Abstract
Objectives
To assess the association of Long COVID with housing insecurity in the United States.
Methods
To compare the prevalence of 3 binary indicators of housing insecurity between people with Long COVID (symptoms >3 months) and COVID-19 survivors who did not report long-term symptoms, we used survey-weighted regression models on 206,969 responses from the Household Pulse Survey, a representative cross-sectional survey of US households collected September 2022–April 2023. Among people with Long COVID, we additionally assessed whether functional impairment, current COVID-19 related symptoms, and symptom impact on day-to-day life were associated with a higher prevalence of housing insecurity.
Results
During the study period, 56,353 respondents with prior COVID-19 experienced symptoms lasting 3 months or longer (27%), representing an estimated 28 million US adults. After adjusting for demographic factors, people with Long COVID were 1.5–2 times as likely to experience significant difficulty with household expenses (Prevalence ratio [PR] 1.48, 95% CI 1.42–1.55), be behind on housing payments (PR 1.48, 95% CI 1.36–1.60), and face likely eviction or foreclosure (PR 1.86, 95% CI 1.58–2.18). The risk of housing insecurity was highest among low-income adults with Long COVID. Among people with Long COVID, functional limitation and current symptoms which impact day-to-day life were associated with higher prevalence of housing insecurity.
Conclusions
Compared with COVID-19 survivors who do not experience long-term symptoms, people with Long COVID are more likely to report indicators of housing insecurity, particularly those of lower socio-economic status, and those with functional limitations or long-term COVID-19 related symptoms impacting day-to-day life. Policies are needed to support people living with chronic illnesses following SARS-CoV-2 infection.
Keywords: Housing, Housing insecurity, Long COVID, Post-acute COVID-19 syndrome, COVID-19
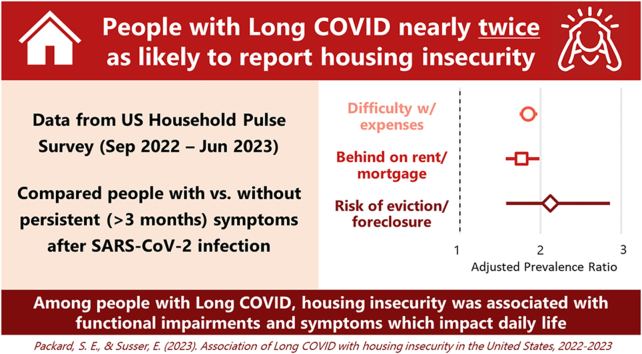
Graphical abstract
Highlights
-
•
Compared to survivors of COVID-19 without long-term symptoms, people with Long COVID are nearly twice as likely to report housing insecurity.
-
•
The highest prevalence of housing insecurity indicators was estimated among people of low socio-economic status who report Long COVID.
-
•
Among people with Long COVID, housing insecurity was more likely among those with functional limitations and symptoms which impact daily life.
-
•
Despite reduced incidence of COVID-19, people with chronic illness following infection feel sustained socio-economic impacts of the pandemic.
1. Introduction
Our lives are anchored around the places we call home. Maintaining a safe, secure place of residence is among the foremost concerns for every person and family, intimately linked to nearly every aspect of our lives and well-being. At the population level, the determinants and consequences of access to housing are likewise fundamental to public health (Gonzalez & Fullilove, 2020; Shaw, 2004). Not only do chronic health problems and disability adversely impact access to adequate and stable housing, but unstable housing is empirically related to subsequent physical and mental health outcomes (Cusack et al., 2021; Elder & King, 2019; Kang, 2022; Rao et al., 2023).
Unfortunately, many people in the United States face the very real threat of housing insecurity. The homeless population in the United States is over a half a million people and growing, and prior to the COVID-19 pandemic more than 2 million households were being threatened with evictions in formal court filings each year, with evictions carried out on 6–7% of renting households (Gromis et al., 2022; National Alliance to End Homelessness, 2023). Early in the pandemic, housing insecurity was recognized as a significant public health issue under threat of exacerbation by economic stresses experienced in 2020. As a result, policies were enacted at multiple levels of government, including a federal eviction moratorium issued by the Centers for Disease Control and Prevention, as US households struggled with the direct and indirect impacts of COVID-19 (Benfer et al., 2021; Raajkumar, 2022).
The end of the federal eviction moratorium in August 2021 coincided with an increasing awareness that a significant proportion of those who survive SARS-CoV-2 infection go on to develop long-term sequelae, indicating a potential public health crisis affecting millions (Phillips & Williams, 2021). Long COVID, also known as Post-Acute Sequelae of COVID-19 and Post-COVID Conditions, is an umbrella term for a range of etiologies and illness experiences resulting from or triggered by COVID-19 infection, presenting with heterogeneous severity, duration, and symptomatology across multiple organ systems (Castanares-Zapatero et al., 2022; Davis, McCorkell, Vogel, & Topol, 2023; Michelen et al., 2021). Many people who develop Long COVID will experience profound livelihood changes due to the onset of significant physical or cognitive impairments, which have been linked to a number of adverse social and economic outcomes including social exclusion and reduced employment (Nittas et al., 2022). To date, however, no studies have assessed the degree to which people living with Long COVID face increased risk of housing insecurity.
Data from the Household Pulse Survey (HPS), a nationally representative survey of US households produced by the Census Bureau to monitor the social and economic impact of the COVID-19 pandemic (US Census Bureau, 2022c), have been used by researchers to describe the inter-relationship of housing insecurity with financial hardship, disability, and health status during various stages of the pandemic (Bushman & Mehdipanah, 2022; Friedman, 2023; Kim, 2021). In mid-2022, the survey added new questions about long term symptoms following acute COVID-19, making it the first source of nationally representative surveillance data on Long COVID in the United States (Levine, 2022; US Census Bureau, 2022b).
The present study uses these data to assess the association of Long COVID with housing insecurity among US adults with a history of COVID-19. Specifically, we hypothesized that compared to people who had COVID-19 but did not report long-term symptoms, those who report symptoms lasting longer than 3 months that they did not have prior to their infection (henceforth Long COVID) would be more likely to report indicators of housing insecurity including significant difficulty with routine household expenses, being behind on rent or mortgage payments, and perceived likelihood of eviction or foreclosure. Additionally, we hypothesized that among people with Long COVID, measures of functional impairment, current symptoms, and impact of symptoms on day-to-day life would be associated with increased prevalence of each indicator of housing insecurity.
2. Materials and methods
2.1. Study population
Respondents to the Household Pulse Survey were recruited from a stratified sample of domiciles in the US Census Bureau's Master Address File, with one adult from each household being invited by phone or email to complete a 20-min online questionnaire (US Census Bureau, 2022a). We accessed Public Use Files from Phases 3.6–3.8 and utilized data from weeks 49–56, representing 8 waves of data collected over 7 months from September 14, 2022–April 10, 2023 (US Census Bureau, 2023). We excluded survey responses without a confirmed history of COVID-19 infection (positive test result or diagnosis from healthcare provider), with onset of COVID-19 in the four weeks prior to taking the survey, and responses missing data on variables used to define the exposures and outcomes (Long COVID and housing insecurity, respectively).
2.2. Measures
2.2.1. Housing tenure and indicators of housing insecurity
Using data available from the HPS, we defined housing tenure as either owning a home or renting. A minimal proportion (<2%) of respondents were non-homeowners who reported occupying their home without making payments; these were respondents of predominantly low socio-economic status and were collapsed into the “renting” category for this analysis. We operationalized three binary indicators of housing insecurity as outcome variables in this study. Significant difficulty with household expenses was defined as responding “Very difficult” to the question “In the last 7 days, how difficult has it been for your household to pay for usual household expenses, including but not limited to food, rent or mortgage, car payments, medical expenses, student loans, and so on?” Being behind on rent or mortgage payments was defined as responding “No” to the questions “Is the household currently caught up on [rent or mortgage] payments?” Those who endorsed being behind on housing payments were additionally asked “How likely is it that your household will have to leave this home or apartment within the next two months because of [eviction or foreclosure]?” and perceived likelihood of eviction or foreclosure was defined as responding “Somewhat likely” or “Very likely” to this question. Respondents who owned their home free and clear or occupying their home without being obligated for rent were classified as being neither behind on payments nor at risk of eviction/foreclosure. Skip logic patterns for questions pertaining to housing insecurity are shown in Fig. S1.
2.2.2. Long COVID status, current symptoms, and measures of functional impairment
Those who reported ever testing positive or being told by a healthcare provider that they had COVID-19 were asked follow-up questions about long-term symptoms. We defined Long COVID as responding affirmatively to the question “Did you have any symptoms lasting 3 months or longer that you did not have prior to having coronavirus or COVID-19? Long term symptoms may include tiredness or fatigue, difficulty thinking, concentrating, forgetfulness, or memory problems (sometimes referred to as “brain fog”), difficulty breathing or shortness of breath, joint or muscle pain, fast-beating or pounding heart (also known as heart palpitations), chest pain, dizziness on standing, menstrual changes, changes to taste/smell, or inability to exercise.” We defined current symptoms as responding affirmatively to “Are you currently experiencing symptoms?“. Those who reported current symptoms were additionally asked “Do these long-term symptoms reduce your ability to carry out day-to-day activities compared with the time before you had COVID-19?” which we used to define symptom impact as “Not at all,” “A little,” or “A lot”. Skip logic patterns for questions pertaining to Long COVID are shown in Fig. S2.
Measures of functional impairment were collected on all survey respondents, unrelated to questions about COVID-19. Adapted from the Washington Group Short Set on Functioning (Weeks, Dahlhamer, Madans, & Maitland, 2021), these questions asked about difficulty with seeing, hearing, cognition, mobility, self-care, and communication. Within each domain, No Limitation was defined as responding “None at all”, Moderate Limitation was defined as responding “Some difficulty”, and Severe Limitation was defined as responding “A lot of difficulty” or “Cannot do at all”.
2.2.3. Socio-demographic covariates
Demographic information was collected on the survey, including age, gender, educational attainment, and prior year household income. In this study, age and gender were a priori treated as confounders as they have been consistently associated with both the exposure and the outcome in previous studies (Davis et al., 2023; Michelen et al., 2021). While socio-economic status (SES) likely plays a role in the hypothesized association, it is not known the degree to which measures of SES such as education and income act as confounders, effect modifiers, or mediators due to less consistent evidence in the literature on Long COVID and economic well-being. Statistical adjustment for confounders can reduce bias of effect estimates, but unnecessary adjustment for effect modifiers, colliders, and mediators can have the opposite impact of increasing bias (Wysocki, Lawson, & Rhemtulla, 2022). To examine SES as both a potential confounder and effect modifier, we first assessed whether adjustment by education and income impacted the strength of association between Long COVID and housing insecurity, and subsequently assessed interaction on both the additive and multiplicative scale, as described below.
To account for missing covariate data, multiple imputation of covariates (age, gender, education, and income) was performed via multiple imputation with chained equations (MICE) using classification and regression trees. The results of statistical models are provided as the pooled results of 10 imputed datasets (Buuren & Groothuis-Oudshoorn, 2011; Doove, van Buuren, & Dusseldorp, 2012). Imputed data were not used for descriptive statistics.
2.3. Statistical analysis
2.3.1. Descriptive analysis
We used person-level survey weights provided by the HPS to estimate counts and proportions of study variables for the target population of US adults with a history of COVID-19. For bivariate descriptive analyses, we estimated the unadjusted survey-weighted proportions of housing insecurity indicators, socio-demographic covariates, functional limitations, and symptoms by Long COVID status.
2.3.2. Statistical models
To assess the association of housing insecurity and Long COVID, we used survey-weighted generalized linear models with a quasi-Poisson distribution, logarithmic link function, and robust standard errors to estimate adjusted prevalence ratios (Zou, 2004). Separate models were fitted for each indicator of housing insecurity in three sets of models as described below.
In the first set of models, we regressed housing insecurity indicators on Long COVID. We specified unadjusted models, models adjusted for age, gender, and survey week, and models additionally adjusted for prior-year income and education level. To further understand potential effect modification by socio-economic status, we specified models with interaction terms between Long COVID and income and models with interaction terms between Long COVID and education, adjusted for age, gender, and survey week. To assess interaction on the additive scale, we used the “ggeffect” function from the “ggeffects” package for R to estimate from these models the marginal mean risk and risk difference of each binary indicator of housing insecurity for the Long COVID and No Long COVID groups at each level of the potential modifiers (Bieler, Brown, Williams, & Brogan, 2010; Lüdecke, 2018). In a second set of models, we regressed indicators of housing insecurity on measures of functional limitation among people with Long COVID, adjusted for age, gender, education, income, and survey week. In the third set of models, we regressed housing insecurity indicators on the presence or absence of current Long COVID symptoms and impact of these symptoms on day-to-day life among people with Long COVID, adjusted for age, gender, education, income, and survey week.
All analyses were performed in R version 4.2.2 using the survey package (Lumley, 2020; R Core Team, 2021). Conforming to Columbia University Institutional Review Boards policy on Use of Publicly Available Datasets for Research, formal ethics review was not required.
3. Results
3.1. Descriptive analysis
A total of 206,969 survey respondents met inclusion criteria across the 8 waves of HPS data, representing an estimated 96,545,653 US adults with a history of confirmed SARS-CoV-2 infection, of whom an estimated 27,824,777 (28.8%) experienced new symptoms lasting 3 months or longer, meeting the study definition of Long COVID. As shown in Table 1, one in five US adults with a history of COVID-19 (20.2%) experienced at least one measure of housing insecurity during the study period, including significant difficulty with household expenses (16.2%), being behind on rent or mortgage payments (7.8%), or being at risk of eviction or foreclosure (2.5%). Inclusion in the study overall and for each sub-analysis is illustrated in Fig. 1. A comparison of included and excluded participants is provided in Table S1.
Table 1.
Selected demographic characteristics, indicators of housing insecurity, functional limitations, and COVID-19 symptoms by illness status among US adults with a history of COVID-19, September 2022–April 2023.
| Characteristic | Long COVID | No Long COVID | Overall |
|---|---|---|---|
| Unweighted n | 56,353 | 150,616 | 206,969 |
| Weighted n | 27,824,777 | 68,720,876 | 96,545,653 |
| Age | 45.7 (15.4) | 46.2 (16.3) | 46.0 (16.1) |
| Race/Ethnicity | |||
| White non-Hispanic | 42,499 (63.7%) | 118,024 (66.5%) | 160,523 (65.7%) |
| White Hispanic | 4,699 (15.8%) | 10,021 (13.1%) | 14,720 (13.9%) |
| Black | 3,727 (9.2%) | 8,412 (8.8%) | 12,139 (8.9%) |
| Asian | 1,673 (3.8%) | 7,340 (5.9%) | 9,013 (5.3%) |
| Other |
3,755 (7.5%) |
6,819 (5.6%) |
10,574 (6.2%) |
| Gender | |||
| Male | 17,496 (36.2%) | 68,475 (50.2%) | 85,971 (46.2%) |
| Female | 37,452 (60.8%) | 79,782 (48.4%) | 117,234 (52.0%) |
| Transgender | 382 (1.2%) | 497 (0.5%) | 879 (0.7%) |
| None of the above |
770 (1.9%) |
1,150 (0.9%) |
1,920 (1.2%) |
| Education | |||
| Less than high school | 1,130 (6.6%) | 1,802 (4.6%) | 2,932 (5.2%) |
| High school graduate | 6,705 (28.0%) | 13,701 (25.7%) | 20,406 (26.3%) |
| Some college or associates | 21,497 (35.7%) | 40,708 (28.6%) | 62,205 (30.6%) |
| Bachelor's degree | 15,199 (17.4%) | 48,704 (22.3%) | 63,903 (20.9%) |
| Graduate degree |
11,822 (12.2%) |
45,701 (18.9%) |
57,523 (17.0%) |
| Income (2021) | |||
| Less than $25,000 | 6,453 (14.3%) | 8,614 (8.5%) | 15,067 (10.2%) |
| $25,000 - $34,999 | 5,269 (12.1%) | 8,794 (8.5%) | 14,063 (9.5%) |
| $35,000 - $49,999 | 6,565 (13.4%) | 12,553 (11.0%) | 19,118 (11.7%) |
| $50,000 - $74,999 | 9,902 (18.4%) | 22,153 (16.8%) | 32,055 (17.2%) |
| $75,000 - $99,999 | 7,924 (13.5%) | 21,075 (14.3%) | 28,999 (14.1%) |
| $100,000 - $149,999 | 9,551 (15.4%) | 30,471 (18.4%) | 40,022 (17.5%) |
| $150,000 and above |
8,927 (13.0%) |
41,993 (22.6%) |
50,920 (19.8%) |
| Marital Status | |||
| Married | 30,864 (54.8%) | 95,387 (61.3%) | 126,251 (59.4%) |
| Widowed/Divorced/Separated | 13,331 (19.2%) | 25,282 (14.1%) | 38,613 (15.6%) |
| Never Married |
12,001 (26.0%) |
29,613 (24.6%) |
41,614 (25.0%) |
| Housing Tenure | |||
| Owned with Mortgage/Loan | 27,885 (46.8%) | 79,430 (49.6%) | 107,315 (48.8%) |
| Owned, No Mortgage | 11,499 (19.5%) | 35,965 (22.6%) | 47,464 (21.7%) |
| Rented | 16,077 (32.0%) | 33,715 (26.6%) | 49,792 (28.1%) |
| Occupied Without Rent Payments |
892 (1.7%) |
1,506 (1.2%) |
2,398 (1.4%) |
| Difficulty Making Living Expenses | |||
| Not at all difficult | 14,664 (19.9%) | 69,795 (36.5%) | 84,459 (31.7%) |
| A little difficult | 17,292 (29.9%) | 42,935 (30.6%) | 60,227 (30.4%) |
| Somewhat difficult | 13,177 (26.1%) | 24,224 (19.9%) | 37,401 (21.7%) |
| Very difficult |
11,220 (24.2%) |
13,662 (13.0%) |
24,882 (16.2%) |
| Current on Rent/Mortgage Payments | |||
| Current | 40,103 (88.7%) | 108,427 (93.7%) | 148,530 (92.2%) |
| Not current |
3,859 (11.3%) |
4,718 (6.3%) |
8,577 (7.8%) |
| Months Behind on Rent/Mortgage Payments | |||
| Current | 40,103 (88.7%) | 108,427 (93.7%) | 148,530 (92.2%) |
| 0-1 | 1,841 (5.2%) | 2,498 (3.0%) | 4,339 (3.7%) |
| 2-3 | 1,210 (3.7%) | 1,225 (1.7%) | 2,435 (2.3%) |
| 4+ | 716 (2.0%) | 729 (1.0%) | 1,445 (1.3%) |
| No response |
92 (0.3%) |
266 (0.5%) |
358 (0.4%) |
| Eviction/Foreclosure in Next 2 Months | |||
| Very likely | 426 (1.4%) | 363 (0.5%) | 789 (0.8%) |
| Somewhat likely | 956 (2.8%) | 841 (1.2%) | 1,797 (1.7%) |
| Not very likely | 1,377 (3.9%) | 1,519 (2.2%) | 2,896 (2.7%) |
| Not likely at all | 1,100 (3.1%) | 1,995 (2.4%) | 3,095 (2.6%) |
| Current on rent/mortgage |
40,103 (88.7%) |
108,427 (93.7%) |
148,530 (92.2%) |
| Housing Insecurity | |||
| No | 42,867 (70.9%) | 133,147 (83.5%) | 176,014 (79.8%) |
| Yes |
13,343 (29.1%) |
17,210 (16.5%) |
30,553 (20.2%) |
| Difficulty seeing | |||
| No difficulty | 30,379 (52.6%) | 107,727 (69.7%) | 138,106 (64.8%) |
| Moderate difficulty | 22,742 (41.0%) | 39,069 (27.1%) | 61,811 (31.1%) |
| Severe difficulty | 3,157 (6.2%) | 3,618 (3.0%) | 6,775 (3.9%) |
| Did not report |
75 (0.2%) |
202 (0.2%) |
277 (0.2%) |
| Difficulty hearing | |||
| No difficulty | 42,156 (75.5%) | 124,202 (83.2%) | 166,358 (80.9%) |
| Moderate difficulty | 11,893 (20.1%) | 22,890 (14.2%) | 34,783 (15.9%) |
| Severe difficulty | 2,091 (4.0%) | 3,059 (2.3%) | 5,150 (2.8%) |
| Did not report |
213 (0.4%) |
465 (0.4%) |
678 (0.4%) |
| Difficulty cognitive | |||
| No difficulty | 19,552 (34.1%) | 95,451 (61.4%) | 115,003 (53.6%) |
| Moderate difficulty | 29,248 (51.1%) | 48,971 (33.3%) | 78,219 (38.4%) |
| Severe difficulty | 7,447 (14.5%) | 5,913 (5.1%) | 13,360 (7.8%) |
| Did not report |
106 (0.2%) |
281 (0.2%) |
387 (0.2%) |
| Difficulty with mobility | |||
| No difficulty | 36,519 (63.8%) | 125,226 (81.5%) | 161,745 (76.4%) |
| Moderate difficulty | 15,288 (27.3%) | 20,993 (14.8%) | 36,281 (18.4%) |
| Severe difficulty | 4,454 (8.7%) | 4,139 (3.5%) | 8,593 (5.0%) |
| Did not report |
92 (0.2%) |
258 (0.2%) |
350 (0.2%) |
| Difficulty with self-care | |||
| No difficulty | 49,808 (86.2%) | 143,931 (94.2%) | 193,739 (91.9%) |
| Moderate difficulty | 5,530 (11.3%) | 5,676 (4.8%) | 11,206 (6.7%) |
| Severe difficulty | 930 (2.3%) | 737 (0.7%) | 1,667 (1.2%) |
| Did not report |
85 (0.2%) |
272 (0.2%) |
357 (0.2%) |
| Difficulty communicating | |||
| No difficulty | 50,052 (86.9%) | 143,989 (94.1%) | 194,041 (92.0%) |
| Moderate difficulty | 5,630 (11.4%) | 5,856 (5.1%) | 11,486 (6.9%) |
| Severe difficulty | 603 (1.5%) | 565 (0.7%) | 1,168 (0.9%) |
| Did not report |
68 (0.2%) |
206 (0.2%) |
274 (0.2%) |
| Current symptoms | |||
| No | 30,452 (55.7%) | 143,180 (99.2%) | 173,632 (86.2%) |
| Yes |
25,901 (44.3%) |
1,164 (0.8%) |
27,065 (13.8%) |
| Symptom impact on day-to-day activities | |||
| Not at all | 5,500 (20.2%) | 5,500 (20.2%) | |
| A little | 14,805 (55.5%) | 14,805 (55.5%) | |
| A lot | 5,588 (24.3%) | 5,588 (24.3%) | |
Fig. 1.
Inclusion of respondents in the study sample for each analysis.
Demographic characteristics, housing data, and health measures are summarized by Long COVID status in Table 1. People with Long COVID were more likely than those without Long COVID to rent rather than own their home and more likely to report all three indicators of housing insecurity. People with Long COVID were also more likely to report moderate or severe functional limitation across each of the five domains assessed. For example, roughly two-thirds of people with Long COVID experienced cognitive limitations, nearly twice the prevalence of those without. Just under half of those with Long COVID were currently experiencing Long COVID symptoms at the time of the survey (44.3%), and around 8 in 10 of these people reported that their symptoms reduced their ability to carry out day-to-day activities compared with the time preceding their active infection (79.8%). People with Long COVID were additionally more likely to report female, transgender, or “none of the above” as their gender, more likely to be widowed, divorced, or separated, less likely to have a college degree, and more likely to report a 2021 household income of $50,000 or less.
3.2. Long COVID and housing insecurity
3.2.1. Long COVID status and housing insecurity
Models of the overall association of Long COVID with housing insecurity are summarized in Table 2. The unadjusted prevalence of housing insecurity among people with Long COVID was roughly twice as high as those without Long COVID, measured as difficulty with household expenses (Prevalence ratio [PR] 1.86, CI 1.78–1.94; P < .001), being behind on rent or mortgage (PR 1.84, CI 1.70–2.00; P < .001), or facing likely eviction or foreclosure (PR 2.51, CI 2.15–2.93; P < .001). These effect estimates were attenuated by roughly 5% in models adjusted for age and gender, and further attenuated by 20–30% in models additionally adjusted for education and prior-year income.
Table 2.
Association between Long COVID, Housing Tenure, and Housing Insecurity among adults with history of confirmed COVID-19 in the United States, September 2022–April 2023.
| Difficulty With Expenses |
Behind on Housing Payments |
Likely Eviction or Foreclosure |
||
|---|---|---|---|---|
| PR (95% CI) | PR (95% CI) | PR (95% CI) | ||
| Unadjusted | No Long COVID | ref | ||
| Long COVID | 1.86 (1.78 – 1.94) | 1.84 (1.70 – 2.00) | 2.51 (2.15 – 2.93) | |
| Partially Adjusted | No Long COVID | ref | ||
| Long COVID | 1.79 (1.71 – 1.87) | 1.77 (1.63 – 1.91) | 2.37 (2.03 – 2.78) | |
| Fully Adjusted | No Long COVID | ref | ||
| Long COVID | 1.48 (1.42 – 1.55) | 1.48 (1.36 – 1.60) | 1.86 (1.58 – 2.18) | |
PR = Adjusted Prevalence Ratio; CI = Confidence Interval.
Models included all respondents who met inclusion criteria for the study (n = 206,969).
Partially Adjusted: Adjusted for age, gender, and survey week.
Fully Adjusted: Adjusted for age, gender, survey week, income, and education.
The role of education and income in the observed association is further explored in Table 3 and Fig. 2. The mean marginal risk of each measure of housing insecurity at 3 levels each of income and education are shown based on interaction models adjusted for age, gender, and survey week. The absolute risk differences in housing insecurity between people with and without Long COVID were higher for low income (3–12%) compared to high income adults (1–4%), but less consistent evidence was provided for interaction on the multiplicative scale, given overlapping confidence intervals between stratum - specific prevalence ratios. Conversely, risk differences were similar across strata of education, but prevalence ratios were higher among adults of higher educational attainment. Notably, the highest predicted risk for housing insecurity was consistently among adults with Long COVID and low income or educational attainment.
Table 3.
Housing insecurity and Long COVID by prior-year income and education level among adults with history of confirmed COVID-19 in the United States, September 2022–April 2023.
| Prior-Year Income (USD) |
Education Level |
|||||
|---|---|---|---|---|---|---|
| $0k – $50k | $50k – $100k | $100k+ | High School or Less | Some College | College Graduate | |
| Difficulty with Household Expenses | ||||||
| No Long COVIDa | 0.26 (0.25, 0.27) | 0.13 (0.12, 0.13) | 0.05 (0.04, 0.05) | 0.21 (0.20, 0.22) | 0.16 (0.15, 0.16) | 0.06 (0.05, 0.06) |
| Long COVIDa | 0.38 (0.36, 0.39) | 0.21 (0.19, 0.22) | 0.08 (0.07, 0.09) | 0.31 (0.29, 0.32) | 0.25 (0.24, 0.26) | 0.13 (0.12, 0.14) |
| Risk Difference | 0.12 (0.10, 0.14) | 0.08 (0.06, 0.09) | 0.04 (0.03, 0.05) | 0.09 (0.07, 0.11) | 0.08 (0.07, 0.10) | 0.06 (0.06, 0.07) |
| Prevalence Ratio |
1.45 (1.37, 1.53) |
1.62 (1.50, 1.75) |
1.90 (1.66, 2.16) |
1.47 (1.35 1.59) |
1.60 (1.51 1.69) |
2.24 (2.09 2.41) |
| Behind on Housing Payments | ||||||
| No Long COVIDa | 0.09 (0.08, 0.10) | 0.05 (0.04, 0.05) | 0.02 (0.01, 0.02) | 0.08 (0.07, 0.08) | 0.05 (0.05, 0.06) | 0.02 (0.02, 0.02) |
| Long COVIDa | 0.14 (0.13, 0.15) | 0.07 (0.06, 0.08) | 0.03 (0.02, 0.03) | 0.11 (0.10, 0.12) | 0.09 (0.09, 0.10) | 0.04 (0.04, 0.05) |
| Risk Difference | 0.04 (0.03, 0.06) | 0.02 (0.01, 0.03) | 0.01 (0.01, 0.02) | 0.03 (0.01, 0.04) | 0.03 (0.02, 0.04) | 0.02 (0.01, 0.02) |
| Prevalence Ratio |
1.51 (1.36, 1.68) |
1.46 (1.27, 1.69) |
1.79 (1.39, 2.30) |
1.43 (1.24, 1.66) |
1.69 (1.53, 1.88) |
1.98 (1.76, 2.24) |
| Risk of Eviction or Foreclosure | ||||||
| No Long COVIDa | 0.03 (0.03, 0.04) | 0.01 (0.01, 0.01) | 0.00 (0.00, 0.00) | 0.08 (0.07, 0.08) | 0.05 (0.05, 0.06) | 0.02 (0.02, 0.02) |
| Long COVIDa | 0.06 (0.05, 0.07) | 0.02 (0.02, 0.02) | 0.01 (0.00, 0.01) | 0.11 (0.10, 0.12) | 0.09 (0.09, 0.10) | 0.04 (0.04, 0.05) |
| Risk Difference | 0.03 (0.02, 0.04) | 0.01 (0.00, 0.01) | 0.01 (0.00, 0.01) | 0.02 (0.01, 0.03) | 0.01 (0.01, 0.02) | 0.00 (0.00, 0.01) |
| Prevalence Ratio | 1.94 (1.62, 2.32) | 1.78 (1.28, 2.47) | 2.74 (1.09, 6.90) | 1.88 (1.45, 2.44) | 2.09 (1.74, 2.51) | 3.57 (2.67, 4.78) |
All estimates and marginal effects adjusted for age, gender, and survey week.
Predicted probability calculated as the estimated marginal mean value of the binary outcome (0–1).
Fig. 2.
Predicted Probabilities of housing insecurity indicators among adults with and without Long COVID by prior year income, calculated as estimated marginal mean values from regression models adjusted for age, gender, and survey week.
3.2.2. Functional impairment among people with long COVID
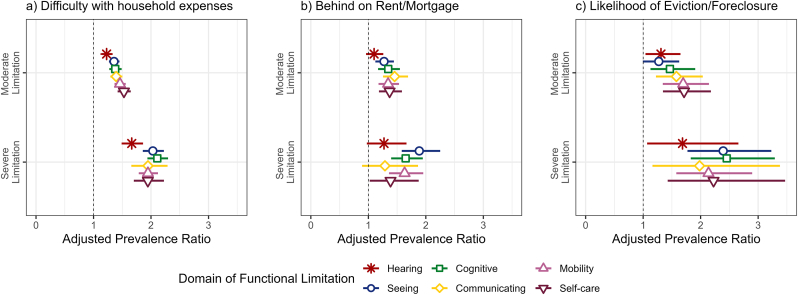
Models of the association between functional impairment and housing insecurity among people with Long COVID and are summarized in Fig. 3 and Table S2. There was a consistent trend of increased housing insecurity among people with Long COVID who reported moderate or severe functional limitation across all domains. Difficulty making household expenses was more strongly associated with severe limitations compared to moderate limitations, but this difference was less apparent for being behind on housing payments or being at risk of eviction or foreclosure.
Fig. 3.
Association of Functional Limitations with Housing Insecurity Among Adults with Long COVID in the United States, September 2022–April 2023. Estimates are displayed as Prevalence Ratios and 95% Confidence Intervals adjusted for age, gender, education, income, and survey week. The reference group for each PR is respondents who reported no functional limitation. Models included all survey respondents with Long COVID (n = 56,353).
3.2.3. Current COVID-related symptoms and symptom impact among people with long COVID
Models estimating the association of housing insecurity with current symptoms and symptom impact on day-to-day life among people with Long COVID are summarized in Table 4a. The adjusted prevalence of housing insecurity was 13–42% higher among people whose symptoms were current compared to those not currently experiencing symptoms. Among those who reported current symptoms, the prevalence of housing insecurity was strongly associated with reported impact of symptoms on day-to-day life compared to the time preceding SARS-CoV-2 infection. Compared to those who reported that their current symptoms did not impact their day-to-day life compared to the time before they had COVID-19, those who reported that their symptoms impacted their life “a lot” were 2–3 times more likely to report difficulty making household expenses (PR 2.75, CI 2.38–3.16) and being behind on rent (PR 2.95, CI 2.24–3.88), and 7 times more likely to be at risk for eviction or foreclosure (PR 7.32, CI 4.38–12.21) (See Table 4b).
Table 4a.
Association between current long COVID symptoms and housing insecurity among adults with long COVID in the United States, September 2022–April 2023.
| Difficulty With Expenses | Behind on Housing Payments | Likely Eviction or Foreclosure | |
|---|---|---|---|
| Symptoms | PR (95% CI) | PR (95% CI) | PR (95% CI) |
| Not Current | ref | ||
| Current | 1.24 (1.17–1.32) | 1.14 (1.01–1.28) | 1.42 (1.14–1.76) |
PR = Adjusted Prevalence Ratio; CI = Confidence Interval. All models adjusted for age, gender, education, income, and survey week.
Models included all respondents with Long COVID (n = 56,353).
Table 4b.
Association Between Impact of Long COVID-related symptoms and Housing Insecurity Among Adults with Long COVID in the United States, September 2022–April 2023.
| Difficulty With Expenses | Behind on Housing Payments | Likely Eviction or Foreclosure | |
|---|---|---|---|
| Symptom Impact | PR (95% CI) | PR (95% CI) | PR (95% CI) |
| None | Ref | ||
| A little | 1.59 (1.38–1.83) | 1.92 (1.45–2.52) | 3.64 (2.13–6.25) |
| A lot | 2.75 (2.38–3.16) | 2.95 (2.24–3.88) | 7.32 (4.38–12.21) |
PR = Adjusted Prevalence Ratio; CI = Confidence Interval. All models adjusted for age, gender, education, income, and survey week. Models of included respondents who reported current symptoms (n = 25,901).
4. Discussion
Based on a large, representative survey of US households during the third year of the COVID-19 pandemic, over 25 million US adults were estimated to have experienced long-term symptoms after infection with SARS-CoV-2. This represents 29% of COVID-19 survivors, which is higher than some conservative estimates of the prevalence of Long COVID but consistent with prior studies in the United States (O'Mahoney et al., 2023; Perlis et al., 2022; Robertson et al., 2023; Spatz et al., 2023). Nearly one third of people with Long COVID were either struggling to make household expenses, behind on housing payments, or facing likely eviction or foreclosure in the near future. These measures of housing insecurity were nearly twice as prevalent among people with Long COVID compared to those who had COVID-19 without long term symptoms. This association was partially attenuated but still strong after adjusting for socio-demographic factors. While Long COVID was associated with housing insecurity at every level of education and income, the highest risk of housing insecurity was found among adults of low SES who also had Long COVID, and it was among low-income adults where Long COVID accounted for the largest absolute difference in risk of housing insecurity. Among people living with Long COVID, the prevalence of housing insecurity was significantly higher among those who reported that these long-term symptoms reduce their ability to carry out day-to-day activities compared to the time prior to their illness, and significantly higher among those who specifically report moderate or severe functional impairments, particularly cognitive, mobility, and self-care limitations.
This research helps illuminate the profound ongoing social and economic consequences of the COVID-19 pandemic. Despite a significant decline in incident COVID-19 cases, hospitalizations, and deaths, the pandemic continues to impact millions of people in the US on a daily basis, particularly those survivors of SARS-CoV-2 infection who go on to experience long-term symptoms. While we are still learning about the underlying causes of Long COVID, it is clear that many survivors of COVID-19 experience lasting health problems, posing a significant population health challenge. Even after the end of the federal Public Health Emergency in the United Statues (Assistant Secretary for Public Affairs, US Department of Health and Human Services, 2023), it is essential that sustained pandemic recovery efforts acknowledge and address the ongoing public health crisis of Long COVID and provide support through continued COVID-19 prevention, disability accommodations at work, supportive housing policies, and renter protections. Just as primary prevention of COVID-19 and supportive policies to prevent homelessness were paramount during earlier pandemic waves, they remain important public health strategies as people continue to experience long-term chronic illness after infection. Integration of policies to address infectious disease, chronic illness, and housing should be considered, as the manifold health and social consequences of housing insecurity and homelessness are well documented and the large and increasing number of people who are already homeless in the United States only adds to their urgency (Gonzalez & Fullilove, 2020).
Our findings are consistent with previous literature that has described how the symptoms and functional limitations experienced by people with Long COVID result in disrupted livelihoods, reduced employment, or increased healthcare spending (Nittas et al., 2022). New onset chronic illness after COVID-19 infection will, for many people, result in challenges to being able to make routine household expenses, including rent or mortgage payments. The results in this study support this by adjusting for potential confounders and demonstrating that among people with Long COVID specifically, the presence and impact of current symptoms was associated with higher prevalence of housing insecurity. However, as this study was not designed to estimate a causal effect, the results are also open to alternate interpretations which will may inform future research. For example, it is also plausible that people with a history of unstable housing due to pre-existing socioeconomic disadvantage, disability, or chronic illness may be more prone to develop sequelae from COVID-19 due to material deprivation, stress, or other factors which could predispose someone to chronic illness triggered by viral infection. While priorities for future research include a better understanding of how the social and structural determinants of health shape the increased risk of socio-economic hardship faced by people with Long COVID, we contend that the added burden of social and economic precarity experienced by people living with Long COVID is a public health concern regardless of the direction of the association. People who were previously financially stable but found themselves experiencing housing insecurity only after developing chronic illness from COVID-19 are in need supportive policies and interventions, but so are those people who were already experiencing economic precarity prior to infection with SARS-CoV-2 and developed Long COVID as a result. Indeed, our results demonstrate the urgency of addressing housing insecurity among people of lower socio-economic status who develop post-acute sequelae of COVID-19, as the highest risk of housing insecurity was observed among those of lower socio-economic status who also had Long COVID. In short, whether Long COVID precedes housing insecurity or vice versa, it is important that policymakers, health providers, and public health officials are aware that a significant population of people who have not recovered from COVID-19 are struggling to make ends meet while effective treatments have yet to be developed.
The strengths of this analysis include leveraging hundreds of thousands of survey responses over a 7-month period from a nationally representative survey during the third year of the COVID-19 pandemic, providing generalizable estimates of the downstream public health manifestations of the first several waves of infections. The following limitations should also be considered when interpreting the results: First, the assessment of Long COVID status in the Household Pulse Survey was subject to several constraints. Only those who reported a positive COVID-19 test or physician-confirmed diagnosis were asked about long-term symptoms, a conditional case definition for Long COVID which excludes people who were unable to access testing or healthcare at the time of their active infection for any reason, despite the fact that the social and structural drivers of inequality in access to these diagnostic resources have been well-documented (Bilal, Tabb, Barber, & Diez Roux, 2021; Mody, Pfeifauf, & Geng, 2021). Determination of illness duration was also not possible from these data, and questions on the impact of Long COVID symptoms on day-to-day life were limited to only those experiencing symptoms at the time of the survey, despite previous research on episodic and relapsing patterns of symptoms in many people with Long COVID (Davis et al., 2021, 2023). Second, during the pandemic there has been a high degree of heterogeneity in housing policies and social assistance programs across localities in the United States, which was not taken into account. If states and cities with higher populations had much different policy environments than their lower population counterparts, it may introduce bias into average national-level estimates of the association between Long COVID and housing insecurity. Third, the potential for recall and selection bias may challenge the internal and external validity of our results. Recall bias, or any tendency of those experiencing housing insecurity to be systematically more or less likely to recall long term symptoms or attribute non-specific symptoms to COVID-19, could bias estimates away from or towards the null, respectively. Overall response rates to the survey are also low and participation from minoritized communities was generally lower than from non-Hispanic white residents. While it is important to consider that the analytic sample may not be completely representative of the target population of US adults with a history of COVID-19, these threats to validity are mitigated by the sampling design and person-level weights based on the Census Bureau's master address file which has been demonstrated to mitigate non-response bias in earlier iterations of the survey (Peterson, Toribio, Farber, & Hornick, 2021). A considerable number of survey respondents were excluded for not completing questions on housing, however these respondents reported lower income and education, but higher prevalence of functional impairment and similar rates of Long COVID symptoms, indicating that the exclusion of these subjects was not likely to bias the results away from the null.
In conclusion, this study draws attention to the fact that millions of people with Long COVID struggle with routine household expenses, including housing payments, and may be at risk of eviction or foreclosure. While longitudinal and qualitative data are needed to describe in more granular and causal terms how the illness experience of Long COVID relates to social and economic hardships in the context of other disruptive long-term impacts of the pandemic, it is clear that the pandemic continues to have deep and sustained impacts on those with viral-onset chronic illness, and a comprehensive response and recovery effort will require acknowledging, monitoring, and supporting people with Long COVID.
Financial disclosure
This work was supported by National Institutes of Mental Health [Grant number T32-MH013043, 2022]
Ethical statement
Conforming to Columbia University Institutional Review Boards policy on Use of Publicly Available Datasets for Research, formal review was not required. All data are fully de-identified and publicly available from the US Census Bureau at https://www.census.gov/programs-surveys/household-pulse-survey/datasets.html.
CRediT authorship contribution statement
Samuel E. Packard: Conceptualization, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. Ezra Susser: Methodology, Supervision, Writing – review & editing.
Declaration of competing interests
The authors declare no conflicts of interest.
Acknowledgements
We would like to thank Lisa McCorkell and Letícia Soares from the Patient-Led Research Collaborative for their helpful comments on a previous draft of this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2023.101586.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
Data are publicly available from the US Census Bureau website, and analytic code is available at https://github.com/sammy-p/hps_housing.
References
- Assistant Secretary for Public Affairs. US Department of Health and Human Services Fact sheet: End of the COVID-19 public health emergency. HHS.Gov. 2023 https://www.hhs.gov/about/news/2023/05/09/fact-sheet-end-of-the-covid-19-public-health-emergency.html [Text] [Google Scholar]
- Benfer E.A., Vlahov D., Long M.Y., Walker-Wells E., Pottenger J.L., Gonsalves G., et al. Eviction, health inequity, and the spread of COVID-19: Housing policy as a primary pandemic mitigation strategy. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2021;98(1):1–12. doi: 10.1007/s11524-020-00502-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieler G.S., Brown G.G., Williams R.L., Brogan D.J. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. American Journal of Epidemiology. 2010;171(5):618–623. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- Bilal U., Tabb L.P., Barber S., Diez Roux A.V. Spatial inequities in COVID-19 testing, positivity, confirmed cases, and mortality in 3 U.S. Cities. Annals of Internal Medicine. 2021;174(7):936–944. doi: 10.7326/M20-3936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bushman G., Mehdipanah R. Housing and health inequities during COVID-19: Findings from the national household Pulse survey. Journal of Epidemiology & Community Health. 2022;76(2):121–127. doi: 10.1136/jech-2021-216764. [DOI] [PubMed] [Google Scholar]
- Buuren S.V., Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. Journal of Statistical Software. 2011;45(3) doi: 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- Castanares-Zapatero D., Chalon P., Kohn L., Dauvrin M., Detollenaere J., Maertens de Noordhout C., et al. Pathophysiology and mechanism of long COVID: A comprehensive review. Annals of Medicine. 2022;54(1):1473–1487. doi: 10.1080/07853890.2022.2076901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cusack M., Montgomery A.E., Cashy J., Dichter M., Byrne T., Blosnich J.R. Examining veteran housing instability and mortality by homicide, suicide, and unintentional injury. Journal of Social Distress and the Homeless. 2021;30(2):174–180. doi: 10.1080/10530789.2020.1801020. [DOI] [Google Scholar]
- Davis H.E., Assaf G.S., McCorkell L., Wei H., Low R.J., Re’em Y., et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinical Medicine. 2021;38 doi: 10.1016/j.eclinm.2021.101019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis H.E., McCorkell L., Vogel J.M., Topol E.J. Long COVID: Major findings, mechanisms and recommendations. Nature Reviews Microbiology. 2023:1–14. doi: 10.1038/s41579-022-00846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doove L., van Buuren S., Dusseldorp E. mice.impute.cart: Imputation by classification and regression trees. 2012. https://www.rdocumentation.org/packages/mice/versions/3.16.0/topics/mice.impute.cart [Computer software]
- Elder J., King B. Housing and homelessness as a public health issue: Executive summary of policy adopted by the American public health association. Medical Care. 2019;57(6):401. doi: 10.1097/MLR.0000000000001115. [DOI] [PubMed] [Google Scholar]
- Friedman C. Housing insecurity of medicaid beneficiaries with cognitive disabilities during the COVID-19 pandemic. Disability and Health Journal. 2023;16(1) doi: 10.1016/j.dhjo.2022.101375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez S.M., Fullilove R.E. Building up housing to break down health disparities. American Journal of Public Health. 2020;110(3):301–302. doi: 10.2105/AJPH.2019.305521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gromis A., Fellows I., Hendrickson J.R., Edmonds L., Leung L., Porton A., et al. Estimating eviction prevalence across the United States. Proceedings of the National Academy of Sciences. 2022;119(21) doi: 10.1073/pnas.2116169119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang S. The cumulative relationship between housing instability and mental health: Findings from the panel study of income dynamics. Journal of Social Distress and the Homeless. 2022;31(2):191–203. doi: 10.1080/10530789.2021.1925038. [DOI] [Google Scholar]
- Kim D. Financial hardship and social assistance as determinants of mental health and food and housing insecurity during the COVID-19 pandemic in the United States. SSM - Population Health. 2021;16 doi: 10.1016/j.ssmph.2021.100862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine R.L. Addressing the long-term effects of COVID-19. JAMA. 2022;328(9):823–824. doi: 10.1001/jama.2022.14089. [DOI] [PubMed] [Google Scholar]
- Lüdecke D. ggeffects: Tidy data frames of marginal effects from regression models. Journal of Open Source Software. 2018;3(26):772. doi: 10.21105/joss.00772. [DOI] [Google Scholar]
- Lumley T. 2020. survey: Analysis of complex survey samples. [Google Scholar]
- Michelen M., Manoharan L., Elkheir N., Cheng V., Dagens A., Hastie C., et al. Characterising long COVID: A living systematic review. BMJ Global Health. 2021;6(9) doi: 10.1136/bmjgh-2021-005427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mody A., Pfeifauf K., Geng E.H. Using lorenz curves to measure racial inequities in COVID-19 testing. JAMA Network Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.32696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance to End Homelessness . 2023. State of homelessness: 2023 edition.https://endhomelessness.org/homelessness-in-america/homelessness-statistics/state-of-homelessness/ [Google Scholar]
- Nittas V., Gao M., West E.A., Ballouz T., Menges D., Wulf Hanson S., et al. Long COVID through a public health lens: An umbrella review. Public Health Reviews. 2022;43 doi: 10.3389/phrs.2022.1604501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Mahoney L.L., Routen A., Gillies C., Ekezie W., Welford A., Zhang A., et al. The prevalence and long-term health effects of long covid among hospitalised and non-hospitalised populations: A systematic review and meta-analysis. eClinicalMedicine. 2023;55 doi: 10.1016/j.eclinm.2022.101762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlis R.H., Santillana M., Ognyanova K., Safarpour A., Lunz Trujillo K., Simonson M.D., et al. Prevalence and correlates of long COVID symptoms among US adults. JAMA Network Open. 2022;5(10) doi: 10.1001/jamanetworkopen.2022.38804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson S., Toribio N., Farber J., Hornick D. United States Census Bureau; 2021. Nonresponse bias report for the 2020 household Pulse survey. Version 1.0. [Google Scholar]
- Phillips S., Williams M.A. Confronting our next national health disaster—long-haul covid. New England Journal of Medicine. 2021;385(7):577–579. doi: 10.1056/NEJMp2109285. [DOI] [PubMed] [Google Scholar]
- R Core Team R: A language and environment for statistical computing. R Foundation for Statistical Computing. 2021 https://www.R-project.org [Computer software] [Google Scholar]
- Raajkumar A. How effective were national, state, and local eviction moratoria? 2022. https://www.federalreserve.gov/econres/notes/feds-notes/how-effective-were-national-state-and-local-eviction-moratoria-20220621.html
- Rao S., Essien U.R., Powell-Wiley T.M., Maddineni B., Das S.R., Halm E.A., et al. Association of US county-level eviction rates and all-cause mortality. Journal of General Internal Medicine. 2023;38(5):1207–1213. doi: 10.1007/s11606-022-07892-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson M.M., Qasmieh S.A., Kulkarni S.G., Teasdale C.A., Jones H.E., McNairy M., et al. The epidemiology of long coronavirus disease in US adults. Clinical Infectious Diseases. 2023;76(9):1636–1645. doi: 10.1093/cid/ciac961. [DOI] [PubMed] [Google Scholar]
- Shaw M. Housing and public health. Annual Review of Public Health. 2004;25(1):397–418. doi: 10.1146/annurev.publhealth.25.101802.123036. [DOI] [PubMed] [Google Scholar]
- Spatz E.S., Gottlieb M., Wisk L.E., Anderson J., Chang A.M., Gentile N.L., et al. Three-month symptom profiles among symptomatic adults with positive and negative severe acute respiratory syndrome coronavirus 2 tests: A prospective cohort study from the inspire group. Clinical Infectious Diseases. 2023;76(9):1559–1566. doi: 10.1093/cid/ciac966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Census Bureau Household Pulse survey technical documentation. Census.Gov. 2022 https://www.census.gov/programs-surveys/household-pulse-survey/technical-documentation.html [Google Scholar]
- US Census Bureau Household Pulse survey phase 3.5. Census.Gov. 2022 https://www.census.gov/newsroom/press-releases/2022/household-pulse-phase-3-5.html [Google Scholar]
- US Census Bureau Measuring household experiences during the coronavirus pandemic. Census.Gov. 2022 https://www.census.gov/householdpulsedata [Google Scholar]
- US Census Bureau Household Pulse survey public use file (PUF) Census.Gov. 2023 https://www.census.gov/programs-surveys/household-pulse-survey/datasets.html [Google Scholar]
- Weeks J.D., Dahlhamer J.M., Madans J.H., Maitland A. Measuring disability: An examination of differences between the Washington group short set on functioning and the American community survey disability questions. National Health Statistics Reports. 2021;161 https://stacks.cdc.gov/view/cdc/107202 [PubMed] [Google Scholar]
- Wysocki A.C., Lawson K.M., Rhemtulla M. Statistical Control requires causal justification. Advances in Methods and Practices in Psychological Science. 2022;5(2) doi: 10.1177/25152459221095823. [DOI] [Google Scholar]
- Zou G. A modified Poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are publicly available from the US Census Bureau website, and analytic code is available at https://github.com/sammy-p/hps_housing.