Abstract
Invasive cervical root resorption (ICRR) is a dental pathology, marked by unexpected destruction originating in the cervical region of the tooth. This comprehensive literature review provides a holistic view into the pathogenesis, clinical manifestation, and precise management of ICRR, aiming to guide endodontists and enhance patient care and treatment outcomes. The review delves into the potential etiology of ICRR, covering contributing factors such as trauma, orthodontic treatment, and other pertinent conditions. It outlines the clinical and radiographic indicators, underscoring the crucial role of early detection and precise diagnosis in effectively managing and halting ICRR progression. The exploration of treatment approaches is thorough, ranging from non-surgical methods like vital pulp therapy or root canal treatment to surgical interventions. This review accentuates the essential role of interdisciplinary collaboration among diverse dental specialties in enhancing ICRR management. It highlights the importance of a consolidated strategy in enhancing treatment outcomes and preserving tooth structure and function. Moreover, it investigates prevention methods, risk evaluation, and identifies prospective research pathways to address the existing knowledge gaps.
Key Words: Endodontics, Invasive Cervical Root Resorption, Interdisciplinary Approach, Pathogenesis, Pulpotomy, Radiographic Examination, Treatment Strategies
Introduction
In 1979, invasive cervical root resorption (ICRR) was first introduced in the dental literature, initially associated with external resorption in pulpless teeth following the action of hydroxyl radicals from bleaching agents [1]. Since then, ICRR has emerged as a formidable challenge in the fields of endodontics and comprehensive dental care. Its clinical presentation, characterized by silent yet aggressive destruction, predominantly affects the cervical region of the dental hard tissues. This pathological enigma highlights the need for innovative and robust diagnostic and treatment approaches. When left untreated, ICRR defects can increase in size and develop more root surface perforations. ICRR has a dynamic nature, and its volumetric increase over time does not result from uniform/linear expansion of the defects [2]. Despite its historical presence, the precise etiology of ICRR is unknown, mixed with a multitude of predisposing factors, including trauma, orthodontic treatment, and various surgical interventions [3].
In light of its multifaceted nature, ICRR underscores the significance of an all-encompassing, accurate diagnostic approach, merging clinical assessments with state-of-the-art imaging technologies. Such a comprehensive strategy is crucial for improving diagnostic precision, thereby facilitating the development of tailored treatment strategies. Traditional treatment methods, primarily external and surgical, are increasingly being replaced by more conservative internal approaches that focus on preserving pulp vitality. This shift indicates the evolving trajectory of ICRR management [4].
ICRR is a complex dental condition that requires the specialized expertise of endodontists for effective management [5]. This review provides a thorough exploration of ICRR, covering its pathogenesis, clinical presentation, diagnostic challenges, and various treatment options, including the use of biocompatible materials. As dental research progresses, this article seeks to contribute to the knowledge base of dental professionals. It aims to explain the complexities of ICRR, empowering endodontists to deliver optimal patient care while preserving dental pulp vitality and overall well-being. This comprehensive review serves as a guide, fostering innovative ICRR management and raising oral health standards for diverse populations.
Pathogenesis of Invasive Cervical Root Resorption
ICRR as a subtype of external inflammatory root resorption [6] stands as a complex and enigmatic dental condition, lacking a precise definition for its etiology and pathogenesis. This intricate pathological process is characterized by the aggressive deterioration of dental hard tissues, including cementum and dentin, primarily manifesting at the outer surfaces of the cervical region of the tooth [7]. Despite extensive research and clinical observations, its pathophysiology remains unclear, giving rise to diverse terminologies and interpretations.
Etiological Enigma
Understanding the exact cause of ICRR remains elusive, resulting in varied interpretations of the underlying pathogenesis. Researchers tackle the fundamental question of whether ICRR is solely driven by inflammatory pathways stimulated by specific bacterial components in the gingival sulcus, or alternatively, if it arises from a benign proliferative fibrovascular or osseous disorder involving abnormal cell signaling or remodeling processes [8]. To definitively resolve these uncertainties, future investigations might employ targeted molecular biological techniques, such as RNA sequencing to identify differentially expressed genes and pathways, enzyme histochemical assays to pinpoint exact resorptive mechanisms, and advanced microbiological analyses to characterize the precise microbial composition and activity at the resorptive line.
Factors Influencing Onset
ICRR, characterized as an enigmatic form of external root resorption, poses a distinct and pathological challenge. It has been extensively described by Heithersay and is defined as a localized resorptive process commencing on the root surface beneath the epithelial attachment and the coronal aspect of the supporting alveolar process, specifically the connective tissue attachment zone [8]. Due to its aggressive nature, the term "invasive cervical root resorption" is favored in this paper. The exact cause of ICRR remains uncertain, with descriptions ranging from an aseptic resorptive process that may become secondarily infected to suggestions that microorganisms play a primary role. While the involvement of dental pulp tissue in ICRR remains debated, environmental factors have been proposed as contributors. These factors include exposed dentin due to an open cement-enamel junction, vascular conjunctive tissue presence, and inflammatory stimuli [9, 10]. Various factors, including genetic predisposition, cysts, autotransplantation, bisphosphonate use, dental trauma, extraction of neighboring teeth, guided tissue regeneration, herpes zoster, impacted teeth, idiopathic factors, internal bleaching, malocclusion, orthodontic treatment, oxalosis, periodontal disease, periodontal therapy, playing wind instruments, poor occlusion pressure, pressure from erupting canines, restorative treatment, surgery, systemic and genetic factors, tooth whitening, transmission of feline viruses to humans, traumatic injuries (luxation and avulsion) and tumors have been implicated as potential causes of ICRR, reflecting its multifactorial nature [3, 7-12]. In addition, a wide range of systemic and local factors and conditions, such as hormonal imbalances, infections, or excessive orthodontic force, can exacerbate and accelerate the development of ICRR, making its progression and management more complex [7]. The complex etiology of ICRR necessitates further research.
Clinical Classification
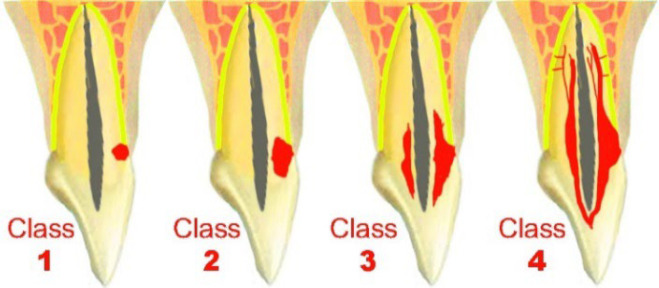
ICRR is clinically classified by Heithersay into four distinct classes based on lesion characteristics [8] (Figure 1). This classification system is essential for both research and clinical assessment of ICRR cases, offering valuable insights into lesion depth and penetration, thus facilitating accurate diagnosis and treatment planning.
Figure 1.
Schematic Classification of ICRR Lesions According to Heithersay
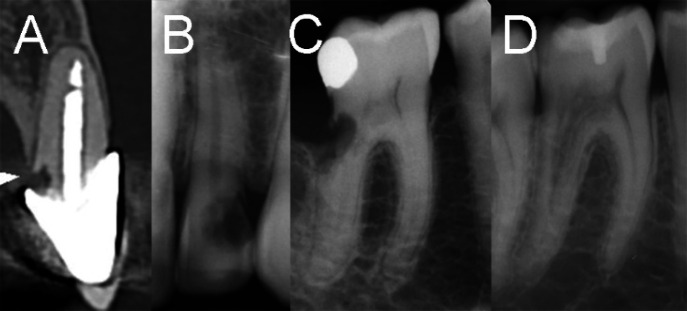
Class 1: Denotes a small ICRR lesion located near the cervical area with shallow penetration into the dentine (Figure 2A).
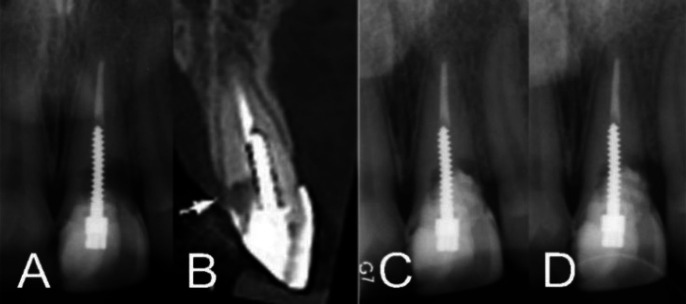
Figure 2.
Radiographic Presentation of various ICRR Cases; A) Class 1 exhibits a small lesion near the cervical area with limited penetration into the dentine; B) In Class 2, a well-defined ICRR lesion is observed close to the coronal pulp chamber; C) Class 3 signifies a deeper invasion, involving the coronal dentine and extending into the coronal third of the root; D) Finally, Class 4 indicates a large ICRR process that extends beyond the coronal third of the root
Class 2: Represents a well-defined ICRR lesion that has penetrated close to the coronal pulp chamber but shows little or no extension into the radicular dentine (Figure 2B).
Class 3: Signifies deeper invasion of dentine by resorbing tissue, involving the coronal dentine and extending into the coronal third of the root (Figure 2C).
Class 4: Indicates a large ICRR process that has extended beyond the coronal third of the root (Figure 2D).
Furthermore, a recent addition to the classification system introduced a three-dimensional perspective to assess ICRR lesions, taking into consideration three critical dimensions: height, circumferential spread, and proximity to the root canal [13]. Height refers to the coronal-apical extent of the lesion based on the Heithersay classification, which further elaborates on the extent of the lesion within the root. The circumferential spread, ranging from ≤90° to >270°, assesses the maximum width of the lesion within the root. Additionally, proximity to the root canal indicates the potential involvement of the pulp. These assessments are typically conducted using various imaging techniques, including periapical radiographs and Cone Beam Computed Tomography (CBCT) scans.
Initiation and Progression
The initiation and progression of ICRR involve a three-stage process in both endodontically treated and vital teeth [3, 14, 15]. Investigating these patterns and mechanisms provides valuable insights into the pathogenesis of ICRR.
Initiation Stage: During the initial phase, ICRR commences below the gingival epithelial attachment, typically at the cementum level, laying the groundwork for the resorptive process. This stage is characterized by the localized destruction of the PDL and unmineralized cementum. It involves the formation of a blood clot and a localized inflammatory response on the exposed dentine [16, 17]. Macrophages migrate to the affected area, giving rise to granulation tissue formation. The exposed dentine becomes vulnerable to resorption from adjacent bone or immune cells. Subsequently, the area undergoes repopulation by various cell types, including bone cells, PDL fibroblasts, and epithelial gingival cells. The stimulation of odontoclastic cells occurs through the expression of 'Receptor Activator of Nuclear Factor k B Ligand' (RANKL). Additionally, hypoxia and bacteria contribute to inflammation and osteoclastogenesis during this phase of ICRR initiation.
Resorption Stage: In the second stage, ICRR advances three-dimensionally toward the pulp space, yet typically avoids breaching it due to the presence of the pericanalar resorption-resistant sheet (PRRS). This protective layer, comprising predentin and dentin with an average thickness of approximately 210 μm, is resistant to resorption. It's crucial to note that the PRRS is frequently removed during root canal treatment, leaving the tooth without a defense mechanism against ICRR.
During this stage, various factors contribute to the progression of ICRR, including infection (bacteria), continuous orthodontic force, and intermittent mechanical stress, such as that from chewing or parafunctional activities. The induction of a hypoxic microenvironment activates osteoclastogenesis, contributing to ICRR progression. The resorptive process invades the tooth structure, affecting cementum, dentine, and enamel in all planes. The direction of clastic cells is influenced by inflammatory mediators and hormones.
Despite the presence of the PRRS, which helps prevent perforation into the root canal, maintaining pulp vitality, there remains the potential for perforation of the root canal in advanced cases. This intricate interplay of factors underscores the complexity of ICRR progression and the challenges it presents in maintaining the structural integrity of the affected tooth.
Repair Stage: The final phase of ICRR involves repair, characterized by the ingrowth and apposition of bonelike tissue into the ICRR cavity. During this stage, simultaneous processes of repair and remodeling take place, with resorption and reparative stages progressing in parallel in different areas of the tooth.
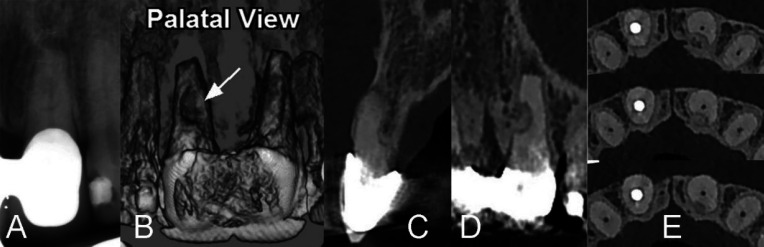
This reversed stage signifies the repair process conducted by osteoblast-like cells, facilitating the ingrowth of bone-like tissue into the ICRR cavity. The reparative tissue, along with the tooth structure, integrates into the normal alveolar bone structure, representing a form of healing. Notably, active remodeling occurs asynchronously at multiple sites, contributing to changes observed in CBCT images during long-term follow-up. This intricate dynamic between resorption and repair underscores the complex nature of ICRR's resolution and emphasizes the importance of understanding these processes for effective clinical management (Figure 3).
Figure 3.
Radiographic Documentation of ICRR in Upper Left Central Incisor. A) Periapical Radiograph: Very slight signs of resorption are detectable in the involved tooth; B) CBCT from Palatal View: Clear depiction of Class 4 ICRR; C, D, & E) CBCT views showcase the remarkable ingrowth and apposition of bonelike tissue into the ICRR cavity, showing a repair stage
Cellular and Molecular Mechanisms
The pathogenesis of ICRR involves the intricate interplay of cellular and molecular mechanisms. This multifaceted process hinges on the recruitment and activation of specialized clastic cells, primarily odontoclasts and osteoclasts. These cells wield potent proteolytic enzymes, which instigate the breakdown of dental hard tissues and the contiguous bone structure. At the molecular level, the orchestration of resorptive cell activity is governed by pivotal elements, such as cytokines and growth factors, including but not limited to RANKL and OPG (Osteoprotegerin). These molecular agents play a critical role in overseeing the dynamics of resorption within the context of ICRR [8].
Recent research has suggested a potential link between ICRR and hypoxia, prompting an extensive study [18]. The diagnosis was established through clinical and radiographic examinations, including cone-beam computed tomographic imaging. Subsequently, the extracted tooth underwent further analysis using nanofocus computed tomographic imaging and immunohistology to investigate the three-dimensional extent and pattern of ICRR. The investigation revealed a higher prevalence of hypoxia-inducible factor 1a-positive cells in the apical resorption area compared to the coronal region, with a similar distribution within the pulp's odontoblasts. This study substantiates the presence of hypoxia in ICRR, emphasizing the existence of a hypoxia gradient within the lesion.
Clinical Consequences
The progression of ICRR can result in significant dental deterioration, potentially culminating in tooth loss, with far-reaching consequences for overall oral health and one's quality of life [19]. A comprehensive comprehension of the intricate pathogenesis of ICRR stands as a fundamental requirement for the development of innovative and targeted treatment approaches, ultimately paving the way for optimal dental health outcomes.
Diagnosis and Clinical Presentation
Understanding ICRR necessitates a comprehensive grasp of its diagnosis and clinical presentation. An accurate identification of ICRR relies on a harmonious blend of clinical evaluation and advanced imaging techniques, profoundly influencing the success of subsequent treatment strategies.
Clinical Examination
ICRR is discovered incidentally during routine dental check-ups, with its insidious onset often lacking overt symptoms, adding complexity to the diagnostic process [3]. The condition is generally painless, except when complications like pulpal or periodontal infections arise. While clinical findings may sometimes be subtle, manifestations can range from minor defects at the gingival margin to pink coronal discoloration, eventually leading to enamel cavitation [20]. The extent of the resorptive process may align with the clinical presentation. In more advanced stages affecting the pulp, patients may experience symptoms such as (ir)reversible pulpitis or apical periodontitis. Diagnosing ICRR defects can be challenging, as early defects in interproximal, labial or lingual areas may go undetected, while cavitated defects on labial or lingual surfaces can be diagnosed visually or through probing. Bleeding on probing is characteristic due to the vascularity of the defects. ICRR may be mistaken for buccal caries, but crucial tactile feedback helps distinguish between the softness of caries and the hardness of ICRR [21]. A 'pink' spot in the cervical aspect of the tooth is pathognomonic, indicating fibrovascular granulation tissue visible through thinned enamel [22]. However, these spots may be challenging to detect on posterior teeth. Discoloration, pink or grey, may occur, with grey discoloration indicating pulp necrosis. ICRR lacks a classic presentation, often appearing incidentally on examinations or showing symptoms related to pulpal involvement. Positive sensibility testing occurs unless the root canal is perforated and pulp necrosis occurs. Hygienists, during routine assessments, are increasingly detecting early ICRR lesions through visual assessment and gentle probing.
Radiographic Evaluation
Radiographic assessment plays a crucial role in enhancing the diagnostic accuracy of ICRR. The radiographic features of these lesions can vary, exhibiting symmetrical or asymmetrical patterns with diverse margins, ranging from well-delineated and smooth to irregularly bordered mottled radiolucencies, sometimes resembling dental caries. A distinctive radiopaque line typically separates the lesion from the root canal, protecting the pulp with a thin layer of predentin until later stages of the resorptive process.
Techniques such as periapical radiography and cone-beam computed tomography (CBCT), alongside modalities like orthopantomography, provide detailed insights into the extent and pattern of root resorption [23, 24]. Among these, CBCT stands out for its capacity to offer a comprehensive view of ICRR in any plane, free from superimpositions of overlying structures and geometric distortions [25]. This capability aligns well with the new classification system for ICRR. In cases involving a history of orthodontic treatment, conducting a comprehensive full-mouth radiographic examination becomes imperative, particularly to rule out the presence of multiple lesions.
Despite the absence of a distinct radiographic appearance for ICRR, various classification systems, including Heithersay's and a proposed 3-dimensional classification, aim to enhance ICRR diagnosis and communication among clinicians [8, 13]. CBCT significantly improves the accuracy of ICRR diagnosis and management, enabling precise visualization of resorptive extensions and hard tissue deposits. Studies confirm CBCT's superiority over periapical radiographs in terms of accuracy and treatment planning [25]. Endodontic literature underscore the importance of CBCT in ICRR management, recognizing its impact on accurate diagnosis and treatment planning [26]. However, it is crucial to justify and adhere to radiation safety principles (ALARA) when utilizing CBCT scans.
Histopathological Insights
Histopathological examination plays a pivotal role in unraveling the intricate nature of ICRR lesions. The histological examination encompasses the portal of entry, where initiation occurs in the cementum below the gingival epithelial attachment, necessitating the destruction or removal of the PDL. Resorption areas and channels expand in three dimensions, encircling and progressing towards the root canal system, resulting in the destruction of dental hard tissues. The PRRS prevents perforation into the root canal and consists of dentine and occasionally bone-like tissue. Repair involves the ingrowth and apposition of reparative bone-like tissue through the portal of entry, appearing as lamellar trabecular bone with islands of woven bone. Remodeling of reparative bone-like tissue entails cyclic resorption and reforming involving clastic and blastic cells, occurring simultaneously in different areas of the same tooth.
Class 2 Lesions, characterized by the presence of fibrous tissue, numerous blood vessels, and clastic resorbing cells near the dentin surface, reveal these elements separated from the dental pulp by the PRRS [27]. In advanced cases, especially Class 3 and Class 4 Lesions, extensive resorptive defects are observed, often filled with fibrovascular and osseous tissues. Within these lesions, bone-like structures form on the resorbed dentin, transforming tooth structure into calcified tissue resembling bone. These advanced lesions also contain spaces filled with fibrovascular tissue. In instances where microorganisms infiltrate the pulp or periodontal ligament space, they can incite a normal inflammatory response.
Proteomic Biomarkers
The development of a non-invasive method for early ICRR detection is essential for successful treatment. Dentin-specific markers, including DMP, DSPP, and their functional domains DPP and DSP, along with inflammatory markers like TNF-α, IL-6, IL1-B, and MicroRNA-29, hold promise as gingival crevicular fluid (GCF) biomarkers for ICRR. In the future, these markers could contribute to the creation of an examination kit for non-invasive resorption biomarker detection in GCF [28]. While the field of proteomic biomarkers is still emerging in the realm of dental disorders, this diagnostic approach shows great potential in reducing the need for invasive procedures i.e. X-ray radiographs.
Differential Diagnosis
It is crucial to accurately distinguish ICRR from similar conditions, such as root caries or internal root resorption, to tailor personalized management strategies [21]. On radiographs, ICRR can sometimes be mistaken for internal resorption. To mitigate this, capturing radiographs from various angles is essential to observe the movement of the lesion, following principles like Clark's rule or the Same Lingual, Opposite Buccal rule. However, it is worth noting that CBCT can provide a more straightforward diagnosis of such conditions [25].
Challenges in Diagnosis
The initial phases of ICRR may often manifest with minimal or no discernible symptoms, resulting in delayed detection and the advancement of the resorptive process. Furthermore, the presence of overlapping symptoms shared with other dental conditions can complicate the diagnostic process. These challenges emphasize the necessity for a comprehensive and multifaceted approach to diagnosis.
Treatment Approaches
The choice of the most suitable treatment for ICRR is highly dependent on the degree/extent and progression of root resorption. This section provides a comprehensive examination of diverse treatment approaches, including their individual success rates, follow-up protocols, and the crucial aspect of patient management.
No-Treatment Strategy (Monitoring)
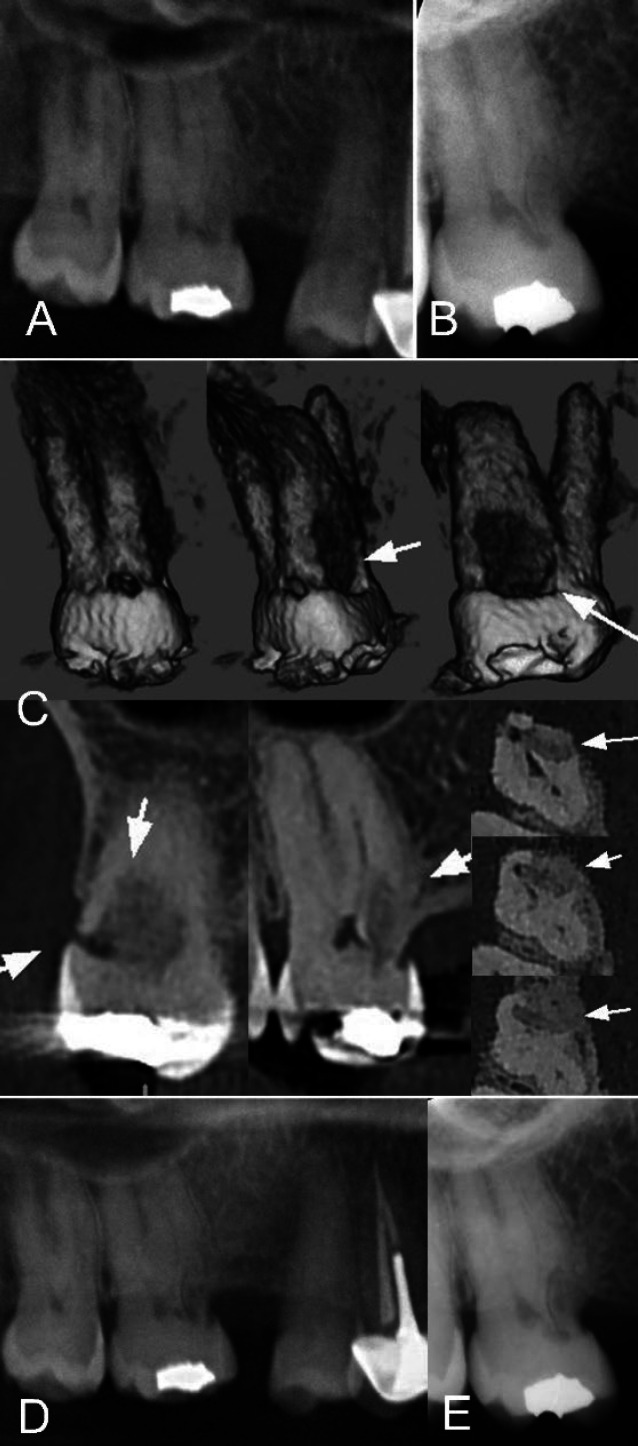
The strategy is designed to manage cases of ICRR that are in the established repair stage (Figure 4) Continuous monitoring is implemented to effectively prevent any further progression of resorption. Patient-centric preferences are carefully considered to ensure adherence to the strategy and maximize therapeutic success.
Figure 4.
Radiographic Assessment and Follow-up of Upper Right Second Molar with ICRR. A) An OPG initially reveals an abnormal view in the mesial aspect of the involved molar; B) This led to a more focused examination with a periapical radiograph; C) To further examine the lesion, a CBCT in various planes revealed an ICRR classified as Class 4, displaying characteristics of an arrested lesion in the repair stage. There was no pulp involvement, and periapical tissues appeared normal. Consequently, a "wait and watch" scenario was approved for the case; D & E) An 8-year follow-up OPG and periapical radiographs establish the appropriateness of the chosen scenario, indicating stable conditions without the need for intervention
Nonsurgical Endodontic Approaches
External Repair: Applied to lesions confined to the cervical region, this is a conservative approach, particularly effective for cases with small portals of entry and significant internal extension. It may be combined with dental pulp management (Figure 5).
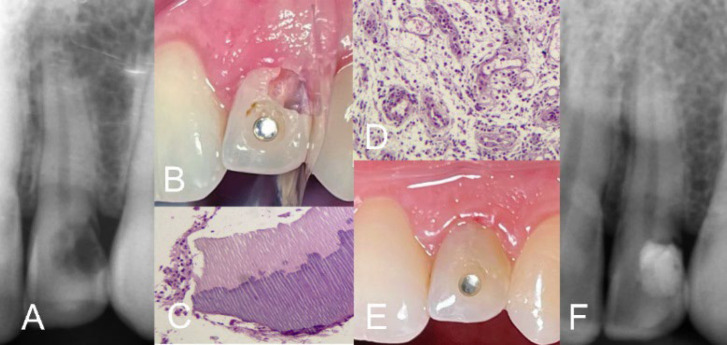
Figure 5.
External Repair of ICRR Class 2 in Upper Left Lateral Incisor. A) Periapical radiograph reveals an ICRR lesion in the involved incisor; B) Non-surgical approach; clinical view after removal of the resorptive tissue from the lesion, exposing the pulp; C and D) Histopathological views of the removed tissue specimen with H&E staining display resorptive dentine pieces with dentinal tubules, and an inflamed tissue; E) Clinical image post-VPT using calcium-enriched mixture and composite filling of the cavity; F) Immediate postoperative radiograph demonstrates the success of VPT and proper coronal filling
Modified Root Canal Treatment : This approach emerges as a viable and strategic option tailored for advanced ICRR, when the pulp is involved or to facilitate reaching the resorptive tissue from inside the tooth (Figure 6). This sophisticated approach intricately addresses the distinct challenges posed by ICRR, combining endodontic expertise with precise restorative methodologies.
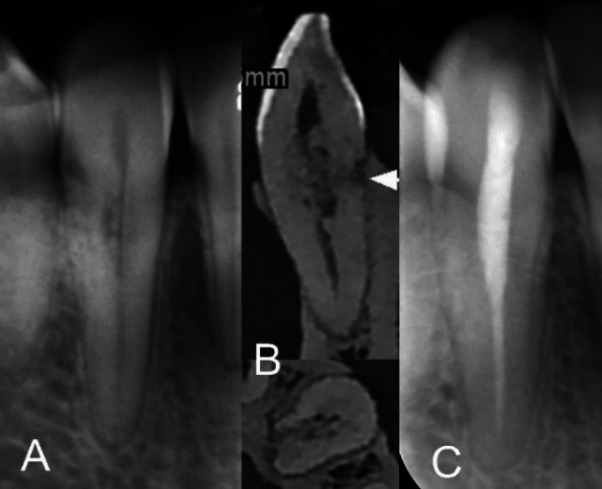
Figure 6.
Asymptomatic ICRR Class 4 in Lower Right Canine; A) Asymptomatic ICRR Class 4 discovered during routine radiographic examination; B) CBCT sagittal and axial views confirm the lesion; C) Immediate postoperative periapical radiograph demonstrates the proper root canal filling with calcium-enriched mixture cement
The treatment initiates with meticulous root canal access to ensure complete exposure of the resorptive lesion. This entails the meticulous removal of any overlying soft or hard tissues, providing unobstructed access to the resorptive site. The process is executed with the aid of appropriate irrigants, facilitating optimal visibility and access to the affected area. Eliminating the resorptive tissue is a pivotal facet of the modified approach.
Mechanical removal, involving specialized burs tailored to the specific characteristics of the lesion, is a standard practice. The objective is to eliminate compromised tissue while preserving as much sound dentin as feasible (Figure 7). Complementary to mechanical removal, the incorporation of chemical agents such as trichloroacetic acid (TCA) compounds or sodium hypochlorite (NaOCl) is considered, aligning with prevailing trends in ICRR management [29]. This dual approach ensures a comprehensive and meticulous elimination of the resorptive tissue, thereby minimizing the risk of recurrence.
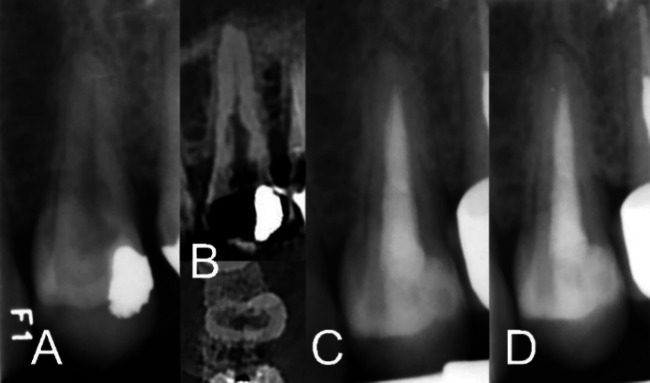
Figure 7.
An ICRR Class 4 in Upper Left First Premolar; A) Asymptomatic ICRR Class 4 discovered during routine radiographic examination; B) CBCT sagittal and axial views confirm the lesion; C) Immediate postoperative periapical radiograph demonstrates the root canal filling with calcium-enriched mixture cement; D) One-year follow-up reveals successful outcomes
The subsequent restorative phase encompasses the use of biocompatible endodontic materials precisely tailored to address the specific challenges presented by ICRR lesions. Calcium silicate-based cements, such as mineral trioxide aggregate (MTA), bioceramics (BC-putty) or calcium-enriched mixture (CEM) cement, are frequently employed [30]. These biomaterials may be utilized in isolation or in combination with composite resins. The combination serves not only to effectively seal the resorptive defect but also to provide structural reinforcement to the affected tooth. The selection of (bio)materials is guided by factors including the location and size of the lesion, aligning with overarching treatment goals. The primary focus remains on achieving a seamless integration of restorative materials with the natural tooth structure, thereby contributing to both the functional and aesthetic rehabilitation of the affected tooth.
Vital Pulp Therapy (VPT) Techniques: These VPT techniques emerge as a highly specialized and minimally invasive intervention designed to safeguard the vitality of the pulp in the context of ICRR. This precision-focused approach prioritizes maintaining pulp functionality while adeptly addressing the distinctive challenges posed by ICRR classifications.
Empirical evidence supporting the success of VPT in ICRR is derived from a focused study involving six patients [4]. This investigation yielded compelling results, demonstrating the sustained functionality of treated teeth. Over an average follow-up period of 19.6 months, the absence of clinical symptoms, such as pain or new resorptive activities, underscored the effectiveness of VPT in managing ICRR with scientific rigor (Figure 8).
Figure 8.
Accidental Detection and Treatment of ICRR. A) ICRR accidentally detected during bitewing radiographic examination; B) Further periapical radiograph reveals an ICRR Class 3 lesion in the involved vital tooth. C) Confirmation of ICRR Class 3 through coronal and axial views in CBCT. D) Postoperative radiograph reveals the successful filling of the lesion with calcium-enriched mixture cement during VPT
The procedure entails achieving appropriate access to expose the defect. For accessible areas, a surgical-length round diamond bur is used, while Gates Glidden drills (sizes #2–4) and Munce burs are employed for lacunae extending into the root around the root canal space [31], utilizing sterile saline solution. The process involves the meticulous excavation of resorptive lacunae, with the extent of pulp removal guided by the necessity to access these lacunae. Bleeding control, if necessary, is accomplished using cotton pellets soaked in 2.5% NaOCl. The subsequent step was adapting endodontic biomaterial into the excavated resorptive lacuna, using a dry cotton pellet to optimize its physical properties. For VPTs, MTA or CEM cement is applied over the remaining dental pulp, in addition to filling and sealing the prepared cavity (Figure 9). A few studies have demonstrated that if a portion of the lesion was not curetted due to limited clinical access, filling the prepared cavity with an optimal seal may still lead to successful outcomes [32, 33]. The final phase of the procedure involves the restoration of the tooth, ensuring a comprehensive and effective treatment approach. If pulp necrosis occurs, then root canal therapy can be considered [34].
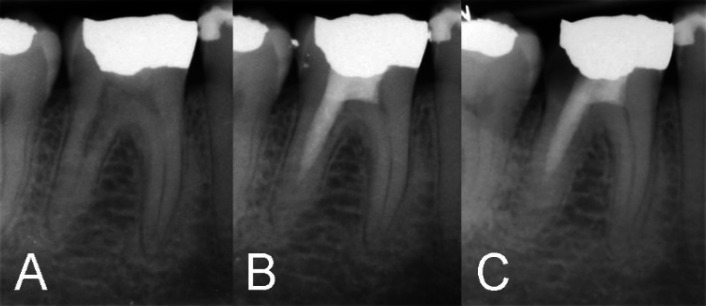
Figure 9.
Accidental Detection and Treatment of ICRR using VPT; A) ICRR was accidentally identified during a routine radiographic examination of an asymptomatic molar; B) Postoperative radiograph shows a full pulpotomy for mesial canals and successful filling of the lesion in the distal canal with calcium-enriched mixture cement during VPT, without reaching the apex; C) five-year follow-ups reveal the cessation of resorption and simultaneously, a normal PDL confirming the successful treatment outcomes
Surgical Approaches
Surgical interventions are the most frequently reported treatment for ICRR cases (particularly Class 3) where lesions extend beyond the reach of non-surgical methods. This better reached externally approach often mandates a periodontal flap to ensure optimal access, especially when lesions extend below the gingival margin. The precision of curettage is of paramount importance during surgery, guaranteeing the meticulous removal of resorptive tissue from the lesion site. In certain instances, achieving complete removal of the ICRR lesion during surgery may pose challenges.
Significantly, alternative techniques can be applied without the requirement for a conventional approach involving the use of a chemical cauterizing agent, such as trichloroacetic acid, for complete lesion eradication. Emerging evidence indicates that Utilizing biomaterials allows for the retention of some portion of the resorptive lesion without detriment to the overall success of the treatment outcomes [4, 35]. Following tissue removal, defect restoration becomes integral, employing a variety of restorative materials, including Geristore, bioceramics, MTA, Biodentine and CEM cement, to uphold the tooth’s structural integrity [36, 37]. These surgical techniques prove instrumental in addressing and mitigating the effects of ICRR, particularly in situations where non-surgical approaches may fall short (Figure 10).
Figure 10.
Management of ICRR in Upper Left Central Incisor; A) Periapical radiograph reveals an ICRR lesion in the involved incisor, which underwent endodontic treatment; B) CBCT coronal image confirms an ICRR Class 2 lesion; C) Immediate post-surgery radiograph shows the incomplete filling of the lesion with calcium-enriched mixture cement, indicating incomplete lesion removal; D) Two-year follow-up radiograph indicates the remaining portion of the resorptive lesion did not compromise the positive treatment outcomes
Moreover, intentional replantation serves as a strategic surgical option when the ICRR defect proves challenging to expose through in situ approaches. This procedure involves the meticulous extraction of the affected tooth, addressing the resorptive defect and perforation repair, followed by replantation into its original socket [38]. To ensure the success of intentional replantation, the repaired defect should be filled with an endodontic biomaterial, contributing to the regeneration of affected root surfaces. Root-end preparation and filling with the same biomaterial become unavoidable steps in this process. Utilizing endodontic biomaterials, such as calcium silicate-based cements like MTA or CEM cement or bioceramics, not only effectively seals the repaired defect but also promotes healing, enhancing treatment outcomes. This comprehensive approach poses challenges due to trauma to the PDL during extraction, therefore requires a meticulous balance of atraumatic extraction techniques and efficient management of the resorptive lesion.
Furthermore, surgical procedures provide avenues for innovative regenerative techniques. Leveraging bioactive materials and growth factors, such as the implementation of resorbable and non-resorbable membranes for guided tissue regeneration, or the application of bioactive materials and growth factors, aims to rejuvenate affected areas, ultimately enhancing treatment outcomes. The integration of these advanced regenerative approaches underscores the ongoing evolution and refinement of surgical strategies for managing ICRR.
Finally, extraction of the affected tooth may be the only option in untreatable cases where there are aesthetic, functional, and/or symptomatic issues. The decision for extraction is typically considered when the extent of resorption, aesthetic concerns, compromised functionality, or the presence of symptoms outweigh the potential benefits of conservative treatments. In such instances, extraction opens the door to various replacement options, including implant-retained crowns, resin-bonded bridges, conventional bridges, removable partial dentures, and considerations of space acceptance.
Mixed and Multidisciplinary Approaches
Cases involving severe ICRR may require a comprehensive, multidisciplinary approach. This approach combines the expertise of multiple dental disciplines, such as endodontics, orthodontics, periodontics, and prosthetics [39, 40] as well as combination of internal and external therapeutic access. An example of this approach is orthodontic extrusion [41]with or without surgical techniques for exposing the ICRR rapidly from within the alveolar socket, reaching sound and healthy tooth material beyond the affected zone suitable for preparation and repair.
Treatment Outcomes
Effective ICRR treatment relies significantly on rigorous follow-up procedures, crucial for assessing treatment outcomes, monitoring potential resorption recurrence, and preserving tooth structure and function. In a study involving 94 patients with 101 affected teeth, the treatment approach encompassed root canal therapy, surgical methods including the topical application of trichloracetic acid, curettage, and restoration with glass-ionomer cement [42]. Remarkably, this approach achieved a 100% success rate for class 1 and 2 ICRR lesions, a 78% success rate for class 3, while class 4 lesions exhibited only a 2% success rate. Surgical treatment was deemed inappropriate for class 4 and many class 3 ICRR cases due to extensive periodontal defects. It is worth noting that severe ICRR cases, while having a 50% survival rate, only showed a 12.5% overall success rate, often necessitating prosthodontic replacement. However, a recent systematic review, incorporating 66 case reports/series, indicated that nearly all treated cases of various ICRR severities were successful [24].
Patient Management and Perspectives
Recognizing and considering the patient’s viewpoint regarding diverse treatment options is of paramount importance. Engaging in comprehensive conversations that encompass the advantages and disadvantages of each treatment, expected outcomes, and post-treatment care is crucial for making well-informed decisions and ultimately boosting patient satisfaction. It’s important to note that, in light of the concept of minimally invasive endodontics and the successful outcomes associated with VPT, clinicians should encourage and guide patients toward minimally invasive endodontic options.
Prevention and Risk Factors
Preventing ICRR is a paramount concern within this domain. An in-depth comprehension of the risk factors that trigger ICRR is fundamental in establishing effective preventive measures. This section delves into the risk factors associated with ICRR and elucidates prevention strategies, underscoring the pivotal role of patient education and awareness.
Unpacking Risk Factors: ICRR often finds its origins in a complex interplay of various risk factors. Factors such as trauma, orthodontic procedures, periodontal treatments, and systemic conditions like hormonal imbalances or genetic predispositions play significant roles in the emergence and progression of ICRR. Recognizing these factors is crucial for mitigating the risk of this pathological condition’s development.
Proactive Prevention Strategies: Effective preventive strategies encompass prompt intervention in cases of trauma, careful management during orthodontic treatments, and routine dental assessments to detect early signs of resorption.
Patient Education and Awareness: An informed patient is a robust defense against ICRR. The importance of patient education cannot be overstated in ICRR prevention. Dentists and endodontists bear the responsibility of disseminating comprehensive information regarding risk factors and early indicators of ICRR, enhancing patient awareness and vigilance. Well-informed patients are more likely to seek timely dental intervention, reinforcing early detection and preventive management of ICRR.
Future Directions and Research Gaps
Improved Diagnostic Tools: Enhancing diagnostic tools for ICRR is crucial. Future research should explore integrating artificial intelligence and machine learning in radiographic assessments to enhance ICRR detection accuracy and speed [43]. Innovative biomarkers in saliva or serum may revolutionize non-invasive diagnostics.
Advancements in Treatment: The search for optimal ICRR treatments continues, with regenerative approaches like stem cell and growth factor utilization showing promise. Research into nanomaterials and biocompatible scaffolds for reconstructing resorbed root surfaces could yield novel treatment techniques.
Long-Term Outcome Assessment: Long-term clinical research is essential to evaluate the durability and efficacy of various ICRR treatments. Detailed studies on restored tooth longevity, potential complications, and their impact on patients’ quality of life are critical.
Providing the highest level of evidence: It is noteworthy to emphasize that, currently, there is a lack of randomized clinical trials specifically addressing ICRR diagnosis and treatment. Conducting such trials is essential to establish robust and standardized diagnostic and treatment protocols.
Interdisciplinary Collaboration: Enhancing collaboration between endodontists, orthodontists, and restorative dentists is vital. Research on the effectiveness of combined treatment planning in complex ICRR cases can offer insights for improved patient outcomes.
Risk Factors and Prevention: A concerted effort to understand distinct risk factors contributing to ICRR susceptibility is essential. Investigating the roles of genetics, systemic conditions, and local factors in ICRR development will aid in tailored prevention strategies.
Patient-Centered Research: Incorporating patient-centered outcomes in future research is crucial to assess ICRR’s practical impact and treatment effects on patients’ daily lives. Evaluations should include quality of life measures, patient-reported pain levels, and psychosocial effects.
Educational Initiatives Enhancement: Raising awareness among dental professionals about ICRR requires comprehensive educational programs and workshops. Evaluating the impact of these educational activities can significantly improve early detection and timely interventions.
Conclusions
Successfully managing ICRR requires early diagnosis, precise treatment, and consistent prevention efforts. This comprehensive exploration underscores the significance of advanced diagnostic tools and innovative treatment approaches in mitigating the impact of ICRR. Collaboration among different dental specialties is essential to enhance patient outcomes and provide holistic care. Emphasizing patient-centered research, enriched with real-world insights, supports the ongoing enhancement of ICRR management strategies, ensuring they meet evolving patient needs and expectations. Looking ahead, these multifaceted strategies illuminate the path for the global dental community, guiding them toward effective and comprehensive ICRR management.
Acknowledgments
NA.
Conflict of interest
None.
Funding support
No funding was received for this study.
Authors’ contributions
Saeed Asgary: Contributed to conception, design, data acquisition/analysis/interpretation, drafted and critically revised the manuscript. Omid Dianat: Contributed to data interpretation, and drafted and critically revised the manuscript. The authors gave their final approval and agreed to be accountable for all aspects of the work.
Informed consent
Written informed consent was obtained from the patients.
References
- 1.Harrington GW, Natkin E. External Resorption Associated with Bleaching of Pulpless Teeth. J Endod. 1979;5(11):344–8. doi: 10.1016/S0099-2399(79)80091-6. [DOI] [PubMed] [Google Scholar]
- 2.Nosrat A, Dianat O, Verma P, Levin MD, Price JB, Aminoshariae A, Rizzante FAP. External Cervical Resorption: A Volumetric Analysis on Evolution of Defects over Time. J Endod. 2023;49(1):36–44. doi: 10.1016/j.joen.2022.10.010. [DOI] [PubMed] [Google Scholar]
- 3.Patel S, Mavridou AM, Lambrechts P, Saberi N. External Cervical Resorption-Part 1: Histopathology, Distribution and Presentation. Int Endod J. 2018;51(11):1205–23. doi: 10.1111/iej.12942. [DOI] [PubMed] [Google Scholar]
- 4.Asgary S, Nourzadeh M, Verma P, Hicks ML, Nosrat A. Vital Pulp Therapy as a Conservative Approach for Management of Invasive Cervical Root Resorption: A Case Series. J Endod. 2019;45(9):1161–7. doi: 10.1016/j.joen.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 5.Rotondi O, Waldon P, Kim SG. The Disease Process, Diagnosis and Treatment of Invasive Cervical Resorption: A Review. Dent J (Basel) 2020;8(3) doi: 10.3390/dj8030064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ne RF, Witherspoon DE, Gutmann JL. Tooth Resorption. Quintessence Int. 1999;30(1):9–25. [PubMed] [Google Scholar]
- 7.Kandalgaonkar SD, Gharat LA, Tupsakhare SD, Gabhane MH. Invasive Cervical Resorption: A Review. J Int Oral Health. 2013;5(6):124–30. [PMC free article] [PubMed] [Google Scholar]
- 8.Heithersay G. Invasive Cervical Resorption. Endodontic Topics. 2004;7:73–92. [Google Scholar]
- 9.Hammarström L, Lindskog S. Factors Regulating and Modifying Dental Root Resorption. Proc Finn Dent Soc. 1992;88 Suppl 1:115–23. [PubMed] [Google Scholar]
- 10.Gold SI, Hasselgren G. Peripheral Inflammatory Root Resorption A Review of the Literature with Case Reports. J Clin Periodontol. 1992;19(8):523–34. doi: 10.1111/j.1600-051x.1992.tb00679.x. [DOI] [PubMed] [Google Scholar]
- 11.Heithersay GS. Invasive Cervical Resorption: An Analysis of Potential Predisposing Factors. Quintessence Int. 1999;30(2):83–95. [PubMed] [Google Scholar]
- 12.Tronstad L. Root Resorption-Etiology, Terminology and Clinical Manifestations. Endod Dent Traumatol. 1988;4(6):241–52. doi: 10.1111/j.1600-9657.1988.tb00642.x. [DOI] [PubMed] [Google Scholar]
- 13.Patel S, Foschi F, Mannocci F, Patel K. External Cervical Resorption: A Three-Dimensional Classification. Int Endod J. 2018;51(2):206–14. doi: 10.1111/iej.12824. [DOI] [PubMed] [Google Scholar]
- 14.Mavridou AM, Hauben E, Wevers M, Schepers E, Bergmans L, Lambrechts P. Understanding External Cervical Resorption Patterns in Endodontically Treated Teeth. Int Endod J. 2017;50(12):1116–33. doi: 10.1111/iej.12744. [DOI] [PubMed] [Google Scholar]
- 15.Mavridou AM, Hauben E, Wevers M, Schepers E, Bergmans L, Lambrechts P. Understanding External Cervical Resorption in Vital Teeth. J Endod. 2016;42(12):1737–51. doi: 10.1016/j.joen.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 16.Polimeni G, Xiropaidis AV, Wikesjö UM. Biology and Principles of Periodontal Wound Healing/Regeneration. Periodontol. 2000;41:30–47. doi: 10.1111/j.1600-0757.2006.00157.x. [DOI] [PubMed] [Google Scholar]
- 17.Chu EY, Deeb JG, Foster BL, Hajishengallis E, Somerman MJ, Thumbigere-Math V. Multiple Idiopathic Cervical Root Resorption: A Challenge for a Transdisciplinary Medical-Dental Team. Front Dent Med. 2021:2. doi: 10.3389/fdmed.2021.652605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mavridou AM, Hilkens P, Lambrichts I, Hauben E, Wevers M, Bergmans L, Lambrechts P. Is Hypoxia Related to External Cervical Resorption? A Case Report. J Endod. 2019;45(4):459–70. doi: 10.1016/j.joen.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 19.Dias C, Closs L, Barletta F, Reston E, Tovo MF, Lambert P. Root Resorption a 6-Year Follow-up Case Report. Open Dent J. 2015;9:103–5. doi: 10.2174/1874210601509010103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel S, Abella F, Patel K, Lambrechts P, Al-Nuaimi N. Clinical and Radiographic Features of External Cervical Resorption-An Observational Study. Int Endod J. 2023;56(12):1475–87. doi: 10.1111/iej.13968. [DOI] [PubMed] [Google Scholar]
- 21.Spielman R, Ameh G. Challenges in Differential Diagnostic and Treatment of Cervical Root Resorption vs Root Caries. 2023;1:1–11. doi: 10.1177/20501684241256468. [DOI] [PubMed] [Google Scholar]
- 22.Asgary S. Management of Pink Spot due to Class IV Invasive Cervical Root Resorption using Vital Pulp Therapy: A Case Report. Iran Endod J. 2023;18(2):110–2. doi: 10.22037/iej.v18i2.41772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Madani Z, Moudi E, Bijani A, Mahmoudi E. Diagnostic Accuracy of Cone-Beam Computed Tomography and Periapical Radiography in Internal Root Resorption. Iran Endod J. 2016;11(1):51–6. doi: 10.7508/iej.2016.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Safi Y, Ghaedsharaf S, Aziz A, Hosseinpour S, Mortazavi H. Effect of Field Of View on Detection of External Root Resorption in Cone-Beam Computed Tomography. Iran Endod J. 2017;12(2):179–84. doi: 10.22037/iej.2017.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vasconcelos Kde F, Nejaim Y, Haiter Neto F, Bóscolo FN. Diagnosis of Invasive Cervical Resorption by Using Cone Beam Computed Tomography: Report of Two Cases. Braz Dent J. 2012;23(5):602–7. doi: 10.1590/s0103-64402012000500023. [DOI] [PubMed] [Google Scholar]
- 26.Bardini G, Orrù C, Ideo F, Nagendrababu V, Dummer P, Cotti E. Clinical Management of External Cervical Resorption: A Systematic Review. Aust Endod J. 2023;49(3):769–87. doi: 10.1111/aej.12794. [DOI] [PubMed] [Google Scholar]
- 27.Heithersay GS. Clinical, Radiologic, and Histopathologic Features of Invasive Cervical Resorption. Quintessence Int. 1999;30(1):27–37. [PubMed] [Google Scholar]
- 28.Mona M, Abbasi Z, Kobeissy F, Chahbandar A, Pileggi R. A Bioinformatics Systems Biology Analysis of the Current Oral Proteomic Biomarkers and Implications for Diagnosis and Treatment of External Root Resorption. Int J Mol Sci. 2021;22(6):3181. doi: 10.3390/ijms22063181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mohammadi Z, Z CC, Shalavi S, Giardino L, Palazzi F, Asgary S. Management of Root Resorption Using Chemical Agents: A Review. Iran Endod J. 2016;11(1):1–7. doi: 10.7508/iej.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Esnaashari E, Pezeshkfar A, Fazlyab M. Nonsurgical Management of an Extensive Perforative Internal Root Resorption with Calcium-Enriched Mixture Cement. Iran Endod J. 2015;10(1):75–8. [PMC free article] [PubMed] [Google Scholar]
- 31.Stropko J. Invasive Cervical Resorption (ICR): A Description, Diagnosis and Discussion of Optional Management-A Review of Four Long-Term Cases. Roots. 2012;4:6–16. [Google Scholar]
- 32.Asgary S, Nosrat A. Conservative Management of Class 4 Invasive Cervical Root Resorption Using Calcium-Enriched Mixture Cement. J Endod. 2016;42(8):1291–4. doi: 10.1016/j.joen.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 33.Asgary S, Roghanizadeh L. Successful Management of a Typical Class 3 Invasive Cervical Root Resorption with Modified Pulpotomy: A Case Report. Iran Endod J. 2024;19(1):56–60. doi: 10.22037/iej.v19i1.44253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lewusz-Butkiewicz K, Kaczor-Wiankowska K, Kulas-Bałaban KW, Szmidt-Kądys M. Treatment of External Cervical Resorption and Its Late Complication: A Case Report. Iran Endod J. 2022;17(1):48–51. doi: 10.22037/iej.v17i1.36672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asgary S, Nosrat A. Conservative Management of Class 4 Invasive Cervical Root Resorption Using Calcium-enriched Mixture Cement. J Endod. 2016;42(8):1291–4. doi: 10.1016/j.joen.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 36.Asgary S, Alim Marvasti L, Kolahdouzan A. Indications and case Series of Intentional Replantation of Teeth. Iran Endod J. 2014;9(1):71–8. [PMC free article] [PubMed] [Google Scholar]
- 37.Eftekhar L, Ashraf H, Jabbari S. Management of Invasive Cervical Root Resorption in a Mandibular Canine Using Biodentine as a Restorative Material: A Case Report. Iran Endod J. 2017;12(3):386–9. doi: 10.22037/iej.v12i3.16668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Okamoto M, Asahi Y, Duncan HF, Kuriki N, Takahashi Y, Hayashi M. Repair of an Extensive External Cervical Resorption Lesion Using Intentional Replantation with Crown Rotation. Case Rep Dent. 2023;2023:2103999. doi: 10.1155/2023/2103999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Silveira LFM, Silveira CF, Martos J. Piovesan EM. Clinical Technique for Invasive Cervical Root Resorption. 2011; 14(4):440–4. doi: 10.4103/0972-0707.87225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bachesk AB, Queiroz AF, Bin LR, Bachesk AB, Pavan AJ. Clinical Approach to External Cervical Resorption in the Anterior Teeth: A Case Report Study. Iran Endod J. 2021;16(2):118–22. doi: 10.22037/iej.v16i2.32373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Emery C. External Cervical Resorption: A Case Study Using Orthodontic Extrusion. Dent Update. 1996;23(8):325–8. [PubMed] [Google Scholar]
- 42.Heithersay GS. Treatment of Invasive Cervical Resorption: an Analysis of Results using Topical Application of Trichloracetic Acid, Curettage, and Restoration. Quintessence Int. 1999;30(2):96–110. [PubMed] [Google Scholar]
- 43.Mohammad-Rahimi H, Dianat O, Abbasi R, Zahedrozegar S, Ashkan A, Motamedian SR, Rohban MH, Nosrat A. Artificial Intelligence for Detection of External Cervical Resorption Using Label-Efficient Self-Supervised Learning Method. J Endod. 2023;S0099-2399:23)00722–7. doi: 10.1016/j.joen.2023.11.004. [DOI] [PubMed] [Google Scholar]