Abstract
Introduction:
A major site of environmental tobacco smoke exposure for children and adults is the home. Few studies have evaluated the impact of e-cigarette or hookah use on home air quality, despite evidence finding toxic chemicals in secondhand e-cigarette aerosols and hookah smoke. Therefore, we assessed the effect of e-cigarette and hookah use on home air quality and compared it to air quality in homes where cigarettes were smoked and where no smoking or e-cigarette use occurred.
Methods:
Non-smoking homes and homes where e-cigarettes, hookah, or cigarettes were used were recruited in the NYC area. Particulate matter with diameter less than 2.5 microns (PM2.5), black carbon, and carbon monoxide (CO) were measured during a smoking or vaping session, both in a “primary” smoking room and in an adjacent “secondary” room where no smoking or vaping occurred. Log transformed data were compared with post-ANOVA Tukey Simultaneous tests.
Results:
Use of hookah significantly increased PM2.5 levels compared to non-smoking homes, in both the primary and secondary rooms, while use of e-cigarettes increased PM2.5 levels only in primary rooms. Additionally, in-home use of hookah resulted in greater CO concentrations than the use of cigarettes in primary rooms.
Conclusions:
The use of e-cigarettes or hookah increases air pollution in homes. For hookah, increases in PM2.5 penetrated even into rooms adjacent to where smoking occurs. Extending smoke-free rules inside homes to include e-cigarette and hookah products is needed to protect household members and visitors from being passively exposed to alternative tobacco products’ aerosols and gases.
Keywords: Electronic cigarettes, hookah waterpipe, home air quality, secondhand smoke
INTRODUCTION
In the US and worldwide, the leading preventable cause of disease and mortality is the use of tobacco products.1,2 The United States Surgeon General has stated that there is no safe level of tobacco smoke exposure, and an extensive body of research demonstrates the profound danger of cigarette-related secondhand smoke (SHS) not only to adults, but also to children, from prenatal and childhood SHS exposure.1,3 While cigarette use in the US has continued to decrease in recent years, from 20.9% in 20054 to 13.7% in 20185 among adults, use of other alternative tobacco products such as electronic cigarettes (e-cigarettes) and hookahs (water pipes, shisha) have increased, particularly among adolescents and younger adults.5–7 The use of e-cigarettes (called “vaping”), in fact, has displaced cigarettes as the most widely used nicotine delivery product among adolescents,8 with recent surveys indicating that 1 in 5 US high school students report currently using e-cigarettes9 (2020) and 4.1% report using hookah in the past 30 days (2018).8 With growing prevalence, exposure to secondhand e-cigarette aerosols and hookah smoke is also likely increasing. However, this line of research has been less studied, and comparatively little is known about the impacts of e-cigarette and hookah use on air quality in real-world settings such as homes, where non-smoking or vaping children and adults may be exposed.
Studies conducted in controlled exposure chambers/rooms or with smoking machines10–13 suggest that use of e-cigarettes releases carbonyls,10 glycerin,10 metals,13 nicotine,11,12,14 propylene glycol,10 volatile organic compounds,11 and ultrafine particles11 into the air. Evaluations in human subjects have found that individuals exposed to secondhand e-cigarette aerosol have increased salivary15,16 and serum17 cotinine levels, increased levels of acrolein biomarkers,16 and alterations in fractional exhaled nitric oxide and respiratory mechanics,18 compared to unexposed individuals or to baseline measures. However, only two of these studies was completed in the home environment, despite the home being an important location for passive exposure to tobacco products.
While the literature on the health effects of hookah smoking is limited, existing data are consistent in finding adverse health outcomes. Evidence suggests that hookah use may be as addictive19,20 and as harmful21–23 as cigarettes, and meta-analyses have linked hookah use to respiratory diseases, various cancers, and cardiovascular disease.24,25 The health effects of hookah SHS exposure are less understood, but include acute symptoms such as wheezing, nasal congestion, elevated exhaled carbon monoxide, and increased inflammatory markers.26–28
A major site of environmental tobacco smoke exposure for all people, but for children in particular, is the home environment.3 Our previous work assessing the effects of hookah smoking on home air quality in the United Arab Emirates found that homes where hookah smoking occurred had higher black carbon (BC), fine particulate (PM2.5), and carbon monoxide (CO) concentrations than homes where cigarette smoking occurred.29 To date, only two studies we are aware of have investigated the effect of e-cigarette use on home air quality.15,30 In one study, the authors demonstrated the presence of ambient air nicotine and increased levels of biomarkers of nicotine exposure;15 in the second only one e-cigarette home and one cigarette home were enrolled.30 The small number of such in-home studies contrasts markedly with the extensive knowledge base on cigarette SHS;3 more studies of in-home e-cigarette and hookah use are greatly needed to inform policy development.
To fill this important gap in our knowledge of how alternative tobacco products impact home air quality, we assessed the effect of e-cigarette and hookah use on indoor air quality in the home, and compared the results to air quality in homes where cigarettes were smoked and where no smoking or e-cigarette use occurred.
METHODS
Study Design, Setting, and Participants
This study was approved by the Institutional Review Board at New York University School of Medicine (Study Number s15-00011). A convenience sample of 57 homes in New York, New Jersey, and Connecticut were recruited: 12 homes where only hookah was smoked (“hookah homes”), 15 homes where only e-cigarettes were used (“e-cigarette homes”); 15 homes where cigarettes were smoked but neither hookah nor e-cigarettes were used (“cigarette homes”), and 15 homes where none of these products were used (“non-smoking/vaping homes”). For homes where e-cigarettes, hookah, or cigarettes were used, air quality was assessed in two rooms: those where active smoking/vaping of e-cigarettes, hookahs, or cigarettes occurred (“primary” rooms), and the rooms adjacent to primary rooms where no smoking or e-cigarette use occurred (“secondary” rooms). For non-smoking/vaping homes, air quality was assessed in one room in each participating home.
Air quality was assessed before (~10 min), during, and after (~10 min) a vaping or smoking session, in both a primary vaping or smoking room and a secondary adjacent non-vaping/non-smoking room. The sampling time during the sessions varied because, for ethical reasons, participants were instructed to smoke/vape as usual. Household inclusion criteria included: reporting customary use of e-cigarettes, hookahs, or cigarettes inside the home or the use of no tobacco products in the home, and the use of a single type of vaping or smoking product during the sampling period. Participants were asked that no vaping or smoking occur in the household for a minimum of 4 hours before the sampling period.
Variables and Measurements
In each home, air quality was assessed with a combination of real time sampling monitors and pre-calibrated pumps attached to filter holders. Integrated PM2.5 gravimetric sampling was done with pre-weighed Teflon filters (PALL Corporation, Michigan, USA) contained in a filter holder equipped with a 2.5 μm size-selective inlet and attached to a calibrated Legacy pump (SKC, Eighty Four, PA, USA), set to a flow rate of 10 L/min. After the sampling period, Teflon filters were sealed and transferred to a laboratory to be acclimated (minimum of 24 hrs) and weighed in a climate-controlled facility set to U.S. EPA standards.31 Real time PM2.5 was measured with a pDR-1500 aerosol monitor with a PM2.5 inlet (Thermo Fisher Scientific, Pittsburgh, Pennsylvania, USA) at 1 min intervals. Before each sampling run, the pDR-1500 was zeroed with a HEPA filter. Real time BC was measured at 1 min intervals with a microaethalometer with a PM2.5 inlet (Model AE51, AethLabs, San Francisco, California, USA). Real time CO was measured at 30 sec intervals with an EL-USB-CO data logger (0-300 ppm, Lascar, Erie, Pennsylvania, USA).
For vaping or smoking sessions, participants were encouraged to vape or smoke as much and for as long as they customarily do. This could include smoking multiple cigarettes or taking multiple puffs of an e-cigarette during the exposure time window. Vaping/smoking sessions for e-cigarettes, hookah, and cigarettes lasted for an average of 47.5, 41.8, and 22.5 minutes, respectively. During the vaping/smoking period, the research team measured air quality in the primary room (where e-cigarettes, hookah, or cigarettes were used) and simultaneously in the secondary room within the house where no vaping or smoking was ongoing. In non-smoking homes air was sampled for an average of 64.4 minutes in one “primary” room.
Information about the ventilation used during the vaping/smoking exposure period (e.g., windows open) were recorded. Room dimensions were obtained (Bosch GLM 20 Laser Measure 65’) to calculate room area for both primary and secondary rooms, as well as the distance between each room type. While participants were not asked directly about use of marijuana in the homes, the research team did ask if any substances had been vaped or smoked in the home on that day.
Statistical Methods
Descriptive statistics, including means, standard deviations, range, and 95% confidence intervals were calculated for each pollutant by home type (e-cigarette, hookah, cigarette, non-smoking/vaping) and room (primary vs. secondary). Each pollutant was considered separately and their log transformed concentrations were compared for significant differences (between home types and between room types within a product category). All main analyses described comparisons of the exposure time period during which active vaping or smoking occurred, as opposed to pre- or post-exposure air quality concentrations.
Comparison of pollutant levels in primary rooms between home types were done using a General Linear Model (GLM) analysis of variance, and a post-ANOVA comparison of log-transformed data with the Tukey Simultaneous Test. Sensitivity analyses adjusting for room area were also conducted. GLM analysis of variance with post-ANOVA comparisons were also completed to compare pollutant levels in secondary rooms between home types. Comparisons between room types within a home and pollutant type (e.g., CO concentrations in hookah primary rooms vs. CO concentrations in hookah secondary rooms) were conducted using two-sample T-tests. Statistical analyses were completed using Minitab 18 (State College, PA: Minitab, Inc.) and STATA 14 (StataCorp, College Station, TX). Plots were developed with Minitab 18 and R Version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Means, standard deviations, and ranges of BC, PM2.5, and CO concentrations during the exposure period in the primary and secondary rooms are shown in Table 1. Briefly, BC ranged from a high of 3.8 μg/m3 (SD = 8.0 μg/m3) during hookah smoking in primary rooms to a low of 0.4 μg/m3 (SD = 0.3 μg/m3) in e-cigarette secondary rooms. PM2.5 ranged from 996.6 μg/m3 (SD = 2,679.5 μg/m3) during e-cigarette vaping in primary rooms to a low of 15.1 μg/m3 (SD = 48.3 μg/m3) in non-smoking/non-vaping homes. CO concentrations were also variable among home types, with a high of 8.4 ppm (SD = 5.8 ppm) in rooms where hookah was being smoked to a low of 0.8 ppm (SD = 1.6 ppm) in e-cigarette secondary rooms. A detailed breakdown of home characteristics, including mean sampling time, room area, and distance between primary and secondary rooms, by pollutant and room type, can be found in Supplementary Table 1. Means and standard errors for each pollutant, product, room, and time period (pre-exposure, exposure, post-exposure) can be found in Supplementary Figures 1–3. As shown in Supplementary Figures 2–3, post-exposure period CO and BC concentrations remained elevated for homes where hookah was smoked.
Table 1.
Mean, standard deviation, and range for black carbon (BC), PM2.5, and carbon monoxide (CO) levels in primary and secondary rooms, by pollutant
| Product Used | Room Type* | BC [μg/m3] | PM2.5 [μg/m3] | CO [ppm] | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Mean (SD) | Range | Mean (SD) | Range | Mean (SD) | Range | ||
| Hookah | Primary | 3.8 (8.0) | 0-26.7 | 308.6 (624.3) | 6.3-1992.4 | 8.4 (5.8) | 0.5-19.2 |
| Hookah | Secondary | 1.1 (1.4) | 0-4.1 | 66.7 (95.2) | 0.7-291.8 | 6.3 (6.9) | 0-23.8 |
| E-cigarette | Primary | 0.8 (1.0) | 0-3.5 | 996.6 (2679.5) | 1.1-9536.9 | 1.6 (2.3) | 0-6.5 |
| E-cigarette | Secondary | 0.4 (0.3) | 0.02-1.0 | 22.4 (33.4) | 0.5-113.2 | 0.8 (1.6) | 0.4.5 |
| Cigarette | Primary | 1.7 (1.5) | 0.4-5.8 | 328.5 (403.3) | 10.6-1156.0 | 1.5 (1.7) | 0-5.8 |
| Cigarette | Secondary | 1.1 (1.0) | 0.2-4.0 | 102.3 (102.7) | 0.6-309.2 | 1.2 (1.5) | 0-4.0 |
| Non-smoking | 0.5 (0.5) | 0-1.5 | 15.1 (48.3) | 0.9-189.7 | 3.0 (1.2) | 2.0-6.6 | |
Primary rooms were defined as rooms where e-cigarettes, cigarettes, or hookahs were being used and secondary rooms were defined as rooms adjacent to where such products were being used
Abbreviations: BC = black carbon; PM2.5 = particulate matter with diameter less than 2.5 micrometers; CO = carbon monoxide; SD = standard deviation
Comparison of Air Quality Between Home Types within Primary Vaping/Smoking Rooms
For primary rooms where vaping or smoking occurred, post-ANOVA comparisons identified significant differences between log-transformed pollutant levels (Figure 1). PM2.5 levels in the rooms where e-cigarettes, hookah, or cigarettes were used were all significantly greater than levels in non-smoking/vaping homes (p ≤ 0.05), but not significantly different from each other. CO levels were significantly higher in the primary rooms where hookah was smoked, compared to rooms where cigarettes were smoked (p ≤ 0.05). No other significant differences were found for CO, and no significant differences were found for BC. Differences of means and 95% confidence intervals are presented in Supplemental Table 2. Sensitivity analyses adjusting for room size were consistent with main results, with one exception: CO concentrations were significantly higher in hookah primary rooms than concentrations in non-smoking/vaping homes.
Figure 1:
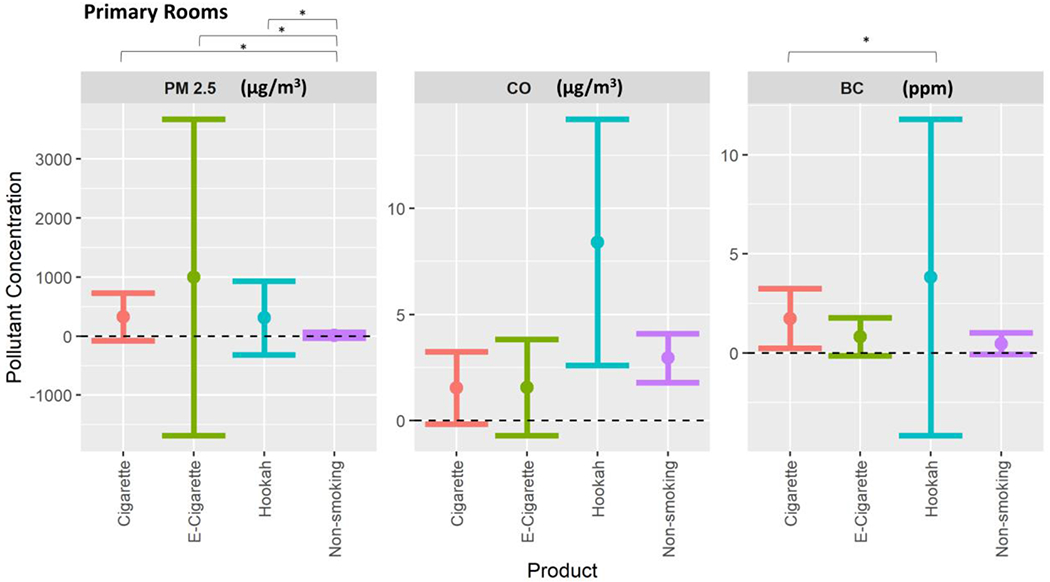
Means (points) plus/minus the standard deviation (lines) for each pollutant by product group, for all “primary” rooms where cigarettes, e-cigarettes, or hookah was used and non-smoking/vaping rooms. PM 2.5 = particulate matter with diameter less than 2.5 micrometers, BC = black carbon, CO = carbon monoxide. * = p ≤ 0.05
Comparison of Air Quality Between Home Types in the Secondary Rooms
Significant differences between log-transformed pollutant levels in homes by tobacco product type were also found for the secondary rooms adjacent to the rooms where active vaping or smoking took place (Figure 2). PM2.5 levels in secondary rooms were significantly greater than levels in non-smoking/vaping homes, but no significant difference was found in PM2.5 between secondary e-cigarette rooms and non-smoking/vaping homes. Additionally, CO levels were greater in hookah secondary rooms compared to e-cigarette secondary rooms. No significant differences were found between secondary room concentrations for BC. Differences of means and 95% confidence intervals for all adjacent room comparisons are shown in Supplemental Table 2.
Figure 2:
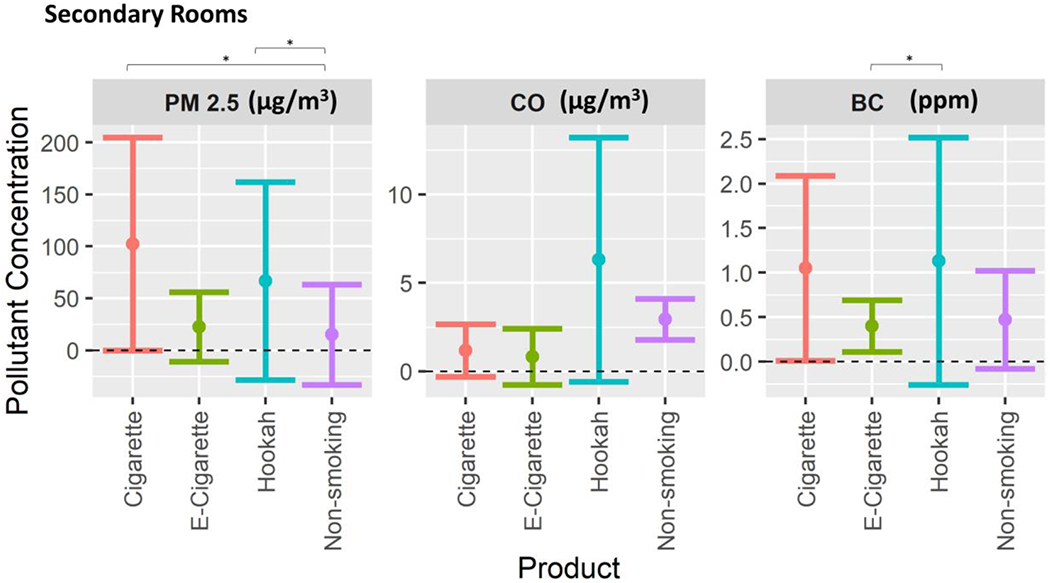
Means (points) plus/minus the standard deviation (lines) for each pollutant by product group, for all “secondary” rooms adjacent to where cigarettes, e-cigarettes, or hookah was used and non-smoking/vaping rooms. PM 2.5 = particulate matter with diameter less than 2.5 micrometers, BC = black carbon, CO = carbon monoxide. * = p ≤ 0.05
Comparison of Air Quality Between Primary and Secondary Rooms
Comparisons between primary and secondary rooms resulted in only one significant pollutant concentration difference: e-cigarette primary rooms had greater BC concentrations than e-cigarette secondary rooms. There were no significant differences in PM2.5, CO, or BC concentrations between primary and secondary rooms in homes where hookah was smoked, and no significant differences in PM2.5 or CO concentrations between primary and secondary rooms in homes where e-cigarettes were used. Although it didn’t reach statistical significance, PM2.5 concentrations were elevated in primary rooms compared to secondary rooms for both e-cigarette and hookah homes.
DISCUSSION
This study is, to our knowledge, one of the first in-home assessments of air quality changes that occur during the use of e-cigarettes and hookah. We measured PM2.5, CO, and BC in both the primary smoking/vaping rooms and in secondary adjacent rooms where non-smoking individuals or children may stay to reduce exposure in homes where e-cigarettes, hookah, or combustible cigarettes are being used. As expected, we found significantly elevated PM2.5 levels in the rooms where e-cigarettes and hookah were being used as compared to non-smoking homes. While this pattern persisted in secondary rooms for hookah, it did not for e-cigarettes, suggesting that secondhand hookah smoke particles may penetrate more readily into adjacent living quarters. Additionally, we found that the use of hookah significantly increased CO concentrations, compared to the use of cigarettes, in primary rooms. These findings suggest that in-home use of both e-cigarettes and hookah contributes to deleterious indoor air quality, and that withdrawing to an adjacent room where alternative tobacco products aren’t being used may not adequately protect household members such as children from exposure to harmful air pollutants, particularly when hookah is used in homes.
At least 3 other studies have evaluated the impact of hookah29 or e-cigarette15,30 use on indoor air quality in homes. Our previous work in Dubai, United Arab Emirates, found that in homes where hookahs were being used, CO concentrations were greater in both the primary and secondary rooms than in both cigarette-smoking homes and non-smoking homes.29 This finding is consistent with what we report here in the United States: homes where hookah was smoked had significantly increased CO levels in primary rooms compared to homes where cigarettes were smoked. It has been well documented that the charcoal used to heat shisha in the hookah waterpipe is the source for the majority of CO emissions generated during hookah smoking.32 Alternative means of heating shisha, such as the use of electric heating modules, may prove successful in reducing secondhand exposure to CO33 emitted by hookah use. The Dubai study also found non-significantly increased PM2.5 levels in homes where hookah was smoked compared to cigarette and non-smoking homes; this is consistent with the significantly increased PM2.5 levels in hookah homes compared to non-smoking/vaping homes observed in the current study. Thus, in-home use of hookah may produce a greater risk of secondhand smoke exposure to the harmful chemicals generated by the combustion of tobacco than occurs with cigarette smoking.
A study conducted by Ballbè and colleagues15 evaluated the impact of in-home e-cigarette use on airborne nicotine and salivary cotinine levels (a biomarker metabolite of nicotine exposure15). The authors found that nicotine levels in homes where e-cigarettes were used were lower compared to homes where cigarettes were used, but greater than the airborne nicotine levels in non-smoking homes.15 They also found that individuals exposed passively to secondhand e-cigarette vapors had increased salivary cotinine levels.15 Other in-home studies have found nicotine on surfaces in the homes of e-cigarette users,30 and increased PM2.5 levels in the 1 home where e-cigarettes were being used, compared to 2 non-smoking homes.14 While we did not assess airborne nicotine or salivary cotinine in home residents, our air quality results suggest that individuals living in homes where e-cigarettes or hookah are used are passively exposed to higher levels of PM2.5, and for hookah, CO. Further studies are needed to assess changes in biomarkers of exposure and effect in non-smoking adults and children passively exposed to secondhand e-cigarette aerosols and hookah smoke, particularly in home environments.
Limitations
This study has a number of limitations. First, because participants were recruited using a convenience sample, they were likely not representative of the greater New York metropolitan area or of the United States. Second, while we instructed the study participants not to vape or smoke any tobacco products (or marijuana) inside the home for at least four hours before the study visit, we cannot be sure that the participants followed instructions. However, whereas our post-hookah session measurements demonstrated that elevation in air pollutant levels lingered after the smoking session ended, our brief ~10 min assessment of air quality before the vaping or smoking sessions demonstrated low air pollution concentrations which were similar to the non-smoking homes, suggesting that the participants did comply (Supplementary Figures 1–3). Third, due to the small sample size, we did not statistically evaluate differences in air pollutant levels by e-cigarette type, although we did observe a trend for higher pollutant levels during the use of subohm-type devices (e.g., Mod/tank type devices or those with a coil resistance level below 1 ohm). Finally, many factors likely impacted inter-home variability, resulting in wide standard deviations and decreased statistical power, ranging from room ventilation and size, duration of vaping/smoking and intensity of product use, type of shisha or charcoal used, type of e-cigarette product used, and number of adults participating in the smoking or vaping sessions. However, including room size in a sub-analysis had minimal impact on the findings. Thus, one of the strengths of our study design is that it was able to discern statistically significant air quality differences in NYC-area and Dubai29 homes even with this real-world variability.
Conclusion
To address indoor air pollution, wide-ranging clean indoor air laws regarding cigarette smoking have been widely adopted by local communities and states across the US. Similarly, at a much slower rate, there is an increase in smoke-free housing policies that restrict smoking of any agent within the building.34–36 Strong public support has contributed to the adoption, at this date, of 100% smoke-free laws by 41 states and 1,320 municipalities.37,38 Understanding the effect of both e-cigarette and hookah use on indoor air quality is essential to supporting ongoing work to augment these clean indoor air laws and smoke-free housing policies, which do not frequently apply to e-cigarette use and sometimes contain loopholes for hookah use (e.g., if the shisha used does not contain nicotine). The World Health Organization has recommended that countries extend their smoking bans in indoor public places to include e-cigarettes in order to restrict uptake and minimize health risks in non-smokers.39 A number of states and municipalities have proceeded accordingly by prohibiting e-cigarettes in traditionally 100% cigarette smoke-free venues (i.e. restaurants and bars), schools, and work places.38 The research reported in this paper suggests that in-home use of e-cigarettes or hookah is also harmful, and that impacts on air quality can extend throughout the home, to rooms where vaping or smoking does not take place. Thus, extending smoke-free rules inside homes to e-cigarettes and hookah appears prudent to further protect people who are passively exposed to aerosols or smoke generated by these alternative tobacco products and delivery systems.
Supplementary Material
WHAT THIS PAPER ADDS.
What is already known on this subject? Use of e-cigarettes and hookah has grown over the last decade, resulting in increased exposure to secondhand aerosols and smoke from these alternative tobacco products. Prior research shows that secondhand e-cigarette aerosols and hookah smoke contain toxic and harmful chemicals.
What important gaps in knowledge exist on this topic? Very few studies have evaluated deleterious air quality from use of e-cigarettes and hookah in real-world settings, such as the home, where exposure to secondhand aerosols or smoke is likely to impact children and adults. Additionally, only one study to our knowledge has measured air quality in both a “primary” active smoking/vaping room, and in a “secondary” adjacent room where children may be placed to protect them from smoke or aerosol exposure.
What this paper adds. This study measures particulate matter (PM2.5), carbon monoxide (CO), and black carbon (BC) levels in homes where e-cigarettes and hookah are being used, both in a primary smoking/vaping room, and in a secondary adjacent room, and compares pollutant concentrations to those found in homes where cigarettes are smoked or where no smoking/vaping occurs. The study finds that smoking either hookah or cigarettes significantly increased PM2.5 levels as compared to non-smoking homes, for both the primary and secondary rooms, while using e-cigarettes increased PM2.5 levels only in the primary rooms. Additionally, in-home use of hookah resulted in greater CO concentrations than the use of cigarettes in primary rooms.
FUNDING
This research was supported by NIH grants 1R21ES026996 and 1R01HL139239. JAS was also supported by NIEHS grant 2T32ES007322-19.
Footnotes
COMPETING INTERESTS
The authors declare no competing interests.
REFERENCES
- 1.US Department of Health and Human Services. The Health Consequences of Smoking - 50 Years of Progress: A Report of the Surgeon General. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health;2014. [Google Scholar]
- 2.Samet JM. Tobacco smoking: the leading cause of preventable disease worldwide. Thoracic surgery clinics. 2013;23(2):103–112. [DOI] [PubMed] [Google Scholar]
- 3.Office on Smoking and Health (US). The Health Consequences of Involuntary Exposure to Tobacco Smoke: of the Surgeon General. 2006. [PubMed]
- 4.Control CfD, Prevention. Tobacco use among adults--United States, 2005. MMWR Morbidity and mortality weekly report. 2006;55(42):1145. [PubMed] [Google Scholar]
- 5.Creamer MR, Wang TW, Babb S, et al. Tobacco product use and cessation indicators among adults—United States, 2018. Morbidity and Mortality Weekly Report. 2019;68(45):1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agaku IT, King BA, Husten CG, et al. Tobacco product use among adults—United States, 2012–2013. MMWR Morbidity and mortality weekly report. 2014;63(25):542. [PMC free article] [PubMed] [Google Scholar]
- 7.Dai H, Leventhal AM. Prevalence of e-cigarette use among adults in the United States, 2014-2018. Jama. 2019;322(18):1824–1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gentzke AS, Creamer M, Cullen KA, et al. Vital signs: tobacco product use among middle and high school students—United States, 2011–2018. Morbidity and Mortality Weekly Report. 2019;68(6):157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang TW, Neff LJ, Park-Lee E, Ren C, Cullen KA, King BA. E-cigarette Use Among Middle and High School Students—United States, 2020. Morbidity and Mortality Weekly Report. 2020;69(37):1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geiss O, Bianchi I, Barahona F, Barrero-Moreno J. Characterisation of mainstream and passive vapours emitted by selected electronic cigarettes. International journal of hygiene and environmental health. 2015;218(1):169–180. [DOI] [PubMed] [Google Scholar]
- 11.Schripp T, Markewitz D, Uhde E, Salthammer T. Does e-cigarette consumption cause passive vaping? Indoor air. 2013;23(1):25–31. [DOI] [PubMed] [Google Scholar]
- 12.Czogala J, Goniewicz ML, Fidelus B, Zielinska-Danch W, Travers MJ, Sobczak A. Secondhand Exposure to Vapors From Electronic Cigarettes. Nicotine & Tobacco Research. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saffari A, Daher N, Ruprecht A, et al. Particulate metals and organic compounds from electronic and tobacco-containing cigarettes: comparison of emission rates and secondhand exposure. Environmental Science: Processes & Impacts. 2014;16(10):2259–2267. [DOI] [PubMed] [Google Scholar]
- 14.Bush D, Goniewicz ML. A pilot study on nicotine residues in houses of electronic cigarette users, tobacco smokers, and non-users of nicotine-containing products. Int J Drug Policy. 2015;26(6):609–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ballbè M, Martínez-Sánchez JM, Sureda X, et al. Cigarettes vs. e-cigarettes: Passive exposure at home measured by means of airborne marker and biomarkers. Environmental Research. 2014;135:76–80. [DOI] [PubMed] [Google Scholar]
- 16.Johnson JM, Naeher LP, Yu X, et al. A biomonitoring assessment of secondhand exposures to electronic cigarette emissions. International journal of hygiene and environmental health. 2019;222(5):816–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flouris AD, Chorti MS, Poulianiti KP, et al. Acute impact of active and passive electronic cigarette smoking on serum cotinine and lung function. Inhalation toxicology. 2013;25(2):91–101. [DOI] [PubMed] [Google Scholar]
- 18.Tzortzi A, Teloniatis SI, Matiampa G, et al. Passive exposure to e-cigarette emissions: Immediate respiratory effects. Tobacco Prevention & Cessation. 2018;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cobb CO, Shihadeh A, Weaver MF, Eissenberg T. Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2011;13(2):78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noonan D, Kulbok PA. New tobacco trends: waterpipe (hookah) smoking and implications for healthcare providers. Journal of the American Academy of Nurse Practitioners. 2009;21(5):258–260. [DOI] [PubMed] [Google Scholar]
- 21.Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. American journal of preventive medicine. 2009;37(6):518–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knishkowy B, Amitai Y. Water-pipe (narghile) smoking: an emerging health risk behavior. Pediatrics. 2005;116(1):e113–119. [DOI] [PubMed] [Google Scholar]
- 23.Shihadeh A. Investigation of mainstream smoke aerosol of the argileh water pipe. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association. 2003;41(1):143–152. [DOI] [PubMed] [Google Scholar]
- 24.Waziry R, Jawad M, Ballout RA, Al Akel M, Akl EA. The effects of waterpipe tobacco smoking on health outcomes: an updated systematic review and meta-analysis. International journal of epidemiology. 2017;46(1):32–43. [DOI] [PubMed] [Google Scholar]
- 25.Montazeri Z, Nyiraneza C, El-Katerji H, Little J. Waterpipe smoking and cancer: systematic review and meta-analysis. Tobacco control. 2017;26(1):92–97. [DOI] [PubMed] [Google Scholar]
- 26.Kumar SR, Davies S, Weitzman M, Sherman S. A review of air quality, biological indicators and health effects of second-hand waterpipe smoke exposure. Tobacco control. 2015;24(Suppl 1):i54–i59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kassem NO, Daffa RM, Liles S, et al. Children’s exposure to secondhand and thirdhand smoke carcinogens and toxicants in homes of hookah smokers. nicotine & tobacco research. 2014;16(7):961–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou S, Behrooz L, Weitzman M, et al. Secondhand hookah smoke: an occupational hazard for hookah bar employees. Tobacco control. 2017;26(1):40–45. [DOI] [PubMed] [Google Scholar]
- 29.Weitzman M, Yusufali AH, Bali F, et al. Effects of hookah smoking on indoor air quality in homes. Tobacco control. 2017;26(5):586–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fernandez E, Ballbe M, Sureda X, Fu M, Salto E, Martinez-Sanchez JM. Particulate Matter from Electronic Cigarettes and Conventional Cigarettes: a Systematic Review and Observational Study. Current environmental health reports. 2015;2(4):423–429. [DOI] [PubMed] [Google Scholar]
- 31.Wood Environment & Infrastructure Solutions Inc. Determination of Particulate Matter (PM) Gravimetric Mass for the Chemical Speciation Network. 2018. GLM3180-009.
- 32.Monzer B, Sepetdjian E, Saliba N, Shihadeh A. Charcoal emissions as a source of CO and carcinogenic PAH in mainstream narghile waterpipe smoke. Food and Chemical Toxicology. 2008;46(9):2991–2995. [DOI] [PubMed] [Google Scholar]
- 33.Brinkman MC, Kim H, Buehler SS, Adetona AM, Gordon SM, Clark PI. Evidence of compensation among waterpipe smokers using harm reduction components. Tobacco control. 2020;29(1):15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trosclair A, Babb S, Murphy-Hoefer R, et al. State-specific prevalence of smoke-free home rules-United States, . Mortal Wkly Rep. 501504. 2007;56:1992–2003. [PubMed] [Google Scholar]
- 35.King BA, Cummings KM, Mahoney MC, Juster HR, Hyland AJ. Multiunit housing residents’ experiences and attitudes toward smoke-free policies. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2010;12(6):598–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.King BA, Travers MJ, Cummings KM, Mahoney MC, Hyland AJ. Prevalence and predictors of smoke-free policy implementation and support among owners and managers of multiunit housing. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2010;12(2):159–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.American Nonsmokers’ Rights Foundation. Overview List- How many Smokefree Laws? 2016.
- 38.American Nonsmokers’ Rights Foundation. States, commonwealth, and territories with 100% smokefree laws in all non-hospitality workplaces, restaurants, and bars. 2016.
- 39.World health Organization. Electronic nicotine delivery systems and electronic non-nicotine delivery systems (ENDS/ENNDS). Geneva: World Health Organization;2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


