Abstract
This article highlights advances in basic science preclinical pain research, clinical research, and psychological research occurring over the 50 years since the International Association for the Study of Pain (IASP was founded. It presents important findings and key trends in these three areas of pain science: basic science, clinical research, and psychological research.
Introduction
Since its inception, the International Association for the Study of Pain (IASP) has aimed to foster high-quality pain research and management through a variety of approaches including its scientific publications (Pain, Pain Reports), books, guidelines, scientific meetings, and educational activities. This article highlights research and clinical advances occurring over the 50 years since IASP was founded. Given the need to be brief we are unable to provide a comprehensive overview of the field. We apologize, in advance, to investigators whose work we fail to mention, omissions that, in fact, illustrate how productive the field has been over the last 50 years. We discuss important findings and key trends in three areas of pain science: basic science preclinical pain research, clinical research, and psychological research. As outlined elsewhere in this special issue of the journal (20), many of these findings and trends have been significanly underpinned by several of the technological advances occurring over this period.
Highlights in Basic Science Preclinical Pain Research
The last 50 years has seen many preclinical discoveries of the mechanisms that contribute to acute and chronic pain. Highlights include characterization of peripheral and central sensitization processes (3,19, 53), transcriptomic analyses of primary sensory and dorsal horn neurons (50, 22) and non-neuronal cells (32) and the development of induced pluripotent stem cell (iPSC)-derived nociceptors (33). Many of these analyses are also expanding in human tissue (45). A particularly notable rodent highlight was discovery of the spinoparabrachial pathway (8) and its connections with forebrain regions that process pain affect.
The development of new animal models of inflammatory and neuropathic pain also provided important insights into chronic pain mechanisms (7). Although these models cannot replicate the clinical condition, they are critical surrogates for the study of novel therapies. Of note has been the development of more reliable, non reflex-based methods to assess ongoing pain in preclinical settings, including conditioned place preference and aversion tests (14) and the grimace scale (34). Technological highlights include powerful optogenetic (27) and Designer Receptors Exclusively Activated by Designer Drugs (DREADDS; 49) - based studies of pain generating and control circuits, as well the new ability to discover novel analgesics through in silico screening of millions of molecules against pain-relevant targets (5,17). Thanks to incredible advances in computer technology, single unit recording has been replaced by electrodes that monitor the activity of hundreds of neurons. Computational power has also greatly expanded the scope of genetic analyses and brain imaging.
It is of interest that neither the use of gabapentinoids nor serotonin-norepinephrine reuptake inhibitors (SNRIs) for neuropathic pain resulted from initial preclinical studies. Rather, their assessment in preclinical studies occurred after their introduction in patients, to manage seizures and depression, respectively. Ziconotide is an exception (36), but unfortunately, its clinical use is limited. However, three clinically translated highlights are especially noteworthy. First, the demonstration, initially in rats, that spinal morphine exerts a powerful analgesic action, with a therapeutic window much greater than after systemic administration (55). Second, recognition of the parallels that characterize the preclinical phenomenon of Diffuse Noxious Inhibitory Controls (DNIC) and the features of Conditioned Pain Modulation (CPM) in patients. These parallels have mechanistic implications in the etiology of fibromyalgia, irritable bowel syndrome, temporomandibular disorder and tension-type headache (41). And third, what is perhaps the most successful preclinical to clinical translation was the discovery of calcitonin gene-related peptide (CGRP), its expression in peptidergic nociceptors and its potency as a vasodilator. Those discoveries provided the rationale for targeting CGRP in migraine (39, 42) with monoclonal antibodies against CGRP or with CGRP receptor blockers. Brain stimulation for chronic pain is now less common but did follow preclinical demonstrations of powerful descending control systems (4). For all of these translational successes, credit should not only go to the collaborative research of scientists and clinicians, but also to the many volunteers who were participants in these studies.
The Nobel Prize awarded for the discovery of the Transient Receptor Potential Vanilloid 1 (TRPV1) and Piezo channels is unquestionably among the most memorable preclinical pain research highlights (35). And there remains a plethora of sensory neuron pain-relevant targets, including voltage-gated Na+, K+ and Ca++ channels (3). Lidocaine, despite its therapeutic window limitations, is still the most effective way to block pain. For this reason, the clinical failure to date of drugs that target and block NaV1.7, loss of function of which leads to pain insensitivity (16), is disappointing. Nevertheless, the search continues for drugs to regulate NaV1.7 and other pain-relevant Na channels (e.g., NaV1.8 and NaV1.9). The discovery of multiple opioid receptors (30) and endorphin subtypes (26) was also groundbreaking, but we still await translation of those findings to improved pain pharmacotherapy. Particularly disappointing is that we still lack a reliable laboratory or clinical biomarker for pain. Here is an important challenge for the new generation of basic and clinical pain researchers.
Highlights in Clinical Pain Research
A cure for chronic pain has not been found, however, a number of milestones in clinical pain research has been seen in the past 50 years. Perhaps the most remarkable one has been the mutual exchange of knowledge and ideas between basic and clinical pain scientists. In the 1970s and 1980s the pain field sparkled with optimism. Basic science studies showed that stimulating brainstem opioid-linked circuits activate descending control systems that target the dorsal horn via the dorsolateral funiculus and suppress nociceptive processing (1,4). Opioids when administered intraspinally produced powerful analgesia (55) without sedation or affecting cognitive function. This observation had an immediate clinical impact on the management of acute pre- and postoperative pain, and certain types of cancer pain (10). However, the enthusiasm for opioids for chronic pain faded substantially with the increasing documentation of side effects associated with opioids. For postoperative pain other multimodal pain strategies were introduced. These strategies not only improved pain management, but also recovery after surgery, so-called fast track surgery (29). In the 1990s many clinical pain trials were carried out with compounds, such as antidepressants and gabapentinoids developed for other conditions, but these showed meaningful clinical pain relief in mainly neuropathic types of pain (18,19).
Systematic reviews and meta-analysis became an important instrument for clinicians to understand what works and what does not work (37). Following a number of negative clinical pain trials, where treatment efficacy was based solely on disease and type of pain, a completely new emphasis emerged, namely a mechanism-based classification approach (54). The key tenet in this approach was that a focus on specific small molecules targeting a specific mechanism may produce the relevant necessary and sufficient pain relief. Noted above is the success of CGRP receptor blockers and monoclonal antibodies to treat and even prevent migraine (39,42). Unfortunately progress in the mechanism-based approach has been limited.
Brain imaging has shown that the complexity of the pain experience is mediated by a neuronal network connecting brain areas involved in sensory, emotional, and cognitive processes (13). Within the last two decades genetic and genomic sequencing has contributed to understanding several Mendelian pain disorders (6). Genetic analysis, careful analysis of symptoms and detailed sensory profiling of patients (2) with common pain conditions are areas being actively explored.
The development of more sophisticated outcome measures for pain beyond simple unidimensional pain scales may move us closer to identifying mechanisms underlying common pain disorders. Epidemiological pain research has great potential, not only for characterizing the prevalence of different types of pain, but also their causes and how to prevent them (11,51). The new classification system for chronic pain (46) may generate new epidemiological data, similar to what has been seen in the field of headache (23). Neuromodulation represents an interesting approach for both invasive and non-invasive electrical therapies for chronic pain (31). However, to rigorously test the effectiveness of these neuromodulation therapies, we need more high quality Randomized Controlled Trials (RCTs).
Highlights in Psychological Pain Research
In the early 1970s, psychological pain research was rapidly moving away from case studies rooted in psychodynamic formulations of chronic pain (i.e. the notions of psychogenic pain/”pain prone patient”). Spurred on by developments in research and pain theory (i.e., the gate control theory, behavioral and cognitive theories) and a growing recognition of the important role that biological, psychological and social factors play in illness and disease (the biopsychosocial model), new assessment and treatment strategies emerged. Advances in psychometrics (multidimensional scaling) informed the development of the McGill Pain Questionnaire (38). Psychophysical measures of sensory, affective, and other domains of pain are now used in many basic (pain threshold/tolerance measures; suprathreshold pain scaling) and applied research settings (e.g., quantitative sensory testing (QST)). The 1980s witnessed growth in the use of standardized psychological instruments and led to one of the most consistent, robust, and interesting findings in this area: i.e., how much individuals experiencing pain vary in their psychological functioning. Early studies using the Minnesota Multiphasic Inventory (MMPI)) found important individual personality differences and subgroups in chronic pain samples (9,43). We now know that such individual variations are apparent on most standardized psychological measures, e.g., those assessing pain-related thoughts, beliefs, expectations, coping, or observed pain-related behaviors. Recent studies show that one can use smartphones and mobile devices to reliably capture within and across day variations in these domains (44). This research can help clinicians better understand and explain variations in how their patients adjust to pain and can guide the tailoring of psychological treatments.
Psychological approaches now encompass a diverse array of empirically validated treatments. Fordyce pioneered a behavioral therapy approach based on operant conditioning (21). Early on, electromyographic (EMG) biofeedback (BFB) was found effective for tension headache. An important landmark study (24) found that changes in cognitions (self-efficacy), not changes in muscle tension (levels of EMG activity), explained the benefits of BFB for tension headache. Mitchell and White (40) were among of the first to develop and test a protocol for managing pain that taught patients cognitive and behavioral skills for managing pain (i.e., cognitive-behavioral therapy (CBT)). Turk (47) provided a comprehensive rationale and detailed description of CBT for chronic pain. Landmark studies demonstrated that CBT protocols could be tested using rigorous RCT methods (e.g., 48,52) and numerous RCTs have now tested psychological pain-treatment protocols (e.g., graded exposure, hypnosis, imagery, meditation, mindfulness training, acceptance and commitment therapy, and partner-assisted treatments). More RCTs testing the efficacy of combining psychological and medication treatments for pain are needed (e.g., 25, 28), given that this combination is used so often clinically. Recent interest in psychological treatments is not only due to growing evidence they may help in managing acute and persistent pain (e.g. in children, older adults, and those having disease-related pain conditions), but also to the possibility that they may limit long-term use of opioids. The current focus on developing novel and disseminable strategies for enhancing access to psychological treatments is important. This could ensure that psychological treatments for pain are more readily available to the large population of individuals who may need and benefit from them (12,15).
Conclusions
Although the field of pain research and clinical practice has advanced considerably in the 50 years since the founding of IASP, it is clear that our understanding and ability to manage pain, in particular chronic pain, remain limited. We believe future advances in basic and applied pain science will provide a key pathway to the goal that we all share: reducing pain and pain-related suffering.
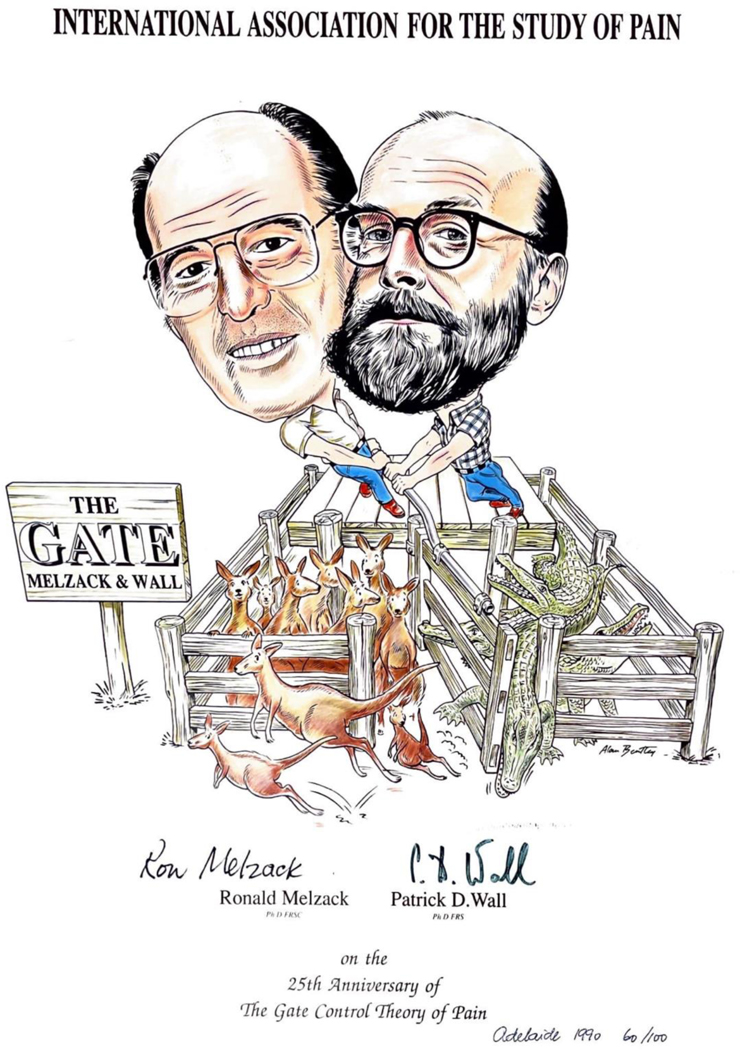
Figure 1:
This IASP poster of the Gate Control Theory, presented in Adelaide at the 1990 World Congress on Pain, celebrated the 25th anniversary of the Ronald Melzack and Patrick D. Wall publication: Pain mechanisms: A new theory. Science. 1965;150:971–979. The theory completely changed the way preclinical and clinical pain researchers addressed questions about the generation of acute and chronic pain, and provided important insights into novel approaches to pharmacological, neuromodulatory and psychological methods to pain management.
Acknowledgements:
This work was supported by: NIH NS R35 NS097306, DARPA-9691, Open Philanthropy (AIB); NIH: 5UH3-AT009790; 239631/1-R01AG064947; 60062239/5R01-CA271220; 5R01-CA249959; 5R01-CA237892; 5R01-CA229425; 5UH3-AR077360-04; 5UH3-AG067493; 5R21-DA052729; U01-DK123813; 5UG3-NR019196 and Novo Nordisk Foundation NNF14OC0011633 (TSJ)
Footnotes
Conflict of Interest:
The authors report no conflict of interest related to this paper.
Contributor Information
Allan I. Basbaum, Department of Anatomy, University California San Francisco, San Francisco, CA USA 94158.
Troels. S Jensen, Danish Pain Research Center, Department of Clinical Medicine, Aarhus University Hosital, DK, 8200 Aarhus N, Denmark.
Francis J. Keefe, Duke Pain Prevention and Treatment Research Program, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center, Durham, NC, USA 27705
REFERENCES:
- 1.Akil H, Mayer DJ, Liebeskind JC. Antagonism of stimulation-produced analgesia by naloxone, a narcotic antagonist. Science 1976;191:961–962. [DOI] [PubMed] [Google Scholar]
- 2.Baron R, Förster M, Binder A. Subgrouping of patients with neuropathic pain according to pain-related sensory abnormalities: a first step to a stratified treatment approach. Lancet Neurol 2012;11:999–1005. [DOI] [PubMed] [Google Scholar]
- 3.Basbaum AI, Bautista DM, Scherrer G, Julius D. Cellular and molecular mechanisms of pain. Cell 2009; 139:267–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basbaum AI, Fields HL Endogenous pain control systems: brainstem spinal pathways and endorphin circuitry. Annu Rev Neurosci 1984;7:309–338. [DOI] [PubMed] [Google Scholar]
- 5.Bender BJ, Gahbauer S, Luttens A, Lyu J, Webb CM, Stein RM, Fink EA, Balius TE, Carlsson J, Irwin JJ, Shoichet BK. A practical guide to large-scale docking. Nat Protoc 2021; 16:4799–4832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bennett DL, Clark AJ, Huang J, Waxman SG, Dib-Hajj SD. The role of voltage-gated sodium channels in pain signaling. Physiol Rev 2019;99:1079–1151. [DOI] [PubMed] [Google Scholar]
- 7.Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain 1988; 33:87–107. [DOI] [PubMed] [Google Scholar]
- 8.Bernard JF, Bester H, Besson JM. Involvement of the spino-parabrachio -amygdaloid and -hypothalamic pathways in the autonomic and affective emotional aspects of pain. Prog Brain Res 1996;107:243–255. [DOI] [PubMed] [Google Scholar]
- 9.Bradley LA, Prokop CK, Margolis R, & Gentry WD Multivariate analyses of the MMPI profiles of low back pain patients. J Beh Med 1978; 1: 253–27. [DOI] [PubMed] [Google Scholar]
- 10.Cousins MJ, Mather LE. Intrathecal and epidural administration of opioids. Anesthesiology 1984;6:276–310. [PubMed] [Google Scholar]
- 11.Crombie IK, Davies HTO, Macrae WA. The epidemiology of chronic pain: time for new directions. Pain 1994;57:1–3. [DOI] [PubMed] [Google Scholar]
- 12.Darnell BD Psychological treatment for chronic pain: Improving access and integration. Psychol Sci in Pub Interest 2021; 22: 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis KD, Flor H, Greely HT, Iannetti GD, Mackey S, Ploner M, Pustilnik A, Tracey I, Treede RD, Wager TD. Brain imaging tests for chronic pain: medical, legal and ethical issues and recommendations. Nature reviews Neurology 2017;13:624–638. [DOI] [PubMed] [Google Scholar]
- 14.De Felice M, Eyde N, Dodick D, Dussor GO, Ossipov MH, Fields HL, Porreca F. Capturing the aversive state of cephalic pain preclinically. Ann Neurol 2013; 74:257–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eccleston C, Blyth FM, Dear BF, Fisher EA, Keefe FJ, Lynch ME, Palermo TM, Reid CR, Williams A. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 2020; 161: 889–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Emery EC, Luiz AP, Wood JN Nav1.7 and other voltage-gated sodium channels as drug targets for pain relief Expert Opin Ther Targets 2016; 20:975–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fink EA, Xu J, Hübner H, Braz JM, Seemann P, Avet C, Craik V, Weikert D, Schmidt MF, Webb CM, Tolmachova NA, Moroz YS, Huang XP, Kalyanaraman C, Gahbauer S, Chen G, Liu Z, Jacobson MP, Irwin JJ, Bouvier M, Du Y, Shoichet BK, Basbaum AI, Gmeiner P. Structure-based discovery of nonopioid analgesics acting through the α2A-adrenergic receptor. Science 2022; 377:eabn7065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, Gilron I, Haanpaa M, Hansson P, Jensen TS, Kamerman PR, Lund K, Moore A, Raja SN, Rice AS, Rowbotham M, Sena E, Siddall P, Smith BH, Wallace M. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet neurology 2015;14:162–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finnerup NB, Kuner R, Jensen TS. Neuropathic pain: From mechanisms to treatment Physiol Rev 2019; 101: 259–301. [DOI] [PubMed] [Google Scholar]
- 20.Flor H, Noguchi K, Treede R-D, Turk DC The role of evolving concepts and new technologies and approaches in advancing pain education, research and management. PAIN 2023. this volume. [DOI] [PubMed] [Google Scholar]
- 21.Fordyce WE, Fowler RS, Lehmann JF, Delateur BJ, Sand PL, Trieschmann RB. Operant conditioning in the treatment of chronic pain. Arch Phys Med & Rehab 1973; 399–408. [PubMed] [Google Scholar]
- 22.Häring M, Zeisel A, Hochgerner H, Rinwa P, Jakobsson JET, Lönnerberg P, La Manno G, Sharma N, Borgius L, Kiehn O, Lagerström MC, Linnarsson S, Ernfors P. Neuronal atlas of the dorsal horn defines its architecture and links sensory input to transcriptional cell types. Nat Neurosci 2018; 21:869–880. [DOI] [PubMed] [Google Scholar]
- 23.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018;38:1–211. [DOI] [PubMed] [Google Scholar]
- 24.Holroyd KA, Nash JM, Pingel JD, Cordingl GE, Jerome A. A comparison of pharmacological (Amitriptyline HCL) and nonpharmacological (cognitive-behavioral) therapies for chronic tension headaches. J Cons Clin Psychol 1991; 59: 387–393. [DOI] [PubMed] [Google Scholar]
- 25.Holroyd KA, Penzien DB, Hursey KG, Tobin DL, Rogers L, Holm JE, Marcille PJ, Hall JR, Chila AG. Change mechanisms in EMG biofeedback training: cognitive changes underlying improvements in tension headache. J Cons Clin Psychol 1984; 52: 1039–1053. [DOI] [PubMed] [Google Scholar]
- 26.Hughes J, Smith TW, Kosterlitz HW, Fothergill LA, Morgan BA, Morris HR. Identification of two related pentapeptides from the brain with potent opiate agonist activity. Nature 1975; 258:577–580. [DOI] [PubMed] [Google Scholar]
- 27.Iyer SM, Vesuna S, Ramakrishnan C, Huynh K, Young S, Berndt A, Lee SY, Gorini CJ, Deisseroth K, Delp SL. Optogenetic and chemogenetic strategies for sustained inhibition of pain. Sci Rep 2016. 6:30570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keefe FJ, Shelby RA, Somers TJ, Varia I, Blazing M, Waters SJ, McKee D, Silva S, She L, Blumenthal JA, O’Connor J, Knowles V, Johnson P, Bradley L. Effects of coping skills training and sertraline in patients with non-cardiac chest pain: A randomized-controlled study. Pain 2011;152, 730–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kehlet H Postoperative pain, analgesia, and recovery-bedfellows that cannot be ignored. Pain 2018;159 Suppl 1:S11–s16. [DOI] [PubMed] [Google Scholar]
- 30.Kieffer BL, Evans CJ. Opioid receptors: from binding sites to visible molecules in vivo. Neuropharmacology. 200956 Suppl 1:205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Knotkova H, Hamani C, Sivanesan E, Le Beuffe MFE, Moon JY, Cohen SP, Huntoon MA. Neuromodulation for chronic pain. Lancet 2021; 397:2111–2124. [DOI] [PubMed] [Google Scholar]
- 32.Kuhn JA, Vainchtein ID, Braz J, Hamel K, Bernstein M, Craik V, Dahlgren MW, Ortiz-Carpena J, Molofsky AB, Molofsky AV, Basbaum AI. Regulatory T-cells inhibit microglia-induced pain hypersensitivity in female mice. Elife. 2021;10:e69056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Labau JIR, Andelic M, Faber CG, Waxman SG, Lauria G, Dib-Hajj SD. Recent advances for using human induced-pluripotent stem cells as pain-in-a-dish models of neuropathic pain. Exp Neurol 2022;358:114223. [DOI] [PubMed] [Google Scholar]
- 34.Langford DJ, Bailey AL, Chanda ML, Clarke SE, Drummond TE, Echols S, Glick S, Ingrao J, Klassen-Ross T, Lacroix-Fralish ML, Matsumiya L, Sorge RE, Sotocinal SG, Tabaka JM, Wong D, van den Maagdenberg AM, Ferrari MD, Craig KD, Mogil JS. Coding of facial expressions of pain in the laboratory mouse. Nat Methods 2010;7:447–449. [DOI] [PubMed] [Google Scholar]
- 35.Ledford H, Ewen Callaway E. Medicine Nobel goes to scientists who discovered biology of senses. Nature 2021;598: 246. [DOI] [PubMed] [Google Scholar]
- 36.Malmberg AB, Yaksh TL. Voltage-sensitive calcium channels in spinal nociceptive processing: blockade of N- and P-type channels inhibits formalin-induced nociception. J Neurosci 1994;14:4882–4890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McQuay HJ, Moore RA. An Evidence-based Resource for Pain Relief: Oxford University Press, 1998. [Google Scholar]
- 38.Melzack R The McGill Pain Questionnaire: Major properties and scoring methods. Pain 1975;1:277–299. [DOI] [PubMed] [Google Scholar]
- 39.Messina R, Goadsby PG. CGRP - a target for acute therapy in migraine: Clinical data Cephalalgia 2019;39:420–427. [DOI] [PubMed] [Google Scholar]
- 40.Mitchell KR, White RG. Behavioral self-management: An application to the problem of migraine headaches. Behavior Ther 1977;8: 213–222. [Google Scholar]
- 41.Moont R, Pud D, Sprecher E, Sharvit G, Yarnitsky D. “Pain inhibits pain” mechanisms: Is pain modulation simply due to distraction? Pain 2010;150:113–120. [DOI] [PubMed] [Google Scholar]
- 42.Olesen J, Diener HC, Husstedt IW, Goadsby PJ, Hall D, Meier U, Pollentier S, Lesko LM. Calcitonin gene-related peptide receptor antagonist BIBN 4096 BS for the acute treatment of migraine. The New England J Med 2004;350:1104–1110. [DOI] [PubMed] [Google Scholar]
- 43.Sternbach R Pain Patients: Traits and Treatments. New York: Academic Press, 1974. [Google Scholar]
- 44.Stone AA, Obbarius A, Junghaenel DU, Wen CKF, Schneider St. High resolution, field approaches for assessing pain: Ecological momentary assessment. Pain 2021;162: 4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tavares-Ferreira D, Shiers S, Ray PR, Wangzhou A, Jeevakumar V, Sankaranarayanan I, Cervantes AM, Reese JC, Chamessian A, Copits BA, Dougherty PM, Gereau RW 4th, Burton MD, Dussor G, Price TJ. Spatial transcriptomics of dorsal root ganglia identifies molecular signatures of human nociceptors. Sci Transl Med 2022;14:eabj8186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, Giamberardino MA, Kaasa S, Korwisi B, Kosek E, Lavand’homme P, Nicholas M, Perrot S, Scholz J, Schug S, Smith BH, Svensson P, Vlaeyen JWS, Wang SJ. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019;160:19–27. [DOI] [PubMed] [Google Scholar]
- 47.Turk DC, Meichenbaum D, Genest M. Pain and behavioral medicine: A cognitive-behavioral perspective. New York: Guilford, 1983. [Google Scholar]
- 48.Turner JA, Comparison of group progressive-relaxation training and cognitive-behavioral group therapy for chronic low back pain. J Cons Clin Psychol 1982;50:757–765. [DOI] [PubMed] [Google Scholar]
- 49.Urban DJ, Roth BL. DREADDs (designer receptors exclusively activated by designer drugs): chemogenetic tools with therapeutic utility. Annu Rev Pharmacol Toxicol 2015;55: 399–417. [DOI] [PubMed] [Google Scholar]
- 50.Usoskin D, Furlan A, Islam S, Abdo H, Lönnerberg P, Lou D, Hjerling-Leffler J, Haeggström J, Kharchenko O, Kharchenko PV, Linnarsson S, Ernfors P. Unbiased classification of sensory neuron types by large-scale single-cell RNA sequencing. Nat Neurosci 2015;18: 145–153. [DOI] [PubMed] [Google Scholar]
- 51.Von Korff M, Dworkin SF, Le Resche L, Kruger A. An epidemiologic comparison of pain complaints. Pain 1988;32:173–183. [DOI] [PubMed] [Google Scholar]
- 52.Williams CACde, Richardson PH Nicholas MK, Harding VR Ridout KL, Ralphs JA Richardson IH, Justins DM Chamberlain H. Inpatient versus outpatient pain management: Results of a randomized controlled trial. Pain 1996;66:13–22. [DOI] [PubMed] [Google Scholar]
- 53.Woolf CJ. Evidence for a central component of post-injury pain hypersensitivity Nature 1983;306:686–688. [DOI] [PubMed] [Google Scholar]
- 54.Woolf CJ, Bennett GJ, Doherty M, Dubner R, Kidd B, Koltzenburg M, Lipton R, Loeser JD, Payne R, Torebjork E. Towards a mechanism-based classification of pain? Pain 1998;77:227–229. [DOI] [PubMed] [Google Scholar]
- 55.Yaksh TL, Rudy TA. Analgesia mediated by a direct spinal action of narcotics. Science. 1976;192:1357–1358. [DOI] [PubMed] [Google Scholar]