By 2060, the number of adults aged 65 or older living in the USA is projected to reach 94.7 million and comprise almost one-quarter of the US population1. Older adults often live with conditions that affect their physical health, psychosocial well-being, cognition and ability to live independently, resulting in complex medical and social needs. Managing these needs requires a multidimensional, integrative approach that addresses not only medical factors but also psychosocial and community factors that affect health and well-being; however, the special training, techniques, tools and expertise to support such an approach are not available in many communities and healthcare settings.
A potential solution to addressing the complex health and well-being needs of older adults comes from artificial intelligence (AI), which is defined in this paper as the science of creating machines and technologies that can reason, learn, plan and make predictions in ways that could surpass human capabilities. In recent years, developments in AI and digital technologies have been working rapidly to profoundly revolutionize healthcare delivery. For example, machine learning can interpret data from wearable devices with sensors (such as smartwatches and smartphones) to monitor patient health and facilitate community care, as well as predict the likely outcome of a given intervention for a given patient2. Voice-based virtual assistants can help patients to implement treatment plans, improve medication adherence and reduce feelings of loneliness and social isolation. Computer vision algorithms enable inference of health conditions in older adults using diagnostic images such as those from computed tomography, magnetic resonance imaging, ultrasound and X-rays. These capabilities can empower patients to proactively take control of their healthcare, which can increase patient engagement, improve the patient experience and enhance well-being and health outcomes.
Barriers to AI use in healthcare for older adults
The path from laboratory demonstration to real-world products continues to challenge AI technologies, particularly when adapting technology to the needs of older adults – and especially those with Alzheimer’s disease and related dementias (AD/ADRD). In healthcare settings, barriers include persistent skepticism about the promised productivity and efficacy gains from AI technologies, concern about potential legal liability for healthcare systems that use these technologies3, inadequate engagement of older adults in the technology development stage and ethical concerns about potentially reinforcing health inequities4,5. Furthermore, older adults are likely to be concerned about the privacy and security of the data collected by these technologies3,6 or to experience cognitive deficits that call into question their ability to consent to having their data collected indefinitely.
The Artificial Intelligence and Technology Collaboratories for Aging Research program
To help to realize the potential of AI and novel technologies to improve the health and well-being of older adults, the National Institute on Aging (NIA) – part of the National Institutes of Health – funded four Artificial Intelligence and Technology Collaboratories (AITCs) and an AITC Coordinating Center in September 2021 (refs. 7,8). This a2 collective serves as a national resource to promote effective aging-focused interdisciplinary AI and technology approaches that help to maintain the independence of older Americans, including persons with dementia (Fig. 1). This is done primarily through an annual pilot award competition that funds investigators from across the country to develop AI tools and technologies that are relevant to improving the lives of older adults and their caregivers, with particular emphasis on advancing the science of care management and aging-in-place for vulnerable older adults or those with AD/ADRD who are receiving skilled home-and community-based services.
Fig.1 |. The AITC program.
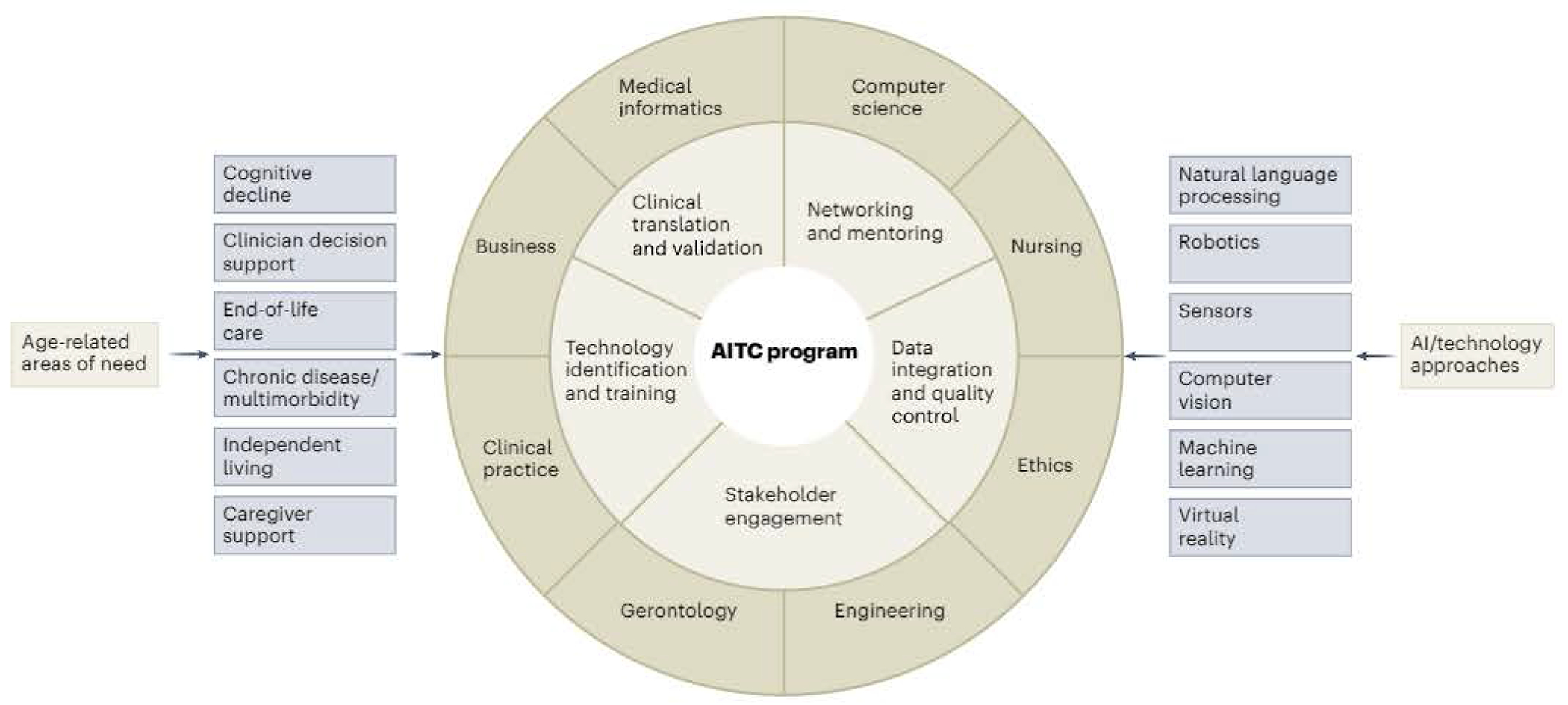
The AITC program connects the healthcare and social needs of older adults with AI and technology approaches that can be leveraged to improve targeted areas of health and well-being.
The NIA has committed US $65 million to funding the AITC program over a 5-year period, earmarking $40 million for technology demonstration projects. In addition to connecting pilot awardees with study sites, datasets and resources within the AITC ecosystem, the AITC program departs from typical NIA center programs in four notable ways: (1) annual pilot award competitions use a common application process adopted by all AITCs and welcome applicants nationally from both within and outside academia; (2) nondilutive pilot awards of up to $200,000 in direct costs are available, higher than the typical amounts offered by other NIA center programs; (3) the program’s coordinating center is not embedded in an academic institution but is instead managed by a small business that can nimbly bridge the worlds of academia, healthcare, venture capital, industry and government; and (4) application solicitation includes proactive engagement with ‘AgeTech’ organizations, investors, incubators, accelerators and startup veterans.
a2 pilot awards competition
The AITC pilot funding program invites applicants to submit applications to develop novel technologies with the potential to improve quality of life and health outcomes for older adults, including individuals with AD/ADRD, and their caregivers. In our first a2 pilot awards competition, the a2 collective received 280 applications, of which approximately two thirds (66%) were focused on AD/ADRD. The vast majority (84%) of applicants were not originally affiliated with any AITC, and about half of the applicants (51%) were from non-academic institutions. The AITCs prioritized projects that sought to develop and deploy innovative technologies to support successful aging and AD/ADRD care at home. A total of 33 projects from the first competition were awarded, of which 44% were led by women. Technologies supported in the first cohort of pilot awards include virtual reality to facilitate social engagement, AI-assisted chat devices to assist caregivers, robotic assistants to calm bouts of dementia-induced aggression in residential centers, home-based movement sensors to predict cognitive decline and wearable devices embedded in earbuds to monitor heart health.
Future pilot technologies could measure activities of daily living, such as grooming; interactions with home infrastructure, indicated by utility use; health indicators, such as vital signs; financial behavior; and psychosocial behavior, including speech patterns and language use. Specific technologies could include sensors, wearables, smart devices such as mobile phones, hardware for telemedicine, robotic devices such as artificial pets and dolls or those to assist with daily living, and chatbots to provide social and informational interaction. Applications to develop AI-based data analysis methods for automated machine learning and clinical decision support are also of interest. The a2 collective will accept applications for the third annual a2 pilot awards competition from 1 May to 31 July 2023. Prospective applicants can access competition information and apply online.
Conclusions
AI and other novel technologies offer promising approaches to mitigate many of the health problems associated with aging, including platforms that offer precision medicine interventions to improve health while minimizing adverse effects. These technologies also support living safely in the community and combat social isolation. The AITC program is part of a growing ecosystem of major initiatives in AI that can accelerate developments to help older adults to lead more independent lives and improve the quality of their care. With transformational research such as that led by the NIA AITCs and incentives for the commercialization of approaches that research shows to be effective, the promise of these technologies to improve the health and quality of life of older adults can be realized.
Acknowledgements
We thank D. Berlyne, C. Garcia, K. Goggans and K. Harr for editorial assistance with the manuscript, and J. Fairman for producing the original figure illustration. This work was supported by grants P30AG073104 (R.C., P.M.A. and J.D.W.), P30AG073107 (N.C. and D.G.); P30AG073105 (G.D., J.K. and J.H.M.), and U24AG073094 (R.M.L.) from the National Institute on Aging, part of the National Institutes of Health.
Directors & Advisors of the AITCs
Peter M. Abadir12, Rama Chellappa12, Niteesh Choudhry34, George Demiris56, Deepak Ganesan7, Jason Karlawish6, Benjamin Marlin7, Rose M. Li8, Najim Dehak2, Alicia I. Arbaje1, Mathias Unberath2, Thomas K. M. Cudjoe1, Suchi Saria2, Esther Oh1, Nancy Lundebjerg10, Christopher G. Chute1, Jason H. Moore9, Phillip Phan1Quincy Samus1, Nancy L. Schoenborn1 & Jeremy D. Walston1
10 American Geriatrics Society.
11 Johns Hopkins Carey Business School, Johns Hopkins University, Baltimore, MD, USA.
Footnotes
Competing interests
The authors declare no competing interests.
References
- 1.Vespa J, Medina L & Armstrong DM Current Population Reports, P25-1144 (US Census Bureau, 2020). [Google Scholar]
- 2.Davenport T & Kalakota R Future Healthc. J 6, 94–98 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh RP, Hom GL, Abramoff MD, Campbell JP & Chiang MF Transl. Vis. Sci. Technol 9, 45 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Char DS, Shah NH & Magnus D N. Engl. J. Med 378. 981–983 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wangmo T, Lipps M, Kressig RW & lenca M BMC Med. Ethics 20, 98 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chu CH et al. Gerontologist 62, 947–955 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NIH. Artificial Intelligence and Technology Collaboratories for Aging Research (P30 – Clinical Trial Optional) (RFA-AG-21-009). grants.nih.gov. https://grants.nih.gov/grants/guide/rfa-files/rfa-ag-21-009.html (2020).
- 8.NIH. Artificial Intelligence and Technology Collaboratories for Aging Research Coordinating Center (AITCC) (R24 Clinical Trial Not Allowed) (RFA-AG-21-018). grants.nih.gov. https://grants.nih.gov/grants/guide/rfa-files/RFA-AG-21-018.html (2020).


