Abstract
Invasive cervical root resorption (ICRR) is a rare and clinically complex condition marked by the progressive loss of dental hard tissues below the junctional epithelium. This case report outlines the management of a 32-year-old female patient presenting with ICRR class 3 affecting a maxillary incisor. Despite the absence of symptoms, the expansive nature of the defect warranted conservative surgical intervention. The procedure involved the surgical removal of inflamed tissues, followed by an ultraconservative modified pulpotomy utilizing calcium-enriched mixture (CEM) cement through a surgical window. The selected intervention is substantiated by its potential benefits, such as minimal removal of tooth structure and the inherent biocompatibility and sealing capabilities of CEM cement. A one-year follow-up revealed arrested resorption, re-establishment of periodontal attachment, and successful esthetic restoration, affirming the efficacy of vital pulp therapy in surgically addressing advanced ICRR. Accurate diagnosis, strategic treatment planning, and a patient-centered approach proved critical in achieving favorable outcomes.
Key Words: Calcium-enriched Mixture, CEM Cement, Endodontics, Invasive Cervical Root Resorption, Pulpotomy, Vital Pulp Therapy
Introduction
Resorption is defined as a process in which parts of a tissue are degraded and lost physiologically or pathologically. In cases of tooth resorption, this process results in the loss of dentine, cementum, or bone, along with the loss of the periodontal ligament (PDL). Tooth resorption is broadly categorized into two types: internal and external tooth/root resorptions [1]. Internal root resorption (IRR) is characterized by the progressive damage of intracanal dentin caused by the activity of multinucleated giant or odontoclastic cells, leading to the replacement of dentin with granulation or abnormal mineralized tissue [2]. External root resorption (ERR) involves the loss of tissues on the outer surface of the tooth, potentially leading to tooth loosening and early loss [3]. Various chemicals have been employed to manage root resorption cases, including sodium hypochlorite (NaOCl), acids, acetazolamide, calcitonin, alendronate, Ledermix, Emdogain, and various biomaterials [4].
Invasive cervical root resorption (ICRR), as a form of ERR, is an uncommon yet clinically challenging condition [5]. It is characterized by the resorption of dental hard tissues on the tooth surface below the junctional epithelium, forming the area of connective tissue attachment [6]. This condition is primarily caused by odontoclastic cells of the periodontium penetrating the outer surface of the root in the cervical region [7]. Despite being silent, ICRR is considered an aggressive form of resorption, which, if left untreated, can lead to tooth mobility, functional impairment, and eventually tooth loss. ICRR is classified into four distinct classes based on the extent and severity of the resorption, each representing a unique clinical challenge [8]. Class 1 ICRR typically involves the coronal portion of the root with limited impact on surrounding structures. In Class 2 ICRR, resorption extends beyond the coronal dentin into the midroot, requiring more extensive intervention. Class 3 ICRR, the focus of the present case report, signifies extensive resorption that encroaches upon both coronal dentin and the mid-root region. Finally, Class 4 ICRR represents the most severe form, with resorption extending into the apical region and often causing significant tooth mobility. Despite its rarity, the management of ICRR class 3 and 4 demands immediate attention due to low success rates and often necessitates a multidisciplinary approach [9].
There have been numerous reports documenting the successful treatment of various types of root resorption, wherein either the entire canal space or the root-end was filled/sealed with calcium-enriched mixture (CEM) cement [10-13]. Nevertheless, with meticulous case selection, vital pulp therapy (VPT) involving CEM cement emerges as a recommended approach for cases of external root resorption (ERR) [14] or ERR/ICRR [15, 16]. The preference for this method is predominantly guided by the exceptional properties inherent in CEM cement, such as superior biocompatibility, effective sealability, and its potential to stimulate tissue regeneration [17, 18]. Furthermore, CEM, when combined with double antibiotic paste, has demonstrated successful management of trauma-induced inflammatory ERR with resistant apical infection [19]. The current case report not only reaffirms the efficacy of this suggested approach in resolving a complex ICRR lesion in a vital tooth but also underscores the substantial restorative and esthetic advantages it offers.
This report details a challenging clinical scenario involving a 32-year-old female patient with Class 3 ICRR in a maxillary incisor. Despite the absence of symptoms, the extensive nature of the resorptive defect mandated a decisive intervention. Addressing such complex ICRR cases poses a significant dilemma for clinicians, with surgical intervention often being the recommended course of action [8, 20, 21]. In this specific instance, we opted for a modified pulpotomy procedure using CEM cement. This case report serves as evidence of the potential of innovative strategies to effectively manage intricate ICRR cases while preserving both function and esthetics, ultimately promoting the well-being of the patient.
Case Presentation
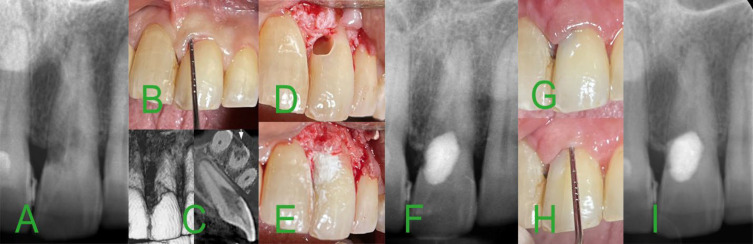
The case involves a 32-year-old female who was referred to our endodontic clinic following a routine dental check-up that revealed an asymptomatic lesion (Figure 1A). With no significant medical history, the patient reported no pain, sensitivity, or discomfort related to her upper incisor teeth. Clinical examination yielded normal findings (Figure 1B), and sensibility dental pulp testing on anterior teeth produced a normal/positive response. No history of previous orthodontic treatments or dental trauma was reported. Diagnostic periapical radiography identified a substantial resorption defect in the crown of tooth #21 (Figure 1A), leading to further assessment via cone-beam computed tomography (CBCT). The CBCT confirmed a large resorptive lesion extending into the mid-root of the tooth, with a mesio-buccal aspect perforation that was not covered by surrounding bone (Figure 1C).
Figure 1.
Clinical and Radiographic Progression of the Treatment of Invasive Cervical Root Resorption (ICRR) Class 3 in Tooth #21; A) Diagnostic periapical radiograph; illustrating the extensive resorption defect in the crown of tooth #21; B) Preoperative clinical photograph; showing the affected tooth with 3-mm periodontal probing depth; C) Cone-beam computed tomography images; demonstrating the resorptive lesion extended into the mid-root of the tooth, with a buccal aspect perforation; D) Intraoperative photograph; showcasing the modified pulpotomy procedure, with the inflamed tissues within the crown carefully curetted; E) Intraoperative photograph; displaying the application of calcium enriched mixture cement to fill and seal the pulp chamber and resorptive defect; F) Intraoperative periapical radiograph; confirming the successful pulpotomy and proper filling/sealing of the defect; G) Clinical photograph taken during the two-week post-treatment period; showing healthy and normal attached gingiva; H) Clinical photograph; indicating normal periodontal probing depths during clinical examination; I) Radiographic evaluation at one-year follow-up; demonstrating arrested resorption and healthy periapical area
Based on clinical and radiographic findings, the patient was diagnosed with asymptomatic pulpitis and Class 3 Invasive Cervical Root Resorption (ICRR) in tooth #21, characterized by extensive invasion of the resorbing tissue into the coronal dentin and midroot. Given the class 3 classification, treatment options were thoroughly discussed, and a conservative surgical intervention with ultraconservative pulp management (utilizing VPT with endodontic materials) was recommended. Alternative options included a surgical procedure with concurrent root canal therapy or a more invasive approach involving tooth extraction and replacement. The patient opted for the conservative surgical approach, and informed consent was obtained.
The procedure commenced with the initiation of an antibacterial (0.12% chlorhexidine) mouth rinse and the administration of local anesthesia with 2% lidocaine plus 1:80000 epinephrine (DarouPakhsh, Tehran, Iran) to ensure the patient's comfort. A mini full-thickness mucoperiosteal flap was carefully created to access the resorptive defect. Delicate curettage was performed on the inflamed tissues, including the affected dental pulp within the crown, as part of a modified pulpotomy procedure (Figure 1D). Limited access and the decision not to further open the surgical access via additional bone removal resulted in a portion of the apical resorptive tissues remaining untouched.
CEM cement (BioniqueDent, Tehran, Iran) was selected as the pulp-protecting and reparative biomaterial, filling and sealing the pulp chamber and the prepared cavity with the resorptive defect in the apical portion (Figure 1E). Intra-treatment periapical radiograph confirmed the successful pulpotomy and proper filling/sealing of the defect (Figure 1F). Subsequently, the surgical flap was carefully repositioned and sutured.
During the two-week post-treatment period, the attached gingiva remained normal (Figure 1G). Clinical examination revealed normal periodontal probing depths, indicating attachment gain (Figure 1H). Over a 1-year recall, the patient remained asymptomatic with a functional tooth, reporting no discoloration or discomfort. The radiographic assessment demonstrated arrested resorption and a healthy periapical area (Figure 1I). This case showcases the effectiveness of the chosen intervention in managing the complex ICRR lesion while preserving function, esthetics, and patient well-being.
Discussion
ICRR is a distinct and frequently perplexing clinical condition encountered within the realm of endodontics. Its inconspicuous advancement and the capacity for substantial tooth structure damage necessitate meticulous evaluation and the choice between nonsurgical or surgical interventions [8, 20]. This case report showcases the effective surgical management of a class 3 ICRR in a 32-year-old female patient, employing a conservative approach that incorporates an ultraconservative pulpotomy technique utilizing CEM cement.
In this particular case, the application of a modified pulpotomy technique using CEM cement was proved to be the right decision. The choice for surgical intervention was justified by the extensive nature of the class 3 ICRR lesion, which had already affected the coronal dentin and extended toward the mid-root region. The objective was not only to arrest the resorptive process but also to restore the tooth both functionally and esthetically. The surgical procedure provided direct access to the affected tissues, including the dental pulp, enabling the meticulous removal of inflamed tissues within the crown. However, complete removal in the apical portion of the ICRR lesion was not achievable. Importantly, this modified pulpotomy was carried out without the necessity for traditional access cavity preparation, and the remaining portion of the resorptive lesion did not compromise the successful treatment outcomes, aligning with previous findings [10, 15]. This approach is noteworthy as it minimizes the removal of tooth structure, thereby enhancing the likelihood of long-term survival for such a tooth.
Contrary to the conventional approach involving the use of a chemical cauterizing agent, trichloracetic acid, along with curettage and restoration [8], the selection of CEM cement as the pulp-protecting and reparative endodontic biomaterial presents distinct advantages i.e. dentinogenesis [22]. Its inherent biocompatibility ensures minimal irritation to surrounding tissues, creating a conducive environment for optimal healing [23]. Moreover, CEM cement exhibits excellent sealing capabilities, efficiently filling the resorptive defect—an essential factor in preventing reinfection and halting further resorption. Additionally, CEM cement has demonstrated potential in promoting tissue regeneration, thereby enhancing the likelihood of favorable long-term outcomes [17, 24].
There are successful cases of the treatment of these cases have been reported in the literature, which the entire canal space was filled with CEM cement [10, 11]. However, If the correct case selection is done according to the clinical and radiographic signs, VPT can be performed as a more conservative and affordable/accessible procedure.
Subsequent follow-ups at two weeks and one-year post-treatment demonstrated favorable clinical and radiographic outcomes. The restoration of healthy and normal attached gingiva, coupled with the maintenance of regular periodontal probing depths, indicates stability and improvement in periodontal health in such cases [25]. Importantly, the patient remained asymptomatic throughout the follow-up period, reporting neither tooth discoloration nor discomfort. Radiographically, the resorption process had been arrested, and a healthy periapical region was maintained.
The success of this case highlights the potential of conservative surgical approaches in managing advanced ICRR lesions. While the choice between surgical and nonsurgical interventions depends on the extent and severity of the lesion [21, 25], as well as patient preferences, this case reaffirms the feasibility and efficacy of the surgical route in selected cases.
It is essential to acknowledge that this approach comes with inherent limitations and considerations. The decision for surgical intervention must be made judiciously, taking into account factors such as the extent of resorption, patient compliance, and the availability of suitable biomaterials. Furthermore, conducting long-term follow-up, as recommended for a period of 3 years [26], is crucial to monitor the stability of the treated tooth and verify the absence of recurrence.
This case report highlights the potential of conservative surgical interventions, such as modified pulpotomy with CEM cement, in the management of advanced ICRR cases. It underscores the importance of accurate diagnosis, treatment planning, and patient communication in achieving successful outcomes. Furthermore, it emphasizes the role of biocompatible endodontic materials in promoting healing, arresting resorption, and restoring tooth esthetics and function.
Conclusions
The successful management of ICRR Class 3 through a conservative surgical approach with ultraconservative modified pulpotomy using CEM emphasizes the importance of personalized treatment strategies. The present report underscores the feasibility and efficacy of the surgical route in selected cases; however, it is crucial to exercise careful judgment, e.g. lesion extent, patient compliance and biomaterial suitability. Notably, the remaining resorptive defect may not adversely affect the overall results. The presented case highlighted the significance of biocompatible endodontic materials in the promotion of healing, halt of resorption, and restoration of esthetics and function. Ultimately, it exemplified the potential for favorable outcomes; including periodontal attachment re-establishment and esthetic restoration, through a patient-centered and evidence-based approach to managing complex ICRR cases.
Acknowledgments
We extend our gratitude to the patient who participated in this case study.
Conflict of interest
None.
Funding support
No funding was received for this study.
Authors' contributions
Saeed Asgary: Contributed to the conception, design, and interpretation of data, drafted, and critically revised the manuscript. Leila Roghanizadeh: Contributed to drafting and critically revising the manuscript. The authors have given their final approval and agreed to be accountable for all aspects of the work.
Informed consent
Written informed consent was obtained from the patient.
References
- 1.Abbott PV, Lin S. Tooth resorption-Part 2: A Clinical Classification. Dent Traumatol. 2022;38(4):267–85. doi: 10.1111/edt.12762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Madani Z, Moudi E, Bijani A, Mahmoudi E. Diagnostic Accuracy of Cone-Beam Computed Tomography and Periapical Radiography in Internal Root Resorption. Iran Endod J. 2016;11(1):51–6. doi: 10.7508/iej.2016.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Safi Y, Ghaedsharaf S, Aziz A, Hosseinpour S, Mortazavi H. Effect of Field Of View on Detection of External Root Resorption in Cone-Beam Computed Tomography. Iran Endod J. 2017;12(2):179–84. doi: 10.22037/iej.2017.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohammadi Z, Z CC, Shalavi S, Giardino L, Palazzi F, Asgary S. Management of Root Resorption Using Chemical Agents: A Review. Iran Endod J. 2016;11(1):1–7. doi: 10.7508/iej.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Asgary S, Dianat O. Invasive Cervical Root Resorption: A Comprehensive Review on Pathogenesis, Diagnosis, and Treatment. Iran Endod J. 2024;19(1):2–12. doi: 10.22037/iej.v19i1.44246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eftekhar L, Ashraf H, Jabbari S. Management of Invasive Cervical Root Resorption in a Mandibular Canine Using Biodentine as a Restorative Material: A Case Report. Iran Endod J. 2017;12(3):386–9. doi: 10.22037/iej.v12i3.16668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel S, Mavridou AM, Lambrechts P, Saberi N. External Cervical Resorption-Part 1: Histopathology, Distribution And Presentation. Int Endod J. 2018;51(11):1205–23. doi: 10.1111/iej.12942. [DOI] [PubMed] [Google Scholar]
- 8.Heithersay GS. Invasive Cervical Resorption. Endodontic Topics. 2004;7(1):73–92. [Google Scholar]
- 9.Bachesk AB, Queiroz AF, Bin LR, Bachesk AB, Pavan AJ. Clinical Approach to External Cervical Resorption in the Anterior Teeth: A Case Report Study. Iran Endod J. 2021;16(2):118–22. doi: 10.22037/iej.v16i2.32373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asgary S, Nosrat A. Conservative Management of Class 4 Invasive Cervical Root Resorption Using Calcium-enriched Mixture Cement. J Endod. 2016;42(8):1291–4. doi: 10.1016/j.joen.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Esnaashari E, Pezeshkfar A, Fazlyab M. Nonsurgical Management of an Extensive Perforative Internal Root Resorption with Calcium-Enriched Mixture Cement. Iran Endod J. 2015;10(1):75–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Kheirieh S, Fazlyab M, Torabzadeh H, Eghbal MJ. Extraoral Retrograde Root Canal Filling of an Orthodontic-induced External Root Resorption Using CEM Cement. Iran Endod J. 2014;9(2):149–52. [PMC free article] [PubMed] [Google Scholar]
- 13.Asgary S, Fazlyab M. Surgical Treatment of an Immature Short-Rooted Traumatized Incisor with an Extensive Apical Lesion using CEM Cement. Iran Endod J. 2015;10(2):148–51. [PMC free article] [PubMed] [Google Scholar]
- 14.Asgary S, Kemal Çalışkan M. Vital Pulp Therapy of a Mature Molar with Concurrent Hyperplastic Pulpitis, Internal Root Resorption and Periradicular Periodontitis: A Case Report. Iran Endod J. 2015;10(4):284–6. doi: 10.7508/iej.2015.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asgary S, Nourzadeh M, Verma P, Hicks ML, Nosrat A. Vital Pulp Therapy as a Conservative Approach for Management of Invasive Cervical Root Resorption: A Case Series. J Endod. 2019;45(9):1161–7. doi: 10.1016/j.joen.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 16.Asgary S. Management of Pink Spot due to Class IV Invasive Cervical Root Resorption using Vital Pulp Therapy: A Case Report. Iran Endod J. 2023;18(2):110–2. doi: 10.22037/iej.v18i2.41772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Utneja S, Nawal RR, Talwar S, Verma M. Current Perspectives of Bio-Ceramic Technology in Endodontics: Calcium Enriched Mixture Cement-Reviewof Its Composition, Properties and Applications. Restor Dent Endod. 2015;40(1):1–13. doi: 10.5395/rde.2015.40.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Asgary S, Alim Marvasti L, Kolahdouzan A. Indications and Case Series of Intentional Replantation of Teeth. Iran Endod J. 2014;9(1):71–8. [PMC free article] [PubMed] [Google Scholar]
- 19.Sabbagh S, Sarraf Shirazi A, Torabzadeh H. Double Antibiotic Paste for Management of External Inflammatory Root Resorption. Iran Endod J. 2018;13(4):569–72. doi: 10.22037/iej.v13i4.22893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bardini G, Orrù C, Ideo F, Nagendrababu V, Dummer P, Cotti E. Clinical Management of External Cervical Resorption: A Systematic Review. Aust Endod J. 2023;49(3):769–87. doi: 10.1111/aej.12794. [DOI] [PubMed] [Google Scholar]
- 21.Asgary S. Surgical Management of Large-Perforated Class 4 Invasive Cervical Root Resorption: A Case Report. J Dent Sci. 2023;18(1):484–5. doi: 10.1016/j.jds.2022.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Asgary S. Micro-computed Tomography Assessment of Full Pulpotomy in a Mature Molar after Five Years: A Case Report. Iran Endod J. 2022;17(4):223–4. doi: 10.22037/iej.v17i4.39717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Naghavi N, Ghoddusi J, Sadeghnia HR, Asadpour E, Asgary S. Genotoxicity and Cytotoxicity of Mineral Trioxide Aggregate and Calcium Enriched Mixture Cements on L929 Mouse Fibroblast Cells. Dent Mater J. 2014;33(1):64–9. doi: 10.4012/dmj.2013-123. [DOI] [PubMed] [Google Scholar]
- 24.Talebzadeh B. Simplified Orthograde Apical Plug and Intra-Orifice Barriers for Resolving a Complex Endodontic Challenge: A Case Report. Iran Endod J. 2023;18(4):271–3. doi: 10.22037/iej.v18i4.43108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Asgary S, Fazlyab M. Surgical Repair of Invasive Cervical Root Resorption with Calcium-Enriched Mixture Cement: A Case Report. Gen Dent. 2015;63(1):37–40. [PubMed] [Google Scholar]
- 26.Heithersay GS. Treatment of Invasive Cervical Resorption: an Analysis of Results using Topical Application of Trichloracetic Acid, Curettage, and Restoration. Quintessence Int. 1999;30(2):96–110. [PubMed] [Google Scholar]