Abstract
Introduction:
This non-randomized clinical trial investigated the outcomes of full pulpotomy in adult molars with irreversible pulpitis, comparing those with calcified and non-calcified pulp chambers over 6 and 12 months.
Materials and Methods:
A total of 101 adult permanent molars with irreversible pulpitis, in individuals over 12 years old, were categorized based on pulp chamber calcification observed in radiographic images by two endodontists. Subsequently, full pulpotomy procedures were performed, achieving hemostasis, and applying a 2 mm layer of calcium-enriched mixture (CEM) cement as a pulp covering agent. After 48 hours, the setting of the CEM cement was verified, followed by the application of a layer of resin-modified glass-ionomer. The tooth was then restored using amalgam. Clinical and radiographic evaluations were conducted at 6-month and 1-year follow-ups by blinded endodontists. Success rates were compared using Fisher's exact test and logistic regression tests with a significance level of 0.05.
Results:
Among the 97 patients with 6-month and 1-year follow-ups, all achieved clinical success. Radiographic success rates were 99% at 6 months and 96.9% at 1 year, regardless of pulp calcification. In the 6-month follow-up, success rates were 98.07% for non-calcified pulp chambers and 100% for calcified pulp chambers. At the 1-year follow-up, success rates were 96.1% and 97.8%, respectively. Statistical analysis showed no significant difference in radiographic success rate between the two groups at both follow-ups (P>0.05).
Conclusions:
Full pulpotomy using CEM cement is a successful treatment for adult permanent teeth with calcified and non-calcified pulp chambers presenting signs and symptoms of irreversible pulpitis up to a 1-year follow-up. This study provides compelling evidence that vital pulp therapy can be effectively employed in the pulpotomy of calcified teeth, at least in the short term.
Key Words: Calcified Teeth, Calcium-Enriched Mixture, CEM Cement, Full Pulpotomy, Deep Caries, Irreversible Pulpitis, Vital Pulp Therapy
Introduction
Dental caries stands as the most widespread non-infectious disease globally, with a significant prevalence that impacts diverse age groups and disadvantaged populations [1]. The Global Burden of Disease report revealed a striking statistic: untreated caries in permanent teeth affected 2.3 billion individuals between1990 to 2017 [2]. In instances where caries progression extends to the dentin without treatment, the dental pulp reacts with inflammation, eventually leading to necrosis and infection [1]. Root canal treatment (RCT), vital pulp therapy (VPT), and tooth extraction constitute the range of treatment options for teeth afflicted with irreversible pulpitis (IP).
RCT for vital teeth demonstrates notably high success rates. However, the long-term survival of endodontically-treated teeth lags behind that observed in vital teeth [3]. Factors contributing to this difference include the decline in sensory and immune functions, as well as the loss of structural integrity following pulp removal [3, 4]. VPT offers a method to protect the life and function of exposed dental pulp caused by caries, trauma, or dental treatments [5]. This approach aims to postpone the necessity for RCT, which could lead to intricate dental procedures, potentially compromising the long-term viability of tooth in comparison to preserving its natural pulp [6].
VPT was initially recommended primarily for immature and young patients [7-9]. However, it has demonstrated effectiveness for mature permanent teeth with carious exposure, as well as cases of IP [10, 11]. The lower cost and time associated with VPT make it a viable alternative to tooth extraction or even RCT [12, 13]. The improvement of VPT techniques, encompassing full, partial and miniature pulpotomy procedures [14], has been propelled by an enhanced comprehension of the defensive and reparative responses exhibited by the dentin-pulp complex when subjected to various stimuli. This understanding, combined with the development of biocompatible pulp capping agents like mineral trioxide aggregate (MTA), has established the reliability of these treatments both in clinical and histological outcomes [1, 15, 16].
MTA as a bioactive endodontic cement (BEC), is frequently used for its compatibility with vital tissues and sealing abilities, resulting in positive outcomes for VPTs [17]. Direct contact with MTA induces heightened activation of dental pulp cells, potentially leading to more efficient pulpal repair and a faster, reliably predictable formation of reparative dentin (11). Additionally, MTA, when in direct contact with pulp cells, stimulates the secretion of vascular endothelial growth factor, supporting the transformation of these cells into odontoblast-like cells and promoting dentinal bridge formation [18].
Calcium-enriched mixture (CEM) cement is a bioactive endodontic material with antibacterial properties and the ability to promote hard tissue formation. It demonstrates comparable efficacy to MTA in various VPTs; its advantages include a quicker setting time, simplified application, and a lower risk of tooth discoloration [19]. A recent systematic review underscored the consistent success of using MTA and other bioactive endodontic cement as pulp capping materials in VPTs, achieving a commendable 93% success rate irrespective of method, tooth developmental stage, or pre-treatment tooth condition [20].
Stem cells play a crucial role in continual tissue regeneration throughout life. However, factors like aging, reparative dentin deposition, trauma, attrition, and recurrent caries can diminish root canal and pulp chamber dimensions, hindering stem cell function and, subsequently, dental pulp regeneration. Notably, studies indicate that metabolic activity endures in the dental pulp cells of elderly individuals, capable of producing pro-inflammatory and matrix-degrading molecules. MicroRNAs and exosomes derived from dental pulp stem cells are emerging as potential treatments for age-related dental issues [21]. Thus, the removal of stimuli and necrotic pulp tissue, followed by the application of a bioactive material for pulp coverage, may establish an optimal environment for pulp recovery, even in calcified teeth.
Despite the substantial body of research on the success of BECs in VPTs, there is a notable absence of studies investigating this approach in the context of aged and calcified teeth. Given the innate regenerative potential of dental pulp and the regenerative properties of pulp stem cells in calcified teeth, it is plausible that effective VPT in calcified teeth can be achieved. Considering the less difficulty and better cost-effectiveness nature of VPT in contrast to RCT, as well as its capacity to conserve tooth structure, this study aims to evaluate the clinical and radiographic outcomes of full pulpotomy in calcified teeth afflicted with IP comparing to non-calcified pulp chambers.
Materials and Methods
Ethical approval for this non-randomized clinical trial was secured from the Ethics and Research Committee, registered under number IRCT2016051027738N2. The study adhered to ethical principles outlined in the Helsinki Declaration [22]. Prior to initiating the treatment, informed consent was obtained from all patients. As part of the ethical protocol, patients were provided the option of free RCT as compensation in the event of treatment failure.
Patient Selection Criteria
In this clinical trial intervention was conducted on all patients referred to the Endodontic Department of Kerman Faculty of Dentistry within a one-year period, based on specific inclusion criteria. The criteria for participation were as follows:
-Vital mature permanent first and second molars with cariously exposed pulp;
-Presence or absence of pain history indicative of IP (lingering pain persisting for more than 10 seconds post-stimulant elimination indicating IP;
-Presence or absence of clinical and radiographic signs of apical periodontitis (AP);
-Positive responses to both cold test (Endo-Frost; Roeko, Langenau, Germany) and electric pulp test (The Elements Diagnostic Unit; SybronEndo, CA, USA), the confirmation of vitality was the observing bleeding after pulp exposure;
-Teeth devoid of localized/generalized periodontal diseases (probing depth ≤3 mm), root resorption;
-Patients exhibiting good oral hygiene and lacking systemic diseases, pregnancy or physical/intellectual disabilities;
-Age of 12 years or older; and
-Requirement for patients to provide informed consent and be available for follow-up appointments.
Exclusion Criteria
The exclusion criteria included the following:
-Negative response to sensitivity tests (cold and electric tests);
-Presence of swelling or sinus tract;
-Uncontrollable bleeding during pulpotomy that persisted after applying a cotton pellet soaked in 5.25% NaOCl for 10 min;
-Lack of bleeding from the canal orifices indicating pulp necrosis or partial necrosis;
-Requirement for intrapulpal injection during treatment; and
-Deemed non-restorable by amalgam based on established definitions and protocols, as well as cases necessitating post placement into the root canal.
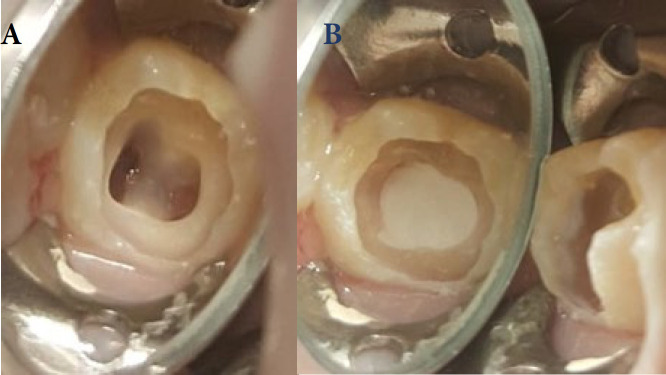
Tooth Selection Criteria
Pulp chamber calcification was defined as a distinct radiopaque mass present within the entire pulp chamber or a portion thereof, accompanied by a reduction in the size of the pulp chamber. When the pulp chamber was completely radiolucent, the tooth was scored as having no pulp chamber calcification (Figure 1) [16]. Each of the two experts independently evaluated 20 periapical radiographs for inter-rater agreement. The calculated kappa coefficient was 97%. In cases of disagreement, a third experienced endodontist was consulted for resolution.
Figure 1.
Teeth were categorized into two groups based on the presence of calcification in their pulp chambers. The upper cases represent individuals with young non-calcified pulp, while the lower cases indicate those with calcified pulp chambers
Periapical radiographic images were taken using analog radiographic film (E-speed film, Skydent, Slovakia) with the parallel technique, utilizing a film holder (XCP; Rinn Co, Elgin, IL, USA), and maintaining consistent exposure conditions (70 kVp, 8 mA, and 0.2 s).
Determining Sample Size
To establish the sample size, a 5% type I error and a 20% type II error were considered, the expected success rate for VPT of non-calcified teeth and calcified teeth were considered 95% and 75%, respectively, and dropout rate 10%, resulting in a calculated sample size of 108 for comparing the two experimental groups.
Clinical Procedure
The full pulpotomy technique involved a sequential series of steps. Prior to initiating treatment, patients were instructed to rinse their mouths with 0.2% chlorhexidine mouthwash (Shahredaru, Iran). Following this, a 2% lidocaine with 1:80,000 epinephrine (Darupakhsh, Tehran, Iran) was administered via an inferior alveolar nerve block for mandibular teeth and buccal infiltration for maxillary teeth. Isolation was achieved using a rubber dam. Caries removal was performed with a low-speed carbide bur.
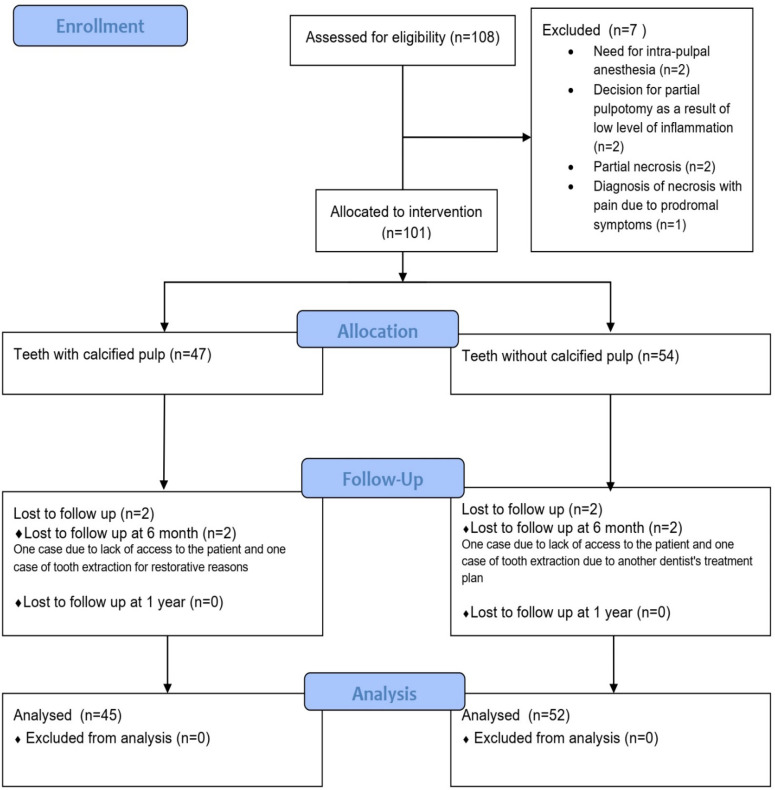
Upon pulp exposure, pulp vitality was confirmed by the presence of bleeding from pulp tissue. Subsequently, a sterile diamond bur (Diatech, Heerbrugg, Switzerland) and a high-speed handpiece (NSK, York, Japan) with water cooling were employed, extending to the orifice of the canals to complete the pulpotomy (Figure 2A). Hemostasis was achieved by irrigating the cavity with sterile normal saline, followed by the application of a sterile cotton pellet moistened with 5.25% NaOCl for 2 minutes, with the possibility of repetition up to 10 minutes. Afterward, CEM cement (BionqueDent; Tehran, Iran) was prepared according to the manufacturer's instructions. A 2 mm layer of CEM cement was applied to the clot-free pulp tissue at the orifice of the canals, followed by a layer of sterile cotton moistened with normal saline (Figure 2B). The tooth was temporarily restored with Coltosol (Golchai, Tehran, Iran). After 48 hours, the temporary dressing was removed, and following the confirmation of CEM cement setting, a layer of glass ionomer (GC Fuji II LC, GC Corp, Tokyo, Japan) was placed and cured for 20 seconds. Next, the tooth was permanently restored with amalgam (110-PLUS, China).
Figure 2.
A) The removal of pulp tissue was done by the high speed handpiece and continuous coolant and the pulp was cut to the canal orifices; B) CEM cement was prepared and placed on clot-free pulp tissue at canal orifices and the whole pulp chamber floor
All treatment procedures were performed within the department of Endodontics. The procedures were carried out on patients referred to the center between May 2015 and May 2016.
Evaluation
Clinical and radiographic evaluations were performed at 6 months and 1 year post-treatment. For patients experiencing severe/intolerable pain during follow-up, RCT was conducted. Amalgam restorations were also assessed in follow-up sessions, and if necessary, the restoration was replaced. Outcomes were determined based on predefined clinical and radiographic criteria [23]. Clinical failures included spontaneous pain, pain upon percussion and palpation, swelling, sinus tracts, mobility, and pocket formation. Radiographic success criteria during follow-up assessments included the absence of periapical radiolucency (PA index≤2) and no evidence of internal or external root resorption.
Blinding
Outcome measurements were performed by two independent board-certified endodontists who were blinded to the group assignments.
Statistical analysis
Fisher's exact test was used to compare success between the two groups. Additionally, a logistic regression model was utilized to control for potential confounding effects of other variables such as age, gender, jaw under treatment, and the presence of previous restoration. The statistical significance was set at 5% level of significance.
Results
A total of 108 patients were enrolled in the study according to the defined inclusion criteria. Initially, 7 patients were excluded from the study due to the following reasons: two cases necessitated intrapulpal anesthesia during treatment, two cases demonstrated partial necrosis, one case displayed complete necrosis with prodromal symptoms mimicking pulpal pain caused by herpes infection, and two cases were excluded due to limited inflammation spread, necessitating partial pulpotomy instead of full pulpotomy. After completing the treatment, post-treatment assessments were carried out on the 101 patients who had undergone full pulpotomy (Figure 3).
Figure 3.
Flow chart of 1 year follow-up
Out of the 101 patients, 73 were women and 28 were men. The participants' ages ranged from 12 to a maximum of 72 years. The mean age of the non-calcified group was lower than the calcified group (P<0.001). However, no significant distinction was observed between the two groups regarding sex, treated jaw, or the presence of prior restorations (Table 1).
Table 1.
Comparison of background variables between two groups
| Variables | n | Calcified Pulp Chamber | Non-calcified Pulp Chamber | P -value |
|---|---|---|---|---|
| Age [year(SD)] | 71.7 (09.24) | 26.7 (26.46) | <0.001 | |
| Sex [(%) n] | Male | (48.31) 17 | (40.23) 11 | 0.36 |
| Female | (51.68) 37 | (59.76) 36 | ||
| Jaw Treated [(%) n] | Maxillary | (44.44) 24 | (82.63) 30 | 0.06 |
| Mandible | (55.55) 30 | (17.36) 17 | ||
| Previous Restoration [(%) n] | Yes | (92.25) 14 | (55.42) 20 | 0.08 |
| No | (07.74) 40 | (44.57) 27 |
In the six-month follow-up, four more participants were excluded from the study. Two participants did not come for follow-up, and two others had their teeth extracted for reasons that were not related to the treatment. In total, 97 patients (~ 96%) took part in the follow ups after 6 months and one year.
Among the 97 patients with 6-month and 1-year follow-ups, all achieved clinical success in both periods. The radiographic success rate, regardless of pulp status in terms of calcification, was 99% at the 6-month and 96.9% at one year follow-up. In the assessment of radiographic success, during the 6-month follow-up, one case of VPT failure was observed in the group without pulp chamber calcification. The radiographic success rate during the first 6 months was 98.07% for the non-calcified group and 100% for the calcified group. During the 1-year follow-up, three other cases of treatment failure were observed during the radiographic examinations. Two of these cases were associated with non-calcified pulp chambers, while one case was observed in the group with calcified pulp chambers. In total, in the one-year follow-up, the radiographic success rate was reported as 96.1% in the non-calcified group and 97.8% in the calcified group. The statistical analysis showed that radiographic success after 6 months (P=0.999) and one year (P=0.999) was not significantly different.
During the 1-year follow-up, 81.2% of patients demonstrated restorations without any signs of defects. In 18 cases, the defects of restorations were successfully fixed and the teeth were restored after the patients returned. Only one case was excluded from the study due to experiencing a cusp fracture three months after VPT which was not restorable.
The multivariate analysis revealed that the variables of age, gender, tooth position in the jaw, restoration before treatment were not confounders for the effect of pulp chamber calcification on radiographic outcome in 6 and 12 months follow-ups (P>0.05).
Discussion
Based on the clinical/radiographic findings, we have determined that using the full pulpotomy method for VPT effectively treats teeth with IP, whether the teeth have calcified or non-calcified pulp. The consistently favorable outcomes observed in both clinical and radiographic evaluations strongly support the use of VPT in cases exhibiting signs and symptoms of IP. These results align with prior clinical studies that have similarly advocated for VPT in managing such cases [23-26]. Notably, our findings emphasize the suitability of VPT, specifically full pulpotomy, as a valuable/reliable treatment option for patients, particularly older individuals who may find extended chair-time challenging during traditional endodontic sessions, especially in the presence of pulp calcification. VPT is an efficient and time-saving alternative, making it a preferred choice in managing these challenging cases.
No previous studies have explored the outcomes of pulpotomy specifically on teeth with calcified pulp chambers. This study represents the first investigation into the success of VPT in calcified teeth. Aging induces notable changes in dental pulp, encompassing reductions in chamber and canal sizes, decreased pulp cellularity, diminished odontoblast size and number, a decline in blood vessels and nerves, and an increase in collagen fiber thickness [27]. Despite these age-related changes, dental pulp stem cells in elderly individuals maintain regenerative capabilities similar to their younger counterparts [28]. The expectation was that, through the removal of stimuli and the use of a biocompatible material, pulp repair could occur even in calcified teeth. In contrast to a retrospective study on DPC using calcium hydroxide, which indicated lower success rates in patients over 60 [29], our study found a high success rate with full pulpotomy using CEM cement in teeth with calcified pulp chambers within a 1-year follow-up. Discrepancies between the studies may arise from factors such as the retention of inflamed pulp in the DPC procedure and the utilization of calcium hydroxide, a material known for its shortcomings in VPT.
Based on evidence-based medicine, there is a need for clinical trial documentation for the clinical application of treatment methods, and there was no clinical trial study with a high level of evidence to answer the question "Are VPT techniques effective treatments in cases with calcified pulp chamber?". Therefore, this study was designed. The highest level of evidence is obtained in randomized clinical trial studies, but randomization was not possible due to the nature of the question of the present study that the samples were placed in two groups with pulp chamber calcification and without calcification.
In this study, variables such as age, gender, jaw under treatment, and the presence of previous restoration did not significantly impact the treatment's success during both the 6- and 12-month follow-ups. This aligns with Kang et al.'s [30] findings, where age, gender, tooth type, and exposure type were reported as non-significant prognostic factors for the success of partial pulpotomy. A systematic review has highlighted the insufficiency of current evidence in thoroughly exploring the influence of a patient's age on the clinical outcomes of VPT. Nonetheless, it is noteworthy that the pulp tissue exhibits a generally high healing capacity in both young and older individuals when the root cause of the dental issue is effectively addressed [31]. A recent review by Duncan et al. [32] also suggested that age and gender do not appear to exert a significant influence on pulpotomy outcomes, emphasizing the absence of a dedicated study specifically designed to investigate these factors as primary objectives.
Over the last decade, advancements in pulp biology and the utilization of biomaterials have spurred studies into pulpotomy as a definitive treatment for adult permanent teeth affected by reversible and irreversible pulpitis. This procedure applies to permanent teeth with both open and closed apices, with greater success observed in patients with immature teeth [32]. In a study by Taha et al., [23] the efficacy of full pulpotomy using Biodentine in mature teeth with signs of IP was explored. Their 6-month follow-up demonstrated clinical/radiographic success rates of 98.4%, while the 1-year follow-up reported clinical success at 100% and radiographic success at 98.4%. Aguilar et al., [31].in a systematic review, reported a 94% success rate for full pulpotomy in patients ranging from 6 to 70 years old with carious pulp exposure, within a 6-month to 1-year follow-up period In another systematic review, Cushley found that pulpotomy in teeth with carious pulp exposure and signs of IP achieved clinical and radiographic success rates of 97.4% and 95.4%, respectively, at the 1-year follow-up [33]. Our study, focusing on mature teeth with carious pulp exposure and signs of IP in patients aged 12 to 72 years, showed radiographic success rates for full pulpotomy of 99% at the 6-month follow-up and 96.9% at the 1-year follow-up, aligning closely with the outcomes reported in the previous studies.
In our study, CEM cement was chosen as the pulp-capping biomaterial. A 2021 systematic review highlighted the efficacy of contemporary bioactive materials in VPT, demonstrating an impressive 93% success rate. Interestingly, factors such as the underlying cause of pulp disease, the specific material used, and the initial diagnosis before the procedure did not significantly impact treatment outcomes [20]. The market has recently seen the introduction of numerous bioactive materials with functionalities akin to MTA. The aim behind developing and introducing these materials is to retain and improve upon favorable characteristics while addressing any limitations of their predecessors [17]. Nevertheless, the comparative superiority of these materials to MTA in the realm of VPT necessitates further exploration through rigorous clinical trials.
CEM cement, a bioactive endodontic material, shares similarities with MTA in terms of cytotoxicity, genotoxicity, and its capacity to promote osteogenic, dentinogenic, cementogenic, and sealing properties [34-37]. Remarkably, this bioactive cement possesses the ability to induce stem cell differentiation and stimulate the formation of hard tissues [34, 38]. In addition, it demonstrates antibacterial properties equivalent to calcium hydroxide and superior to MTA [39]. Furthermore, CEM cement boasts a shorter primary setting time compared to MTA [34]. In cases of pulpotomy for teeth diagnosed with IP, CEM cement has been shown to provide faster pain relief compared to RCT [24]. In a study by Asgary et al., [25].VPT using CEM cement was compared to RCT in permanent molars with IP, revealing that VPT achieved similar clinical success and higher radiographic success rates than RCT at both the 6- and 12-month follow-ups Additionally, in a multi-center study, the outcomes of VPT specifically full pulpotomy using MTA and CEM cement did not exhibit any significant differences in terms of treatment success [26].
Spontaneous and chronic pain have been proposed as clinical indicators of irreversible pulp inflammation [40]. However, contemporary perspectives, considering clinical, biological, and theoretical factors, have led to ongoing debates about categorizing pulp disease as truly irreversible [41, 42] and re-nomenclature [43]. Many studies emphasize the importance of "bleeding time" as a critical parameter to distinguish between reversible and irreversible pulp conditions. If bleeding cannot be controlled within 5 to 10 minutes, it indicates severe pulp inflammation, prompting a recommendation for pulpectomy [41]. In our current research, we specifically included teeth displaying clinical signs of IP. Following pulp exposure, we observed bleeding from all openings, setting a maximum time limit of 10 minutes for inclusion in our study. The success rate exceeding 97%, particularly the absence of immediate failures, underscores the precision of clinical diagnosis and judgment regarding the extent of pulp inflammation. This approach aligns with the conclusions drawn in previous studies [23]. There is an increasing body of evidence advocating for the application of VPT in teeth, regardless of whether clinical signs and symptoms indicate reversible pulpitis or IP, such as the presence of excessive hemorrhage [32, 44-46].
In our study, hemostasis was achieved by applying cotton pellets soaked in a 5.25% NaOCl solution. This solution can be safely employed at various concentrations in direct contact with pulp tissue without compromising the pulp's integrity [41]. The antimicrobial properties of NaOCl offer several advantages, including its ability to induce hemostasis, chemically dissolve blood clots and fibrin, and effectively cleanse dentinal debris and damaged cells in areas of pulp exposure. Furthermore, NaOCl can disinfect the dentin-pulp surface and eliminate the smear layer [41]. Importantly, there is no evidence to suggest that NaOCl negatively affects cell differentiation or the deposition of hard tissue [41]. While chlorhexidine also possesses a wide range of antibacterial properties, it is worth noting that experiments involving gingival fibroblast cell cultures have shown chlorhexidine to exhibit greater toxicity compared to NaOCl [47]. As a result, we chose to use NaOCl in our study.
In our study, we observed 19 cases of restoration defects within one year, encompassing instances of caries recurrence, restoration fractures, and cusp fractures. Of these cases, 18 were successfully restored, but unfortunately, one case resulted in a non-restorable tooth fracture, leading to the necessity of tooth extraction. A study by Pratt et al. [48] underscored the substantial impact of the type of restoration used after RCT on tooth survival. Their findings revealed that teeth treated with amalgam or composite build-up after RCT were 2.29 times more likely to be extracted compared to teeth that received crowns. It is important to note that all restorative procedures in our study were performed by an endodontic postgraduate student, and the operator's proficiency in restorative treatments could be considered a potential factor influencing the success or failure of these restorative interventions, ensuring a high level of internal validity. Due to the high technical sensitivity, challenges in isolating posterior teeth for composite restoration, limited restoration skills of the operator, and the heightened risk of caries in our patient population, we opted to use amalgam as the restorative material. A systematic review also reported no noticeable difference in the success of pulpotomy when using either amalgam or composite as the final restoration material in caries-exposed permanent teeth [49].
In our study, teeth were categorized based on the presence or absence of pulp chamber calcification. Those with a completely radiolucent pulp chamber were classified as having no calcification, while those exhibiting radiopacity within the pulp chamber or a narrow, disk-like appearance were designated as having calcification [50]. It is important to acknowledge that we did not assess the size/shape of the calcifications. A limitation of our study is the descriptive nature of the criteria used for this categorization; future research employing quantitative criteria could enhance the precision of study outcomes. Additionally, the one-year follow-up represents a short-term assessment, and extended monitoring over more prolonged periods is recommended for a comprehensive understanding of patients' conditions. When comparing VPT to RCT, VPT provides a simpler, more cost-effective approach with significant socio-economic implications for oral health and patient quality of life. However, continuous monitoring of patients receiving VPT for teeth with IP is essential over an extended period, similar to those undergoing RCT, underscoring the necessity for long-term recall to ensure timely intervention if needed. Early intervention is crucial to prevent the slow progression of asymptomatic pulp disease [20].
To improve the applicability of our study, we recommend replicating similar investigations with diverse practitioners and larger patient groups for broader relevance. Additionally, exploring alternative VPT techniques, like partial pulpotomy and direct pulp capping, in teeth with calcification compared to those without, could provide valuable insights.
Conclusion
This study affirms the efficacy of VPT with CEM cement for treating IP, irrespective of pulp chamber calcification. No significant disparities in clinical and radiographic success were noted between calcified and non-calcified groups during the 6-month and one-year follow-up. Age, gender, treated jaw, and pre-treatment restorations were not influential factors in VPT success. This establishes pulpotomy as a viable alternative to RCT or extraction in calcified teeth, providing novel evidence for the effective application of VPT in such cases.
Acknowledgments
We express our sincere gratitude to the Endodontology Research Center at Kerman University of Medical Sciences for their support.
Conflict of interest
None.
Funding support
This research was partially funded by Kerman University of Medical Sciences (grant number: 94/646).
Authors' contributions
Conceptualization: A. Shahravan Data Curation: A. Shahravan, A. Farhadi, H. Manochehrifar. Formal Analysis: A. Shahravan, AH. Nekouei. Methodology: A. Shahravan. Project Adminstration: A. Shahravan, H. Manochehrifar. Validation: A. Shahravan, Anahita Safarzadeh, H. Manochehrifar. Writing- Original Draft: All authors. Writing- Review & Editing: All authors.
Informed consent:
Written informed consent was obtained from the patients.
References
- 1.Bjørndal L, Simon S, Tomson PL, Duncan HF. Management of Deep Caries and the Exposed Pulp. Int Endod J. 2019;52(7):949–73. doi: 10.1111/iej.13128. [DOI] [PubMed] [Google Scholar]
- 2.Bernabe E MW, Hernandez CR, Bailey J, et al. Global, Regional, and National Levels and Trends in Burden of Oral Conditions from 1990 to 2017: A Systematic Analysis for the Global Burden of Disease 2017 Study. J Dent Res. 2020;99(4):362–73. doi: 10.1177/0022034520908533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caplan DJ, Cai J, Yin G, White BA. Root Canal Filled Versus Non-Root Canal Filled Teeth: A Retrospective Comparison of Survival Times. J Public Health Dent. 2005;65(2):90–6. doi: 10.1111/j.1752-7325.2005.tb02792.x. [DOI] [PubMed] [Google Scholar]
- 4.Awawdeh L, Hemaidat K, Al-Omari W. Higher Maximal Occlusal Bite Force in Endodontically Treated Teeth Versus Vital Contralateral Counterparts. J Endod. 2017;43(6):871–5. doi: 10.1016/j.joen.2016.12.028. [DOI] [PubMed] [Google Scholar]
- 5.Wells C DC, McCormack S. Vital Pulp Therapy for Endodontic Treatment of Mature Teeth: A Review of Clinical Effectiveness, Cost-Effectiveness, and Guidelines [Internet] Canadian Agency for Drugs and Technologies in Health; 2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546327. [PubMed] [Google Scholar]
- 6.Ghoddusi J, Forghani M, Parisay I. New Approaches in Vital Pulp Therapy in Permanent Teeth. Iran Endod J. 2014;9(1):15–22. [PMC free article] [PubMed] [Google Scholar]
- 7.Nosrat A, Asgary S. Apexogenesis of a Symptomatic Molar with Calcium Enriched Mixture. Int Endod J. 2010;43(10):940–4. doi: 10.1111/j.1365-2591.2010.01777.x. [DOI] [PubMed] [Google Scholar]
- 8.Sharaan M, Ali A. Mineral Trioxide Aggregate vs Calcium-Enriched Mixture Pulpotomy in Young Permanent Molars with a Diagnosis of Irreversible Pulpitis: A Randomized Clinical Trial. Iran Endod J. 2022;17(3):106–13. doi: 10.22037/iej.v17i3.35706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sabbagh S, Sarraf Shirazi A, Eghbal MJ. Vital Pulp Therapy of a Symptomatic Immature Permanent Molar With Long-Term Success. Iran Endod J. 2016;11(4):347–9. doi: 10.22037/iej.2016.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asgary S, Fazlyab M, Sabbagh S, Eghbal MJ. Outcomes of Different Vital Pulp Therapy Techniques on Symptomatic Permanent Teeth: A Case Series. Iran Endod J. 2014;9(4):295–300. [PMC free article] [PubMed] [Google Scholar]
- 11.Ashraf H, Rahmati A, Amini N. Vital Pulp Therapy with Calcium-Silicate Cements: Report of Two Cases. Iran Endod J. 2017;12(1):112–5. doi: 10.22037/iej.2017.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leong DJX, Yap AU. Vital Pulp Therapy in Carious Pulp-Exposed Permanent Teeth: An Umbrella Review. Clin Oral Investig. 2021;25(12):6743–56. doi: 10.1007/s00784-021-03960-2. [DOI] [PubMed] [Google Scholar]
- 13.Yazdani S, Jadidfard MP, Tahani B, Kazemian A, Dianat O, Alim Marvasti L. Health Technology Assessment of CEM Pulpotomy in Permanent Molars with Irreversible Pulpitis. Iran Endod J. 2014;9(1):23–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Asgary S, Nourzadeh M, Eghbal MJ. Miniature Pulpotomy of Symptomatic Mature Permanent Teeth: A Report of Two Cases. Iran Endod J. 2016;11(1):75–8. doi: 10.7508/iej.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asgary S, Parirokh M, Eghbal MJ, Ghoddusi J, Eskandarizadeh A. SEM Evaluation of Neodentinal Bridging after Direct Pulp Protection with Mineral Trioxide Aggregate. Aust Endod J. 2006;32(1):26–30. doi: 10.1111/j.1747-4477.2006.00004.x. [DOI] [PubMed] [Google Scholar]
- 16.Cushley S, Duncan HF, Lappin MJ, Chua P, Elamin AD, Clarke M, El-Karim IA. Efficacy of Direct Pulp Capping for Management of Cariously Exposed Pulps in Permanent Teeth: A Systematic Review and Meta-Analysis. Int Endod J. 2021;54(4):556–71. doi: 10.1111/iej.13449. [DOI] [PubMed] [Google Scholar]
- 17.Parirokh M, Torabinejad M, Dummer PMH. Mineral Trioxide Aggregate and other Bioactive Endodontic Cements: An Updated Overview-Part I: Vital Pulp Therapy. Int Endod J. 2018;51(2):177–205. doi: 10.1111/iej.12841. [DOI] [PubMed] [Google Scholar]
- 18.Paranjpe A, Smoot T, Zhang H, Johnson JD. Direct Contact with Mineral Trioxide Aggregate Activates and Differentiates Human Dental Pulp Cells. J Endod. 2011;37(12):1691–5. doi: 10.1016/j.joen.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Utneja S, Nawal RR, Talwar S, Verma M. Current Perspectives of Bio-Ceramic Technology in Endodontics: Calcium Enriched Mixture Cement-Review of Its Composition, Properties and Applications. Restor Dent Endod. 2015;40(1):1–13. doi: 10.5395/rde.2015.40.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sabeti M, Huang Y, Chung YJ, Azarpazhooh A. Prognosis of Vital Pulp Therapy on Permanent Dentition: A Systematic Review and Meta-analysis of Randomized Controlled Trials. J Endod. 2021;47(11):1683–95. doi: 10.1016/j.joen.2021.08.008. [DOI] [PubMed] [Google Scholar]
- 21.Iezzi I, Pagella P, Mattioli-Belmonte M, Mitsiadis TA. The Effects of Ageing on Dental Pulp Stem Cells, the Tooth Longevity Elixir. Eur Cell Mater. 2019;37:175–85. doi: 10.22203/eCM.v037a11. [DOI] [PubMed] [Google Scholar]
- 22.World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA. 2013;310(20):2191–4. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 23.Taha NA, Abdelkhader SZ. Outcome of Full Pulpotomy Using Biodentine in Adult Patients with Symptoms Indicative of Irreversible Pulpitis. Int Endod J. 2018;51(8):819–28. doi: 10.1111/iej.12903. [DOI] [PubMed] [Google Scholar]
- 24.Asgary S, Eghbal MJ. The Effect of Pulpotomy using a Calcium-Enriched Mixture Cement versus One-Visit Root Canal Therapy on Postoperative Pain Relief in Irreversible Pulpitis: A Randomized Clinical Trial. Odontology. 2010;98(2):126–33. doi: 10.1007/s10266-010-0127-2. [DOI] [PubMed] [Google Scholar]
- 25.Asgary S, Eghbal MJ, Ghoddusi J, Yazdani S. One-Year Results of Vital Pulp Therapy in Permanent Molars with Irreversible Pulpitis: An Ongoing Multicenter, Randomized, Non-Inferiority Clinical Trial. Clin Oral Investig. 2013;17(2):431–9. doi: 10.1007/s00784-012-0712-6. [DOI] [PubMed] [Google Scholar]
- 26.Asgary S, Eghbal MJ. Treatment Outcomes of Pulpotomy in Permanent Molars with Irreversible Pulpitis Using Biomaterials: A Multi-Center Randomized Controlled Trial. Acta Odontol Scand. 2013;71(1):130–6. doi: 10.3109/00016357.2011.654251. [DOI] [PubMed] [Google Scholar]
- 27.Burke FM, Samarawickrama DY. Progressive Changes in the Pulpo-Dentinal Complex and Their Clinical Consequences. Gerodontology. 1995;12(12):57–66. doi: 10.1111/j.1741-2358.1995.tb00132.x. [DOI] [PubMed] [Google Scholar]
- 28.Bressan E, Ferroni L, Gardin C, Pinton P, Stellini E, Botticelli D, Sivolella S, Zavan B. Donor Age-Related Biological Properties of Human Dental Pulp Stem Cells Change in Nanostructured Scaffolds. PLoS One. 2012;7(11):e49146. doi: 10.1371/journal.pone.0049146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dammaschke T, Leidinger J, Schäfer E. Long-term Evaluation of Direct Pulp Capping-Treatment Outcomes Over an Average Period Of 6 1 Years. Clin Oral Investig. 2010;14(5):559–67. doi: 10.1007/s00784-009-0326-9. [DOI] [PubMed] [Google Scholar]
- 30.Kang CM, Sun Y, Song JS, Pang NS, Roh BD, Lee CY, Shin Y. A Randomized Controlled Trial of Various MTA Materials for Partial Pulpotomy in Permanent Teeth. J Dent. 2017;60:8–13. doi: 10.1016/j.jdent.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 31.Aguilar P, Linsuwanont P. Vital Pulp Therapy in Vital Permanent Teeth with Cariously Exposed Pulp: A Systematic Review. J Endod. 2011;37(5):581–7. doi: 10.1016/j.joen.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 32.Duncan HF, El-Karim I, Dummer PMH, Whitworth J, Nagendrababu V. Factors That Influence the Outcome of Pulpotomy in Permanent Teeth. Int Endod J. 2023;56 Suppl 2:62–81. doi: 10.1111/iej.13866. [DOI] [PubMed] [Google Scholar]
- 33.Cushley S, Duncan HF, Lappin MJ, Tomson PL, Lundy FT, Cooper P, Clarke M, El Karim IA. Pulpotomy for Mature Carious Teeth with Symptoms of Irreversible Pulpitis: A Systematic Review. J Dent. 2019;88:103158. doi: 10.1016/j.jdent.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 34.Asgary S, Shahabi S, Jafarzadeh T, Amini S, Kheirieh S. The Properties of a New Endodontic Material. J Endod. 2008;34(8):990–3. doi: 10.1016/j.joen.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 35.Naghavi N, Ghoddusi J, Sadeghnia HR, Asadpour E, Asgary S. Genotoxicity and Cytotoxicity of Mineral Trioxide Aggregate and Calcium Enriched Mixture Cements on L929 Mouse Fibroblast Cells. Dent Mater J. 2014;33(1):64–9. doi: 10.4012/dmj.2013-123. [DOI] [PubMed] [Google Scholar]
- 36.Asgary S, Alim Marvasti L, Kolahdouzan A. Indications and Case Series of Intentional Replantation of Teeth. Iran Endod J. 2014;9(1):71–8. [PMC free article] [PubMed] [Google Scholar]
- 37.Asgary S, Verma P, Nosrat A. Treatment Outcomes of Full Pulpotomy as an Alternative to Tooth Extraction in Molars with Hyperplastic/Irreversible Pulpitis: A Case Report. Iran Endod J. 2017;12(2):261–5. doi: 10.22037/iej.2017.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Asgary S. Micro-computed Tomography Assessment of Full Pulpotomy in a Mature Molar after Five Years: A Case Report. Iran Endod J. 2022;17(4):223–4. doi: 10.22037/iej.v17i4.39717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Asgary S, Kamrani FA. Antibacterial Effects of Five Different Root Canal Sealing Materials. J Oral Sci. 2008;50(4):469–74. doi: 10.2334/josnusd.50.469. [DOI] [PubMed] [Google Scholar]
- 40.Carrotte P, Association BD. A Clinical Guide to Endodontics: British Dental Association. 2003. [Google Scholar]
- 41.AAE Position Statement on Vital Pulp Therapy. J Endod. 2021;47(9):1340–4. doi: 10.1016/j.joen.2021.07.015. [DOI] [PubMed] [Google Scholar]
- 42.Asgary S, Eghbal MJ. Challenging the Misnomer of Irreversible Pulpitis and Deliberating the Urgent Need for Reclassification of Pulpal Diseases Based on the Efficacy of Vital Pulp Therapies: An Overview of Systematic Reviews. Iran Endod J. 2023;18(4):202–5. doi: 10.22037/iej.v18i4.43035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eghbal MJ, Asgary S. Reconsidering the Nomenclature of Irreversible Pulpitis: A Call for Change. Iran Endod J. 2023;18(4) doi: 10.22037/iej.v18i4.43217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Asgary S, Kemal Çalışkan M. Vital Pulp Therapy of a Mature Molar with Concurrent Hyperplastic Pulpitis, Internal Root Resorption and Periradicular Periodontitis: A Case Report. Iran Endod J. 2015;10(4):284–6. doi: 10.7508/iej.2015.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Asgary S, Roghanizadeh L. Tampon Pulpotomy: Long-term Successful Results of a Molar with Irreversible Pulpitis and Previous Vital Pulp Therapy Failure. Iran Endod J. 2023;18(3):165–7. doi: 10.22037/iej.v18i3.42508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ardavan A, Roghanizadeh L, Asgary S. Tampon Vital Pulp Therapy in the Management of Excessive Haemorrhage in Inflamed Pulps: A Hypothesis. Iran Endod J. 2023;18(4):274–6. doi: 10.22037/iej.v18i4.43232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bajrami D, Hoxha V, Gorduysus O, Muftuoglu S, Zeybek ND, Küçükkaya S. Cytotoxic Effect of Endodontic Irrigants In Vitro. Med Sci Monit Basic Res. 2014;20:22–6. doi: 10.12659/MSMBR.890247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pratt I, Aminoshariae A, Montagnese TA, Williams KA, Khalighinejad N, Mickel A. Eight-Year Retrospective Study of the Critical Time Lapse between Root Canal Completion and Crown Placement: Its Influence on the Survival of Endodontically Treated Teeth. J Endod. 2016;42(11):1598–603. doi: 10.1016/j.joen.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 49.Alqaderi H, Lee CT, Borzangy S, Pagonis TC. Coronal Pulpotomy for Cariously Exposed Permanent Posterior Teeth with Closed Apices: A Systematic Review and Meta-Analysis. J Dent. 2016;44:1–7. doi: 10.1016/j.jdent.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 50.Sener S, Cobankara FK, Akgünlü F. Calcifications of the Pulp Chamber: Prevalence and Implicated Factors. Clin Oral Investig. 2009;13(2):209–15. doi: 10.1007/s00784-008-0212-x. [DOI] [PubMed] [Google Scholar]