Abstract
Background
Between 2016 and 2020, over 600,000 youth were served annually by the foster care system. Despite approximately half of foster youth struggling with emotional or behavioral challenges, few receive much-needed services to address their mental health concerns. Family-based interventions are efficacious in addressing both youth and caregiver mental health needs; however, foster youth participation in these family-based interventions is limited by many barriers, including out-of-home placement far from their family of origin. Telehealth is a promising tool for mitigating barriers to access to treatment interventions for foster youth and their families.
Objective
This study aims to understand child welfare system professionals’ perspectives on enabling factors and barriers to providing family-based interventions via telehealth to youth in out-of-county foster care placement.
Methods
This qualitative study derived themes from 3 semistructured focus groups with child welfare system professionals. Participants were asked to discuss how family-based interventions are delivered to foster youth and their caregivers in their jurisdictions, as well as to share their thoughts about how to use telehealth to improve access to family-based interventions for families with youth in out-of-home placement. Data were analyzed using constant comparative analysis and inductive thematic analysis, with the Behavioral Model for Vulnerable Populations as the theoretical framework.
Results
Participants were 19 child welfare system professionals (eg, social workers, residential treatment staff, and supervisors) who participated in 1 of the 3 focus groups (6-7/group). Most participants were women (n=13, 68%), White individuals (n=10, 53%), and social workers (n=8, 42%). On average, participants worked in the child welfare system for 16.6 (SD 8.3) years. Participants identified multilevel factors impacting family-based intervention delivery including environmental factors (eg, Medicare billing and presumptive transfer), predisposing characteristics (eg, psychological resources), enabling factors (eg, transportation and team-based youth-centered care), and need factors (eg, motivation to engage). Participants expressed optimism that telehealth could increase access to needed mental health care, diverse providers, and longevity of care while also expressing some concerns regarding telehealth access and literacy.
Conclusions
Child welfare system professionals highlight the need to develop policies and telehealth interventions that are youth versus placement centered, include resources that limit barriers and bolster motivation for engagement, and follow a team-based care model. Findings from this study inform how telehealth can be used to increase access to and engagement with family-based interventions for youth in out-of-home placements and their caregivers of origin.
Keywords: foster youth, telehealth, family-based interventions, mental health
Introduction
Background
Approximately one-third of all children and over half of Black children in the United States experience a Child Protective Services investigation for maltreatment (ie, physical, sexual, or emotional abuse or neglect) before the age of 18 years [1]. In 2020, a total of 631,832 youth were served by foster care (ie, out-of-home placement organized by child welfare services) [2], with Black and Indigenous youth having the highest risk of placement [3]. Although nearly half of foster youth exhibit clinically significant emotional and behavioral needs, one study found that only 11.7% connected with mental health services within 1 year of maltreatment investigation. Access is especially limited for Black and Latinx foster youth [4,5].
Family-based interventions are the gold standard for addressing externalizing and internalizing mental health disorders in adolescents, including foster youth [6,7]. Strengthening interpersonal relationships between youth and caregivers bolsters a youth’s social competence and behavioral adjustment, reduces caregiver stress, and supports family reunification [7,8]. Unfortunately, many foster youth are placed far from caregivers (eg, in January 2022, in Northern California Bay Area counties, 22%-66% of youth aged 0-21 years were placed out of county) [9], making in-person family-based interventions challenging.
Telehealth, which has been shown to have comparable feasibility, outcomes in assessment and symptom reduction, and satisfaction as in-person care, may circumvent this barrier and improve access to mental health interventions [10-12]. Telehealth service delivery for foster youth and families has been shown to maintain service quality, improve access and engagement, and be perceived by users as beneficial [13-15]. Recently, there has been increased interest in telehealth, as the COVID-19 pandemic has provided the impetus for the rapid adoption of videoconferencing in many settings, including the juvenile justice system, which also separates youth from their families. Given the feasibility and acceptability of telehealth service delivery, there has been a call to leverage technology for mental health interventions for system-involved youth and their families [16]. While research into telehealth delivery of mental health services is gaining momentum, little is known about the effectiveness of family-based telehealth interventions for foster youth and their families or how best to implement such services.
Objective
The aim of this study was to understand child welfare system professionals’ perspectives to inform the adaptation of an existing empirically supported, in-person, family-based affect management intervention for telehealth delivery tailored for foster youth.
Methods
Study Design
This study analyzes focus group data to guide the iterative adaptation of an empirically supported, in-person, family-based affect management intervention [17] to serve foster youth and their families via telehealth as part of phase 1 of the Family Telehealth Project. The overall study aims to improve behavioral health outcomes and reduce housing instability among adolescent foster youth (aged 12-18 y) placed out of county, for whom in-person family-based interventions with caregivers of origin are typically not feasible [18]. Phase 2 is an ongoing clinical trial to evaluate the effectiveness of this intervention.
Sample
Eligible participants were English-speaking child welfare system professionals (eg, social workers, supervisors, and program staff) working with foster youth and their families. Staff at child welfare services in a Northern California county and a short-term residential therapeutic program (STRTP) in Southern California, a placement for some Northern California youth, were recruited by phone and email. Eligibility screening was performed and informed consent was obtained over phone (using DocuSign to document written consent) or in person before the focus group. Eligible individuals were invited to a one-time focus group at their workplace. Additional participants were identified by snowball sampling.
Data Collection
Three in-person 90-minute focus groups were conducted between December 2019 and February 2020, with 6 to 7 participants per group, a notetaker, and facilitators. Facilitators used a standardized semistructured guide targeting (1) the current landscape of family-based interventions for foster youth, (2) perspectives on content topics for a family-based intervention, and (3) recommendations for telehealth delivery (eg, timing). The participants completed a brief demographic questionnaire at the end of the focus group. Focus group discussions were audio recorded, transcribed verbatim, and deidentified. Facilitators and notetakers used written notes to draft debriefs including key themes and issues to address in the next focus group (eg, unclear questions and timing).
Ethical Considerations
All study procedures were approved by the institutional review board of the University of California, San Francisco (number 19-28922). The focus group participants provided written informed consent before participation. Personal data collected in this study included information about the system professionals’ demographics, thoughts about telehealth and family-based interventions for child welfare–involved families, and digital recordings of focus groups. No names or other identifying information was included in the analytic data and during focus groups. Participants were reminded frequently not to indicate their name or any identifying information about themselves or others. Focus group transcripts were deidentified before analysis. Participants were provided with food during the focus group and, if allowed by their agency, offered a US $40 Visa gift card as compensation.
Qualitative Analysis
Using inductive thematic analysis, 3 authors reviewed transcripts and created an initial coding scheme [19]. Two authors independently coded all focus group transcripts, updated the coding scheme to resolve coding differences, reviewed each transcript twice to create a master coding scheme, and reviewed again to develop master transcripts coded in ATLAS.ti (version 8.0; ATLAS.ti Scientific Software Development GmbH) [20] for each focus group. Two coders drafted and revised analytic memos using the constant comparative analysis method [21] to identify and categorize key themes from the data [22].
Theoretical Framework
The Behavioral Model for Vulnerable Populations [23] represents a revision of the Behavioral Model of Health Services Use [24] and was used as a theoretical framework to organize emerging themes from the focus groups. This model suggests that health care utilization is influenced by a population’s predisposing characteristics, enabling resources, and overall need [24]. Subsequent revisions to the original theoretical model incorporated environmental factors (health care system and external environment), health outcomes, definitions of health behavior as personal health practices and health service utilization, and feedback loops to emphasize interactions between components [24]. The Behavioral Model for Vulnerable Populations is an adaptation designed to understand health services utilization among underserved populations including people from minoritized groups, children, and those with housing instability by adding “Vulnerable Domains,” in addition to “Traditional Domains,” for each variable (eg, mental illness in predisposing characteristics; competing needs and transportation in enabling factors) [23]. With “Vulnerable Domains” variables in mind, our data are presented using a version of the model published by Phillips et al [25], highlighting contextual factors including provider-related variables. The authors acknowledge that the term “vulnerable” is problematic given the placement of blame on the individual rather than on an inadequate system; however, the term is used for consistency with the theoretical model [23].
Results
Overview
Participants (N=19; 6-7/group) predominantly identified as women (n=13, 68%), White (n=10, 53%), non-Latinx (n=14, 74%), and social workers (n=8, 42%). On average, participants worked in child welfare services for 16.6 (SD 8.3) years. Table 1 presents additional demographic information.
Table 1.
Demographic characteristics of child welfare system professionals who participated in 1 of 3 focus groups (N=19).
| Characteristic | Participants, n (%) | |||
| Gender | ||||
|
|
Women | 13 (68) | ||
|
|
Men | 6 (32) | ||
| Age (y) | ||||
|
|
25-34 | 5 (26) | ||
|
|
35-44 | 7 (37) | ||
|
|
45-54 | 5 (26) | ||
|
|
55-64 | 2 (11) | ||
| Racea | ||||
|
|
American Indian or Alaska Native | 1 (5) | ||
|
|
Asian | 2 (11) | ||
|
|
Black, African American, or Haitian | 4 (21) | ||
|
|
White | 10 (53) | ||
|
|
Mixed race | 2 (11) | ||
|
|
Otherb | 4 (21) | ||
| Ethnicity | ||||
|
|
Hispanic or Latinx | 5 (26) | ||
| Setting and role | ||||
|
|
Human services agency | 12 (63) | ||
|
|
|
Case manager | 1 (5) | |
|
|
|
Social worker | 8 (42) | |
|
|
|
Supervisor | 3 (16) | |
|
|
STRTPc | 7 (37) | ||
|
|
|
Mental health or substance use coordinator | 2 (11) | |
|
|
|
Psychotherapist | 1 (5) | |
|
|
|
STRTP staff | 2 (11) | |
|
|
|
Administrator | 1 (5) | |
|
|
|
Supervisor | 1 (5) | |
aCategories are not mutually exclusive and reflect how participants self-identified.
bOther: Three wrote Latinx or Hispanic. One wrote Mexican/French.
cSTRTP: short-term residential therapeutic program.
Participants identified multilevel factors impacting family-based intervention utilization (Figure 1), including environmental factors (Table 2) and population characteristics (Table 3).
Figure 1.
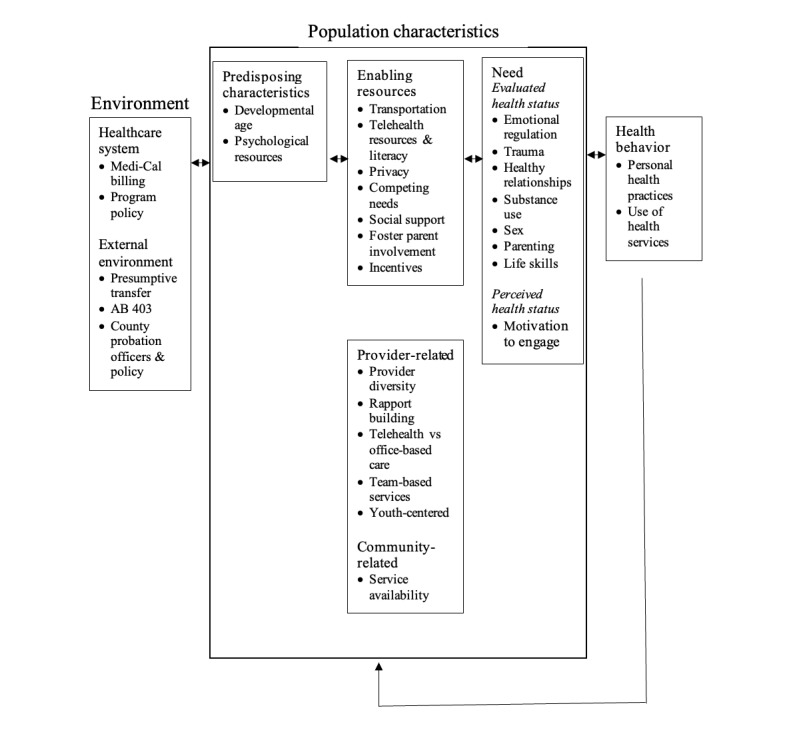
Factors, per child welfare system professionals, influencing the implementation of family-based telehealth interventions for foster youth and their families. Organized using the Behavioral Model of Health Services for Vulnerable Populations [23] and Utilization Model [25], both adaptations of the Behavioral Model of Health Services Use [24]. AB: Assembly Bill.
Table 2.
Environmental variables affecting the utilization of family-based interventions for foster youth and families per child welfare system professionals.
| Variable | Example quotations | |
| Healthcare system variables | ||
|
|
Medi-Cal billing |
|
|
|
Program policy |
|
| External environment variables | ||
|
|
Presumptive transfer |
|
|
|
Assembly Bill 403 |
|
|
|
County POsb and policy |
|
aSTRP: short-term residential therapeutic program.
bPO: probation officer.
Table 3.
Population characteristics affecting the utilization of family-based interventions for foster youth and families, per child welfare system professionals.
| Variable | Example quotations | |||
| Predisposing variables | ||||
|
|
Developmental age |
|
||
|
|
Psychological resources |
|
||
| Enabling resource variables | ||||
|
|
Transportation |
|
||
|
|
Telehealth resources and literacy |
|
||
|
|
Privacy |
|
||
|
|
Competing needs |
|
||
|
|
Social support |
|
||
|
|
Foster parent involvement |
|
||
|
|
Incentives |
|
||
| Enabling provider-related variables | ||||
|
|
Provider diversity |
|
||
|
|
Rapport building |
|
||
|
|
Telehealth vs office-based care |
|
||
|
|
Team-based services |
|
||
|
|
Youth centered |
|
||
| Enabling community-related variables | ||||
|
|
Service availability |
|
||
| Need variables | ||||
|
|
Evaluated health status | |||
|
|
|
Emotional regulation, trauma, healthy relationships |
|
|
|
|
|
Substance use, parenting, sex, life skills |
|
|
|
|
Perceived health status | |||
|
|
|
Motivation to engage |
|
|
aBART: Bay Area Rapid Transit.
bSRO: single room occupancy.
cSTRTP: short-term residential therapeutic program.
dLGBT: lesbian, gay, bisexual, transgender.
eISFC: intensive supportive foster care.
fRegional center: Locally based nonprofit private corporation coordinated by the Department of Developmental Services in California to serve as a local resource to connect individuals with developmental disabilities and their families to services.
gDBT: dialectical behavior therapy.
Environmental Factors
Medi-Cal, state, and program policies were cited by participants as environmental barriers to the continuity of care with mental health providers. Multiple participants described presumptive transfer (policy Assembly Bill 1299: “responsibility for providing or arranging for specialty mental health services shall promptly transfer from the county of original jurisdiction to the county in which the foster child resides”) [26] as a major impediment, given that youth must change providers when moving counties for placement. One social worker explained that while waiving presumptive transfer is an option, obtaining approval often delays services. A social work supervisor wished that Medi-Cal coverage for mental health care would be state-wide rather than county-based coverage to promote consistency and access to providers. Participants also noted the impact on provider continuity of Assembly Bill 403, a policy outlawing group homes (facilities providing 24-hour nonmedical care and supervision to youth aged <19 years who are under court jurisdiction or who are dependents of the court) and instead requiring STRTPs [27]. STRTPs are similar to group homes but are additionally mandated to provide in-house specialized therapeutic treatment [28]. Every time foster youth enter an STRTP, they must establish care with that STRTP’s in-house providers and discontinue care with prior providers.
Program policies limiting the distance a provider can travel to work with youth was cited as a barrier to treatment. Participants explained that one local provider of wraparound services, a team-based service delivery model using a strength-based need-driven approach [29], can only travel up to 90 miles, disrupting care when youth are placed farther away. Rare exceptions are made, often based on distance, rather than a youth’s needs.
An administrator cited a county’s Medi-Cal approval process to use telehealth as a barrier; the process involves documenting nuanced policies and procedures that are Health Insurance Portability and Accountability Act (HIPAA) compliant, approval by the mental health contract and the specific mental health program, and an annual review. A social work supervisor also expressed concerns that if the youth are already in individual therapy, additional family-based therapy may not be paid for by Medi-Cal.
Varying roles and policies of probation officers by county were discussed as impacting treatment for youth who are dually involved in juvenile justice and foster care. Participants at an STRTP serving dually involved youth explained that probation officers, depending on the county, have the ability to decide when, how, and which support persons could be involved in a youth’s care, timing of family visits or reunification, and placement of youth in independent living programs versus with their primary support person (if not a legal guardian). They also shared that probation officers may not provide a projected court date for completion of services and possible reunification, which per an administrator, “creates unnecessary anxiety” for youth and limits the ability to use home visits to practice problem solving, communication, boundaries and accountability skills learned in placement.
Population Characteristics: Predisposing Characteristics
Participants highlighted that a youth’s trauma history can affect their emotion regulation skills, psychological resources, and relationships with caregivers. Multiple participants expressed a desire for family-based interventions to be offered to transitional-age youth. One social worker highlighted transitional age (16-24 years) as an especially vulnerable period:
...And a lot of them, because of the trauma they experienced, their biological age is not necessarily matching their emotional, developmental [age]...
Social worker
In 2 focus groups, participants expressed concerns that youth would feel uncomfortable sharing sensitive information (eg, sexual health) during family-based telehealth sessions with caregivers of origin with whom they are building a relationship or with multiple adults, including providers and family, at once. Two participants commented that frequent meetings with many providers, such as in wraparound services, can be overwhelming for youth. A STRTP staff member added “...and a lot of times, they just want to be kids. Yeah, they just want their downtime, so it really depends on the individual.” Similarly, participants indicated caregiver mental health and lack of openness during sessions as barriers to treatment. A social worker added that it is advantageous when a caregiver has a therapist to support communication between the caregiver’s therapist and the youth’s providers. One social worker explained that both caregivers and youth can be resistant to therapy due to discomfort and believed that a skills-based intervention would be less overwhelming. In contrast, a mental health or substance use coordinator believed that a structured skills-based intervention could be challenging for youth to “stay focused” if they want to discuss other topics with family.
Population Characteristics: Enabling Resources
A lack of resources (transportation, time, and finances) was highlighted as a barrier to in-person family-based interventions. All 3 focus groups cited transportation barriers, including lack of access to a vehicle, driver, or funding, and difficulty with limited complex public transportation routes. Participants observed that offering transportation resources to families facilitated connections with providers; however, they noted limitations due to liability when directly transporting youth. Limited time and competing needs were highlighted as salient barriers. An administrator described families as “multi-stressed,” and a psychotherapist noted that caregivers’ work caused scheduling constraints. The participants explained that with limited time to be together, many families prefer quality time over therapy. Participants at an STRTP explained that youth at their facility also have competing program and community obligations including school, extracurricular activities, employment, and groups. Some participants believed that providing incentives to caregivers would help increase their engagement in family-based interventions. They reflected on the challenges of consistent caregiver involvement and their experience of seeing incentives work.
In discussions about telehealth, access to resources (technology, technology literacy, privacy) and feasibility were considered. Some participants said that most youth and adults are “attached” to their phones, making engagement and feasibility easier. One social worker commented that many youth without cellular service connected to caregivers via Wi-Fi using WhatsApp or Messenger. Participants expressed concerns that some families have limited access to technology, especially computers and Wi-Fi; a supervisor suggested that the provision of stipends for smart technology or the internet could facilitate participation. Participants discussed programs that provide clients with free smart phones, noting the variable reliability of devices (iFoster and Obama phones). Multiple participants expressed the need to address the limited technology literacy of some caregivers. Participants also discussed privacy concerns including people intentionally eavesdropping, difficulty finding private spaces with Wi-Fi, and providers needing HIPAA-compliant technology. A case manager stated that for some caregivers, a safe environment outside the home is preferred to facilitate family meetings and provide therapeutic boundaries. Alternatively, a supervisor commented that with the flexibility of telehealth, youth can control the level of confidentiality based on their location during sessions.
Social support was discussed as an enabling resource for family-based interventions. Multiple participants expressed an interest in an inclusive definition of family, identifying siblings, foster parents, or any adult figure beyond just parents who can provide consistent social support and develop strong connections with the youth. A supervisor suggested that sibling participation would allow for continued connection and could address mutual trauma from separation. Favoring a broad definition of social support, a social worker explained the following:
12 to 17-year-olds, the reality for the youth that come to us, they’re not going back to the parent.
Social worker
One social worker expressed that in some instances, involving parents can be counterproductive if they have their own mental health needs and are not ready to engage as caregivers. An additional caveat discussed was “because a lot of youth are unaccompanied, when they come into foster care, the parents’ services get bypassed,” and family therapy is not offered. They emphasized consistency and connection, understanding that their work with youth is time limited.
Participants suggested involving foster parents to collaborate with caregivers on consistent rules, model parenting skills during visits, and help with logistics, such as transportation. Participants added that their involvement could be an opportunity for youth to meet foster families before placement. Two social workers explained that increased foster parent involvement could be particularly effective closer to reunification. A social worker explained that court permission must be granted to biological parents to visit the foster homes. An additional barrier, especially for younger youth, is some foster parents’ unwillingness to have biological parents in their homes or know their address.
Population Characteristics: Provider-Related Variables
Participants identified several provider-related enabling factors for family-based interventions, including rapport with families, team-based services, a youth-centered approach, and choice of service delivery modality. A case manager shared that some families mistrust government agencies, and multiple participants emphasized that building relationships leads to better engagement of families with interventions. An STRTP administrator explained providing “food or furniture or whatever they need to pass a home assessment,” “helping them get into services,” or “see(ing) their kid be engaged” in the program can help build trust. Participants shared the value of “trying our best to empower the family and really establishing the fact that we’re here to work as a team and you’re the expert on your child” in addition to reinforcing “we’re here to help, we’re not here to judge.” A supervisor observed that engaging creatively in youth interests, such as “therapy while shooting baskets... [going] out to lunch, or... therapy while taking a walk” is particularly effective for rapport building.
Two focus groups highlighted team-based models of care that support collaboration among agencies and service providers as important for treatment success. Wraparound services and an adaptation called intensive supportive foster care were explained as successful team-based models of 2 to 3 providers including case managers, care coordinators, therapists, and psychiatrists. Unlike wraparound services, intensive supportive foster care is attached to a particular foster family agency. A participant at an STRTP explained that their program uses a team-based model, including caseworkers who are present as a “source of stability,” care coordinators who serve as mental health clinicians and address acute escalation, and clinical supervisors. Participants explained that having a diverse team of providers facilitates rapid intervention when situations escalate. Additional team members can include the youth, caregivers, youth’s attorney, court appointed special advocate (CASA) mentors (ie, volunteer court–appointed special advocates who often follow youth from placement to placement), and aftercare workers who check in with the family. Participants emphasized the importance of a communication workflow between clinicians delivering a telehealth intervention and the family’s primary clinician in the event of a crisis.
Multiple participants cited the importance of youth- and family-centered services:
I might direct someone to be a little more strategic or structural versus experiential based on what’s going on within a family.
Supervisor
A youth-centered approach is also manifested through “family team meetings where the whole team and the family and the youth get together.” As previously discussed, billing by placement is a major barrier to prioritizing needs of youth, who may take time to build trust with their providers. Multiple participants commented that the session frequency, length, and topics covered should be guided by a youth’s needs. Furthermore, some participants agreed with youth requests for diverse providers who share their identity characteristics (ie, sexual identity, race, ethnicity, culture, and gender) to engender trust. Multiple participants commented on the lack of providers who can provide services in non-English languages, resulting in “a lot get[ting] lost in translation.” Participants believed that interventions would be more successful if clinicians had expertise working with diverse populations, including those with low literacy levels, monolingual Spanish speakers, and youth with developmental delays.
When considering the modality for providers to deliver family-based interventions, participants discussed the advantages and disadvantages of telehealth. Multiple participants favored in-person, video, or hybrid sessions over phone-based sessions. Participants expressed that incorporating some in-person sessions could provide “that real element” and have clinical advantages. Many agreed that the engagement and tolerance of session length varies based on the modality and amount of face-to-face interaction: in person>video>phone. The perceived benefits of telehealth included eliminating transportation barriers, consistency of care for youth who moved for placement or college, flexibility of when and where sessions take place, rapid connection to clients during emergencies, access to diverse providers with shared identity, ease of discussing sensitive topics on screen versus in person, and increased engagement due to high phone use among adults and youth. Concerns included youth “clicking away at something else” and thus needing in-person supervision, interventionists missing behavioral cues making de-escalation and rapport building harder, youth feeling intimidated with multiple adults on screen and no support system physically with them, and families having limited exposure to a youth’s progress leading to less engagement in treatment planning, as well as the aforementioned barriers related to access to technology, privacy concerns, and billing and program policies.
Community-Related Variables
Multiple participants discussed limited appropriate service availability as a barrier to treatment, especially for youth with cognitive delays, dual diagnosis, serious mental illness, behavioral challenges, and/or parenting their own children. Participants explained that they must use general referrals even when the service is unable to meet the youth’s unique needs, and this may expose them to other youth who could exploit them. When programs do exist, they may be unfeasibly distant. In addition, a social worker explained how talk therapy is used for everyone but does not work for many. Even when different therapy modalities are available, the limited quantity of services and associated waitlists are prohibitive. Multiple participants discussed how the quantity and quality of resources varies by county. Smaller counties were noted to have fewer staff and less robust services than counties with better funding and greater monitoring and accountability for services. When services are available, distance and transportation pose barriers to access.
Need Variables
Participants discussed how variables influencing emotional and behavioral symptoms are areas of evaluated need that could benefit from therapeutic interventions. An STRTP staff member explained that the extent of behavioral challenges affects how much family-based work is needed before home visits or reunification. The suggested session topics included emotional regulation, trauma, fostering healthy relationships, substance use, sex, parenting, and life skills. A social worker explained youth’s complex emotions may manifest as acting out. A case manager observed “parents are probably having a parallel process” on “regulating how they react to the world.” Trauma and the associated emotions especially those related to entry into foster care were suggested topics in all 3 focus groups. Describing the trauma related to entry into foster care, participants explained that many youth are hoping for an apology from their caregivers of origin. Additional suggested topics included domestic violence and healthy relationships, including from whom to seek support from, “how to deal with your feelings about wanting love and how to get it in a healthy way,” and understanding how interpersonal conflict between youth and caregivers manifests in other relationships. A social worker commented that “socioeconomic dependence” in relationships is relevant but overlooked. Substance use, especially marijuana, was perceived as prevalent; one social worker estimated that 80% of the youth with whom they have worked with use substances. A participant at an STRTP serving dually involved youth thought that discussing delinquency or justice involvement would be relevant. Although multiple participants agreed that sexual health is an important topic, some were apprehensive of youth being comfortable with intimate discussions with their caregivers with whom they are building a relationship or with multiple adults. Some worried that dually-involved youth would also be uncomfortable with intimate discussions when probation was involved in the parent-child relationship. They stated that youth may be more comfortable discussing intimacy individually with a noncaregiver. Participants commented that rule setting is challenging for many biological and foster parents. They perceived benefits to setting “ground rules, expectations, and compromises” before placement or before reunification. In addition, parenting as a youth was suggested as a topic for a subset of clients. Independent living skills, including “financial skills, like budgeting, housing”; “organization, like calendar, to-do lists”; “following through, like to appointments”; “returning calls”; and “goal setting” were suggested in all 3 focus groups.
Motivation to engage in care can be viewed as a proxy for perceived health status and self-evaluated need for services. Multiple participants reported a perceived lack of motivation to engage by some youth due to forced therapy with multiple providers. Participants commented that many youth are ambivalent and frustrated with retelling their story to paid professionals. They may also be more willing to engage in therapy, depending on their treatment stage and how interesting they find a therapy session. The perceived lack of motivation of some caregivers to engage or have their youth engage in treatment is also a barrier. The participants cited competing demands, displaced responsibility, and resistance to change as factors that diminish motivation and perceived need. An STRTP staff member explained that many families do not realize that they must play an active role in treatment. Per stakeholders, caregiver motivation to engage can be hindered by limited exposure to youth progress.
Discussion
Principal Findings
When developing and implementing an intervention to best serve foster youth and their families, child welfare system professionals’ perspectives are invaluable, given their knowledge of barriers and enabling factors. Participants identified environmental and population characteristic variables, emphasizing the complexity of structural and individual aspects that influence service utilization and treatment. Barriers to family-based telehealth interventions, especially relevant to foster youth and their families, include placement-focused care due to policies restricting the delivery and payment of treatment; perceived lack of engagement; and less access to transportation, technology, privacy, and time. Enabling factors include social support, foster parent involvement, and financial incentives. Providers can further support success by prioritizing youth-centered team-based care, minimizing changes in providers, increasing provider diversity and specialized service availability, and focusing on intervention topics relevant to lived experiences. Notably, these themes overlap with a systems of care framework, which includes the core values of choosing services and supports that are (1) family driven and youth guided, (2) community based, and (3) culturally and linguistically competent [30].
This study supports telehealth as a promising modality to minimize barriers and bolster enabling factors when delivering family-based interventions to foster youth and their caregivers of origin. The study participants were optimistic that telehealth could improve access to consistent care, remove transportation barriers, and better match diverse or specialized providers to youth. Previous studies suggest that foster youth and their families view telehealth as favorable and effective in reducing barriers to engagement, such as transportation [13,14]. A recent study indicated that telehealth service delivery for foster youth is comparable to in-person service delivery, and families attended more appointments via telehealth than in-person services [15]. In addition, although this study occurred before the COVID-19 pandemic, during which telehealth was rapidly implemented, our findings align with those of a survey of foster youth, caregivers, and foster parents during the COVID-19 pandemic; the survey had most participants self-identifying as Black or Latinx that is reflective of the overrepresentation of Black and Latinx youth in child welfare. Of the 228 participants, 77.2% (n=176) found telehealth to be of high quality, and 196 participants indicated telehealth as useful in increasing access and continuity of care [14].
Strengths and Limitations
A major strength of this study is that multiple perspectives were captured, including those of social workers, STRTP staff, mental health or substance use coordinators, case managers, and supervisors, who are well positioned to identify system-related barriers and enabling factors. Participants worked on average over 16 years in the child welfare system, suggesting that they have extensive experience working with the population. We did not assess their educational background in our assessment, which could have impacted professional views. Given that this is a nascent area of research with respect to conducting family-based telehealth interventions with families separated by the foster care system, our study was not intended to produce widely generalizable findings, which are still needed. Participants were employed in Northern and Southern California counties, suggesting that the results may be generalizable to these parts of California but may not generalize to other states or other parts of California. For example, barriers including state policies such as presumptive transfer and California Medicaid billing are state specific, while enabling factors such as transportation, foster parent involvement, and service availability are likely shared by foster youth and their families across the nation and beyond. In addition, although youth and family perspectives were discussed by the participants, they were not directly captured. The sample size of 3 focus groups with 19 participants may be viewed as limited; however, we were guided by the literature suggesting adequate saturation with relatively small sample sizes [31,32].
Conclusions
Child welfare system professionals provided important considerations when creating and implementing a family-based intervention for foster youth and their caregivers of origin. Drawing from their perspectives, we must advocate for policies and services that are youth centered rather than placement centered, provide resources to limit barriers, bolster motivation to engage, and structure teams to promote collaboration.
Acknowledgments
We thank our community and system partners and the youth and families for their invaluable contributions to this research. This work was supported by the Visa Foundation (principal investigator [PI]: MT-S), the American Psychological Association (PIs: JBF and MT-S), and the National Institute on Drug Abuse (grants K23DA050798 and K24DA046569; PIs: JBF and MT-S). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, Visa Foundation, or the American Psychological Association. This work was previously presented at the American Psychiatric Association Annual Meeting, New Orleans, Louisiana (May 22, 2022).
Abbreviations
- CASA
court appointed special advocates
- HIPAA
Health Insurance Portability and Accountability Act
- STRTP
short-term residential therapeutic program
Data Availability
The data set generated during this study is not publicly available due to ethical concerns about possible reidentification with this small study sample. Study metadata (eg, focus group guide and codebook) are available from the corresponding author on request.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Kim H, Wildeman C, Jonson-Reid M, Drake B. Lifetime prevalence of investigating child maltreatment among US children. Am J Public Health. 2017 Feb;107(2):274–80. doi: 10.2105/AJPH.2016.303545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.AFCARS report #28. U.S. Department of Health and Human Services. 2021. Nov 19, [2022-03-28]. https://www.acf.hhs.gov/cb/report/afcars-report-28 .
- 3.Wildeman C, Emanuel N. Cumulative risks of foster care placement by age 18 for U.S. children, 2000-2011. PLoS One. 2014 Mar 26;9(3):e92785. doi: 10.1371/journal.pone.0092785. https://dx.plos.org/10.1371/journal.pone.0092785 .PONE-D-13-34875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hurlburt MS, Leslie LK, Landsverk J, Barth RP, Burns BJ, Gibbons RD, Slymen DJ, Zhang J. Contextual predictors of mental health service use among children open to child welfare. Arch Gen Psychiatry. 2004 Dec;61(12):1217–24. doi: 10.1001/archpsyc.61.12.1217. https://europepmc.org/abstract/MED/15583113 .61/12/1217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burns BJ, Phillips SD, Wagner HR, Barth RP, Kolko DJ, Campbell Y, Landsverk J. Mental health need and access to mental health services by youths involved with child welfare: a national survey. J Am Acad Child Adolesc Psychiatry. 2004 Aug;43(8):960–70. doi: 10.1097/01.chi.0000127590.95585.65.S0890-8567(09)61359-9 [DOI] [PubMed] [Google Scholar]
- 6.Diamond G, Josephson A. Family-based treatment research: a 10-year update. J Am Acad Child Adolesc Psychiatry. 2005 Sep;44(9):872–87. doi: 10.1097/01.chi.0000169010.96783.4e.S0890-8567(09)62193-6 [DOI] [PubMed] [Google Scholar]
- 7.Leve LD, Fisher PA, Chamberlain P. Multidimensional treatment foster care as a preventive intervention to promote resiliency among youth in the child welfare system. J Pers. 2009 Dec;77(6):1869–902. doi: 10.1111/j.1467-6494.2009.00603.x. https://europepmc.org/abstract/MED/19807861 .JOPY603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walton E. In-home family-focused reunification: a six-year follow-up of a successful experiment. Soc Work Res. 1998 Dec;22(4):205–14. doi: 10.1093/swr/22.4.205. [DOI] [Google Scholar]
- 9.Out-of-county placements - Q2 23. California Child Welfare Indicators Project. [2022-09-03]. https://ccwip.berkeley.edu/childwelfare/static/PlacementGrids/r/fcp/s .
- 10.Gloff NE, LeNoue SR, Novins DK, Myers K. Telemental health for children and adolescents. Int Rev Psychiatry. 2015;27(6):513–24. doi: 10.3109/09540261.2015.1086322. [DOI] [PubMed] [Google Scholar]
- 11.Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, Yellowlees PM. The effectiveness of telemental health: a 2013 review. Telemed J E Health. 2013 Jun;19(6):444–54. doi: 10.1089/tmj.2013.0075. https://europepmc.org/abstract/MED/23697504 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barnett P, Goulding L, Casetta C, Jordan H, Sheridan-Rains L, Steare T, Williams J, Wood L, Gaughran F, Johnson S. Implementation of telemental health services before COVID-19: rapid umbrella review of systematic reviews. J Med Internet Res. 2021 Jul 20;23(7):e26492. doi: 10.2196/26492. https://www.jmir.org/2021/7/e26492/ v23i7e26492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keilman P. Telepsychiatry with child welfare families referred to a family service agency. Telemed J E Health. 2005 Feb;11(1):98–101. doi: 10.1089/tmj.2005.11.98. [DOI] [PubMed] [Google Scholar]
- 14.Telehealth white paper: accomplishments of telehealth within New York’s child welfare system: an exploratory survey. Clinicians in Child Welfare. 2020. [2022-07-31]. https://goodshepherds.org/wp-content/uploads/2021/01/Teleheath-White-Paper.pdf .
- 15.Coon JC, Bush H, Rapp JT. Eight months of telehealth for a state-funded project in foster care and related services: progress made and lessons learned. Behav Anal Pract. 2022 Mar 16;15(4):1348–60. doi: 10.1007/s40617-022-00682-z. https://europepmc.org/abstract/MED/35313702 .682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tolou-Shams M, Bath E, McPhee J, Folk JB, Porche MV, Fortuna LR. Juvenile justice, technology and family separation: a call to prioritize access to family-based telehealth treatment for justice-involved adolescents' mental health and well-being. Front Digit Health. 2022 May 23;4:867366. doi: 10.3389/fdgth.2022.867366. https://europepmc.org/abstract/MED/35677312 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tolou-Shams M, Dauria E, Conrad SM, Kemp K, Johnson S, Brown LK. Outcomes of a family-based HIV prevention intervention for substance using juvenile offenders. J Subst Abuse Treat. 2017 Jun;77:115–25. doi: 10.1016/j.jsat.2017.03.013. https://europepmc.org/abstract/MED/28476263 .S0740-5472(16)30340-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Folk JB, Gill H, Ordorica C, Rodriguez CA, Holloway ED, Meza J, Tolou-Shams M. An ecodevelopmental framework for engaging diverse youth in foster care and their families into technology-based family intervention research trials. Front Digit Health. 2022 May 13;4:866139. doi: 10.3389/fdgth.2022.866139. https://europepmc.org/abstract/MED/35633735 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006 Jun;27(2):237–46. doi: 10.1177/1098214005283748. [DOI] [Google Scholar]
- 20.Friese S. Qualitative Data Analysis with ATLAS.ti. Thousand Oaks, CA: SAGE Publications; 2012. [Google Scholar]
- 21.Taylor SJ, Bogdan R. Introduction to Qualitative Research Methods: A Guidebook and Resource. Hoboken, NJ: Wiley; 1998. [Google Scholar]
- 22.Miles MB, Huberman AM, Saldana J. Qualitative Data Analysis: A Methods Sourcebook Third Edition. Thousand Oaks, CA: SAGE Publications; 2013. Apr 5, [Google Scholar]
- 23.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000 Feb;34(6):1273–302. https://europepmc.org/abstract/MED/10654830 . [PMC free article] [PubMed] [Google Scholar]
- 24.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. doi: 10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- 25.Phillips KA, Morrison KR, Andersen R, Aday LA. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998 Aug;33(3 Pt 1):571–96. https://europepmc.org/abstract/MED/9685123 . [PMC free article] [PubMed] [Google Scholar]
- 26.Medi-Cal: specialty mental health services: foster children. LegiScan. 2016. Sep 25, [2022-03-07]. https://legiscan.com/CA/text/AB1299/id/1430838 .
- 27.AB 403 (stone): foster youth: continuum of care reform. CASA of Mendocino County. 2015. [2022-02-20]. http://mendocinocasa.org/wp-content/uploads/2015/01/AB403_FactSheet-Continuum-of-Care-CCR.pdf .
- 28.Facility types. California Department of Social Services. [2022-03-13]. https://www.cdss.ca.gov/inforesources/childrens-residential/resources-for-providers/facility-information .
- 29.California wraparound. California Department of Social Services. [2022-03-13]. https://www.cdss.ca.gov/inforesources/cdss-programs/foster-care/wraparound .
- 30.Stroul BA, Blau GM, Friedman RM. Updating the system of care concept and philosophy. Georgetown University Center for Child and Human Development, National Technical Assistance Center for Children’s Mental Health. 2010. [2022-09-18]. https://portal.ct.gov/-/media/DCF/Mental_Health/pdf/UpdatingTheSOCConcept2010pdf.pdf .
- 31.Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, Burroughs H, Jinks C. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907. doi: 10.1007/s11135-017-0574-8. https://europepmc.org/abstract/MED/29937585 .574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hennink M, Kaiser BN. Sample sizes for saturation in qualitative research: a systematic review of empirical tests. Soc Sci Med. 2022 Jan;292:114523. doi: 10.1016/j.socscimed.2021.114523. https://linkinghub.elsevier.com/retrieve/pii/S0277-9536(21)00855-8 .S0277-9536(21)00855-8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data set generated during this study is not publicly available due to ethical concerns about possible reidentification with this small study sample. Study metadata (eg, focus group guide and codebook) are available from the corresponding author on request.


