical relevance remains largely unknown. There has been a report of ATF5’s upregulation and involvement in THP-1 cell differentiation in vitro (86). The status of tumor microenvironment is closely related to treatment response in patients (87). Further investigations into the expression of ATF5 across diverse cell types could facilitate a comprehensive understanding of ATF5’s role in CTCL and its associated microenvironment.
In conclusion, our results revealed the tumor-specific upregulation of the transcription factor ATF5, which positively correlated with worse treatment responses. Upregulated ATF5 promoted CTCL through the PI3K/AKT/mTOR pathway and conferred resistance to ER stress in CTCL. Our study uncovered the functional roles of ATF5 in promoting CTCL and provided new insights into the distinct features between malignant T cells and normal T cells.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://doi.org/10.6084/m9.figshare.24151839.v1.
Ethics statement
The studies involving humans were approved by Peking University First College Hospital Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. The animal study was approved by Institutional Animal Care and Use Committee of Peking University First Hospital. The study was conducted in accordance with the local legislation and institutional requirements.
Author contributions
MC: Investigation, Validation, Writing – original draft, Visualization. PL: Methodology, Investigation, Writing – original draft. XL: Data curation, Writing – original draft, Resources. FL: Data curation, Writing – original draft, Methodology. YQ: Data curation, Writing – original draft, Formal Analysis. PT: Funding acquisition, Supervision, Writing – review & editing. YW: Supervision, Writing – review & editing, Funding acquisition, Project administration.
Acknowledgments
The authors acknowledge the faculties and students of Department of Dermatology and Venereology at Peking University First Hospital for their support in patient recruitment and follow-up. The authors would like to thank members in Beijing Key Laboratory of Molecular Diagnosis on Dermatoses for their help in interpreting the results.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by grants from the National Key Research and Development Program of China (No. 2022YFC2504701), National Nature Science Foundation of China (No. 82273003 and No. 82173021), and the Capital Clinical Diagnosis and Treatment Technology Research and Transformation Application Program of China (No. Z211100002921069).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2023.1282996/full#supplementary-material
References
- 1. Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. (2005) 105(10):3768–85. doi: 10.1182/blood-2004-09-3502 [DOI] [PubMed] [Google Scholar]
- 2. Dummer R, Vermeer MH, Scarisbrick JJ, Kim YH, Stonesifer C, Tensen CP, et al. Cutaneous T cell lymphoma. Nat Rev Dis Primers. (2021) 7(1):61. doi: 10.1038/s41572-021-00296-9 [DOI] [PubMed] [Google Scholar]
- 3. Harmon CB, Witzig TE, Katzmann JA, Pittelkow MR. Detection of circulating T cells with CD4+CD7- immunophenotype in patients with benign and Malignant lymphoproliferative dermatoses. J Am Acad Dermatol (1996) 35(3 Pt 1):404–10. doi: 10.1016/S0190-9622(96)90605-2 [DOI] [PubMed] [Google Scholar]
- 4. Jones D, Dang NH, Duvic M, Washington LT, Huh YO. Absence of CD26 expression is a useful marker for diagnosis of T-cell lymphoma in peripheral blood. Am J Clin Pathol (2001) 115(6):885–92. doi: 10.1309/U1Y6-J4AG-5M4M-7AYV [DOI] [PubMed] [Google Scholar]
- 5. Dulmage B, Geskin L, Guitart J, Akilov OE. The biomarker landscape in mycosis fungoides and Sézary syndrome. Exp Dermatol (2017) 26(8):668–76. doi: 10.1111/exd.13261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang Y, Wang Y, Yu R, Huang Y, Su M, Xiao C, et al. Molecular markers of early-stage mycosis fungoides. J Invest Dermatol (2012) 132(6):1698–706. doi: 10.1038/jid.2012.13 [DOI] [PubMed] [Google Scholar]
- 7. Schrader AM, Jansen PM, Willemze R. TOX expression in cutaneous T-cell lymphomas: an adjunctive diagnostic marker that is not tumour specific and not restricted to the CD4(+) CD8(-) phenotype. Br J Dermatol (2016) 175(2):382–6. doi: 10.1111/bjd.14508 [DOI] [PubMed] [Google Scholar]
- 8. Bagot M, Moretta A, Sivori S, Biassoni R, Cantoni C, Bottino C, et al. CD4(+) cutaneous T-cell lymphoma cells express the p140-killer cell immunoglobulin-like receptor. Blood. (2001) 97(5):1388–91. doi: 10.1182/blood.V97.5.1388 [DOI] [PubMed] [Google Scholar]
- 9. Bagot M, Porcu P, Marie-Cardine A, Battistella M, William BM, Vermeer M, et al. IPH4102, a first-in-class anti-KIR3DL2 monoclonal antibody, in patients with relapsed or refractory cutaneous T-cell lymphoma: an international, first-in-human, open-label, phase 1 trial. Lancet Oncol (2019) 20(8):1160–70. doi: 10.1016/S1470-2045(19)30320-1 [DOI] [PubMed] [Google Scholar]
- 10. Lambert SA, Jolma A, Campitelli LF, Das PK, Yin Y, Albu M, et al. The human transcription factors. Cell. (2018) 172(4):650–65. doi: 10.1016/j.cell.2018.01.029 [DOI] [PubMed] [Google Scholar]
- 11. Buccitelli C, Selbach M. mRNAs, proteins and the emerging principles of gene expression control. Nat Rev Genet (2020) 21(10):630–44. doi: 10.1038/s41576-020-0258-4 [DOI] [PubMed] [Google Scholar]
- 12. Morgan MP, Finnegan E, Das S. The role of transcription factors in the acquisition of the four latest proposed hallmarks of cancer and corresponding enabling characteristics. Semin Cancer Biol (2022) 86(Pt 3):1203–15. doi: 10.1016/j.semcancer.2022.10.002 [DOI] [PubMed] [Google Scholar]
- 13. Lam EW, Gomes AR. Forkhead box transcription factors in cancer initiation, progression and chemotherapeutic drug response. Front Oncol (2014) 4:305. doi: 10.3389/fonc.2014.00305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schödel J, Grampp S, Maher ER, Moch H, Ratcliffe PJ, Russo P, et al. Hypoxia, hypoxia-inducible transcription factors, and renal cancer. Eur urology. (2016) 69(4):646–57. doi: 10.1016/j.eururo.2015.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Karin M. Nuclear factor-kappaB in cancer development and progression. Nature. (2006) 441(7092):431–6. doi: 10.1038/nature04870 [DOI] [PubMed] [Google Scholar]
- 16. Li ZY, Zhu YX, Chen JR, Chang X, Xie ZZ. The role of KLF transcription factor in the regulation of cancer progression. BioMed Pharmacother. (2023) 162:114661. doi: 10.1016/j.biopha.2023.114661 [DOI] [PubMed] [Google Scholar]
- 17. Kumar P, Mistri TK. Transcription factors in SOX family: Potent regulators for cancer initiation and development in the human body. Semin Cancer Biol (2020) 67(Pt 1):105–13. doi: 10.1016/j.semcancer.2019.06.016 [DOI] [PubMed] [Google Scholar]
- 18. Mao C, Huang C, Hu Z, Qu S. Transcription factor CASZ1 increases an oncogenic transcriptional process in tumorigenesis and progression of glioma cells. MedComm. (2022) 3(4):e182. doi: 10.1002/mco2.182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bushweller JH. Targeting transcription factors in cancer - from undruggable to reality. Nat Rev Cancer. (2019) 19(11):611–24. doi: 10.1038/s41568-019-0196-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Karamouzis MV, Gorgoulis VG, Papavassiliou AG. Transcription factors and neoplasia: vistas in novel drug design. Clin Cancer Res (2002) 8(5):949–61. [PubMed] [Google Scholar]
- 21. Liu X, Jin S, Hu S, Li R, Pan H, Liu Y, et al. Single-cell transcriptomics links Malignant T cells to the tumor immune landscape in cutaneous T cell lymphoma. Nat Commun (2022) 13(1):1158. doi: 10.1038/s41467-022-28799-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wang Y, Su M, Zhou LL, Tu P, Zhang X, Jiang X, et al. Deficiency of SATB1 expression in Sezary cells causes apoptosis resistance by regulating FasL/CD95L transcription. Blood. (2011) 117(14):3826–35. doi: 10.1182/blood-2010-07-294819 [DOI] [PubMed] [Google Scholar]
- 23. Klemke CD, Brenner D, Weiss EM, Schmidt M, Leverkus M, Gülow K, et al. Lack of T-cell receptor-induced signaling is crucial for CD95 ligand up-regulation and protects cutaneous T-cell lymphoma cells from activation-induced cell death. Cancer Res (2009) 69(10):4175–83. doi: 10.1158/0008-5472.CAN-08-4631 [DOI] [PubMed] [Google Scholar]
- 24. Vinson C, Myakishev M, Acharya A, Mir AA, Moll JR, Bonovich M. Classification of human B-ZIP proteins based on dimerization properties. Mol Cell Biol (2002) 22(18):6321–35. doi: 10.1128/MCB.22.18.6321-6335.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shi R, Tang YQ, Miao H. Metabolism in tumor microenvironment: Implications for cancer immunotherapy. MedComm. (2020) 1(1):47–68. doi: 10.1002/mco2.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fang W, Zhou T, Shi H, Yao M, Zhang D, Qian H, et al. Progranulin induces immune escape in breast cancer via up-regulating PD-L1 expression on tumor-associated macrophages (TAMs) and promoting CD8(+) T cell exclusion. J Exp Clin Cancer Res (2021) 40(1):4. doi: 10.1186/s13046-020-01786-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tosi A, Cappellesso R, Dei Tos AP, Rossi V, Aliberti C, Pigozzo J, et al. The immune cell landscape of metastatic uveal melanoma correlates with overall survival. J Exp Clin Cancer Res (2021) 40(1):154. doi: 10.1186/s13046-021-01947-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rindler K, Jonak C, Alkon N, Thaler FM, Kurz H, Shaw LE, et al. Single-cell RNA sequencing reveals markers of disease progression in primary cutaneous T-cell lymphoma. Mol Cancer (2021) 20(1):124. doi: 10.1186/s12943-021-01419-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Liu F, Gao Y, Xu B, Xiong S, Yi S, Sun J, et al. PEG10 amplification at 7q21.3 potentiates large-cell transformation in cutaneous T-cell lymphoma. Blood (2022) 139(4):554–71. doi: 10.1182/blood.2021012091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Campbell BA, Scarisbrick JJ, Kim YH, Wilcox RA, McCormack C, Prince HM. Time to next treatment as a meaningful endpoint for trials of primary cutaneous lymphoma. Cancers. (2020) 12(8):2311. doi: 10.3390/cancers12082311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Juliana CA, Yang J, Rozo AV, Good A, Groff DN, Wang SZ, et al. ATF5 regulates beta-cell survival during stress. Proc Natl Acad Sci U S A. (2017) 114(6):1341–6. doi: 10.1073/pnas.1620705114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wang YT, Lim Y, McCall MN, Huang KT, Haynes CM, Nehrke K, et al. Cardioprotection by the mitochondrial unfolded protein response requires ATF5. Am J Physiol Heart Circulatory Physiol (2019) 317(2):H472–H8. doi: 10.1152/ajpheart.00244.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Torres-Peraza JF, Engel T, Martín-Ibáñez R, Sanz-Rodríguez A, Fernández-Fernández MR, Esgleas M, et al. Protective neuronal induction of ATF5 in endoplasmic reticulum stress induced by status epilepticus. Brain (2013) 136(Pt 4):1161–76. doi: 10.1093/brain/awt044 [DOI] [PubMed] [Google Scholar]
- 34. Troutman TD, Hu W, Fulenchek S, Yamazaki T, Kurosaki T, Bazan JF, et al. Role for B-cell adapter for PI3K (BCAP) as a signaling adapter linking Toll-like receptors (TLRs) to serine/threonine kinases PI3K/Akt. Proc Natl Acad Sci U S A. (2012) 109(1):273–8. doi: 10.1073/pnas.1118579109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Singh MD, Ni M, Sullivan JM, Hamerman JA, Campbell DJ. B cell adaptor for PI3-kinase (BCAP) modulates CD8(+) effector and memory T cell differentiation. J Exp Med (2018) 215(9):2429–43. doi: 10.1084/jem.20171820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Deason K, Troutman TD, Jain A, Challa DK, Mandraju R, Brewer T, et al. BCAP links IL-1R to the PI3K-mTOR pathway and regulates pathogenic Th17 cell differentiation. J Exp Med (2018) 215(9):2413–28. doi: 10.1084/jem.20171810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Peng Y, Wang Y, Zhou C, Mei W, Zeng C. PI3K/akt/mTOR pathway and its role in cancer therapeutics: are we making headway? Front Oncol (2022) 12:819128. doi: 10.3389/fonc.2022.819128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hua H, Kong Q, Zhang H, Wang J, Luo T, Jiang Y. Targeting mTOR for cancer therapy. J Hematol Oncol (2019) 12(1):71. doi: 10.1186/s13045-019-0754-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cristofoletti C, Bresin A, Picozza M, Picchio MC, Monzo F, Helmer Citterich M, et al. Blood and skin-derived Sezary cells: differences in proliferation-index, activation of PI3K/AKT/mTORC1 pathway and its prognostic relevance. Leukemia. (2019) 33(5):1231–42. doi: 10.1038/s41375-018-0305-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hai TW, Liu F, Coukos WJ, Green MR. Transcription factor ATF cDNA clones: an extensive family of leucine zipper proteins able to selectively form DNA-binding heterodimers. Genes Dev (1989) 3(12b):2083–90. doi: 10.1101/gad.3.12b.2083 [DOI] [PubMed] [Google Scholar]
- 41. Zoncu R, Efeyan A, Sabatini DM. mTOR: from growth signal integration to cancer, diabetes and ageing. Nat Rev Mol Cell Biol (2011) 12(1):21–35. doi: 10.1038/nrm3025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Saxton RA, Sabatini DM. mTOR signaling in growth, metabolism, and disease. Cell. (2017) 168(6):960–76. doi: 10.1016/j.cell.2017.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Düvel K, Yecies JL, Menon S, Raman P, Lipovsky AI, Souza AL, et al. Activation of a metabolic gene regulatory network downstream of mTOR complex 1. Mol Cell (2010) 39(2):171–83. doi: 10.1016/j.molcel.2010.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Marzec M, Liu X, Kasprzycka M, Witkiewicz A, Raghunath PN, El-Salem M, et al. IL-2- and IL-15-induced activation of the rapamycin-sensitive mTORC1 pathway in Malignant CD4+ T lymphocytes. Blood. (2008) 111(4):2181–9. doi: 10.1182/blood-2007-06-095182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bobrowicz M, Slusarczyk A, Domagala J, Dwojak M, Ignatova D, Chang YT, et al. Selective inhibition of HDAC6 sensitizes cutaneous T-cell lymphoma to PI3K inhibitors. Oncol Lett (2020) 20(1):533–40. doi: 10.3892/ol.2020.11587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Nakai S, Kiyohara E, Watanabe R. Malignant and benign T cells constituting cutaneous T-cell lymphoma. Int J Mol Sci (2021) 22(23):12933. doi: 10.3390/ijms222312933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chen Z, Gao X, Yu D. Longevity of vaccine protection: Immunological mechanism, assessment methods, and improving strategy. VIEW. (2022) 3(1):20200103. doi: 10.1002/VIW.20200103 [DOI] [Google Scholar]
- 48. Fan Q, Dai H, Bai J, Xu J, Ma Q, Fei Z, et al. Degradation-resistant implanted biomaterials establish an immunosuppressive microenvironment that induces T cell exhaustion by recruiting myeloid cells. Fundam Res (2022) 2(4):648–58. doi: 10.1016/j.fmre.2021.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Willerslev-Olsen A, Krejsgaard T, Lindahl LM, Litvinov IV, Fredholm S, Petersen DL, et al. Staphylococcal enterotoxin A (SEA) stimulates STAT3 activation and IL-17 expression in cutaneous T-cell lymphoma. Blood. (2016) 127(10):1287–96. doi: 10.1182/blood-2015-08-662353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Vieyra-Garcia PA, Wei T, Naym DG, Fredholm S, Fink-Puches R, Cerroni L, et al. STAT3/5-dependent IL9 overexpression contributes to neoplastic cell survival in mycosis fungoides. Clin Cancer Res (2016) 22(13):3328–39. doi: 10.1158/1078-0432.CCR-15-1784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kopp KL, Ralfkiaer U, Gjerdrum LM, Helvad R, Pedersen IH, Litman T, et al. STAT5-mediated expression of oncogenic miR-155 in cutaneous T-cell lymphoma. Cell Cycle (2013) 12(12):1939–47. doi: 10.4161/cc.24987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Vowels BR, Cassin M, Vonderheid EC, Rook AH. Aberrant cytokine production by Sezary syndrome patients: cytokine secretion pattern resembles murine Th2 cells. J Invest Dermatol (1992) 99(1):90–4. doi: 10.1111/1523-1747.ep12611877 [DOI] [PubMed] [Google Scholar]
- 53. Vowels BR, Lessin SR, Cassin M, Jaworsky C, Benoit B, Wolfe JT, et al. Th2 cytokine mRNA expression in skin in cutaneous T-cell lymphoma. J Invest Dermatol (1994) 103(5):669–73. doi: 10.1111/1523-1747.ep12398454 [DOI] [PubMed] [Google Scholar]
- 54. Persengiev SP, Devireddy LR, Green MR. Inhibition of apoptosis by ATFx: a novel role for a member of the ATF/CREB family of mammalian bZIP transcription factors. Genes Dev (2002) 16(14):1806–14. doi: 10.1101/gad.992202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hai T, Hartman MG. The molecular biology and nomenclature of the activating transcription factor/cAMP responsive element binding family of transcription factors: activating transcription factor proteins and homeostasis. Gene. (2001) 273(1):1–11. doi: 10.1016/S0378-1119(01)00551-0 [DOI] [PubMed] [Google Scholar]
- 56. Persengiev SP, Green MR. The role of ATF/CREB family members in cell growth, survival and apoptosis. Apoptosis an Int J programmed Cell death. (2003) 8(3):225–8. doi: 10.1023/A:1023633704132 [DOI] [PubMed] [Google Scholar]
- 57. Mittal AK, Hegde GV, Aoun P, Bociek RG, Dave BJ, Joshi AD, et al. Molecular basis of aggressive disease in chronic lymphocytic leukemia patients with 11q deletion and trisomy 12 chromosomal abnormalities. Int J Mol Med (2007) 20(4):461–9. doi: 10.3892/ijmm.20.4.461 [DOI] [PubMed] [Google Scholar]
- 58. Bisikirska B, Bansal M, Shen Y, Teruya-Feldstein J, Chaganti R, Califano A. Elucidation and pharmacological targeting of novel molecular drivers of follicular lymphoma progression. Cancer Res (2016) 76(3):664–74. doi: 10.1158/0008-5472.CAN-15-0828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Rousseau J, Gagné V, Labuda M, Beaubois C, Sinnett D, Laverdière C, et al. ATF5 polymorphisms influence ATF function and response to treatment in children with childhood acute lymphoblastic leukemia. Blood. (2011) 118(22):5883–90. doi: 10.1182/blood-2011-05-355560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sheng Z, Li L, Zhu LJ, Smith TW, Demers A, Ross AH, et al. A genome-wide RNA interference screen reveals an essential CREB3L2-ATF5-MCL1 survival pathway in Malignant glioma with therapeutic implications. Nat Med (2010) 16(6):671–7. doi: 10.1038/nm.2158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Dluzen D, Li G, Tacelosky D, Moreau M, Liu DX. BCL-2 is a downstream target of ATF5 that mediates the prosurvival function of ATF5 in a cell type-dependent manner. J Biol Chem (2011) 286(9):7705–13. doi: 10.1074/jbc.M110.207639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Liu DX, Qian D, Wang B, Yang JM, Lu Z. p300-Dependent ATF5 acetylation is essential for Egr-1 gene activation and cell proliferation and survival. Mol Cell Biol (2011) 31(18):3906–16. doi: 10.1128/MCB.05887-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Nukuda A, Endoh H, Yasuda M, Mizutani T, Kawabata K, Haga H. Role of ATF5 in the invasive potential of diverse human cancer cell lines. Biochem Biophys Res Commun (2016) 474(3):509–14. doi: 10.1016/j.bbrc.2016.04.131 [DOI] [PubMed] [Google Scholar]
- 64. Horwitz SM, Koch R, Porcu P, Oki Y, Moskowitz A, Perez M, et al. Activity of the PI3K-δ,γ inhibitor duvelisib in a phase 1 trial and preclinical models of T-cell lymphoma. Blood. (2018) 131(8):888–98. doi: 10.1182/blood-2017-08-802470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Huen A, Haverkos BM, Zain J, Radhakrishnan R, Lechowicz MJ, Devata S, et al. Phase I/ib study of tenalisib (RP6530), a dual PI3K δ/γ Inhibitor in patients with relapsed/refractory T-cell lymphoma. Cancers (2020) 12(8):2293. doi: 10.3390/cancers12082293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Bresin A, Cristofoletti C, Caprini E, Cantonetti M, Monopoli A, Russo G, et al. Preclinical evidence for targeting PI3K/mTOR signaling with dual-inhibitors as a therapeutic strategy against cutaneous T-cell lymphoma. J Invest Dermatol (2020) 140(5):1045–53.e6. doi: 10.1016/j.jid.2019.08.454 [DOI] [PubMed] [Google Scholar]
- 67. Kittipongdaja W, Wu X, Garner J, Liu X, Komas SM, Hwang ST, et al. Rapamycin suppresses tumor growth and alters the metabolic phenotype in T-cell lymphoma. J Invest Dermatol (2015) 135(9):2301–8. doi: 10.1038/jid.2015.153 [DOI] [PubMed] [Google Scholar]
- 68. Nguyen CN, Iyer SP, Duvic M, Barde PJ, Nair A, Routhu KV, et al. Complete Response to tenalisib and romidepsin with long-term maintenance using tenalisib monotherapy in a patient with relapsed and refractory sézary syndrome. Invest New Drugs (2023) 41(2):350–5. doi: 10.1007/s10637-022-01315-6 [DOI] [PubMed] [Google Scholar]
- 69. Cosenza M, Civallero M, Fiorcari S, Pozzi S, Marcheselli L, Bari A, et al. The histone deacetylase inhibitor romidepsin synergizes with lenalidomide and enhances tumor cell death in T-cell lymphoma cell lines. Cancer Biol Ther (2016) 17(10):1094–106. doi: 10.1080/15384047.2016.1219820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Yu XX, Zhu MY, Wang JR, Li H, Hu P, Qing YJ, et al. LW-213 induces cell apoptosis in human cutaneous T-cell lymphomas by activating PERK-eIF2α-ATF4-CHOP axis. Acta pharmacologica Sinica. (2021) 42(2):290–300. doi: 10.1038/s41401-020-0466-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Chen X, Cubillos-Ruiz JR. Endoplasmic reticulum stress signals in the tumour and its microenvironment. Nat Rev Cancer. (2021) 21(2):71–88. doi: 10.1038/s41568-020-00312-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Izumi S, Saito A, Kanemoto S, Kawasaki N, Asada R, Iwamoto H, et al. The endoplasmic reticulum stress transducer BBF2H7 suppresses apoptosis by activating the ATF5-MCL1 pathway in growth plate cartilage. J Biol Chem (2012) 287(43):36190–200. doi: 10.1074/jbc.M112.373746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Gorrell L, Makareeva E, Omari S, Otsuru S, Leikin SER. Mitochondria, and ISR Regulation by mt-HSP70 and ATF5 upon Procollagen Misfolding in Osteoblasts. Adv Sci (Weinh). (2022) 9(29):e2201273. doi: 10.1002/advs.202201273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Song S, Chew C, Dale BM, Traum D, Peacock J, Yamazaki T, et al. A requirement for the p85 PI3K adapter protein BCAP in the protection of macrophages from apoptosis induced by endoplasmic reticulum stress. J Immunol (2011) 187(2):619–25. doi: 10.4049/jimmunol.0903425 [DOI] [PubMed] [Google Scholar]
- 75. Li LJ, Chai Y, Guo XJ, Chu SL, Zhang LS. Effects of endoplasmic reticulum stress on autophagy and apoptosis of human leukemia cells via inhibition of the PI3K/AKT/mTOR signaling pathway. Mol Med Rep (2018) 17(6):7886–92. doi: 10.3892/mmr.2018.8840 [DOI] [PubMed] [Google Scholar]
- 76. Yang N, Qu YJ, Cheng Y, Liang T, Zhang MN, Zhang D, et al. Endoplasmic reticulum stress regulates proliferation, migration and invasion of human ovarian cancer SKOV3 cells through PI3K/AKT/mTOR signaling pathway. Cancer Biomarkers section A Dis markers. (2017) 19(3):263–9. doi: 10.3233/CBM-160424 [DOI] [PubMed] [Google Scholar]
- 77. Ozcan U, Ozcan L, Yilmaz E, Düvel K, Sahin M, Manning BD, et al. Loss of the tuberous sclerosis complex tumor suppressors triggers the unfolded protein response to regulate insulin signaling and apoptosis. Mol Cell (2008) 29(5):541–51. doi: 10.1016/j.molcel.2007.12.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Kang YJ, Lu MK, Guan KL. The TSC1 and TSC2 tumor suppressors are required for proper ER stress response and protect cells from ER stress-induced apoptosis. Cell Death differentiation. (2011) 18(1):133–44. doi: 10.1038/cdd.2010.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Mafi S, Ahmadi E, Meehan E, Chiari C, Mansoori B, Sadeghi H, et al. The mTOR signaling pathway interacts with the ER stress response and the unfolded protein response in cancer. Cancer Res (2023) 83(15):2450–60. doi: 10.1158/0008-5472.CAN-22-3032 [DOI] [PubMed] [Google Scholar]
- 80. Schewe DM, Aguirre-Ghiso JA. ATF6alpha-Rheb-mTOR signaling promotes survival of dormant tumor cells in vivo. Proc Natl Acad Sci U.S.A. (2008) 105(30):10519–24. doi: 10.1073/pnas.0800939105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Chen S, Wu J, Jiao K, Wu Q, Ma J, Chen D, et al. MicroRNA-495-3p inhibits multidrug resistance by modulating autophagy through GRP78/mTOR axis in gastric cancer. Cell Death Dis (2018) 9(11):1070. doi: 10.1038/s41419-018-0950-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Watatani Y, Ichikawa K, Nakanishi N, Fujimoto M, Takeda H, Kimura N, et al. Stress-induced translation of ATF5 mRNA is regulated by the 5'-untranslated region. J Biol Chem (2008) 283(5):2543–53. doi: 10.1074/jbc.M707781200 [DOI] [PubMed] [Google Scholar]
- 83. Zhou D, Palam LR, Jiang L, Narasimhan J, Staschke KA, Wek RC. Phosphorylation of eIF2 directs ATF5 translational control in response to diverse stress conditions. J Biol Chem (2008) 283(11):7064–73. doi: 10.1074/jbc.M708530200 [DOI] [PubMed] [Google Scholar]
- 84. Hetz C, Zhang K, Kaufman RJ. Mechanisms, regulation and functions of the unfolded protein response. Nat Rev Mol Cell Biol (2020) 21(8):421–38. doi: 10.1038/s41580-020-0250-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Teske BF, Fusakio ME, Zhou D, Shan J, McClintick JN, Kilberg MS, et al. CHOP induces activating transcription factor 5 (ATF5) to trigger apoptosis in response to perturbations in protein homeostasis. Mol Biol Cell (2013) 24(15):2477–90. doi: 10.1091/mbc.e13-01-0067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Shi R, Wang J, Zhang Z, Leng Y, Chen AF. ASGR1 promotes liver injury in sepsis by modulating monocyte-to-macrophage differentiation via NF-κB/ATF5 pathway. Life Sci (2023) 315:121339. doi: 10.1016/j.lfs.2022.121339 [DOI] [PubMed] [Google Scholar]
- 87. Qu S, Huang C, Zhu T, Wang K, Zhang H, Wang L, et al. OLFML3, as a potential predictor of prognosis and therapeutic target for glioma, is closely related to immune cell infiltration. VIEW. (2023) 4(2):20220052. doi: 10.1002/VIW.20220052 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://doi.org/10.6084/m9.figshare.24151839.v1.