Abstract
Background
During the confinement, there was an increase in the incidence of mental disorders such as depression and anxiety. In this regard, affectivity is of particular interest, as emotions play a fundamental role in overall mental health. The literature on COVID-19 in this population has often focused on the analysis of risk factors for mental health, while less attention has been paid to protective factors. In this paper, we propose an inclusive model of risk and protective factors for adolescent mental health through the indirect effect of negative and positive affect.
Methods
This was a cross-sectional study with a Spanish community sample of 477 adolescents (Mage = 16.23, range:14 to 20 years old; 43.4% were boys; response rate: 100%). We measured the perceived hardness of confinement, worrying about contagion, quality of relationships at home, pleasant activities, affect (positive and negative), and mental health.
Results
The results revealed a positive relationship between the perceived hardness of confinement and worrying about contagion with mental health, through the indirect effect of negative affect, and a positive relationship between home relationships and pleasant activities with mental health through an indirect effect of positive affect.
Conclusion
Our results suggest that different types of emotions generated by the various contextual variables associated with COVID-19 may have a differential impact on mental health. These findings support the inclusive model of risk and protective factors for adolescent mental health. Practical implications, future studies, and limitations are discussed.
Keywords: COVID-19, adolescents, mental health, affectivity, contextual variables
Introduction
The appearance of COVID-19 at the end of 2019 led to a worldwide state of health alert and the subsequent period of home confinement during early 2020. From this moment on, all efforts were directed towards studying how the virus interacted with the organism and with mental health. The lockdown strategy implemented to control the pandemic involved closing schools and businesses. These measures imposed social isolation, which resulted in drastic changes to society’s lifestyle, which had great potential to cause a strong psychological impact on the population.1–3 These confinement effects can lead to a significant decline in mental health, especially in adolescents,4,5 who are more likely to develop psychopathological issues compared to adults.1,6–8 For example, in the social context, confinement disrupted interactions with friends, extended family, and educators. For instance, research has shown that the prevalence of mental disorders in adolescents, such as anxiety, depression, sleep disorders, OCD, and post-traumatic stress disorder symptoms increased during confinement compared to pre-pandemic periods.9–11
There is now a broad consensus on the influence of emotions on mental health, that is, positive and negative affect. Positive affect (eg, satisfaction, enthusiasm, optimism, pleasure) is related to greater resilience, happiness, creativity, and even longer life expectancy12 while low levels of positive affect are associated with depression and anxiety.13,14 In contrast, negative affect (eg, sadness, hostility, loneliness, fear) promotes behavioral inhibition and attentional self-focus and often predisposes individuals to mood disorders such as anxiety and depression.15 In this sense, imposed home confinement can be regarded as an aversive experience due to the isolation and the modification of daily habits it generates. This type of confinement can provoke extreme changes in the emotional state of the adolescent population, generating strong negative affectivity such as anger, confusion, and distress.6,7 A longitudinal study conducted by Fernández-Abascal and Martín-Díaz16 reported a decrease in positive affectivity in adults during confinement compared to pre-pandemic periods. A study by Muñoz-Navarro et al17 in younger populations reported a higher incidence of emotional disturbances during the initial COVID-19 outbreak. In addition, the limited interaction with the usual community network can lead to intense negative emotionality, such as feelings of loneliness.18,19
The literature on the impact of COVID-19 on adolescent mental health has proposed different risk factors, such as worrying about contagion, lack of information, family economic destabilization, and the hardness of confinement.6,20 In this regard, worrying about contagion and hardness of confinement are the factors that have received the most attention. For example, the results of a meta-analysis by Nearchou et al2 found that worrying about contagion (both self and family members) predicted the occurrence of affective disorders, somatic symptomatology, OCD, and an increase in behaviour problems among young people. Regarding the perceived hardness of confinement, several studies have shown how the characteristics and hardness of confinement were related to the occurrence of post-traumatic stress symptoms, anger, frustration, and avoidance behaviours, which may influence mental health more than other variables such as personality.6,21,22 Within this context, Spain suffered one of the harshest lockdowns (15 March to 4 May 2020), which severely disrupted the lives of its population in the short, medium, and long term.23
Additionally, the literature has also shown how certain variables could be protective factors for adolescent mental health during confinement, such as family relationships and engagement in activities. It is important to consider that home confinement also entailed an overexposure to the nuclear family (or household inhabitants). In this sense, family dynamics play a fundamental role in psychological and emotional health24,25 and the ability to manage different life domains, such as effectively coping with crises.26 Previous studies show that higher levels of family adaptability are associated with higher levels of positive affectivity,27 a lower likelihood of engaging in dysfunctional behaviours,28 and a lower likelihood of developing depressive symptomatology during the pandemic.29 Conversely, inadequate family support, latent family conflict, the presence of psychopathology, and economic stress may foster dysfunctional relationships among family members, which can lead to the development of negative affectivity,30 depressive symptomatology,31 and even domestic violence.32,33 Some countries have reported increased calls to emergency services and reports of domestic violence during confinement.34 However, engaging in pleasant activities (eg, cooking, reading, sport) contributes to increased levels of happiness and well-being.35,36 It has been shown that engaging in enjoyable activities through emotional regulation is associated with lower levels of depressive symptomatology and greater positive affectivity,37,38 the latter of which was reduced in the outbreak of the pandemic.39 Thus, it appears that the establishment of healthy family relationships may be a protective factor for mental health.
The previous literature on the impact of COVID-19 on adolescent mental health has focused on the prevalence of risk factors that contribute to the development of psychopathologies during confinement2,3 and, to a lesser extent, analysing the protective factors that enable a preventive approach to the mental health of adolescents in confinement.17,39 This work aims to bring together both perspectives by proposing an inclusive model of risk and protective factors associated with the mental health of the adolescent population through the indirect role of positive and negative affect. In this study, we analysed four contextual variables associated with COVID-19: the perceived hardness of confinement and worrying about contagion as risk factors for mental health; and on the other hand, relationships at home and engagement in pleasant activities as protective factors for mental health. Thus, we propose that the four contextual variables under study associated with confinement can provoke changes in mental health through affectivity. As an additional objective, we analysed possible gender differences in the study variables and the relationships between them. The consequences of COVID-19 continue to wreak havoc on socialisation, economics, and general health worldwide, and this work aims to contribute to a deeper understanding of the mechanisms underlying the potential differential impact of these consequences on adolescent mental health. This theoretical knowledge could then inform the design of effective prevention and coping strategies that could be implemented to improve the social climate and crisis management in this life cycle period when adverse events can be particularly problematic and developmentally determinant.
Given the objectives of the study, the working hypotheses were: (1) perceived hardness of confinement and worrying about contagion are positively related to negative affect and negatively related to positive affect; (2) relationships at home and pleasant activities are negatively related to negative affect and positively related to positive affect; (3) mental health is negatively related to negative affect and positively related to positive affect; (4) according to our proposed inclusive model of risk and protective factors for mental health, on the one hand, high levels of perceived hardness of confinement and worrying about contagion indirectly decrease mental health through the indirect effect the mediating effect of affectivity, while on the other hand, high levels of adequate relationships at home and pleasant activities indirectly increase mental health also through the mediation of indirect effect of affectivity.
Methods
Participants
A community sample of 477 students from 10 high schools in Andalusia (Spain) participated in the study. The age range of the sample was from 14 to 20 years (Mage = 16.23, SD = 1.50), with 207 boys (43.4%) and 270 girls (56.6%). The researchers contacted each high school in advance and agreed with the relevant teachers about passing the different tests. High school students participated in the study with written informed consent from their parents/legal guardians. Participants were informed of the confidentiality and anonymity of their responses and were treated in accordance with the Helsinki declaration.40 This study was approved by the Research Ethics Committee of the University of Málaga (approval number: 10–2019-H).
Instruments and Procedure
Students completed the battery of questionnaires in an online format via the LimeSurvey platform (www.limesurvey.org) at home under the instruction of their teachers, taking an estimated 25 minutes. The instruments used were:
Mental health was assessed using the mental health subscale (MH-5) of the Survey SF-36 Questionnaire (SF-36)41 in its Spanish validation.42 It consists of five items measuring vitality, social functioning, emotional role, and mental health on a Likert scale ranging from 1 (never) to 6 (always) points. Higher scores on this subscale indicate poorer mental health. In our sample, internal consistency was good for this subscale: α =0.82.
Positive and negative affect was measured using the Positive and Negative Affect Schedule (PANAS13) in its Spanish validation.43 This scale consists of 20 items measured on a Likert scale ranging from 1 (very slightly or never) to 5 (extremely), of which 10 measure negative affect and 10 positive affect. This scale measures affective states, moods, and traits at the time point indicated by the experimenters in the instructions section. For example, high scores on positive affect indicate an energetic and highly attentive state, while low scores reflect sad and dazed states. In contrast, high scores on negative affect indicate the presence of subjective distress, while low scores indicate states of serenity and calmness. In our sample, the internal consistency of this questionnaire was good for both positive affect (α = 0.82) and negative affect (α = 0.80).
Four items were employed to measure the four COVID-19 contextual variables under study on a Likert scale from 1 (totally agree) to 7 (totally disagree). These items were designed according to previous literature assessing COVID-related variables during the period of confinement (see the systematic review of Nearchou et al2). First, Perceived hardness of confinement was assessed through the item: this confinement is harder than I thought it would be (in Spanish: este confinamiento está siendo más duro de lo que pensaba). The item I am worried about getting infected or my family members getting infected with the coronavirus was used for Worrying about contagion (in Spanish: me preocupa contagiarme o que mis familiares se contagien con el coronavirus). To measure the Relationships at home and Pleasant activities, the items in the last two weeks, the relationships between the people living in my house are good (in Spanish: en estas dos últimas semanas, las relaciones entre las personas que viven en mi casa son buenas) and in these last two weeks I have engaged in activities at home that I like and make me feel good (eg exercise, watching series, reading, listening to music, cooking, etc.) (in Spanish: en estas dos últimas semanas hago actividades en casa que me gustan y me hacen sentir bien (por ejemplo: ejercicio, ver series, leer, escuchar música, cocinar, etc.) were used respectively.
Statistical Analysis
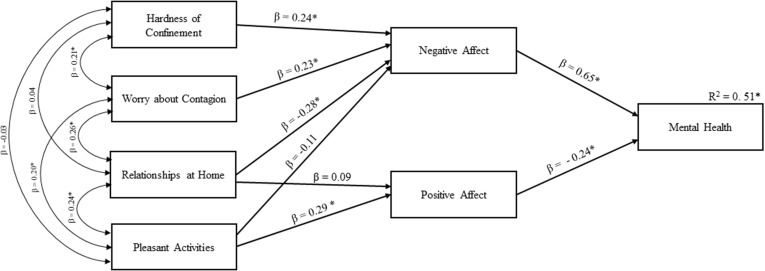
First, descriptive analyses of the variables under study were calculated. Second, comparison of means analyses were carried out using Student’s t-tests to assess possible gender differences. Third, Pearson’s correlations were conducted to examine associations between variables. Fourth, a stepwise multiple regression analysis was conducted to identify which of the studied variables were significant predictors of Mental health. Finally, we conducted a path analysis to test our hypothesis about whether the COVID-19 contextual variables (that is, risk and protective factors) are related to Mental health via the indirect effect of Positive Affect (PA) and Negative Affect (NA) (see Figure 1). This model included the risk factors of Hardness of confinement and Worrying about contagion and the protective factors of Relationships at home and Pleasant activities as exogenous variables, PA and NA as intervening variables, and Mental health as an endogenous variable. Only previous significant correlations were introduced as paths in the model.
Figure 1.
Representation of the path model including COVID-19 contextual variables as exogenous variables, PA and NA as intervening variables, and Mental Health as an endogenous variable. Standardized path coefficients (β) and explained variance (R2) are displayed. Asterisks indicate statistical significance at p < 0.05.
All analyses were carried out using the statistical package SPSS version 24.0 (IBM Corporation, Armonk NY, USA), setting an alpha significance level of 0.05. IBM AMOS 21.0 software was used to perform the path analysis and the bias-corrected bootstrapping method was used to estimate indirect effects (5000 samples, 95% CI).
Results
Table 1 provides descriptive statistics for each of the variables under study and the gender differences (t-Student). Compared to boys, girls showed significantly higher scores on Worrying about contagion (p = 0.02), NA (p < 0.001) and Mental health (higher scores on this subscale indicate poorer mental health) (p < 0.001). In contrast, boys scored significantly higher than girls on PA (p < 0.001). Cohen’s d for these gender differences ranged from 0.21 to 0.60, indicating that the effect sizes were small to medium (see Table 1).
Table 1.
Descriptive Statistics (Mean and Standard Deviation) for the Total Sample Divided by Gender, t-Tests (t-Value and Cohen’s d) for Gender Comparisons of COVID-19 Contextual Variables, Affect, and Mental Health
| Mean for the Total Sample (SD) | Mean for Boys (SD) | Mean for Girls (SD) | T-Test Between Genders | Cohen’s d | |
|---|---|---|---|---|---|
| Hardness of confinement | 4.35 (1.99) | 4.31 (1.96) | 4.39 (2.02) | −0.43 | 0.04 |
| Worrying about contagion | 5.93 (1.72) | 5.73 (1.93) | 6.09 (1.52) | −2.22* | 0.21 |
| Relationships at home | 5.61 (1.60) | 5.64 (1.61) | 5.58 (1.59) | 0.44 | 0.04 |
| Pleasant activities | 6.06 (1.45) | 6.10 (1.34) | 6.02 (1.52) | 0.62 | 0.06 |
| Positive affect | 3.03 (0.71) | 3.16 (0.68) | 2.93 (0.72) | 3.65** | 0.33 |
| Negative affect | 2.04 (0.66) | 1.89 (0.59) | 2.14 (0.69) | −4.18** | 0.39 |
| Mental health | 2.79 (0.97) | 2.48 (0.87) | 3.03 (0.97) | −6.43** | 0.60 |
Notes: p < 0.05*; p < 0.01**.
Pearson’s correlations between the variables under study are shown in Table 2. Mental health was positively related to Hardness of confinement (r = 0.32, p < 0.001), Worring about contagion (r = 0.15, p < 0.001) and NA (r = 0.67, p < 0.001), and negatively related to Relationships at home (r = −0.25, p < 0.001), Pleasant activities (r = −0.19, p < 0.001) and PA (r = -0. 30, p < 0.001). In addition, PA showed a positive relationship with Relationships at home (r = 0.16, p < 0.001) and Pleasant activities (r = 0.31, p < 0.001). In contrast, the NA subscale was positively related to Hardness of confinement (r = 0.28, p < 0.001) and Worrying about contagion (r = 0.18, p < 0.001), and negatively with Relationships at home (r = −0.24, p < 0.001) and Pleasant activities (r = −0.14, p < 0.001).
Table 2.
Pearson’s Correlation Between the Four COVID-19 Contextual Variables, Affect, and Mental Health
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Hardness of confinement | – | 0.21** | 0.04 | −0.03 | −0.07 | 0.28** | 0.32** |
| 2. Worrying about contagion | – | 0.26** | 0.20** | 0.04 | 0.18** | 0.15** | |
| 3. Relationships at home | – | 0.25** | 0.16** | −0.24** | −0.25** | ||
| 4. Pleasant activities | – | 0.31** | −0.14** | −0.19** | |||
| 5. Positive affect | – | −0.09 | −0.30** | ||||
| 6. Negative affect | – | 0.67** | |||||
| 7. Mental health | – |
Note: p < 0.01**.
A stepwise multiple regression analysis was conducted to establish the variables that best predicted Mental health (gender was also entered as a predictor). The results revealed that the final model accounted for 55% of the explained variance and included Hardness of confinement, Relationships at home, PA, NA, and gender as significant predictors of Mental health. Statistical details are shown in Table 3.
Table 3.
Summary of the Results for the Final Model Resulting from the Stepwise Regression Analysis
| Criterion | Predictors | B | Std. error | β | t | p |
|---|---|---|---|---|---|---|
| Mental health | Hardness of confinement | 0.07 | 0.02 | 0.15 | 4.56 | < 0.001 |
| Relationship at home | −0.05 | 0.02 | −0.08 | −2.55 | < 0.05 | |
| Positive affect | −0.28 | 0.04 | −0.20 | −6.43 | < 0.001 | |
| Negative affect | 0.83 | 0.05 | 0.57 | 16.74 | < 0.001 | |
| Gender | 0.27 | 0.06 | 0.14 | 4.31 | < 0.001 | |
| Constant | 1.49 | 0.23 | 6.57 | < 0.001 |
Note: R2 = 0.55, p < 0.001.
Finally, the path analysis that included the four COVID-19 contextual variables as exogenous variables, AN and AP as intervening variables, and Mental health as an endogenous variable revealed an optimal fit of the model (CFI = 0.97; GFI = 0.99; SRMR = 0.03) and explained 51% of the variance in Mental health. Only significant correlations were entered into the model. Figure 1 shows the diagram and results of the path model. On the one hand, the analysis revealed that Hardness of confinement and Worrying about contagion were indirectly and positively related to Mental health through NA (indirect effect of Hard confinement: = 0.07, 95% CI [0.047, 0.103]; indirect effect of Worrying about contagion = 0.08, 95% CI [0.053, 0.114]). On the other hand, Relationships at home and Pleasant activities revealed negative indirect effects on Mental health through NA (indirect effect of Relationships at home = −0.11, 95% CI [−0.148, −0.076]; indirect effect of Pleasant activities = −0.05, 95% CI [−0.088, −0.023]). Moreover, a positive indirect effect of Pleasant activities on Mental health through PA was also observed (indirect effect = −0.05, 95% CI [−0.068, −0.029]).
Discussion
This research aimed to develop an inclusive model of the risk and protective factors associated with adolescent mental health through the indirect effect of positive and negative affect. In this work, we bring together both perspectives since previous research on the impact of COVID-19 on adolescent mental health has focused on negative consequences2,3,44 rather than protective factors.17,39 We investigated contextual factors associated with confinement that can cause changes in mental health through affectivity (confinement hardness, worrying about contagion, relationships at home, and pleasant activities). Moreover, gender differences were analysed.
In relation to hypothesis 1 (H1), our findings revealed that adolescents who scored higher in perceived hardness of confinement and worrying about contagion scored higher in negative affect, but there was no change in positive affect. In other words, it appears that adolescents who found confinement harder and were more worried about getting infected experienced a greater degree of negative emotions. These results partially support this hypothesis, which aligns with various studies demonstrating that adolescents presented emotional alterations during confinement and displayed unpleasant emotions such as fear, worry, or stress.6,7,45,46 Furthermore, Nearchou et al,2 in a meta-analysis of young adults, discovered that emotional responses related to COVID-19, such as worry and fear of contracting the virus, were associated with depression and anxiety, both of which are mental health outcomes characterized by significant negative emotions.47
In contrast, regarding hypothesis 2 (H2), our results showed that adolescents who perceived a good quality of their relationships at home and engaged in enjoyable activities during lockdown scored higher in positive affect and lower in negative affect. This finding supports our second prediction. In the following paragraphs, we will further examine the alignment of our H2 results with the existing literature.
Concerning relationships at home, in line with our findings, previous research has shown that strong family dynamics play a pivotal role in helping individuals cope with challenging situations.26 For instance, during periods of confinement, a cohesive family environment acts as a protective factor against stress, loneliness, and depressive symptoms,29,48 while adolescents in less cohesive families tend to experience heightened feelings of isolation.30 Moreover, studies on confinement have also shown that family stress has worsened problems like gender-based violence, significantly affecting the mental health of family members.32,49,50
Regarding pleasant activities, it is now well known that engaging in pleasurable activities is a form of emotional regulation, which is related to higher levels of positive affect and lower levels of negative affect (eg, depressive symptoms).37,38 During confinement, it has been shown that engaging in these activities was associated with higher levels of affective and cognitive happiness.39 In contrast, the infrequent or absent engagement in these activities during this period has been linked to negative affect (eg, stress, anxiety, and depressive symptoms) among adolescents.8,45
Concerning hypothesis 3 (H3), our findings on mental health and affectivity align with prior research, which suggests that poorer mental health is associated with an increase in negative affect13–15 and a decrease in positive affect,12 as discussed in more detail below.
Regarding hypothesis 4 (H4), our primary focus was to propose an inclusive model of risk and protective factors through the indirect effect of positive and negative affect for understanding adolescents’ mental health during the lockdown period. In this model, we propose perceived hardness of confinement and worrying about contagion as risk factors. Conversely, positive relationships at home and engagement in pleasant activities are presented as protective factors. These factors have a differential impact on adolescents’ mental health through their indirect influence on affect—both positive and negative (see to Figure 1 for further clarification). Our results reveal that engagement in pleasant activities —understood as a protective factor— during confinement can act as a promoter of good mental health through its impact on positive affect. However, it seems that the absence (or low frequency) of these activities during confinement, together with the perceived hardness of confinement and worry about COVID-19 infection (self or family members) —understood as risk factors— may facilitate the emergence of mental health-related problems in adolescents through negative affect. These results partially confirm our H4 and are consistent with previous findings in adolescents. Previous studies have shown that greater engagement in pleasurable activities is related to greater positive affect and that positive affect, in turn, is related to increased mental health.38,51 In addition, previous literature shows how engaging in pleasurable activities can reduce depressive symptoms37 and is recommended in therapies for this disorder.52 In the same vein, confinement has also been shown to have direct negative effects on mental health.6,17,21,22,45 For example, fears —negative affect— related to COVID-19 predict anxiety, OCD symptoms and depression in adolescents.2 Furthermore, rigid rules of confinement have been related to post-traumatic symptomatology, avoidance behaviours and negative affect (such as anger and frustration), harming mental health.6,21,22
In relation to our exploratory analysis of gender, we found that girls showed significantly higher scores in worrying about contagion, negative affect, and mental health than boys. In contrast, boys scored significantly higher than girls on positive affect, differences that are consistent with most of the studies found in the literature. Pre-pandemic studies indicates that adolescent girls show higher levels of distress, such as stress and anxiety.53,54 One possible explanation is that the lockdown may have exacerbated pre-existing conditions and heightened levels of worry,55,56 as various investigations have shown a more pronounced impact of the pandemic on girls’ mental health compared to boys,57–59 even in the case of depressive disorders.3 The differences in positive and negative affect may also be explained by the fact that girls tend to respond more intensely to emotions related to aversion60 while boys tend to rank their emotional states more neutrally.61 Moreover, during the lockdown period, it appears that adolescent girls tend to use social media more and display higher levels of self-concern compared to boys, potentially leading to a greater impact on their well-being.45,62 Finally, when interpreting these differences, we must consider other potential contributing factors, such as biological factors and those associated with gender inequity (ie, a higher likelihood of experiencing interpersonal violence).63,64
Certain limitations of this work should be considered. First, this study adopted a cross-sectional design, which means that we cannot infer causality. Future studies should implement longitudinal designs to establish temporal relations. Second, all variables were measured using self-reports. It would thus be interesting for future research to obtain data from other informants, especially for mental health indicators. Third, due to COVID-19, adolescents completed the tests online, and unfortunately, we cannot ensure that these conditions did not lead to bias in the responses. Finally, the sample is all Spanish, which limits the generality of the results across cultures. Further investigations must either expand the sample or replicate the studies in other countries. Moreover, more research is needed on how the adolescent gender can influence psychological aspects in crisis situations.
Despite these limitations, this is the first study to provide evidence on how contextual variables of confinement affect adolescents’ mental health through affectivity. Our findings can have important practical implications for developing strategies to improve adolescents’ mental health, especially in situations with characteristics similar to confinement (eg, coping with imposed adverse conditions). Furthermore, our results support the notion that promoting participation in enjoyable activities among adolescents as a form of emotional regulation can help increase their positive affect, recognizing this as a potential strategy with evidence of enhancing adolescents’ well-being. Training in emotional regulation skills would allow attenuating the negative emotionality generated by certain adverse events (in this case, the fear of contagion and the perception of the hardness of the situation), while encouraging the generation of strategies aimed at increasing positive affectivity, such as participation in pleasurable activities.
Conclusion
This work provides a deeper understanding of the variables related to COVID-19 that could have a differential impact on adolescent mental health. These variables encompass the severity of confinement perceived, concerns about contagion, the quality of relationships at home, and engaging in enjoyable activities. We developed an inclusive risk and protective factors model that demonstrated the impact of these variables on adolescent mental health through the indirect effect of positive and negative affect. This theoretical framework can serve as a foundation for designing and implementing effective prevention and coping strategies for managing crises during this critical phase of life when adverse events can be particularly challenging.
Acknowledgments
This work has been supported by the collaboration of the University of Málaga, the Regional Ministry of Economy and Knowledge, Junta de Andalucía, by the Spanish Ministry of Economy, Industry and Competitiveness, and by the Spanish Ministry of Education and Vocational Training.
Funding Statement
This work was funded by the Regional Ministry of Economy and Knowledge, Junta de Andalucía (UMA18-FEDERJA-137) to Alberto Megías Robles and (UMA18-FEDERJA-114) to Rosario Cabello and Pablo Fernández Berrocal, and the Spanish Ministry of Education and Vocational Training (FPU18/00610 to María T. Sánchez López and FPU19/02042 to Desirée Llamas-Díaz).
Data Sharing Statement
Study data are available upon request from correspondence author Rosario Cabello (rcabello@uma.es).
Ethics Approval and Consent to Participate
High school students participated in the study with written informed consent from their parents/legal guardians. Participants were informed of the confidentiality and anonymity of their responses and all methods were performed in accordance with the Helsinki declaration.40 This study was approved by the Research Ethics Committee of the University of Málaga (approval number: 10-2019-H). Written informed consent was required from parents/legal guardians to participate in the study.
Disclosure
The authors declare that they have no conflict or competing interests.
References
- 1.Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218–1239.e3. doi: 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nearchou F, Hennessy E, Flinn C, Niland R, Subramaniam SS. Exploring the impact of covid-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health. 2020;17(22):1–19. doi: 10.3390/ijerph17228479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Santomauro DF, Herrera AMM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holmes EA, O’Connor RC, Perry VH, et al. Mental illness during COVID-19. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tan W, Hao F, McIntyre RS, et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. 2020;87:84–92. doi: 10.1016/j.bbi.2020.04.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hossain MM, Sultana A, Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Epidemiol Health. 2020;42:1–11. doi: 10.4178/epih.e2020038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viner R, Russell S, Saulle R, et al. School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the first COVID-19 wave: a systematic review. JAMA Pediatr. 2022:1–10. doi: 10.1001/jamapediatrics.2021.5840 [DOI] [PubMed] [Google Scholar]
- 9.Ma L, Mazidi M, Li K, et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021;293(June):78–89. doi: 10.1016/j.jad.2021.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Heal. 2020;4(6):421. doi: 10.1016/S2352-4642(20)30109-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Golberstein E, Gonzales G, Meara E. How do economic downturns affect the mental health of children? Evidence from the national health interview survey. JAMA Pediatr. 2019;28(8):955–970. doi: 10.1002/hec.3885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fredrickson BL, Losada MF. Positive affect and the complex dynamics of human flourishing. Am Psychol. 2005;60(7):678–686. doi: 10.1037/0003-066X.60.7.678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- 14.Sirgy MJ. Positive balance: a hierarchical perspective of positive mental health. Qual Life Res. 2019;28(7):1921–1930. doi: 10.1007/s11136-019-02145-5 [DOI] [PubMed] [Google Scholar]
- 15.Mor N, Doane LD, Adam EK, et al. Within-person variations in self-focused attention and negative affect in depression and anxiety: a diary study. Cogn Emot. 2010;24(1):48–62. doi: 10.1080/02699930802499715 [DOI] [Google Scholar]
- 16.Fernández-Abascal EG, Martín-Díaz MD. Longitudinal study on affect, psychological well-being, depression, mental and physical health, prior to and during the COVID-19 pandemic in Spain. Pers Individ Dif. 2021;172:1–10. doi: 10.1016/j.paid.2020.110591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muñoz-Navarro R, Cano Vindel A, Schmitz F, Cabello R, Fernández-Berrocal P. Emotional disorders during the COVID-19 Outbreak in Spain: the role of sociodemographic risk factors and cognitive emotion regulation strategies. Heal Educ Behav. 2021;48(4):412–423. doi: 10.1177/10901981211014101 [DOI] [PubMed] [Google Scholar]
- 18.Wang T, Chen P, Xiang J, et al. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;382(18):1708–1720. doi: 10.1056/NEJMc2001737.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghosh R, Dubey MJ, Chatterjee S, Dubey S. Impact of COVID-19 on children: special focus on the psychosocial aspect. Minerva Pediatr. 2020;72(3):226–235. doi: 10.23736/S0026-4946.20.05887-9 [DOI] [PubMed] [Google Scholar]
- 20.Liu S, Liu Y, Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: a cross-sectional survey. Psychiatry Res. 2020;289:113070. doi: 10.1016/j.psychres.2020.113070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fernández RS, Crivelli L, Guimet NM, Allegri RF, Pedreira ME. Psychological distress associated with COVID-19 quarantine: latent profile analysis, outcome prediction and mediation analysis. J Affect Disord. 2020;277(August):75–84. doi: 10.1016/j.jad.2020.07.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ben-Ezra M, Sun S, Hou WK, Goodwin R. The association of being in quarantine and related COVID-19 recommended and non-recommended behaviors with psychological distress in Chinese population. J Affect Disord. 2020;275:66–68. doi: 10.1016/j.jad.2020.06.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cutuli D. Cognitive reappraisal and expressive suppression strategies role in the emotion regulation: an overview on their modulatory effects and neural correlates. Front Syst Neurosci. 2014;8:1–6. doi: 10.3389/fnsys.2014.00175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoagwood KE, Cavaleri MA, Olin SS, et al. Family support in children’s mental health: a review and synthesis. Clin Child Fam Psychol Rev. 2010;13(1):1–45. doi: 10.1007/s10567-009-0060-5 [DOI] [PubMed] [Google Scholar]
- 25.Olson DH, Sprenkle DH, Russell CS. Circumplex model of marital and family system: i. Cohesion and adaptability dimensions, family types, and clinical applications. Fam Process. 1979;18:3–28. doi: 10.1111/j.1545-5300.1979.00003.x [DOI] [PubMed] [Google Scholar]
- 26.Skinner H, Steinhauer P, Sitarenios G. Family assessment measure (FAM) and process model of family functioning. J Fam Ther. 2000;22(2):190–210. doi: 10.1111/1467-6427.00146 [DOI] [Google Scholar]
- 27.Rask K, Åstedt-Kurki P, Paavilainen E, Laippala P. Adolescent subjective well-being and family dynamics. Scand J Caring Sci. 2003;17(2):129–138. doi: 10.1046/j.1471-6712.2003.00118.x [DOI] [PubMed] [Google Scholar]
- 28.Jiang SY, Liu RD, Jiang RH, Hong W, Jin FK. Family functioning and bullying victimization: effects of extraversion and problem behaviors. Chinese J Clin Psychol. 2018;26:1006–1010. doi: 10.16128/j.cnki.1005-3611 [DOI] [Google Scholar]
- 29.Mariani R, Renzi A, Di Trani M, Trabucchi G, Danskin K, Tambelli R. The impact of coping strategies and perceived family support on depressive and anxious symptomatology during the coronavirus pandemic (COVID-19) lockdown. Front Psychiatry. 2020;11:1–9. doi: 10.3389/fpsyt.2020.587724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ren ZX. Family cohesion and loneliness in college students: coping style’s mediating effect. China J Heal Psychol. 2020;28:1066–1070. doi: 10.13342/j.cnki.cjhp.2020.07.025 [DOI] [Google Scholar]
- 31.Santini ZI, Jose PE, York Cornwell E, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Heal. 2020;5(1):e62–e70. doi: 10.1016/S2468-2667(19)30230-0 [DOI] [PubMed] [Google Scholar]
- 32.Peterman A, Potts A, O’Donnell M, et al. Pandemics and Violence Against Women and Children. Washington DC: Center for Global Development; 2020. [Google Scholar]
- 33.Zhang H. The influence of the ongoing COVID-19 pandemic on family violence in China. J Fam Violence. 2020;1–11. doi: 10.1007/s10896-020-00196-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Campbell AM. An increasing risk of family violence during the Covid-19 pandemic: strengthening community collaborations to save lives. Forensic Sci Int Rep. 2020;2:1–3. doi: 10.1016/j.fsir.2020.100089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheldon KM, Lyubomirsky S. Revisiting the sustainable happiness model and pie chart: can happiness be successfully pursued? J Posit Psychol. 2021;16(2):145–154. doi: 10.1080/17439760.2019.1689421 [DOI] [Google Scholar]
- 36.Klug HJP, Maier GW. Linking goal progress and subjective well-being: a meta-analysis. J Happiness Stud. 2015;16(1):37–65. doi: 10.1007/s10902-013-9493-0 [DOI] [Google Scholar]
- 37.McRae K, Gross JJ. Supplemental material for emotion regulation. Emotion. 2020;20(1):1–9. doi: 10.1037/emo0000703.supp [DOI] [PubMed] [Google Scholar]
- 38.John OP, Gross JJ. Healthy and unhealthy emotion regulation: personality processes, individual differences, and life span development. J Pers. 2004;72(6):1301–1334. doi: 10.1111/j.1467-6494.2004.00298.x [DOI] [PubMed] [Google Scholar]
- 39.Gutiérrez-Cobo MJ, Megías-Robles A, Gómez-Leal R, Cabello R, Fernández-Berrocal P. Is it possible to be happy during the covid-19 lockdown? A longitudinal study of the role of emotional regulation strategies and pleasant activities in happiness. Int J Environ Res Public Health. 2021;18(6):1–11. doi: 10.3390/ijerph18063211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.World Medical Association. Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. Seoul: WMA; 2009. [Google Scholar]
- 41.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): i. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002 [DOI] [PubMed] [Google Scholar]
- 42.Alonso J, Prieto L, Ferrer M, et al. Testing the measurement properties of the Spanish version of the SF-36 Health Survey among male patients with chronic obstructive pulmonary disease. J Clin Epidemiol. 1998;51(11):1087–1094. doi: 10.1016/s0895-4356(98)00100-0 [DOI] [PubMed] [Google Scholar]
- 43.Sandín B, Chorot P, Lostao L, Joiner TE, Santed MA, Valiente RM. Escalas PANAS de afecto positivo y negativo: validación factorial y convergencia transcultural. Psicothema. 1999;11(1):37–51. [Google Scholar]
- 44.Thakur H, Stutts M, Choi JW, Temple JR, Cohen JR. Adolescent loneliness during the COVID-19 pandemic: the role of pre-pandemic risk factors. Child Indic Res. 2022;16:617–639. doi: 10.1007/s12187-022-09984-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pizarro-Ruiz JP, Ordóñez-Camblor N. Effects of Covid-19 confinement on the mental health of children and adolescents in Spain. Sci Rep. 2021;11(1):1–10. doi: 10.1038/s41598-021-91299-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Toscano C, Lopes P, Ramos C, Baptista J. Emotional and behavioral health among portuguese toddlers during the COVID-19 crisis: the impact of social isolation and caregiving distress. Child Indic Res. 2023;16(1):69–85. doi: 10.1007/s12187-022-09964-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Young KS, Sandman CF, Craske MG. Positive and negative emotion regulation in adolescence: links to anxiety and depression. Brain Sci. 2019;9(4):76. doi: 10.3390/brainsci9040076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ye B, Zeng Y, Im H, Liu M, Wang X, Yang Q. The relationship between fear of COVID-19 and online aggressive behavior: a moderated mediation model. Front Psychol. 2021;12(February):1–11. doi: 10.3389/fpsyg.2021.589615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xie X, Xue Q, Zhou Y, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020;174(9):898–900. doi: 10.1001/jamapediatrics.2020.1619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Asanjarani F, Kumar A, Kalani S. Student subjective wellbeing amidst the covid-19 pandemic in Iran: role of loneliness, resilience and parental involvement. Child Indic Res. 2023;16(1):53–67. doi: 10.1007/s12187-022-09963-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Headey B, Kelley J, Wearing A. Dimensions of mental health: life satisfaction, positive affect, anxiety and depression. Soc Indic Res. 1993;29(1):63–82. doi: 10.1007/BF01136197 [DOI] [Google Scholar]
- 52.Lewinsohn PM, Graf M. Pleasant activities and depression. J Consult Clin Psychol. 1973;41(2):261–268. doi: 10.1037/h0035142 [DOI] [PubMed] [Google Scholar]
- 53.Murray KM, Byrne DG, Rieger E. Investigating adolescent stress and body image. J Adolesc. 2011;34(2):269–278. doi: 10.1016/j.adolescence.2010.05.004 [DOI] [PubMed] [Google Scholar]
- 54.Sadler K, Vizard T, Ford T, et al. Mental health of children and young people in England, 2017; 2018.
- 55.de Los D VM, López-Aymes G, Ruvalcaba NA, et al. Emotions and reactions to the confinement by COVID-19 of children and adolescents with high abilities and community samples: a mixed methods research study. Front Psychol. 2020:11(November):1–14. doi: 10.3389/fpsyg.2020.585587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Russell BS, Hutchison M, Tambling R, Tomkunas AJ, Horton AL. Initial challenges of caregiving during COVID-19: caregiver burden, mental health, and the parent–child relationship. Child Psychiatry Hum Dev. 2020;51(5):671–682. doi: 10.1007/s10578-020-01037-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang C, Riyu P, Xiaoyang W, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Heal Med. 2021;26(1):13–22. doi: 10.1080/13548506.2020.1746817 [DOI] [PubMed] [Google Scholar]
- 59.Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sharp C, van Goozen S, Goodyer I. Children’s subjective emotional reactivity to affective pictures: gender differences and their antisocial correlates in an unselected sample of 7–11-year-olds. J Child Psychol Psychiatry Allied Discip. 2006;47(2):143–150. doi: 10.1111/j.1469-7610.2005.01464.x [DOI] [PubMed] [Google Scholar]
- 61.Mouw JM, Van Leijenhorst L, Saab N, Danel MS, van den Broek P. Contributions of emotion understanding to narrative comprehension in children and adults. Eur J Dev Psychol. 2019;16(1):66–81. doi: 10.1080/17405629.2017.1334548 [DOI] [Google Scholar]
- 62.Twenge JM, Martin GN. Gender differences in associations between digital media use and psychological well-being: evidence from three large datasets. J Adolesc. 2020;79(January):91–102. doi: 10.1016/j.adolescence.2019.12.018 [DOI] [PubMed] [Google Scholar]
- 63.Riecher-Rössler A. Sex and gender differences in mental disorders. Lancet Psychiatry. 2017;4(1):8–9. doi: 10.1016/S2215-0366(16)30348-0 [DOI] [PubMed] [Google Scholar]
- 64.Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175(11):1142–1150. doi: 10.1001/jamapediatrics.2021.2482 [DOI] [PMC free article] [PubMed] [Google Scholar]