Abstract
Objectives:
To identify sociodemographic and policy environment characteristics of early adopters of retail tobacco control policies in U.S. localities.
Methods:
We interviewed a sample of local tobacco control programs on policy progress for 33 specific policies, along with other program characteristics. We combine these results with secondary data in logistic regression analysis.
Results:
Eighty (82% of 97) county tobacco control programs from 24 states were interviewed. Localities with lower smoking rates (OR: 0.7; 95%: 0.6-0.9) or higher excise taxes (OR: 6.0; 95%: 1.4-26.0) were more likely to have adopted a retail policy by late 2015. Early adopters were less likely to have voted majority Republican in the 2012 election (OR: 0.03; 95%: 0.00-0.34) or to have higher percentages of African American population (OR: 0.9; 95%: 0.8-0.99).
Conclusions:
While localities with more resources, eg, program capacity, political will or policy options, were more likely to adopt policies by 2015, those with higher smoking rates and proportions of priority populations were less likely to do so. As local retail policy work becomes more commonplace, only time will tell if this “rich-get-richer” trend continues, or if the contexts in which retail policies are adopted diversify.
Keywords: point-of-sale; policy (local, state, federal, international); tobacco product; tobacco regulation; tobacco use
INTRODUCTION
Calls to reduce health disparities through place-based strategies are increasing.1,2 For tobacco-related disparities, these calls include regulation of the retail environment.3,4 Many retailers – in many different types of stores – sell tobacco in the U.S. The Food and Drug Administration would need to perform over 1,000 inspections every day to inspect each of the estimated 375,000 tobacco retailers in the U.S. just once each year. Meanwhile, most of the almost $1 million per hour ($966, 872)5,6 that the 5 large U.S. tobacco companies spend on marketing aims to reduce the price of products for consumers in the retail environment. Moreover, this reported total includes retail marketing expenditures for only cigarettes and smokeless tobacco, and excludes unreported expenditures for cigars, cigarillos, e-cigarettes, hookah, and other products. Tobacco companies use advertisements, product placement and price promotions in stores to promote perceptions that tobacco is normative (more popular than it really is), encourage initiation, increase impulse purchases, and deter cessation.7 Strategies also include advertisements and coupons on or in packs and direct-to-consumer coupons, some with location-specific data about users’ proximity to retailers with time-limited offers.8 Spatial inequities in tobacco retailer density,9 market segmentation and micro-targeted marketing10 create or perpetuate tobacco-related disparities, all of which help drive the increased consideration and adoption of local, place-based strategies to regulate the retail environment.
Four categories of policies address interrelated aspects of the retail environment, focusing on place, price, products, and promotion (sometimes called the 4 Ps).11 Place policies regulate where tobacco is sold, eg, restricting tobacco sales to certain types of merchants like tobacconists. Price policies use non-tax approaches to increase product prices, eg, restricting discounts or establishing minimum product pricing. Product policies regulate which products are available, eg, restricting flavored products, and Promotion policies focus on placement and size of advertising and product displays in stores, eg, product display restrictions or countermarketing.
Even as traditional tobacco control policy adoption has stalled (eg, smoke-free air and excise tax),12 retail-focused tobacco regulation is proliferating, both internationally and, to a lesser extent, in the U.S. While 60 countries have completely banned tobacco advertising in the retail environment, others (eg, Australia, New Zealand, U.K.) have partial bans on retail advertising or tobacco product displays.11,13 Some of the bans have “trickled up” from local or other subnational policy passage, as in Scotland and the U.K.14 In the U.S., over 280 cities and other local jurisdictions in addition to the states of Hawaii, California, New Jersey, Oregon, Maine, and Massachusetts have raised minimum legal sales age to 21.15 In 2014, New York City changed the minimum age for tobacco to 21, along with passing “Sensible Tobacco Enforcement”, which limited price discounts, enforced a minimum price, and regulated acceptable packaging; then in 2017 raised the minimum price and capped the number of available retailer licenses among other provisions.16,17 In Minnesota, St. Paul, Brooklyn Center, and Maplewood have implemented price floors on packs of cigarettes.18
Regulatory science about retail policies focuses on retailer compliance to existing laws, such as licensing, youth sales restrictions, and other point-of-sale restrictions.19–22 Another vein of research focuses on public opinion of potential retail policies, like caps on the number of licenses, banning products, increasing minimum sales ages, and others.23–26 Much of the remaining science on retail policy in tobacco control is evaluative and tends to emphasize the impact of regulation on the environment, eg, retailer density reductions,27–31 or the consequences of policies on tobacco use by youth and young adults.14,32–35
Little research exists on the diffusion of local retail policy, leaving a gap in regulatory science. Investigating how and where policies start and spread has been critical to advance traditional tobacco control policies such as tobacco taxes and smoke-free air laws.36–38 Like in many policy domains, for smoke-free air laws, localities learned from the experiences of early adopters.39 As retail policies begin to diffuse across U.S. localities, the goal of this paper is to identify political and sociodemographic characteristics of early adopters to better understand the factors associated with retail policy adoption. 9,40,41
METHODS
This study uses a combination of primary and secondary data to investigate local-level retail policy adoption. The primary data come a larger project, Advancing Science and Policy in the Retail Environment (ASPiRE), funded from the National Cancer Institute’s State and Community Tobacco Control Initiative.42 Our sample of counties was drawn using a probability proportionate to population size (PPS) method from all counties in the contiguous U.S., and served multiple purposes. As is relevant here, we interviewed local tobacco control program managers in the counties, and , through a separate project aim, sampled and surveilled tobacco retailers in each county.43 To accomplish these aims, a sample size of 100 counties (out of 3,142 total) was drawn initially, leaving 97 after removing duplicates, and 26% of the 2012 U.S. population resided in these counties.44
We conducted structured interviews via telephone with county or city tobacco control staff from July through October 2015. Respondents were identified as local tobacco control program managers by the Centers for Disease Control and Prevention (CDC) Office on Smoking and Health. Interviews lasted for approximately one hour, during which we asked whether the county or any of its constituent governments had adopted retail policies, from a list of 33 possible policies. The 33 policies included an array of approaches such as those aiming to reduce tobacco retailer density, increase prices through non-tax approaches, raise the minimum legal sales age for tobacco, and regulate e-cigarette sales. Appendix A contains a list of the 33 policies along with the number of localities reporting having adopted each. We also asked program managers about perceived barriers and useful resources for pursuing retail tobacco control strategies. More information on the specific policies and study are available elsewhere.45
The primary outcome is whether any jurisdiction in the county had adopted any local retail policies at the time of the interview. This does not include any policies implemented by the state, only those that go beyond state-level laws. We combined the responses to 33 individual policies (Appendix A) into one variable with 2 categories, where 0 = no retail tobacco policies adopted and 1 = at least one local retail policy adopted by late 2015.
Policy & program environment
We also asked whether tobacco-related store assessments had ever been performed within the county. Retail marketing surveillance – in-person visits to stores to record prices and advertising characteristics – is performed in states and localities on an ongoing basis or as part of specific tobacco control awareness or policy campaigns. 46 With participation of state/local tobacco control programs, non-governmental organization, public health attorneys and the Centers for Disease Control, the Standardized Tobacco Assessment for Retail Settings (STARS) was developed and released in 2014.46 The instrument was quickly adopted by many states and localities to ease data collection and neighborhood comparisons.42,46 In our interviews, respondents chose from 4 possible answers for whether store assessments had ever been performed: no assessments performed, assessments performed with STARS, assessments performed via another instrument, or assessments performed using multiple instruments. This variable was collapsed into 2 categories (0 = no store assessments, or 1 = store assessments performed). The third variable from the interviews represents tobacco control program capacity. We asked program managers about barriers to retail tobacco policy work for their program, and collapsed answers referring to inadequate funding or insufficient numbers of staff into limited program capacity. This variable is also coded into one of 2 categories: 0 = capacity is sufficient, and 1 = capacity is limited for retail tobacco policy.
Other measures included for the policy context as potential correlates of retail policy status are excise taxes, state preemption of local regulation of retail licensing and smoke-free air, and majority party vote in 2012. We weighted cigarette excise taxes by population in counties wherein individual cities had local taxes (data from the American Lung Association and various municipal websites), and added these to current state and federal rates.47 We include 2 variables for state preemptions on local tobacco retailer licensing and of smoke-free air ordinances to control for the various types of state-level tobacco-related preemptions of local policymaking. For these 2 variables, counties were coded as 0 = not preempted by the state, and 1 = preempted. Finally tobacco industry objections to local policy restrictions are often framed as anti-business,40 and previous work has found that Republican-led states have lower excise taxes than their Democratic counterparts.48 Accordingly, we account for the majority party ideology of localities. Counties where the Democratic Party’s presidential candidate garnered more than 50% of the vote in 2012 were coded Democrat and others were coded Republican.49
Demography
We included demographic indicators for the counties, to control for historically underserved low-income and African-American populations. The variables, median household income (MHHI) and percentage of population that was non-Hispanic African American, were collected from the U.S. Census44 and MHHI was recoded into units of $10,000s for scale. We also include adult smoking prevalence obtained from the County Health Rankings and Roadmap Data, which uses data originating from the BRFSS.50
Multivariable logistic regression was used to assess variables related to early adoption, and analyses were performed in R (version 3.4.2) and RStudio (version 1.1.383).
RESULTS
Out of the 97 counties selected, 80 counties (82%) from 24 states completed interviews. Respondent counties were home to 24% of the US population versus 26% in the entire sample, and no significant differences were found between respondent and the 17 non-responding counties in terms of size or region, or from particular states (eg, counties in Connecticut, Texas, Ohio, and Kansas were among non-responders). Forty of the 80 counties (50%) reported adopting at least one retail tobacco policy by late 2015. Nearly half (46%) of local tobacco control programs reported limited capacity, although nearly two-thirds (64%) had assessed retail tobacco marketing in stores at least once. Regarding tobacco control policies, 45% had a licensing preemption, 46% had a smoke-free air law preemption, and excise taxes ranged from $1.12 to $6.62 (mean = $2.67). Sixty-six percent of the counties were Democratic, percentage of African Americans in the population ranged from 0.3 to 57.3% (mean = 11.87%), the lowest median household income for counties was 26,668 and the highest was $109,383 (mean = $57,411), and adult smoking prevalence in 2012 ranged from 7.4% to 28.5% (mean = 17.8%).
Table 1 compares summary statistics for early adopters and others. On average, smoking rates and African-American population proportions were lower for early adopters, and levels of income and cigarette excise taxes were higher in counties that were early adopters. The majority of early adopters were not subject to either type of preemption (retailer licensing or smoke-free air). A higher percentage of Democratic counties adopted policies than Republican majority ones. Early adopters also included larger percentages of counties that did not report limited capacity as well as those that conducted store assessments, compared to the other counties.
Table 1.
Characteristics of counties by policy adoption.
| Indicator | Adopted policy | Did not adopt policy |
|---|---|---|
|
| ||
| Group mean | Group mean | |
|
|
||
| Demography | ||
| Adult smoking rate | 15.8% | 19.7% |
| African-American pop. | 9.5% | 14.3% |
| Median household income | $62,317 | $52,511 |
| Policy & program context | ||
| Excise tax (weighted) | $3.04 | $2.30 |
| Percentage of group | Percentage of group | |
|
|
||
| Local retailer licensing | ||
| Not preempted | 55.7% | 44.3% |
| Preempted | 31.6% | 68.4% |
| Local smoke-free air | ||
| Not preempted | 54.8% | 45.2% |
| Preempted | 33.3% | 66.7% |
| Party majority | ||
| Democratic | 65.2% | 34.8% |
| Republican | 29.4% | 70.6% |
| Program capacity | ||
| Sufficient | 53.8% | 46.2% |
| Limited | 33.3% | 66.7% |
| Store assessments | ||
| Conducted | 64.3% | 35.7% |
| Not conducted | 34.2% | 65.8% |
Note: from a sample of 80 U.S. Counties, late 2015.
Table 2 shows the results of a logistic regression model of whether a county or any of its constituent cities had adopted at least one retail policy by 2015. All else equal, as county smoking rates or the percentage of African American in the population increase, the probability of policy adoption decreased. A dollar increase in excise tax for the typical county predicted a six-fold increase in the likelihood of policy adoption, but localities that were preempted from enacting retailer licensing or smoke-free air were much less likely to adopt a policy than their non-preempted counterparts (143:1 and 12:1), and Republican majority counties were also less likely than Democratic ones (33:1) to adopt a policy. Counties with limited local program capacity were less likely (48:1) than others, but those that had previously performed retail tobacco assessments were over 6 times as likely to adopt policies than those who had not. Controlling for all these phenomena, median income was not related to adoption. Though some of the odds ratios are extreme, perhaps due to a relatively small sample size, there were no issues with model convergence, and we performed diagnostics for potential multicollinearity, linearity of the predictors with predictions and influential observations, all of which were acceptable.
Table 2.
Relationship of retail policy adoption to tobacco use, sociodemographic, policy context, and program characteristics.
| Predictor | Odds ratio | 95% CI |
|---|---|---|
| Demography | ||
| Adult smoking rate (%) | 0.707 | [0.551; 0.908] |
| African American pop. (%) | 0.917 | [0.843; 0.996] |
| Median household income ($10,000s) | 0.647 | [0.328; 1.277] |
| Policy & program context | ||
| Excise tax, weighted ($) | 5.977 | [1.383; 25.826] |
| Licensing preemption: Yes | 0.007 | [0.000; 0.146] |
| Smoke-free air preemption: Yes | 0.081 | [0.009; 0.714] |
| Majority Party 2012: Republican | 0.030 | [0.003; 0.341] |
| Limited program capacity: Yes | 0.021 | [0.002; 0.295] |
| Performed store assessments: Yes | 6.667 | [1.113; 39.931] |
|
| ||
| Log-likelihood (df = 10) | −23.728 | |
| Observations correctly predicted (%) | 81.250 | |
| Observations | 80 | |
Notes: Odds ratio estimates and intervals that did not include 1.0 are in bold. Odds ratios for binary variables (the bottom 5 variables) indicate the predicted difference in the odds of policy adoption for the absence of the condition vs its presence. For example, localities with tobacco retailer licensing preemptions in place were 143 times less likely (1/0.007) than those without licensing preemptions to adopt a policy, while localities that had performed store assessments were over 6 times more likely (6.667/1) to adopt a policy than those who had not. The odds ratios for smoking rate and African American population indicate the predicted difference or increase in odds when either percentage increases by one; the odds ratio for weighted excise tax is for a difference or increase of one dollar; odds ratio for median household income if for a difference or increase of $10,000.
All the panels in Figure 1 show how the probability of having a policy changes in 2 typical counties: one Democrat and one Republican. The top row shows the predicted probability of retail policy adoption across the ranges of adult smoking rates, African American population proportions, and cigarette excise tax levels (with all other variables held at their mean or modal value, as appropriate). Since the confidence intervals overlap and this does not always indicate whether there is an actual, ie, statistically significant, difference, the panels in the bottom row show the difference in predicted probability between Democrat and Republican counties. When 2012 smoking rates were low, the chances of having adopted a policy by 2015 were quite high. However, as smoking rates increased, there was markedly less certainty– coupled with decreased probability– of retail policy adoption. Results indicate much the same trend for African American population. Policy probability in 2015 was high for localities with smaller 2012 African American population proportions, but as these increased the odds of retail policy adoption became both less and less clear. The opposite is true for cigarette excise taxes. When these taxes were low in 2012, policy probability was also relatively lower, but as taxes increased above $3.50 or so, chances of policy adoption by 2015 were higher and also more certain.
Figure 1:
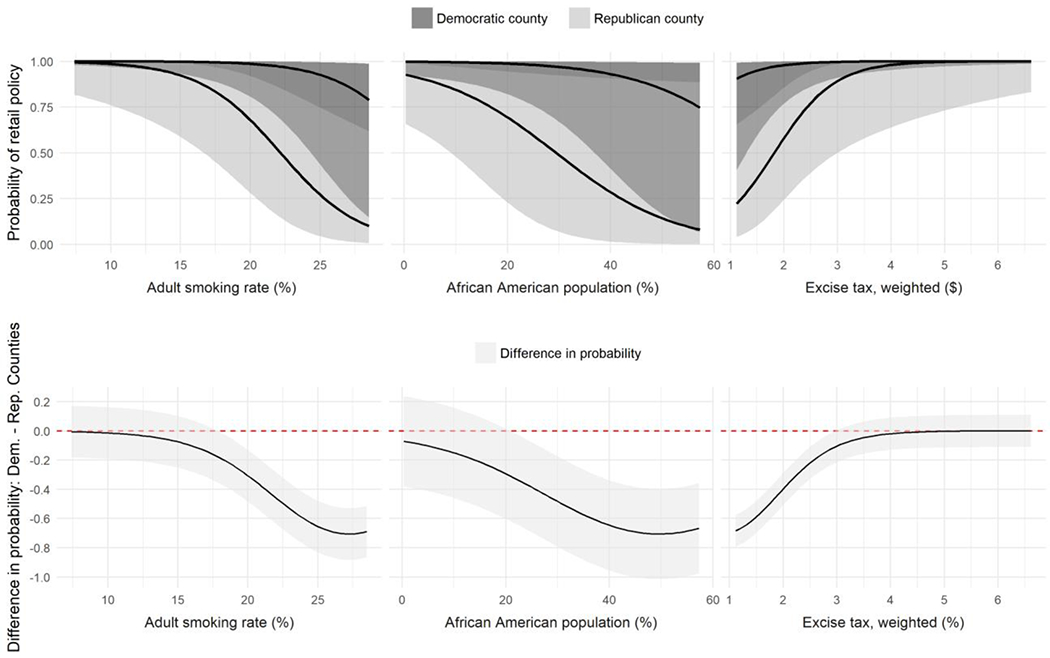
The top row of graphs shows the probabilities of policy adoption across ranges of smoking rates, African American population and excise taxes. The bottom row shows the differences in predicted probability of policy adoption for each between Democrat and Republican counties. Shading indicates 95% confidence intervals.
Turning to local tobacco control preemptions and program characteristics, Figure 2 shows the probability of retail policy adoption for the same 2 types of typical counties. Localities without preemption of licensing or smoke-free air ordinances had higher chances of having adopted a policy by 2015 than their preempted counterparts. Counties with programs not reporting limited capacity (ie, those with adequate capacity) had markedly better probability of policy adoption. Finally, localities in which store audits had been conducted also saw a higher chance of having adopted a retail tobacco policy by late 2015 than those that had not assessed stores.
Figure 2:
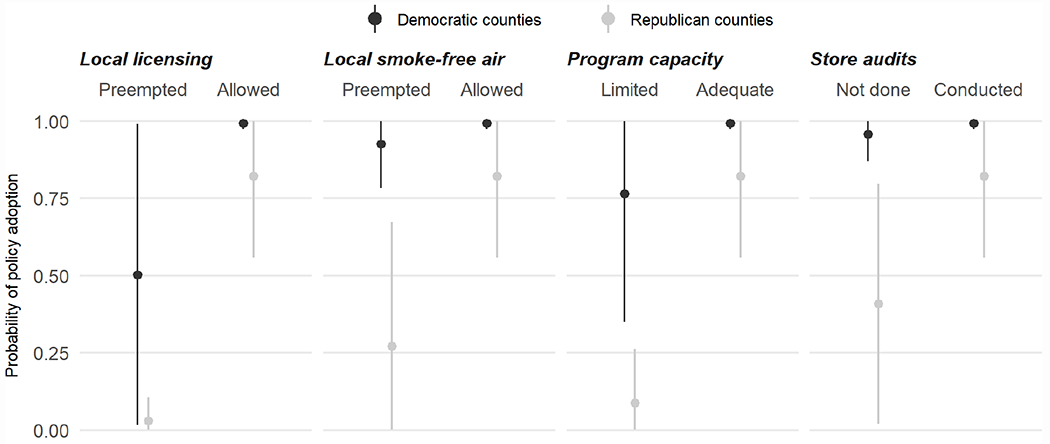
Comparing the probabilities of retail policy adoption by smoke-free and licensing preemption status and program characteristics. Lines represent 95% confidence intervals.
DISCUSSION
In the absence of federal and often times state restrictions on the retail environment, local jurisdictions are increasingly adopting retail tobacco control policies to counter the tobacco industry’s pervasive influence at the point of sale. In our sample of 80 U.S. counties, half of them had adopted at least one retail tobacco control policy by late 2015. These counties are diverse in income and race, as well as in tobacco control program capacity, preemption environment and political party alignment.
We found that the probability of adopting a retail tobacco policy was much greater in counties with lower smoking rates and higher excise taxes, suggesting that localities where tobacco control efforts have been successful may have an advantage in pursuing retail tobacco policies. Conversely, localities with higher smoking rates, lower excise taxes, and higher proportions of priority populations were much less likely to have adopted a retail policy; however, these communities stand to benefit more from policies aimed at reducing the omnipresence of tobacco products, since traditional tobacco control efforts have been less successful. As retail policy work becomes more commonplace at the local level, only time will tell if this “rich-get-richer” trend continues, or if the contexts in which retail policies are adopted diversify. .
Many of the findings here can be conceptualized in terms of resources. Localities with greater access to resources, eg, human and financial ones, along with more political will or policy options, are also more successful in efforts or at least more likely to adopt retail tobacco policies. State preemption takes away potential resources and options for local tobacco control programs. In our sample, those preempted from establishing local retailer licensing requirements have among the lowest likelihoods of adopting any retail policy. Licensing is the cornerstone of retail tobacco policy, as licensing requirements, among other benefits, help tobacco control programs and partners 1) know where tobacco retailers are located, 2) perform routine store surveillance to know what types of products, promotions, and marketing are most prevalent in each neighborhood, and 3) pay for and facilitate enforcement of other local retail policies. In this way, preemption in one area may have implications well beyond that area or be associated with a decreased likelihood of pursuing any local tobacco control strategy. Similarly, programs situated in Republican-leaning jurisdictions may face a relative scarcity of one of the most important resources – political will for tobacco control initiatives – as compared to Democratic.
Data generated from performing store assessments serve as a resource for tobacco control programs to learn about neighborhood differences and to build awareness among stakeholders and policymakers. Assessments are noticeably associated with enhanced likelihood of adopting retail policies. Consistent with the belief that “all politics are local”, routine assessments of the retail environment provide stakeholders and policy makers with evidence to inform arguments for context-specific policy solutions to retail tobacco problems. The organization and execution of community-wide or even cross-neighborhood store assessments also rely on access to resources: a strong tobacco control program and partnerships. Under-resourced programs –those with limited funding or staff – are also markedly less likely to adopt retail policies than their counterparts with sufficient capacity.
One caveat to our findings may be that just 80 counties were included, even though the current data from interviews with tobacco control programs about retail policies represents the largest-to-date sample of U.S. counties. Future work can replicate and explore these results through different samples of counties or other jurisdictional levels in studies that focus on place and context in retail tobacco control policy. These studies might also 1) test causality between contextual factors and retail policy adoption, which is difficult with a relatively small sample of 80 counties, 2) help to fill potential gaps here, such as the absence of available data about level of CDC-recommended tobacco control expenditures locally, and 3) gauge whether our findings for early adopters hold true as retail tobacco policy adoption rates and policy environments change.
IMPLICATIONS FOR TOBACCO REGULATION
The current U.S. Surgeon General , VADM Jerome M. Adams, has pledged to “facilitate locally led solutions to the nation’s most difficult health problems.”51 The importance of place is evident in this pledge. The current study identifies which specific local characteristics are associated with adoption of place-based local policies that regulate the retail environment for tobacco, which is the leading cause of preventable death in the U.S.52 For decades, tobacco regulation for states and localities concentrated mainly on smoke-free air laws and excise taxes. After earlier successes in these policy domains in many localities, and the Family Smoking Prevention and Control Act of 2009, which preserved and reiterated the authority of states and localities, retail-focused tobacco control strategies garner a growing proportion of local tobacco policy work. These policies aim not only to decrease initiation and to increase cessation, but also to attenuate disparities across neighborhoods and communities by focusing at the local level. Our findings that policy adoption was less likely among localities with higher smoking rates, higher proportions of African Americans, or less-resourced tobacco control programs suggest that geographic- and population-based disparities in use may worsen and the fiscal consequences of tobacco-related illness may be prolonged if these trends continue. While these strategies are relatively new to tobacco control and evidence of their efficacy continues to build, it is important not only to consider context in assessments of their impact, but also in the feasibility of their application.
Acknowledgments
Funding for data collected in this study was provided by grant number U01 CA154281, the National Cancer Institute’s State and Community Tobacco Control Initiative. One researcher was also supported by National Cancer Institute grant 5R01-CA067850. The funders had no involvement in the study design, collection, analysis, writing or interpretation.
APPENDIX A:
Policies and number of localities reporting adoption.
| Policy | Localities* |
|---|---|
|
Place: policies that regulate where tobacco products are sold |
|
|
| |
| Cap the number of retailer licenses available in an area | 6 |
| Establish and increase retailer licensing fees | 25 |
| Establish retailer licensing for ENDS | 17 |
| Establish zoning laws to restrict where tobacco retailers can be located | 3 |
| Restrict retailer-to-retailer proximity | 4 |
| Restrict sales around youth locales | 10 |
| Restrict the types of retailers allowed to sell ENDS | 8 |
| Restrict the types of retailers allowed to sell tobacco products | 5 |
|
Price: policies that increase prices of tobacco products |
|
|
| |
| Establish minimum pack sizes for OTPs | 4 |
| Establish minimum price laws | 1 |
| Establish mitigation fee | 0 |
| Establish sunshine laws | 0 |
| Establish taxes on ENDS | 0 |
| Restrict coupon distribution | 4 |
| Restrict coupon redemption | 3 |
| Restrict discounts | 2 |
|
Product Availability: policies that regulate which products are available and to whom |
|
|
| |
| Establish or raise the minimum legal sales age for ENDS | 11 |
| Raise the minimum legal sales age for tobacco products | 6 |
| Restrict the sales of flavored products | 5 |
| Restrict times for sales | 0 |
|
Promotion: policies that focus on placement and size of advertising and product displays |
|
|
| |
| Establish content-neutral advertising limits | 10 |
| Limit the number of products displayed | 0 |
| Limit the times products can be displayed | 0 |
| Mandate graphic warnings at the point of sale | 0 |
| Mandate posting of quit line information at point of sale | 0 |
| Prohibit displays of products | 0 |
| Prohibit self-service access to ENDS | 14 |
| Prohibit self-service access to OTPs | 16 |
| Restrict advertising by location | 5 |
| Restrict indoor advertising sizes or placement | 2 |
| Restrict manner of advertising | 0 |
| Restrict outdoor advertising | 0 |
| Restrict times advertising can be displayed | 0 |
County tobacco control programs out of 80 responding that reported policy adoption (county or city)
Footnotes
Human Subjects Statement
Primary data collection through semi-structured interviews with tobacco control program managers for data used in this manuscript was declared EXEMPT for human subjects research by the Institutional Review Board and Human Research Protection Office at Washington University in St. Louis on September 21, 2015. Document ID # 201109159
Conflict Of Interest Statement
All authors have no conflicts of interest to declare.
Contributor Information
Todd B. Combs, Washington University in St. Louis, George Warren Brown School of Social Work, Center for Public Health Systems Science, St. Louis, MO.
Deena Brosi, Washington University in St. Louis, George Warren Brown School of Social Work, Center for Public Health Systems Science, St. Louis, MO.
Veronica Chaitan, Washington University in St. Louis, George Warren Brown School of Social Work, Center for Public Health Systems Science, St. Louis, MO.
Eda He, Washington University in St. Louis, George Warren Brown School of Social Work, Center for Public Health Systems Science, St. Louis, MO.
Douglas A. Luke, Washington University in St. Louis, George Warren Brown School of Social Work, Center for Public Health Systems Science, St. Louis, MO.
Lisa A. Henriksen, Stanford University, Medicine, Stanford Prevention Research Center, Stanford, CA.
References
- 1.Dankwa-Mullan I, Pérez-Stable EJ. Addressing Health Disparities Is a Place-Based Issue. Am J Public Health. 2016;106(4):637–639. doi: 10.2105/AJPH.2016.303077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scribner RA, Simonsen NR, Leonardi C. The Social Determinants of Health Core: Taking a Place-Based Approach. Am J Prev Med. 2017;52(1):S13–S19. doi: 10.1016/j.amepre.2016.09.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koh H Place Matters for Tobacco Control. JAMA. 2016;316(7):700–701. doi: 10.1001/jama.2016.10537 [DOI] [PubMed] [Google Scholar]
- 4.Mukherjea A, Green LW. Tobacco and Behavior Change. In: Kahan S, Gielen AC, Fagan PJ, Green LW, eds. Health Behavior Change in Populations. Baltimore: Johns Hopkins University Press; 2014:153–187. [Google Scholar]
- 5.Federal Trade Commission. Federal Trade Commission Cigarette Report for 2015.; 2017:34. https://www.ftc.gov/system/files/documents/reports/federal-trade-commission-cigarette-report-2015-federal-trade-commission-smokeless-tobacco-report/2015_cigarette_report.pdf. Accessed January 19, 2018.
- 6.Federal Trade Commission. Federal Trade Commission Smokeless Tobacco Report for 2015.; 2017:37. https://www.ftc.gov/system/files/documents/reports/federal-trade-commission-cigarette-report-2015-federal-trade-commission-smokeless-tobacco-report/2015_smokeless_tobacco_report.pdf. Accessed January 19, 2018.
- 7.Paynter J, Edwards R. The impact of tobacco promotion at the point of sale: a systematic review. Nicotine Tob Res Off J Soc Res Nicotine Tob. 2009;11(1):25–35. doi: 10.1093/ntr/ntn002 [DOI] [PubMed] [Google Scholar]
- 8.Seidenberg AB, Jo CL. Cigarette couponing goes mobile. Tob Control. 2017;26(2):233–234. doi: 10.1136/tobaccocontrol-2016-052996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ribisl KM, Luke DA, Henriksen L. The case for a concerted push to reduce place-based disparities in smoking-related cancers. JAMA Intern Med. 2016;176(12):1799–1800. doi: 10.1001/jamainternmed.2016.6865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JGL, Henriksen L, Rose SW, Moreland-Russell S, Ribisl KM. A Systematic Review of Neighborhood Disparities in Point-of-Sale Tobacco Marketing. Am J Public Health. 2015;105(9):e8–e18. doi: 10.2105/AJPH.2015.302777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Henriksen L Comprehensive tobacco marketing restrictions: promotion, packaging, price and place. Tob Control. 2012;21(2):147–153. doi: 10.1136/tobaccocontrol-2011-050416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holmes CB, King BA, Babb SD. Stuck in Neutral: Stalled Progress in Statewide Comprehensive Smoke-Free Laws and Cigarette Excise Taxes, United States, 2000–2014. Prev Chronic Dis. 2016;13. doi: 10.5888/pcd13.150409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO Framework Convention on Tobacco Control Secretariat. Best Practices on Implementation of the Tobacco Advertising and Display Ban at Point of Sale (Article 13 of the WHO FCTC); A Four-Country Study: Ireland, Norway, Finland and the United Kingdom. http://www.who.int/fctc/publications/best_practices_art13_whofctc.pdf. Accessed January 23, 2018.
- 14.Haw S, Amos A, Eadie D, et al. Determining the impact of smoking point of sale legislation among youth (Display) study: a protocol for an evaluation of public health policy. BMC Public Health. 2014;14:251. doi: 10.1186/1471-2458-14-251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Preventing Tobacco Addiction Foundation. Tobacco 21. Tobacco 21. https://tobacco21.org/. Published n.d. Accessed January 22, 2018.
- 16.Moreland-Russell S, Combs T, Schroth K, Luke D. Success in the city: the road to implementation of Tobacco 21 and Sensible Tobacco Enforcement in New York City. Tob Control. 2016;25(Suppl 1):i6–i9. doi: 10.1136/tobaccocontrol-2016-053089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mayor de Blasio Signs Sweeping Legislation to Curb Smoking, Tobacco Usage. The official website of the City of New York. http://157.188.76.61:8004/office-of-the-mayor/news/565-17/mayor-de-blasio-signs-sweeping-legislation-curb-smoking-tobacco-usage. Published August 28, 2017. Accessed July 19, 2018.
- 18.Brock B, Carlson SC, Moilanen M, Schillo BA. Effectiveness of Local Policy Efforts to Increase the Price of Cheap Cigars in Minnesota. Am J Public Health. 2017;107(1):127–129. doi: 10.2105/AJPH.2016.303517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pearson DC, Song L, Valdez RB, Angulo AS. Youth tobacco sales in a metropolitan county: factors associated with compliance. Am J Prev Med. 2007;33(2):91–97. doi: 10.1016/j.amepre.2007.04.010 [DOI] [PubMed] [Google Scholar]
- 20.Rose SW, Myers AE, D’Angelo H, Ribisl KM. Retailer Adherence to Family Smoking Prevention and Tobacco Control Act, North Carolina, 2011. Prev Chronic Dis. 2013;10. doi: 10.5888/pcd10.120184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coxe N, Webber W, Burkhart J, et al. Use of tobacco retail permitting to reduce youth access and exposure to tobacco in Santa Clara County, California. Prev Med. 2014;67:S46–S50. doi: 10.1016/j.ypmed.2014.01.023 [DOI] [PubMed] [Google Scholar]
- 22.Fry R, Burton S, Williams K, et al. Retailer licensing and tobacco display compliance: are some retailers more likely to flout regulations? Tob Control. 2017;26(2):181–187. doi: 10.1136/tobaccocontrol-2015-052767 [DOI] [PubMed] [Google Scholar]
- 23.Shahab L, West R. Public support in England for a total ban on the sale of tobacco products. Tob Control. 2010;19(2):143–147. doi: 10.1136/tc.2009.033415 [DOI] [PubMed] [Google Scholar]
- 24.Farley SM, Coady MH, Mandel-Ricci J, et al. Public opinions on tax and retail-based tobacco control strategies. Tob Control. 2015;24(e1):e10–e13. doi: 10.1136/tobaccocontrol-2013-051272 [DOI] [PubMed] [Google Scholar]
- 25.Whyte G, Gendall P, Hoek J. Advancing the retail endgame: public perceptions of retail policy interventions. Tob Control. 2014;23(2):160–166. doi: 10.1136/tobaccocontrol-2013-051065 [DOI] [PubMed] [Google Scholar]
- 26.Rose SW, Emery SL, Ennett S, McNaughton Reyes HL, Scott JC, Ribisl KM. Public Support for Family Smoking Prevention and Tobacco Control Act Point-of-Sale Provisions: Results of a National Study. Am J Public Health. 2015;105(10):e60–e67. doi: 10.2105/AJPH.2015.302751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jin Y, Lu B, Klein EG, Berman M, Foraker RE, Ferketich AK. Tobacco-Free Pharmacy Laws and Trends in Tobacco Retailer Density in California and Massachusetts. Am J Public Health. 2016;106(4):679–685. doi: 10.2105/AJPH.2015.303040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Myers AE, Hall MG, Isgett LF, Ribisl KM. A comparison of three policy approaches for tobacco retailer reduction. Prev Med. 2015;74:67–73. doi: 10.1016/j.ypmed.2015.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reducing Tobacco Retail Density in San Francisco: A Case Study. :16.
- 30.Luke DA, Hammond RA, Combs T, et al. Tobacco Town: Computational Modeling of Policy Options to Reduce Tobacco Retailer Density. Am J Public Health. 2017;107(5):740–746. doi: 10.2105/AJPH.2017.303685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pearson AL, Cleghorn CL, Deen FS van der, et al. Tobacco retail outlet restrictions: health and cost impacts from multistate life-table modelling in a national population. Tob Control. 2017;26(5):579–585. doi: 10.1136/tobaccocontrol-2015-052846 [DOI] [PubMed] [Google Scholar]
- 32.Dunlop S, Kite J, Grunseit AC, et al. Out of Sight and Out of Mind? Evaluating the Impact of Point-of-Sale Tobacco Display Bans on Smoking-Related Beliefs and Behaviors in a Sample of Australian Adolescents and Young Adults. Nicotine Tob Res Off J Soc Res Nicotine Tob. 2015;17(7):761–768. doi: 10.1093/ntr/ntu180 [DOI] [PubMed] [Google Scholar]
- 33.Li W, Gouveia T, Sbarra C, et al. Has Boston’s 2011 cigar packaging and pricing regulation reduced availability of single-flavoured cigars popular with youth? Tob Control. 2017;26(2):135–140. doi: 10.1136/tobaccocontrol-2015-052619 [DOI] [PubMed] [Google Scholar]
- 34.Farley SM, Johns M. New York City flavoured tobacco product sales ban evaluation. Tob Control. 2017;26(1):78–84. doi: 10.1136/tobaccocontrol-2015-052418 [DOI] [PubMed] [Google Scholar]
- 35.Leatherdale ST, Strath JM. Tobacco retailer density surrounding schools and cigarette access behaviors among underage smoking students. Ann Behav Med. 2007;33(1):105–111. doi: 10.1207/s15324796abm3301_12 [DOI] [PubMed] [Google Scholar]
- 36.Warner KE. State legislation on smoking and health: A comparison of two policies. Policy Sci. 1981;13(2):139–152. doi: 10.1007/BF00136006 [DOI] [Google Scholar]
- 37.Pacheco J The Social Contagion Model: Exploring the Role of Public Opinion on the Diffusion of Antismoking Legislation across the American States. J Polit. 2012;74(1):187–202. doi: 10.1017/s0022381611001241 [DOI] [Google Scholar]
- 38.Shipan CR, Volden C. Bottom-Up Federalism: The Diffusion of Antismoking Policies from U.S. Cities to States. Am J Polit Sci. 50(4):825–843. doi: 10.1111/j.1540-5907.2006.00218.x [DOI] [Google Scholar]
- 39.Shipan CR, Volden C. The Mechanisms of Policy Diffusion. Am J Polit Sci. 52(4):840–857. doi: 10.1111/j.1540-5907.2008.00346.x [DOI] [Google Scholar]
- 40.Henriksen L, Mahoney M. Tobacco industry’s T.O.T.A.L. interference. Tob Control. March 2017:tobaccocontrol-2016–053530. doi: 10.1136/tobaccocontrol-2016-053530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Farrelly MC, Chaloupka FJ, Berg CJ, et al. Taking Stock of Tobacco Control Program and Policy Science and Impact in the United States. J Addict Behav Ther. 2017;1(2). https://www.imedpub.com/abstract/taking-stock-of-tobacco-control-program-and-policy-science-and-impact-in-the-united-states-20344.html. Accessed March 1, 2018. [PMC free article] [PubMed] [Google Scholar]
- 42.Behavioral Research Program: State and Community Tobacco Control Research Initiative. National Cancer Institute - Division of Cancer Control & Population Sciences Population Sciences. https://cancercontrol.cancer.gov/brp/tcrb/state-community.html. Published March 7, 2017. Accessed January 22, 2018.
- 43.Ribisl KM, Luke DA, Bohannon DL, Sorg AA, Moreland-Russell S. Reducing Disparities in Tobacco Retailer Density by Banning Tobacco Product Sales Near Schools. Nicotine Tob Res. 2017;19(2):239–244. doi: 10.1093/ntr/ntw185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.US Census Bureau. ACS 2012 (5-Year Estimates). Social Explorer. https://www.socialexplorer.com/tables/ACS2012_5yr. Published n.d. Accessed December 12, 2016. [Google Scholar]
- 45.Luke DA, Sorg AA, Combs T, et al. Tobacco retail policy landscape: a longitudinal survey of US states. Tob Control. 2016;25(Suppl 1):i44–i51. doi: 10.1136/tobaccocontrol-2016-053075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Henriksen L, Ribisl KM, Rogers T, et al. Standardized Tobacco Assessment for Retail Settings (STARS): dissemination and implementation research. Tob Control. 2016;25(Suppl 1):i67–i74. doi: 10.1136/tobaccocontrol-2016-053076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.American Lung Association. Tobacco: Cigarette & Tobacco Taxes. American Lung Association. http://www.lung.org/our-initiatives/tobacco/taxes/. Published n.d. Accessed April 11, 2017. [Google Scholar]
- 48.Golden SD, Ribisl KM, Perreira KM. Economic and Political Influence on Tobacco Tax Rates: A Nationwide Analysis of 31 Years of State Data. Am J Public Health. 2013;104(2):350–357. doi: 10.2105/AJPH.2013.301537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dave Leip’s Atlas of U.S. Presidential Elections. https://uselectionatlas.org/. Accessed February 13, 2018.
- 50.County Health Rankings & Roadmap. Health Data 2012. Social Explorer. https://www.socialexplorer.com/tables/HD2012. Accessed December 12, 2016. [Google Scholar]
- 51.Biography of the Surgeon General | SurgeonGeneral.gov. https://www.surgeongeneral.gov/about/biographies/bio-sg.html. Accessed February 13, 2018. [Google Scholar]
- 52.U.S. Department of Health and Human Services. The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014:944. https://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf. [Google Scholar]


