Abstract
Background
Malnutrition causes nutrient deficiencies that have both physical and clinical consequences in severe acute malnutrition children. Globally, there were 47 million wasted children under the age of five in 2019. One in four were located in sub-Saharan Africa, with half being in South Asia. This study aims to apply the Boruta algorithm to identify the determinants of undernutrition among children under five living in Dera Ghazi Khan, one of the marginalized districts of densely populated Punjab Province in Pakistan.
Methods
A multicenter cross-sectional study design was used to collect data from 185 children with severe acute malnutrition aged under five years visiting the OTPs centers located in Dera Ghazi Khan, Punjab, Pakistan. A purposive sampling technique was used to collect data using a pretested structured questionnaire from parents/caregivers regarding family sociodemographic characteristics, child nutrition, and biological and healthcare characteristics. Anthropometric measurements, including height, weight, and mid-upper arm circumference, were collected. The Boruta models were used to incorporate the children’s anthropometric, nutritional, and household factors to determine the important predictive variables for undernutrition using the Boruta package in R studio.
Results
This study included 185 children, with a mean age of 15.36 ± 10.23 months and an MUAC of 10.19 ± 0.96 cm. The Boruta analysis identifies age, mid-upper arm circumference, weaning practices, and immunization status as important predictors of undernutrition. Income per month, exclusive breastfeeding, and immunization status were found to be key factors of undernutrition in children under the age of five.
Conclusion
This study highlights age, mid-upper arm circumference, weaning practices, and immunization status as key determinants of weight-for-height and weight-for-age in children under five years. It also suggests that economic context may influence undernutrition. The findings can guide targeted strategies for combating undernutrition.
Keywords: Malnutrition, Undernutrition, Stunting, Wasting
Introduction
Malnutrition causes nutrient deficiencies that have both physical and clinical consequences in severe acute malnutrition children. Stunting is a form of undernutrition that is characterized by a child’s height for age Z score (SD ≤ 2) [1]. Wasting is characterized by low weight for height and poses a greater risk than stunting [2]. Wasting and stunting are often described as “acute” and “chronic” undernutrition, respectively. Underweight is characterized as a low weight-for-age. Underweight children might be stunted, wasted, or both [3]. Globally, there were 47 million wasted children under the age of five in 2019. One in four were located in sub-Saharan Africa, with half being in South Asia. South Asia had almost two out of every five stunted children [4].
Malnutrition still affects young children under the age of five in developing countries such as Pakistan. In Pakistan, 12 million children are stunted, with a national average of 40.2%. Stunting rates in Pakistan remain globally critical, with a slow reduction rate. Wasting among young children is increasing and had a prevalence of 17.7% in 2017, leading to a nutrition emergency in Pakistan [5]. Malnutrition is a major cause of intergenerational starvation, destroying the future productivity of nations and raising the economic burden [6]. Studies conducted in low-income countries have shown that male children are more likely to be stunted than their female counterparts, with a high prevalence in sub-Saharan Africa. Some studies conducted in Asia have documented that female children are more vulnerable [7, 8].
Malnutrition is caused by several interrelated variables and has both acute and chronic negative health effects [9]. The key factors contributing to child undernutrition are political unpredictability, poverty, and a lack of education that leads to inadequate dietary intake. The most typical causes of undernutrition in children are conditions such as diarrhea and inflammatory bowel syndrome, which have an impact on children’s development and growth [10, 11]. Child malnutrition can be influenced by several variables, such as fetal growth retardation, a lack of exclusive breastfeeding, incorrect complementary feeding, recurrent illnesses, food scarcity, and vitamin deficiencies [10, 12].
Malnutrition is the main cause of morbidity and mortality in children under five, and Pakistan ranks 22nd in the world for underfive child mortality [13]. Pakistan has recently faced natural disasters such as floods, famine/drought, and earthquakes [14]. A study of 656 households in the flood-affected areas of Pakistan found that 40.5% of children suffer from stunting, with factors such as age, maternal age, family type, water quality, and toilet facilities [15]. Similarly, a study in Khyber Pakhtunkhwa, Pakistan, revealed that 46% of children suffer from MUAC-based malnutrition, highlighting the need for targeted community-based nutrition awareness programs [16]. The most concerning effect of these catastrophes is the rise in childhood malnutrition. Previous studies have focused on explaining poverty and low socioeconomic status as the main cause of malnutrition in Pakistan.
The present study used the Boruta algorithm, a novel approach to studying malnutrition determinants, to fill a gap in the literature by focusing on southern Punjab, Pakistan. The algorithm’s ability to handle high-dimensional data and its ability to identify key determinants could guide more effective policies. This study is critical for comprehending the current situation with undernutrition among children under 5 years. The integration of diverse data sources, such as socioeconomic, health, and environmental data, could provide a more holistic understanding of malnutrition and undernutrition in particular. The possible contributions of the study to policy might highlight its importance.
Malnutrition can be caused by a variety of variables and requires creating an effective response strategy. The policy environment significantly influences the implementation and efficacy of nutrition interventions. Understanding the malnutrition framework is crucial for policy formulation and strategic actions, but its translation depends on a strong local understanding of subcomponents and their interactions. Previous research has typically used only univariate methods to identify the determinants of malnutrition [17, 18]. Recent research has employed the Boruta relevant feature selection wrapper algorithm to identify the key predictive determinants for undernutrition [19]. The Boruta algorithm compares the original attributes’ importance with random, permuted copies and eliminates irrelevant features [20].
Undernutrition in children under five requires a comprehensive public health approach, addressing factors such as illiteracy, poverty, and poor living standards through policies and awareness. Undernutrition treatments still cause significant morbidity and mortality, necessitating effective interventions to prevent millions of child deaths annually and contribute to sustainable development goals. This study aims to apply the Boruta algorithm to identify the important predictors of undernutrition among children under five living in Dera Ghazi Khan, which is one of the marginalized districts of the densely populated Punjab province in Pakistan.
Materials and methods
Study design and setting
A multicenter cross-sectional study was carried out for data collection during March 2021 to June 2022. The “National Program for Family Planning and Primary Health Care” operated four functional outpatient therapeutic program centers (OTPs) at basic health units (BHUs), including Samina, Jhokutra, and Aaliwala, and one OTP at a rural health center (RHC), Kotchutta, of Dera Ghazi Khan, Punjab, Pakistan, for the collection of children with severe acute malnutrition. These four centers were selected because they were more active than the others, with an appropriate number of workers, patients, and therapeutic food. Participants in the study were selected from these government-designated centers for the treatment of malnutrition. These chosen areas of Dera Ghazi Khan District are underdeveloped, with poor socioeconomic situations, poverty, insecure housing tenure, overpopulation, and unclean living conditions.
Study population
A purposive sampling technique was used to recruit children aged 6–59 months living in district Dera Ghazi Khan diagnosed with “severe acute malnutrition” without chronic comorbidities. A mid-upper arm circumference (MUAC) of ≤ 11.5 cm, a weight for height Z score of -3, or bilateral edema of grades 1–2 were used as the World Health Organization-suggested inclusion criteria for severe acute malnutrition [21]. All of the children had good general health, and they shared the same racial and language background. Parents/caregivers were informed of the study’s purpose and provided with a written consent form to participate in the study. Children with severe malnutrition-related problems such as severe hypoglycemia, severe anemia, severe pitting edema, anorexia, hypothermia, or high pyrexia were excluded.
Sample size
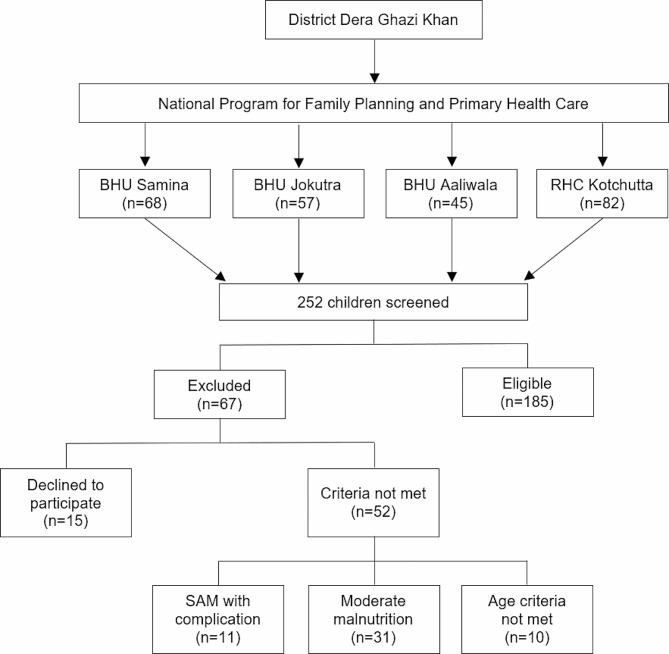
The cross-sectional study formula was used to determine the sample size, with the error term (d) set at 0.05 and the prevalence of severe malnutrition (p) at 11%. A sample size of 151 was calculated using the following formula (Eq. 1), and this number was raised to 185 to increase study precision, strength, and accuracy. A total of 252 children were screened for participation in this study, with 67 being excluded due to not satisfying the inclusion criteria (Fig. 1).
Fig. 1.
Flowchart of sample selection
 |
1 |
Data collection
Parents were interviewed at OTP centers using a structured questionnaire that had been pretested to gather information about family sociodemographics (income, parental education, occupation, household size, and family structure), infant and young child feeding (IYCF), anthropometric measurements (height, weight, and MUAC) and healthcare characteristics (child medical history, immunization record, and access to healthcare). Income from all sources in Pakistani rupees (PKR) was used to estimate the monthly income of the family.
In accordance with WHO recommendations, complementary feeding practices (amount, variety, and frequency) and exclusive breastfeeding were evaluated [22]. The vaccination record served as evidence that the Expanded Program of Immunization (EPI) schedule for child immunization had been followed [23]. The child’s medical history was assessed to identify wasting, stunting, and underweight. Parents/caregivers provided a history to identify seizure disorders and neurological deficits in children; sick children were excluded.
For children who had hospital deliveries, the gestational age was derived from the antenatal record; in cases of home deliveries, it was based on the mother’s narrative. The number of lost gestational weeks was deducted from the present age to account for premature birth in children up to 24 months of age (37 weeks gestation).
Nutritional supervisors conducted anthropometric measurements, recording double anthropometric values if they differed from one another. Children’s weight was assessed without clothing or in light outfits using SECA 336 baby scales, while children 2 years or older were weighted using SECA 874 Electronic Scale. Infant/child weights were calculated as the difference between these two measures and were close to 10 g.
A length-measuring board with a fixed headrest and an adjustable foot piece (SECA GmbH & Co. KG, Hamburg, Germany) was used to measure the recumbent length of children under 87 cm in height to the nearest 0.1 cm. Children who were taller than 87 cm were measured by having them stand with their heels touching a flat horizontal plate attached to the measurement board. The WHO Child Growth Standards were used to generate the weight-for-height Z scores and the height-for-age Z scores [1]. WHO ANTHRO, version 3.2.2, was used to classify the nutritional status of the children.
Data analysis
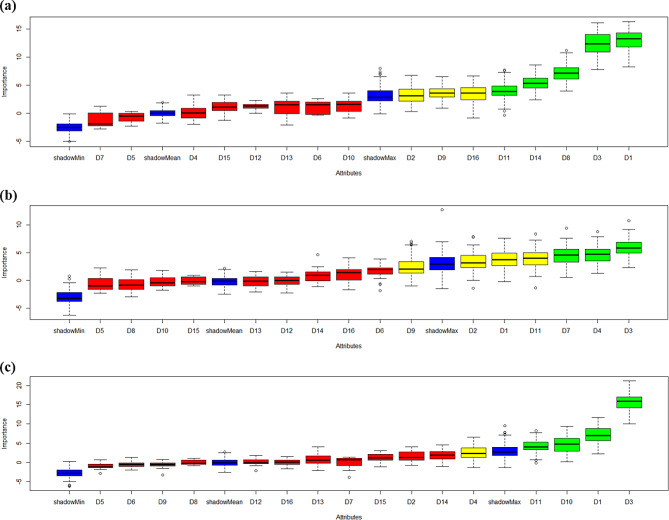
The demographic and household characteristics are presented as categorical variables to show the frequency distribution by using IBM SPSS 25.0. In addition, for statistical analyses, we used the Boruta package, which is available from the comprehensive R archive network at https://cran.r-project.org/web/packages/Boruta/index.html. The determinants were identified using the Boruta feature selection, and the variables’ importance scores were calculated for weight-for-height, weight-for-age, and undernutrition. Undernutrition data generated from the Boruta outcome are presented in the graphs. Blue boxplots represent a shadow attribute’s minimum, average, and maximum Z scores for the undernutrition determinants. Z scores of qualities that were rejected are presented in red and confirmed are presented in green boxplots. The attStats function also generates a data frame with Z score statistics for each attribute.
Ethics approval
The provincial and district health departments of Punjab, Pakistan, gave their approval for the study to be conducted. The University of Punjab in Pakistan’s Ethical Review and Advanced Study Research Board (ref-9/2352-ACAD) gave its approval to all procedures involving human subjects during this study, which was carried out following the Declaration of Helsinki’s principles [24]. All subjects provided written consent to participate in the study.
Results
This study included 185 children, with a mean age of 15.36 ± 10.23 months, who had a MUAC of 10.19 ± 0.96 cm. In terms of gender, the study included 81 male participants (43.8%) and 104 female participants (56.2%). When considering monthly income, the majority of participants (69.2%) had an income of ≤ 15,000 PKR, while 30.8% had an income ranging from 15,000 to 35,000 PKR. Among the study participants, 22.7% reported a history of a parasite, whereas the majority (77.3%) had no such history. In terms of TB, 43.8% of the participants had a history of TB. Additionally, 15.1% of the participants reported a history of measles. The participants experienced varying numbers of illness episodes, with 54.1% reporting 1–7 episodes and 45.9% having 8–15 episodes. Only 19.5% of the mothers exclusively breastfed their infants, whereas the majority (80.5%) did not. In addition, 89.2% of the subjects had inadequate complementary feeding practices, as shown in Table 1.
Table 1.
Characteristics of the study participants
| Determinant code | Variable | Category | n (%) |
|---|---|---|---|
| D1 |
Age (15.36 ± 10.23 Months) |
≤ 12 months | 112 (60.5) |
| 13–24 Months | 45 (24.3) | ||
| ≥ 25 Months | 28 (15.1) | ||
| D2 | Gender | Male | 81 (43.8) |
| Female | 104 (56.2) | ||
| D3 | Mid Upper Arm Circumference (MUAC) (10.19 ± 0.95 cm) | ≤ 10 cm | 99 (53.5) |
| ≥ 10.1 cm | 86 (46.5) | ||
| D4 | Income per month | ≤ 15,000 PKR | 128 (69.2) |
| 15,000–35,000 PKR | 57 (30.8) | ||
| D5 | History of parasite | Yes | 42 (22.7) |
| No | 143 (77.3) | ||
| D6 | History of measles | Yes | 28 (15.1) |
| No | 157 (84.9) | ||
| D7 | History of scabies | Yes | 28 (15.1) |
| No | 157 (84.9) | ||
| D8 | History of TB | Yes | 81 (43.8) |
| No | 104 (56.2) | ||
| D9 | Exclusive breastfeeding | Yes | 36 (19.5) |
| No | 149 (80.5) | ||
| D10 | Weaning practices | Adequate | 45 (24.3) |
| Nonadequate | 140 (75.7) | ||
| D11 | Immunization | Incomplete | 46 (24.9) |
| Complete | 139 (75.1) | ||
| D12 | Father’s education | Primary & above | 73 (39.5) |
| No education | 112 (60.5) | ||
| D13 | Mother’s education | Primary & above | 52 (28.1) |
| No education | 133 (71.9) | ||
| D14 | Hygiene | Good | 20 (10.8) |
| Poor | 165 (89.2) | ||
| D15 | Underfive siblings | ≤ 2 | 144 (77.8) |
| ≥ 3 | 41 (22.2) | ||
| D16 | Household size | 1–10 | 23 (12.4) |
| ≥ 10 | 162 (87.6) |
The Boruta analysis was conducted to identify the determinants that have significant importance in predicting weight-for-height among children under five years. The analysis revealed several key findings and suggested that age (D1) emerged as the most important determinant, consistently demonstrating high importance scores across multiple iterations. Mid-upper arm circumference (D3) also exhibited significant importance and was consistently identified as important in all iterations. Additionally, weaning practices (D10) and the immunization status of the children (D11) were found to be important determinants, as shown in Fig. 1a; Table 2.
Table 2.
Determinants importance scores from Boruta algorithm for weight-for-height
| Determinants | Meanimp | Medianimp | Minimp | Maximp | Normhits | Decision |
|---|---|---|---|---|---|---|
| Age | 7.11 | 7.02 | 2.20 | 11.61 | 0.93 | Confirmed |
| Gender | 1.56 | 1.28 | -0.71 | 4.08 | 0.03 | Rejected |
| MUAC | 15.69 | 15.88 | 9.99 | 21.18 | 1.00 | Confirmed |
| Income per month | 2.56 | 2.37 | -1.31 | 6.62 | 0.43 | Tentative |
| History of Parasites | -0.97 | -1.08 | -2.83 | 0.66 | 0.00 | Rejected |
| History of Measles | -0.45 | -0.48 | -1.93 | 1.27 | 0.00 | Rejected |
| History of Scabies | -0.11 | 0.68 | -3.82 | 1.46 | 0.00 | Rejected |
| History of TB | 0.00 | -0.22 | -0.80 | 1.15 | 0.00 | Rejected |
| Exclusive feeding | -0.63 | -0.48 | -3.22 | 0.78 | 0.00 | Rejected |
| Weaning practices | 4.70 | 4.74 | 0.20 | 9.41 | 0.73 | Confirmed |
| Immunization | 4.16 | 4.08 | -0.09 | 8.22 | 0.70 | Confirmed |
| Father Education | 0.11 | -0.02 | -2.12 | 1.82 | 0.00 | Rejected |
| Mother Education | 0.72 | 0.65 | -2.17 | 4.04 | 0.02 | Rejected |
| Hygiene | 1.93 | 1.95 | -1.05 | 4.52 | 0.07 | Rejected |
| Under5-siblings | 1.22 | 1.17 | -1.16 | 3.06 | 0.00 | Rejected |
| Household size | 0.00 | 0.05 | -1.61 | 1.52 | 0.00 | Rejected |
However, income per month (D4) displayed a moderate importance score and was labelled tentative, requiring further investigation for confirmation. On the other hand, determinants such as gender (D2), history of a parasite (D5), history of measles (D6), history of scabies (D7), history of TB (D8), exclusive breastfeeding (D9), father’s education (D12), mother’s education (D13), hygiene (D14), under five siblings (D15), and household size (D16) were rejected as unimportant, as shown in Fig. 2a; Table 2. These findings provide valuable insights into the factors influencing weight-for-height and can inform future research and modelling efforts in this domain.
Fig. 2.
a-c: Variable importance scores from the Boruta algorithm for (a) weight-for-height, (b) weight-for-age, and (c) underweight. Blue boxplots represent a shadow attribute’s minimum, average, and maximum Z scores. Z scores of qualities that were rejected and confirmed, respectively, are represented by red and green boxplots
The study also aimed to determine the important determinants for predicting weight-for-age using the Boruta algorithm. Determinants MUUAC and income per month emerged as confirmed determinants, consistently demonstrating significant importance in multiple iterations. A history of scabies also showed consistent importance and was confirmed as a significant determinant. On the other hand, age, sex, exclusive feeding and immunization displayed moderate importance and were labelled tentative, indicating the need for further investigation. The study found that factors such as history of parasites (D5), measles (D6), tuberculosis (D8), weaning practices (D10), parents’ education (D12, D13), hygiene (D14), under5-siblings (D15), and household size (D16) were not significant in predicting weight-for-age, as shown in Fig. 2b; Table 3. The Boruta analysis identified age, income per month, exclusive feeding, and immunization as significant determinants for predicting underweight, with gender and history of tuberculosis as tentative determinants. Rejected determinants had little influence, as shown in Fig. 2c; Table 4.
Table 3.
Determinants importance scores from the Boruta algorithm for weight-for-age
| Determinants | Meanimp | Medianimp | Minimp | Maximp | Normhits | Decision |
|---|---|---|---|---|---|---|
| Age | 3.85 | 3.75 | -0.21 | 7.64 | 0.61 | Tentative |
| Gender | 3.44 | 3.19 | -1.40 | 7.87 | 0.58 | Tentative |
| MUAC | 5.97 | 5.88 | 2.33 | 10.78 | 0.92 | Confirmed |
| Income per month | 4.68 | 4.74 | 1.24 | 8.82 | 0.77 | Confirmed |
| History of Parasites | -0.58 | -1.02 | -2.30 | 2.26 | 0.01 | Rejected |
| History of Measles | 1.58 | 1.97 | -1.85 | 3.84 | 0.02 | Rejected |
| History of Scabies | 4.47 | 4.55 | 0.55 | 9.44 | 0.71 | Confirmed |
| History of TB | -0.65 | -0.85 | -2.94 | 1.92 | 0.00 | Rejected |
| Exclusive feeding | 2.35 | 2.03 | -0.97 | 7.01 | 0.41 | Tentative |
| Weaning practices | -0.23 | -0.40 | -1.77 | 1.86 | 0.00 | Rejected |
| Immunization | 3.89 | 4.03 | -1.35 | 8.38 | 0.63 | Tentative |
| Father Education | -0.14 | 0.02 | -2.26 | 1.45 | 0.00 | Rejected |
| Mother Education | -0.27 | -0.13 | -2.12 | 1.61 | 0.00 | Rejected |
| Hygiene | 0.92 | 0.90 | -1.13 | 4.66 | 0.02 | Rejected |
| Under5-siblings | -0.04 | -0.18 | -1.02 | 0.95 | 0.00 | Rejected |
| Household size | 1.19 | 1.41 | -1.70 | 4.07 | 0.03 | Rejected |
Table 4.
Determinants importance scores from the Boruta algorithm for underweight
| Determinants | Meanimp | Medianimp | Minimp | Maximp | Normhits | Decision |
|---|---|---|---|---|---|---|
| Age | 4.60 | 4.57 | 1.56 | 8.90 | 0.72 | Confirmed |
| Gender | 3.23 | 3.01 | -0.45 | 9.43 | 0.46 | Tentative |
| MUAC | 0.09 | 0.36 | -1.44 | 2.33 | 0.00 | Rejected |
| Income per month | 5.02 | 4.97 | -0.19 | 11.35 | 0.75 | Confirmed |
| History of Parasites | -0.31 | -0.08 | -3.27 | 1.85 | 0.02 | Rejected |
| History of Measles | 0.78 | 0.67 | -1.78 | 3.19 | 0.03 | Rejected |
| History of Scabies | 2.03 | 1.89 | -2.33 | 5.52 | 0.14 | Rejected |
| History of TB | 3.45 | 3.54 | 0.20 | 7.13 | 0.54 | Tentative |
| Exclusive feeding | 5.63 | 5.70 | 0.91 | 12.00 | 0.83 | Confirmed |
| Weaning practices | -0.38 | -0.73 | -2.44 | 3.26 | 0.01 | Rejected |
| Immunization | 4.82 | 5.14 | -0.26 | 9.49 | 0.73 | Confirmed |
| Father Education | 3.85 | 3.66 | 0.26 | 8.24 | 0.65 | Tentative |
| Mother Education | 1.30 | 1.07 | -1.03 | 4.18 | 0.04 | Rejected |
| Hygiene | 0.42 | 0.31 | -1.27 | 2.23 | 0.00 | Rejected |
| Under5-siblings | 0.58 | 0.31 | -1.32 | 2.40 | 0.02 | Rejected |
| Household size | 2.00 | 2.22 | -1.22 | 5.00 | 0.19 | Rejected |
Discussion
The present study aimed to identify the important determinants for predicting weight-for-height, weight-for-age, and underweight using the Boruta algorithm. The findings from the Boruta analysis provided valuable insights into the factors influencing these anthropometric measurements. The Boruta algorithm was chosen for this analysis due to its robustness in handling multiple features, capturing nonlinear pattern relationships, and providing more robust discriminant power than classical statistics. For weight-for-height, the Boruta analysis identified age, MUAC, weaning practices, and immunization as confirmed determinants. Age, with the highest importance score, consistently demonstrated its significance across multiple iterations. For weight-for-age, the Boruta analysis revealed MUAC, income per month, and history of scabies as confirmed determinants. MUAC and income per month consistently displayed significant importance scores, highlighting their influence on weight-for-age prediction. In the case of undernutrition, the Boruta analysis confirmed age, income per month, exclusive feeding, and immunization as important determinants. Age, income per month, and immunization consistently demonstrated significant importance, suggesting their strong association with underweight.
Children of poor families with a monthly income less than 15,000 PKR were more prone to wasting than those with a relatively higher monthly income (15,000–35,000 PKR). This result is consistent with previous research that highlights a strong relationship between poverty and malnutrition [25]. Monthly family income can impact food intake, malnutrition, and limited resources for low-income families [26]. Financial limitations often make it difficult for people to obtain nutritious food, medical care, and a healthy standard of living, which affects the nutrition of children [27].
Undernutrition has been strongly associated with complementary feeding practices. A higher rate of undernutrition was observed in children who received inadequate complementary feeding. This finding is in alignment with other research emphasizing the need for adequate and timely introduction of complementary foods in promoting optimal growth and development [28]. Inappropriate complementary feeding and weaning practices lead to chronic malnutrition in children.
Improving infant and young child feeding practices is crucial for improving nutrition, health, and development in children aged 0–22 months, ultimately impacting child survival [29]. The WHO’s guidelines recommend complementary feeding for infants and young children aged 6–22 months in low-, middle-, and high-income countries [30]. Breast milk or infant formula alone is insufficient to meet the infant’s energy needs or offer enough amounts of specific nutrients such as protein, zinc, iron, and fat-soluble vitamins from that age [31]. The WHO Global Strategy for Infant and Young Child Feeding recommends introducing solid, semisolid, and soft foods at six months of age, while continuing breastfeeding, to prevent malnutrition [32].
Children who have a balanced diet or enough food have a positive tendency towards healthy development and growth. Malnutrition results from inappropriate weaning procedures and can significantly impair nutritional status [4]. Breastfeeding for the first 24 months of a child’s life, together with complementary feeding, ensures that they receive a sufficient amount of nutrients and a balanced diet, both of which are essential to the child’s growth and the prevention of malnutrition [22]. Mother’s milk alone cannot meet the nutritional requirements of growing children, so breastfeeding should start at birth and continue until the child’s second birthday in combination with complementary feeding to prevent acute and chronic malnutrition [22, 33, 34]. Due to the lack of vital nutrients needed for children’s healthy growth and development, continuing to breastfeed without complementary feeding after six months of age may increase the risk of malnutrition [22].
Malnutrition, both acute and chronic, can result from inappropriate and nonexclusive breastfeeding. According to research conducted in Pakistan, 45.8% of mothers started breastfeeding their children as soon as they were born, and 48.4% of infants were exclusively breastfed [5]. Because the mother’s milk contains an appropriate proportion of the nutrients the infant needs, exclusive nursing should begin within the first hour of delivery [22, 35]. Malnutrition in children caused by infectious diseases could also affect their growth and development [36, 37]. Inflammation increased the likelihood of stunting and malnutrition in children with a history of TB [36].
Compared to children with one or two siblings, children with three or more siblings are more likely to be stunted. Increased family size may affect food availability, resulting in underweight or stunted children [4, 33, 34]. Acute or chronic malnutrition is more likely to develop in children with birth intervals of less than two years [33]. The resources needed to appropriately feed every child become more scarce as the number of children under five in a family increases [4, 37, 38].
The healthy growth and development of newborns and young children are significantly influenced by the education of mothers. The majority of the mothers in the present study were uneducated, and the children they raised had higher nutrient deficiencies. Stunting and wasting may be avoided by an educated mother, as she will be more aware of her child’s nutritional requirements [35].
The cross-sectional design of this study has certain drawbacks. The study’s small sample size and limited coverage in one district limit its potential for strong results, suggesting the need for longitudinal research across multiple districts. Anthropometric measurements were carried out by qualified individuals, which supports the integrity of the data. A deeper understanding of the dynamic nature of a child’s growth and development could be achieved by carefully examining children’s nutritional status.
Conclusion
The study reveals that age and mid-upper arm circumference are key determinants of weight-for-height and weight-for-age in children under five years, emphasizing the need for interventions targeting specific age groups and practical measures to assess nutritional status. Weaning practices and immunization status are crucial determinants of child development, emphasizing the need for comprehensive health and nutrition programs. Income per month’s importance varies, suggesting that economic context may influence child undernutrition and requires further investigation.
The Boruta analysis revealed that factors such as gender, parasite history, and exclusive breastfeeding are less influential in predicting undernutrition in children. These findings can guide policymakers, healthcare professionals, and researchers in developing targeted strategies to combat undernutrition in children.
Acknowledgements
Not applicable.
Abbreviations
- CI
Confidence interval
- CMAM
Community Management of Acute Malnutrition
- EPI
Expanded Program of Immunization
- PKR
Pakistani rupee
- SD
Standard deviation
- TB
Tuberculosis
- WHO
World Health Organization
Author contributions
Conceptualization: J.S., R.Z. and MI; Data curation: Z.A. and MSB; Formal analysis: Z.A, and MSB; Writing– original draft: J.S and MSB; Writing– reviewing & editing: R.Z., R.M.A., M.S.B., Z.A., G.M.J.B., MI and F.F.; supervision: R.Z. G.M. J.B. and F.F. All authors read and approved the final version of the manuscript.
Funding
This research received no supporting funds from any funding agency in the public, commercial, or not-for-profit sector.
Data availability
Data are available from the corresponding author upon reasonable request.
Declarations
Ethical approval and consent to participate
The provincial and district health departments of Punjab, Pakistan, gave their approval for the study to be conducted. The study was conducted after the approval of the Ethical Review and Advanced Study Research Board of the University of Punjab, Pakistan (ref-9/2352-ACAD). It followed the Declaration of Helsinki’s principles. Written informed consent was obtained from the parents of the participants after introducing them to the purpose of the study.
Consent for publication
Not applicable.
Competing interests
RZ and FF are Associate Editors at BMC Public Health. All the other authors declare no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO child growth standards and the identification of severe acute malnutrition in infants and children: a joint statement by the World Health Organization and the United Nations children’s fund. Geneva: World Health Organization; 2009. Available from: http://www.ncbi.nlm.nih.gov/books/NBK200775/ [PubMed]
- 2.Briend A, Khara T, Dolan C. Wasting and stunting-similarities and differences: policy and programmatic implications. Food Nutr Bull. 2015;36:15–23. doi: 10.1177/15648265150361S103. [DOI] [PubMed] [Google Scholar]
- 3.Richard SA, Black RE, Gilman RH, Guerrant RL, Kang G, Lanata CF, et al. Wasting is associated with stunting in early childhood. J Nutr. 2012;142(7):1291–6. doi: 10.3945/jn.111.154922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levels and trends in child malnutrition: UNICEF/WHO/The world bank group joint child malnutrition estimates. Key findings of the 2021 edition. Available from: https://www.who.int/publications-detail-redirect/9789240025257
- 5.Key findings of National Nutrition Survey Pakistan. 2018. UNICEF; 2019; Available from: https://www.unicef.org/pakistan/media/1951/file/Final
- 6.Jesmin A, Yamamoto SS, Azam Malik A, Haque MA. Prevalence and determinants of chronic malnutrition among Preschool children: a cross-sectional study in Dhaka City, Bangladesh. J Health Popul Nutr. 2011;29(5):494–9. doi: 10.3329/jhpn.v29i5.8903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Espo M, Kulmala T, Maleta K, Cullinan T, Salin ML, Ashorn P. Determinants of linear growth and predictors of severe stunting during infancy in rural Malawi. Acta Paediatr. 2002;91(12):1364–70. doi: 10.1111/j.1651-2227.2002.tb02835.x. [DOI] [PubMed] [Google Scholar]
- 8.Khatun M, Stenlund H, Hörnell A. BRAC initiative towards promoting gender and social equity in health: a longitudinal study of child growth in MATLAB, Bangladesh. Public Health Nutr. 2004;7(8):1071–9. doi: 10.1079/PHN2004652. [DOI] [PubMed] [Google Scholar]
- 9.Khan S, Zaheer S, Safdar NF. Determinants of stunting, underweight and wasting among children < 5 years of age: evidence from 2012–2013 Pakistan demographic and Health Survey. BMC Public Health. 2019;19:358. doi: 10.1186/s12889-019-6688-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Egata G, Berhane Y, Worku A. Predictors of acute undernutrition among children aged 6 to 36 months in east rural Ethiopia: a community based nested case– control study. BMC Pediatr. 2014;14:91. doi: 10.1186/1471-2431-14-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Talbert A, Thuo N, Karisa J, Chesaro C, Ohuma E, Ignas J, et al. Diarrhoea complicating severe acute malnutrition in Kenyan children: a prospective descriptive study of risk factors and outcome. PLoS ONE. 2012;7(6):e38321. doi: 10.1371/journal.pone.0038321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ogunlesi T, Ayeni V, Adekanmbi A, Fetuga B. Determinants of timely initiation of complementary feeding among children aged 6–24 months in Sagamu, Nigeria. Niger J Clin Pract. 2014;17(6):785. doi: 10.4103/1119-3077.144399. [DOI] [PubMed] [Google Scholar]
- 13.UNICEF. The state of the world’s children. 2015: Reimagine the future. Innovation for every child. UNICEF; 2014. Available from: https://www.unicef.org.uk/wp-content/uploads/2014/11/state-of-the-worlds-children-2014.pdf
- 14.Hussain A, Chaudhary MN, Jafri SZH, Malik S, Ali N. Awan D-e-S. Climate Change and its impacts on Pakistan. J Posit School Psychol. 2022;6(8):9195–217. [Google Scholar]
- 15.Haq IU, Mehmood Z, Afzal T, Khan N, Ahmed B, Nawsherwan, et al. Prevalence and determinants of stunting among preschool and school-going children in the flood-affected areas of Pakistan. Braz J Biol. 2022;82:e249971. doi: 10.1590/1519-6984.249971. [DOI] [PubMed] [Google Scholar]
- 16.Haq IU, Mehmood Z, Khan N, Khan MN, Israr M, Ali Khan E, et al. Risk factors of mid-upper arm circumference (MUAC) based child malnutrition in the Flood-affected areas of Pakistan: a cross-sectional study: child malnutrition in flood-hit areas. Ecol Food Nutr. 2021;60(4):491–507. doi: 10.1080/03670244.2021.1872024. [DOI] [PubMed] [Google Scholar]
- 17.Ma ZF, Wang CW, Lee YY, Editorial Malnutrition: a cause or a consequence of poverty? Front Public Health. 2022;9:796435. doi: 10.3389/fpubh.2021.796435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siddiqui F, Salam RA, Lassi ZS, Das JK. The intertwined relationship between malnutrition and poverty. Front Public Health. 2020;8:453. doi: 10.3389/fpubh.2020.00453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sisimayi C, Mupandawana M, Mutambwa M, Sisimayi T, Njovo H. An application of machine learning and advanced econometrics techniques on population survey datasets in Zimbabwe.
- 20.Kursa MB, Rudncki WR. Feature selection with the Boruta Package. J Stat Softw. 2010;36(11):1–13. doi: 10.18637/jss.v036.i11. [DOI] [Google Scholar]
- 21.Williams PCM, Berkley JA. Guidelines for the treatment of severe acute malnutrition: a systematic review of the evidence for antimicrobial therapy. Paediatr Int Child Health. 2018;38(Suppl 1):21. doi: 10.1080/20469047.2017.1409453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Infant and young child feeding. WHO; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding
- 23.Expanded Programme on Immunization. World Health Organization - Regional office for the Eastern Mediterranean; 2023. Available from: http://www.emro.who.int/pak/programmes/expanded-programme-on-immunization.html
- 24.World Medical Associaton World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 25.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet. 2013;382(9890):427–51. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 26.Nott J. Malnutrition in a modernizing economy: the changing aetiology and epidemiology of Malnutrition in an African Kingdom, Buganda c.1940–73. Med Hist. 2016;60(2):229–49. doi: 10.1017/mdh.2016.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ruel MT, Alderman H. Nutrition-sensitive interventions and programmes: how can they help to accelerate progress in improving maternal and child nutrition? The Lancet. 2013;382(9891):536–51. doi: 10.1016/S0140-6736(13)60843-0. [DOI] [PubMed] [Google Scholar]
- 28.Dewey KG, Adu-Afarwuah S. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Matern Child Nutr. 2008;4(Suppl 1):24–85. doi: 10.1111/j.1740-8709.2007.00124.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.UNICEF. Indicators for assessing infant and young child feeding practices: definitions and measurement methods. Geneva: World Health Organization and the United Nations Children’s Fund; 2021.
- 30.WHO Guideline for complementary feeding of infants and young children 6–23 months of age. Geneva: World Health Organization; 2023. Available from: http://www.ncbi.nlm.nih.gov/books/NBK596427/ [PubMed]
- 31.Dewey KG. Nutrition, Growth, and complementary feeding of the Brestfed infant. Pediatr Clin North Am. 2001;48(1):87–104. doi: 10.1016/S0031-3955(05)70287-X. [DOI] [PubMed] [Google Scholar]
- 32.WHO/UNICEF. Global strategy for infant and young child feeding. Available from: https://www.who.int/publications-detail-redirect/9241562218
- 33.Kahssay M, Woldu E, Gebre A, Reddy S. Determinants of stunting among children aged 6 to 59 months in pastoral community, Afar region, North East Ethiopia: unmatched case control study. BMC Nutr. 2020;6:9. doi: 10.1186/s40795-020-00332-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eunice MJ, Cheah WL, Lee PY. Factors influencing malnutrition among Young Children in a Rural Community of Sarawak. Mal J Nutr. 2014;20(2):145–64. [Google Scholar]
- 35.Nambuusi BB, Ssempiira J, Makumbi FE, Kasasa S, Vounatsou P. The effects and contribution of childhood diseases on the geographical distribution of all-cause underfive mortality in Uganda. Parasite Epidemiol Control. 2019;5:e00089. doi: 10.1016/j.parepi.2019.e00089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wagstaff A, Bustreo F, Bryce J, Claeson M, WO–World Bank Child Health and Poverty Working Group. Child health: reaching the poor. Am J Public Health. 2004;94(5):726–36. [DOI] [PMC free article] [PubMed]
- 37.Chattopadhyay N, Saumitra M. Developmental outcome in children with malnutrition. J Nepal Paediatr Soc. 2016;36(2):170–7. doi: 10.3126/jnps.v36i2.14619. [DOI] [Google Scholar]
- 38.Gupta N, Kabra M. Approach to the diagnosis of developmental delay– the changing scenario. Indian J Med Res. 2014;139(1):4–6. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the corresponding author upon reasonable request.