Abstract
Objective
We designed a Patient and Family Participation Education Program (PFEP) with the aim of fostering a positive attitude and enhancing the competencies of hospital nurses required for effective patient and family participation in care.
Methods
In a Dutch university hospital, we conducted a before-after study. The PFEP comprising three courses: family conversation, supporting shared decision-making, and health literacy. We assessed nursing attitudes using the FINC-NA questionnaire and competencies with a separate questionnaire before and three months after the program. Changes in attitudes and competencies were analyzed using regression analysis.
Results
Twenty-two nurses participated in the education group, and 58 participated as controls.
After three months, the change scores for the education group were statistically significantly higher on the total attitude score (FINC-NA) compared to the control group. Moreover, in six out of twelve competencies, the education group demonstrated significantly higher scores than the control group.
Conclusion
The educational program appeared effective in promoting nurses' attitudes and feelings of competencies towards patient and family-centered care.
Innovation
A blended education program focusing on patient and family has potential value for implementation in hospital care settings, especially for hospitals aiming to cultivate a more patient- and family-centered environment.
Keywords: Patient family centered care, Education program, Family conversation, Shared decision making, Health literacy
Highlights
-
•
A Education Program was developed comprising three courses: family conversation, shared decision making, and health literacy.
-
•
The educational program effectively promoted nurses' attitudes and feelings of competencies towards patient- and family-centered care.
-
•
For nurses it remains difficult to practice this acquired attitude and competencies.
1. Introduction
Patient Family Centered Care (PFCC) is a central tenet for healthcare quality nowadays and is considered a crucial part of healthcare [1]. The Institute for Patient- and Family-Centered Care (IPFCC) defines PFCC as ‘mutually beneficial partnerships between healthcare providers, patients, and families in healthcare planning, delivery, and evaluation of care’ [2]. PFCC emphasized four core values, i.e. dignity and respect, information sharing, participation, and collaboration with patients and families [3]. These values challenge nurses in general to consider families as integral members of the healthcare team and to extend the care to patients in relation with their families [4]. Moreover, patient and family participation has positive effects in reducing family members' stress, anxiety, and depression, while also potentially enhancing satisfaction and fostering improved relationships with healthcare practitioners [5].
Despite the growing body of evidence that PFCC also directly impacts clinical outcomes, such as better compliance with medication regimes, fewer complications, and lower stress and anxiety levels [5,6], the implementation of PFCC in hospitals is still hampered [[7], [8], [9], [10], [11]]. Frequently reported reasons are ambiguous feelings and lack of competence in applying PFCC in daily hospital practice [6,8,9]. Especially the attitude of nurses is considered an important prerequisite for inviting and engaging families and for implementing PFCC [9,12].
To improve nurses' attitudes and competencies different PFCC educational programs have been developed [[13], [14], [15]]. These studies report on PFCC education programs in specialized surroundings, such as the intensive care unit, pediatric wards, and adult palliative wards, making the transferability of the results to general nursing wards problematic. Evaluations of these programs showed increased knowledge and skills among nurses [[13], [14], [15]]. However, the transferability of these results is limited due to different settings and low robust research designs. As PFCC educational programs have the potential to influence nurses' attitude and competencies positively, we developed a Patient and Family Participation Education Program (PFEP) for general hospital wards. We hypothesized that this program affects nurses' attitudes and competencies towards patient and family participation, resulting in a feeling of readiness to put PFCC into practice.
Therefore, we executed a study to assess:
-
(1)
the effect of an educational program on nurses' attitudes and competencies towards patient and family participation, and.
-
(2)
how nurses used the acquired competencies and changed attitudes towards patient and family participation into practice.
2. Methods
2.1. Study design
We used a controlled before-after design in which the participants completed questionnaires at different times. Additional interviews were executed to explore how nurses put the competencies and attitudes into practice after participation in the education program. This study was executed between June 2021 and June 2022.
2.2. Participants and setting
The study occurred in Amsterdam University Medical Centers (Amsterdam UMC), the Netherlands. Amsterdam UMC provides highly specialized care to patients of all ages. PFCC was officially incorporated into the hospital's mission statement in 2019. Focus groups with nurses and patients guided the implementation of this statement into practice. Adequate training in PFCC was considered essential, which resulted in the developing of this PFEP.
2.3. Sample size
We aimed to recruit 30 registered nurses working on different general wards to join the PFEP. All nurses must be registered in a mandatory national register for healthcare professionals as per the Individual Healthcare Professions Act (so-called BIG-register). Nurses who followed the educational program formed the education group. From the same wards, 60 registered nurses who did not participate in the PFEP were recruited as controls (control group). All participants were recruited through self-selection. After finishing the educational program and the quantitative data collection, we selected randomly participants for a qualitative evaluation.
2.4. Educational program
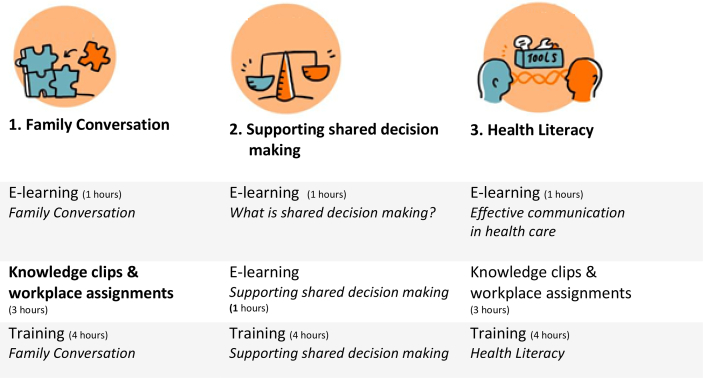
The PFEP was designed as a blended program, including individual e-learnings, workplace assignments, and group sessions with a trainer and an actor (see Fig. 1). Participation was on a voluntary basis. Based on the mission statement and the aforementioned focus groups, an educational program was developed with three courses. The program includes the courses: (1) family conversation, (2) supporting shared decision making, and (3) health literacy. The underlying theoretical framework of the course family conversation is the family nursing conversation (FNC) intervention, adapted by Broekema and colleagues [11]. The Family Nursing Conversation is structured into four stages and consists of twelve components that can be applied to both outlining and structuring the family conversation. The course supporting shared decision making is based on findings and theory of Bos et al. [16]. There are three elements to support nurses in their efforts to engage patients and families in the shared decision-making process: (a) checking the quality of a decision, (b) complementing shared decision making and (c) facilitating shared decision-making. The course health literacy focused on specific communication skills, such as the teach-back method, using graphics and pictures to support patients and family members in managing their health literacy [17].
Fig. 1.
Outline of the educational program.
2.5. Nurses' attitude and competencies (Quantitative data)
First, we collected demographic and professional data such as age, gender, highest level of education, number of years of work experience, and setting. Furthermore, we asked the participants for an overall score on their attitude to families participating and collaborating in patient care on a scale 0–10; a higher score represents a more positive attitude. Nurses' attitudes and competencies were measured through two self-report questionnaires.
The Family Importance in Nurses Care – Nurses' Attitudes (FINC-NA) was used to explore nurses' attitudes regarding the importance of families in nursing care. FINC-NA is a 26-item questionnaire with a five-point Likert response scale ranging from 1 = totally disagree to 5 = totally agree [18]. Total scores range from 26 to 130, with higher scores indicating a more supportive attitude towards families. The FINC-NA yields four dimensions with the following labels: “family as a resource in nursing care” (Fam-RNC, 10-items); “family as a conversational partner” (Fam-CP, 8-items); “family as a burden” (Fam—B, 4-items); and “family as its own resource” (Fam-OR, 4-items) [19]. The FINC-NA was translated using the bidirectional translation method for linguistic–cultural adaptation, validated, and showed good psychometric properties in previous research [19].
A second questionnaire was used to measure twelve self-perceived competencies of nurses. This questionnaire is based on the competencies considered for initiating family participation in nursing care described by Hengeveld et al. [20]. In this research 72 competencies were distilled from the literature and ranked by 69 international experts in the field of family participation. All competencies were sorted based on mean scores. The competencies with a mean score > 7.00 were included in the questionnaire of our study. This resulted in a 12-item questionnaire with a five-point Likert response scale from 1 = totally disagree to 5 = totally agree.
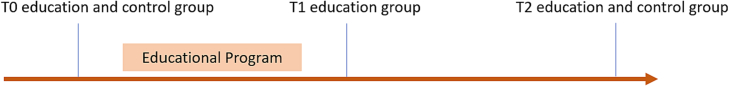
We asked the participants of the PFEP to fill out the questionnaires at three time points in order to explore changes over time: before the educational program (T0) to measure nurses' baseline attitudes and competencies, and one week (T1) and three months after completing the education program (T2). The controls filled out the questionnaires at T0 and T2. See Fig. 2. Data were collected through an online survey tool (Castor EU HQ, Amsterdam, the Netherlands). Reminders for each time point were sent twice via e-mail with one week in between. The items of the FINC-NA and the competencies were mandatory to ensure no missing values on these questionnaires.
Fig. 2.
Controlled before-after design.
2.6. Statistical analyses (Quantitative data)
Descriptive statistics were used to present the demographic and professional characteristics of the participants. Continuous data are presented as mean and standard deviation (SD) or median and interquartile range (IQR) depending on the normality of distribution. Categorical data are expressed as numbers and percentages (%). Differences in characteristics between the education and control group were determined by Student t-test, Mann-Whitney U test, Fisher exact test or Chi-square test when appropriate. We calculated change scores per item on both questionnaires between T0 and T2. Multivariable linear regression techniques were used to explore differences in change scores between the education and control group after correcting for baseline differences between the education and control group. To explore differences in attitude and competencies over time repeated measure ANOVA was used. A p-value of <0.05 was considered statistically significant. All analyses were performed using SPSS version 28.
2.7. Nurses' experiences (Qualitative evaluation)
We conducted a short qualitative evaluation to explore the participants' experiences with the educational program four months after finishing the program, and to provide additional context to the quantitative data. Therefore, four semi-structured interviews were executed with randomly selected nurses who were willing to share their experiences. Based on the preliminary and specifically the outspoken results of the surveys a fixed topic list was created for this evaluation. The main topics during the interview were about the sense of the attitudes and competencies and the implementation of what was learned in practice. The interviews were executed by one of the researchers with experience in qualitative research (PvO), audiotaped and transcribed verbatim. Two researchers (PvO, JMM) independently read iteratively the transcripts in order to identify recurrent issues. The results of the two researchers were compared and discussed.
2.8. Ethical considerations
The Institutional Review Board of the Amsterdam UMC, location AMC decided that ethical approval of this study was not required according to the Medical Research Involving Human Subjects Act (W21_137). Participants were informed about the study and were ensured the anonymity of the data. We asked all participants for informed consent at the start of the first questionnaire and before starting the interview. All data were stored in a secure place on the hospital server and analyzed and reported anonymously.
3. Results
3.1. Characteristics of participants
In total, 30 nurses participated in the educational program, of whom 26 (87%) completed the program and 22 (73%) completed all three surveys. Four nurses dropped out early due to the workload on the COVID-19 wards. In the control group, 60 participants were recruited, and 58 participants (97%) completed the two surveys. The median age of the participants was 28 years (IQR 25–39.5). Most nurses (86.2%) were educated at the bachelor's level or higher. The self-reported score on attitude towards family participation was 8 (IQR 7–9). The two groups differed in working hours, with 50% working >32 hours a week in the control group versus 27.3% in the education group. Also, in the education group, 81.8% of the participants had a personal experience with illness in the family versus 53.4% in the control group. The characteristics of the participants are presented in Table 1.
Table 1.
Demographic and professional characteristics of the respondents at baseline.
| Total (n = 80) | Education (n = 22) | Control (n = 58) | p-value | |
|---|---|---|---|---|
| Age, median (IQR) | 28 (25–39.25) | 29 (26–51) | 28 (24–36.25) | 0.171 |
| Gender, number (%) | 0.322 | |||
| Female | 75 (93.8%) | 22 (100%) | 53 (91.4%) | |
| Male | 5 (6.2%) | – | 5 (8.6%) | |
| Work experience, number (%) | 0.663 | |||
| <2 years | 15 (18.8%) | 3 (13.6%) | 12 (20.7%) | |
| 2–5 years | 28 (35.0%) | 7 (31.8%) | 21 (36.2%) | |
| 6–10 years | 8 (10.0%) | 3 (13.6%) | 5 (8.6%) | |
| 11–15 years | 7 (8.8%) | 1 (4.5%) | 6 (10.3%) | |
| >15 years | 22 (27.5%) | 8 (36.4%) | 14 (24.1%) | |
| Educational level, number (%) | 0.123 | |||
| <Bachelor | 11 (13.8%) | 5 (22.7%) | 6 (10.3%) | |
| Bachelor | 55 (68.8%) | 11 (50.0%) | 44 (75.9%) | |
| Bachelor plusa | 10 (12.5%) | 5 (22.7%) | 5 (8.6%) | |
| Master degree | 4 (5.0%) | 1 (4.5%) | 3 (5.2%) | |
| Working hrs/week, number (%) | 0.033 | |||
| <24 h | 10 (12.5%) | 6 (27.3%) | 4 (6.9%) | |
| 25–32 h | 35 (43.8%) | 10 (45.5%) | 25 (43.1%) | |
| >32 h | 35 (43.8%) | 6 (27.3%) | 29 (50.0%) | |
| Attitude towards family participationb, median (IQR) | 8 (7–9) | 8 (7–9) | 8 (7.75–9) | 0.711 |
| Personal experience with illness in the family, number (%) | 0.032 | |||
| Yes | 49 (61.3%) | 18 (81.8%) | 31 (53.4%) | |
| No | 31 (38.8%) | 4 (18.2%) | 27 (46.6%) |
Bachelor with an additional specialization, e.g. pediatric nursing, oncology nursing.
Self perceived attitude on a scale from 0 (negative) to 10 (positive).
Mann-Whitney U test.
Fisher exact test.
Chi square test.
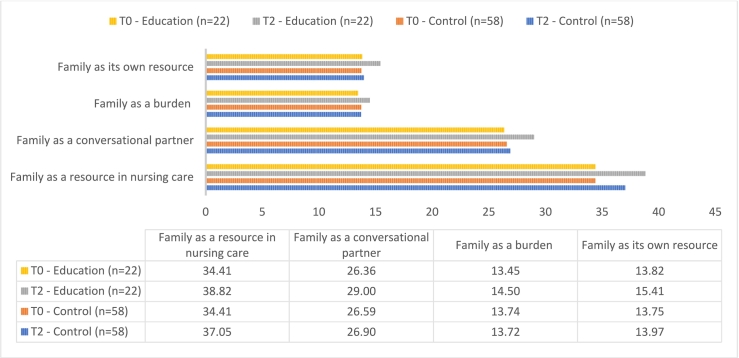
3.2. Nurses' attitude
The absolute difference in scores on the FINC-NA was higher between T0 and T2 in the education group than in the control group. The mean differences in the education group increased on all four subdomains of the FINC-NA, with a mean increase of the total FINC-NA score of 6.27 after three months. After correction for baseline differences, the differences in change scores between the two groups were statistically significant in the total FINC-NA score (p = 0.005), as well as in the dimensions FAM-CP (p = 0.01) and FAM-OR (p = 0.02), See Fig. 3 and Table 2.
Fig. 3.
Means in nurses' attitude between education group and control group before (T0) and after three months (T2).
Table 2.
Mean differences in attitude between the education group and control group at T0 and T2.
| Dimension (Score range) | Education (n = 22) | Control (n = 58) | ß | SE | p-value |
|---|---|---|---|---|---|
| Family as its own resource (4–20) | 1.05 | −0.02 | 1.32 | 0.57 | 0.02 |
| Family as a burden (4–20) | 1.59 | 0.21 | 0.94 | 0.50 | 0.06 |
| Family as a conversational partner (8–40) | 2.64 | 0.31 | 2.58 | 1.03 | 0.01 |
| Family as a resource in nursing care (10–50) | 4.41 | 2.64 | 1.91 | 0.99 | 0.06 |
| TOTAL FINC-NA (26–130) | 6.27 | −0.09 | 6.60 | 2.28 | 0.005 |
Note: corrected for baseline differences working hours/week and personal experience.
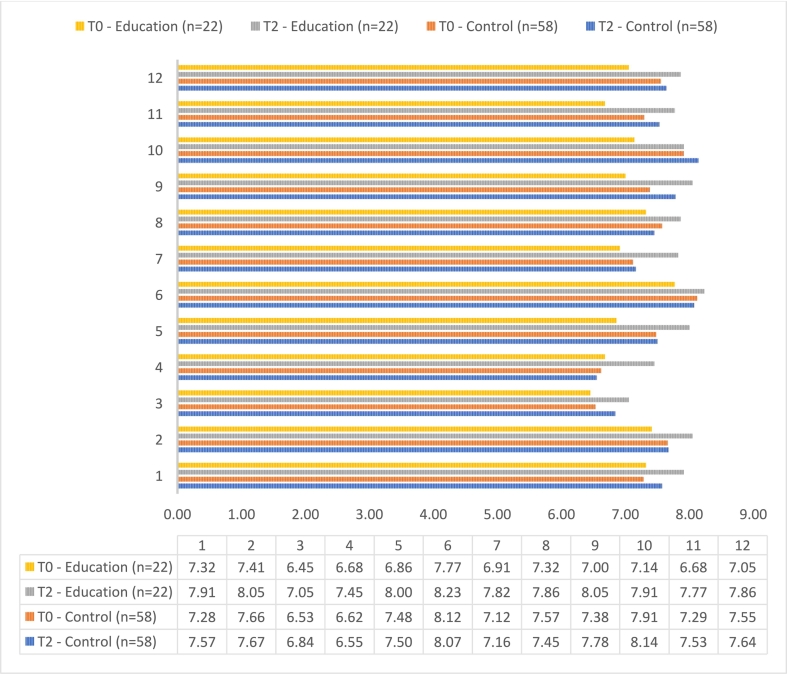
3.3. Nurses` competencies
Regarding the self-assessed competence level, the control group had higher scores on competence levels than the education group at baseline (T0). However, nurses in the education group scored higher overall than the control group after three months (T2). They had a larger absolute difference between T0 and T2 than the control group. After correction for baseline differences, the education group demonstrated a statistically significant higher rate of feeling competent on six of the twelve competencies compared with the control group after three months. See Fig. 4 and Table 3.
Fig. 4.
Means in competencies between the education and control group before (T0) and after three months (T2).
Table 3.
Mean differences in competencies between the education group and control group at T0 and T2.⁎
| Education (n = 22) | Control (n = 58) | ß | SE | p-value | |
|---|---|---|---|---|---|
| 1. I feel able to provide appropriate and timely information to patients and family members to facilitate understanding and support informed decison making. | 0.59 | 0.29 | 0.44 | 0.39 | 0.27 |
| 2. I feel able to identify and respond to the needs of patients and family members. | 0.64 | 0.17 | 0.72 | 0.32 | 0.03 |
| 3. I feel able to prioritize goals to achieve the outcomes deemed most important by patients and family members. | 0.59 | 0.31 | 0.28 | 0.43 | 0.51 |
| 4. I feel able to acknowledge patients and family members as the source of control, and full partner in providing care based on respect for patients' preferences, values, needs and family members' expertise. | 0.77 | −0.07 | 0.95 | 0.45 | 0.04 |
| 5. I feel able to support patients and family members to participate in decision making regarding care, at the level with which they are comfortable. | 1.14 | 0.02 | 0.98 | 0.35 | 0.006 |
| 6. I feel able to communicate in an honest, compassionate, non-judgmental and calm manner to family members. | 0.45 | −0.05 | 0.51 | 0.33 | 0.12 |
| 7. I feel able to promote, guide and monitor active participation of family members in care for patients in accordance with preferences of patients and family members. | 0.91 | 0.03 | 0.94 | 0.43 | 0.03 |
| 8. I feel able to enhance or reinforce the patients' and family members' senses of autonomy and self-determination through education and support. | 0.55 | −0.12 | 0.64 | 0.36 | 0.08 |
| 9. I feel able to provide coherent and congruent information in easily understood language to keep the family members informed about diagnoses, treatments, progress, prognosis and transfers. | 1.05 | 0.40 | 0.82 | 0.37 | 0.03 |
| 10. I feel able to collaborate with all members of the healthcare team to facilitate the provision of physical and emotional care support to patients and family members. | 0.77 | 0.22 | 0.64 | 0.38 | 0.10 |
| 11. I feel able to assess family members' preferred level of participation and role in decision making. | 1.09 | 0.24 | 0.84 | 0.41 | 0.04 |
| 12. I feel able to promote family presence in accordance with patient's preferences. | 0.81 | 0.09 | 0.76 | 0.38 | 0.05 |
Note: corrected for baseline differences, namely working hours per week and personal experience.
Repeated measures ANOVA.
3.4. Attitude and competencies over time
Quantitative data examined how nurses developed their attitude and competencies over time
(Table 4). Three months after completing the educational program, there was a significant improvement in two out of the four attitudes domains of the FINC-NA, and eight out of the twelve competencies. On all four subdomains of the FINC-NA the mean differences increased over time. The differences in change scores were statistically significant in the dimension Family as a conversational partner (p = 0.02) and Family as its own resource (p = 0.002). Of the eight competencies which were statistically significant, the mean differences of seven of these competencies increased over time (T0, T1 and T2). Except for the competency; I feel able to prioritize goals to achieve the outcomes deemed most important by patients and family members. The mean difference of this competencies decreased between T1 and T2.
Table 4.
Results of the learned attitude and competencies over time (T0, T1 and T2).⁎
| T0 (n = 22) |
T1 (n = 22) |
T2 (n = 22) |
p-value | |
|---|---|---|---|---|
| A1. Family as a resource in nursing care | 34.41 (3.50) | 39.45 (3.86) | 38.82 (4.63) | 0.89 |
| A2.Family as a conversational partner | 26.36 (3.95) | 28.64 (2.90) | 29.00 (3.64) | 0.02 |
| A3. Family as a burden | 13.45 (2.30) | 14.64 (2.44) | 14.50 (2.18) | 0.35 |
| A4. Family as its own resource | 13.82 (1.92) | 15.23 (1.38) | 15.41 (1.84) | 0.002 |
| C1. I feel able to provide appropriate and timely information to patients and family members to facilitate understanding and support informed decision making. | 7.32 (1.36) | 7.68 (0.78) | 7.91 (0.61) | 0.05 |
| C2. I feel able to identify and respond to the needs of patients and family members. | 7.41 (1.09) | 8.00 (0.87) | 8.05 (0.84) | 0.27 |
| C3. I feel able to prioritize goals to achieve the outcomes deemed most important by patients and family members. | 6.45 (1.26) | 7.50 (1.06) | 7.05 (1.25) | 0.01 |
| C4. I feel able to acknowledge patients and family members as the source of control, and full partner in providing care based on respect for patients' preferences, values, needs and family members' expertise. | 6.68 (1.36) | 7.09 (1.07) | 7.45 (0.91) | 0.02 |
| C5. I feel able to support patients and family members to participate in decision making regarding care, at the level with which they are comfortable. | 6.86 (1.04) | 7.77 (0.61) | 8.00 (0.76) |
0.03 |
| C6. I feel able to communicate in an honest, compassionate, non-judgmental and calm manner to family members. | 7.77 (1.07) | 8.09 (0.97) | 8.23 (0.92) |
0.02 |
| C7. I feel able to promote, guide and monitor active participation of family members in care for patients in accordance with preferences of patients and family members. | 6.91 (1.48) | 7.59 (0.96) | 7.82 (0.85) | 0.01 |
| C8. I feel able to enhance or reinforce the patients' and family members' senses of autonomy and self-determination through education and support. | 7.32 (1.00) | 7.77 (0.75) | 7.86 (0.71) | 0.06 |
| C9. I feel able to provide coherent and congruent information in easily understood language to keep the family members informed about diagnoses, treatments, progress, prognosis and transfers. | 7.00 (1.02) | 7.45 (1.14) | 8.05 (0.72) | 0.24 |
| C10. I feel able to collaborate with all members of the healthcare team to facilitate the provision of physical and emotional care support to patients and family members. | 7.14 (1.25) | 7.86 (0.64) | 7.91 (0.97) | 0.005 |
| C11. I feel able to assess family members' preferred level of participation and role in decision making. | 6.68 (1.62) | 7.64 (0.85) | 7.77 (0.97) | 0.006 |
| C12. I feel able to promote family presence in accordance with patient's preferences. | 7.05 (1.65) | 7.64 (0.90) | 7.86 (0.71) | 0.03 |
Repeated measures ANOVA.
3.5. Qualitative evaluation (context)
Based on four interviews, we identified the following (recurrent) issues: nurses experienced that family can be an important source of information. However, it takes time and patience as a healthcare professional to experience the benefits of family presence. Because the time investment is an issue, nurses believes the team must support and practice family involvement to ensure continuity. One nurse mentioned that she involved a family in care, but it stopped when she left.
Furthermore, a nurse reported that they are more consciously asking about the needs of patients and their families. Enquiries are made of patients' and family members' expectations.
However, in daily practice family involvement is limited to informing patients and family members and in the end nurses and doctors often determine what will happen.
One nurse mentioned that it appears difficult to bring the different perspectives of patients, family and healthcare professionals together as standard care. For example, conversations are often held when not everyone is present. This can cause confusion for the patient and family. It should be organized so that everyone is present at each of these conversations. Furthermore, nurses are aware of how they can be more responsive to patients and the family. But in the daily practice, it is not executed due to different organizational factors.
4. Discussion and conclusion
4.1. Discussion
This study aimed to evaluate the effect of a Patient and Family Participation Education Program on nurses' attitude and feelings of competence towards patient and family participation and to explore if they could bring the new knowledge and skills into practice. Our results show an improved attitude of nurses towards patient and family participation three months after participation in the educational program, compared to a control group. Also, compared to controls, nurses feel more competent on six out of twelve competencies after the education program. In addition, the impact of this education program on daily practice seems to be influenced by team and organizational factors.
Our results are congruent with previous studies in which other educational programs also demonstrated a significant effect on knowledge and skills regarding the participation of family members and patients [15,21,22]. However, these studies are executed on specific care units such as the neonatology. Our results show an improved effect on a heterogeneous group of nurses working on different wards in an academic hospital. The confirmation by our results strengthens the evidence that an educational program can improve attitude and competencies. In addition, our study expands this knowledge by qualitative information showing the difficulties nurse face to integrating PFCC into daily practice, despite the improved attitude and competencies. This phenomenon was reported previously by Younas et al., who reported that students can acquire competencies, but the adaptation of the competencies into practice, e.g. by the translation into explicit tasks, seemed difficult [22]. Furthermore, Shamali et al. conducted a large international study among nurses' attitudes regarding family involvement. They also used the FINC-NA questionnaire, and found that, among other factors, having a strategy for family care in the workplace is associated with a more favorable attitude towards family involvement. The PFEP can be an integral component of such a strategy [23].
Based on the qualitative evaluation, the impact of an educational program on clinical practice seems to be affected by team and organizational factors. Previous studies support these findings [10,[24], [25], [26], [27]]. It is suggested that a shift in behavioural change is not only reached by a shift in attitudes and competencies, but also by contextual factors essential to enable individual behaviour [25]. Organizational factors, such as staff organization, culture and resources, affect promoting and sustaining patient and family participation [10,26]. McCabe showed when an educational program, such as the Patient and Family Participation Education Program, takes place in an environment where skills and attitudes are embraced, it can change clinical practice immediately [26]. Furthermore, an organizational context with inclusion and support will help healthcare professionals to enable a practice change towards patient and family participation [27]. These findings suggest that only an educational program is not sufficient to make the change in practice, it should also requires team interventions [24,28]. Future research is needed to explore the additional value of team interventions to improve the impact of an interdisciplinary educational program.
However, this PFEP holds potential value for implementation in hospital care settings, especially in hospitals aiming to foster a more patient and family centered care environment. It is worth considering that nurses who proactively enroll in this program may already possess a positive attitude towards patient and family centered care. This could potentially result in a ceiling effect in their responses at baseline. Nonetheless, the program still appears to positively influence their attitudes, suggesting that it may have also an effect on nurses with less favorable initial perspectives on patient and family centered care. Notably, the control group in our study scored higher on the competencies than the educational group at baseline. This may be explained by the fact that the control group overestimated their competencies, which can be explained by Dunning-Kruger effect. This means that people who are unskilled do not have the metacognitive ability to realize their incompetence, resulting in an overestimation of their skills [29]. Future research should focus on the effect of a PFEP on the entire nursing team. It might also be necessary and desirable to modify this PFCC educational program to an interdisciplinary one. Additionally, alternative evaluation methods, such as shadowing nurses to assess their approaches, should be considered. Another way could be by asking feedback from patients and their families to assess the perceived level of patient- and family-centeredness in care delivery using a validated tool. Hence, we are currently actively engaged in the development of a novel instrument designed to assess how effectively nurses provide patient and family centered care, as perceived by family members. Nurse researchers at Griffith University, situated on the Gold Coast of Australia, are leading this collaborative endeavor.
Finally, we acknowledge several limitations of this study. First, the sample might not be representative for all registered nurses. As the educational program was voluntary, the participants likely were more than average motivated to work on their attitude and competencies. There were some baseline differences between the groups (working hours and personal experiences). However, we corrected for these differences. Although these minor baseline differences, the attitudes and competencies of the educational and control groups were quite similar at baseline. Randomization was considered, however, nurses' motivation and preferences regarding participation in the PFEP (or not) could potentially result in a high dropout rate immediately after randomization, thereby limiting the generalizability of the results to real-world clinical practice. Therefore, we choose to give priority to nurses who wanted to participate in the education program. Also, the study was conducted in one hospital and participants were selected through self-selection which may limit the generalizability of our results. Secondly, this study is limited by the drop-outs during the educational program. It is possible this drop-out was not at random, and influence on the results cannot be ruled out. Thirdly, the participants of the education and control groups were recruited from the same ward, so there may have lead to between-group contamination. Despite this possible confounding, only significant changes in the intervention were observed. Lastly, the qualitative evaluation was limited to four interviews only. The findings of this evaluation were used as additional context and shows limited insight of the additional effects of this educational program.
4.2. Innovation
This study contributes to the growing body of literature studying the effectivity of patient and family participation education programs. In contrast to previous publications that focused on nurses from specialized units [[13], [14], [15]], our education program is unique as it is developed for a heterogeneous group of nurses working on a variety of general wards. The knowledge, skills and attitudes we identified as essential to implement PFCC, are taught with e-learnings, workplace assignments and short face-to-face training group sessions. This innovative combination give the participants possibilities to tailor the content to specific working situations and personalized learning goals [30]. In addition, the education program acknowledge the complexity of PFCC that goes beyond knowledge [9,12]. Therefore, this education program specifically aims to influence the attitude of nurses towards PFCC. Finally, as time constrains are common in clinical nursing nowadays, this program was designed as a compact blended educational program to facilitate participation.
4.3. Conclusion
The patient family education program appeared to effectively promote nurses' attitudes and feelings of competencies towards patient and family participation. However, although we should interpret the qualitative evaluation with caution, some nurses mentioned that it still remains difficult to practice this acquired attitude and competencies. Team and organizational factors could influence this education program's impact on how nurses perform in daily practice. Hence, we assert that the PFEP holds value, while also recognizing the necessity of a multi-component strategy to facilitate the transition to a patient- and family-centered hospital environment. This may involve engaging other healthcare professionals and implementing team-based interventions.
Funding
This project was sponsored by an innovation grant of the Amsterdam UMC, the Netherlands.
CRediT authorship contribution statement
Peter van Oort: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Formal analysis, Data curation, Conceptualization. Jolanda Maaskant: Writing – review & editing, Validation, Methodology, Funding acquisition, Formal analysis, Data curation, Conceptualization. Marie Louise Luttik: Writing – review & editing, Data curation. Anne Eskes: Writing – review & editing, Validation, Supervision, Methodology, Data curation.
Declaration of Competing Interest
None.
References
- 1.Carman K.L., Dardess P., Maurer M., Sofaer S., Adams K., Bechtel C., et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff. 2013;32:223–231. doi: 10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]
- 2.Institute for Patient- and Family-Centered Care What is Patient- and Family-Centered Care? 2020. https//www.ipfcc.org/about/pfcc.html (Accessed December 2020)
- 3.Kuo D.Z., Houtrow A.J., Arango P., Kuhlthau K.A., Simmons J.M., Neff J.M. Family-centered care: current applications and future directions in pediatric health care. Matern Child Health J. 2012;16:297–305. doi: 10.1007/s10995-011-0751-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shields L., Pratt J., Hunter J. Family centred care: a review of qualitative studies. J Clin Nurs. 2006;15:1317–1323. doi: 10.1111/j.1365-2702.2006.01433.x. [DOI] [PubMed] [Google Scholar]
- 5.Park M., Giap T.T., Lee M., Jeong H., Jeong M., Go Y. Patient- and family-centered care interventions for improving the quality of health care: a review of systematic reviews. Int J Nurs Stud. 2018;87:69–83. doi: 10.1016/j.ijnurstu.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 6.Mackie B.R., Mitchell M., Marshall A. The impact of interventions that promote family involvement in care on adult acute-care wards: an integrative review. Collegian. 2018;25:131–140. doi: 10.1016/j.colegn.2017.01.006. [DOI] [Google Scholar]
- 7.Svavarsdottir E.K., Tryggvadottir G.B., Sigurdardottir A.O. Knowledge translation in family nursing: does a short-term therapeutic conversation intervention benefit families of children or adolescents within a hospital setting? Findings from the Landspitali University Hospital Family Nursing Implementation Project. J Fam Nurs. 2012;18:303–327. doi: 10.1177/107484071244920. [DOI] [PubMed] [Google Scholar]
- 8.Luttik M.L.A., Goossens E., Ågren S., Jaarsma T., Mårtensson J., Thompson D.R., et al. Attitudes of nurses towards family involvement in the care for patients with cardiovascular diseases. Eur J Cardiovasc Nurs. 2017;16:299–308. doi: 10.1177/1474515116663143. [DOI] [PubMed] [Google Scholar]
- 9.Benzein E., Johansson P., Arestedt K.F., Saveman B.I. Nurses’ attitudes about the importance of families in nursing care: a survey of Swedish nurses. J Fam Nurs. 2008;14:162–180. doi: 10.1177/1074840708317058. [DOI] [PubMed] [Google Scholar]
- 10.Hagedoorn E.I., Paans W., Jaarsma T., Keers J.C., van der Schans C.P., Luttik M.L.A. The importance of families in nursing care: attitudes of nurses in the Netherlands. Scand J Caring Sci. 2021;35:1207–1215. doi: 10.1111/scs.12939. [DOI] [PubMed] [Google Scholar]
- 11.Broekema S., Paans W., Roodbol P.F., Luttik M.L.A. Nurses’ application of the components of family nursing conversations in home health care: a qualitative content analysis. Scand J Caring Sci. 2020;34:322–331. doi: 10.1111/scs.12731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maaskant J.M., van Wessel I.M.E., Seller-Boersma A.S., Jongerden I., Paulus F., Eskes A.M. Nurses’ attitudes regarding family-centered care: psychometric properties and survey findings. J Nurs Meas. 2022;30:733–747. doi: 10.1891/JNM-D-21-00024. [DOI] [PubMed] [Google Scholar]
- 13.Eggenberger S.K., Sanders M. A family nursing educational intervention supports nurses and families in an adult intensive care unit. Aust Crit Care. 2016;29:217–223. doi: 10.1016/j.aucc.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Gibbs D., Warren I.M. Implementing infant and family-centred developmental care: exploring the impact of an innovative educational initiative. Acta Paediatr. 2023;112:264–272. doi: 10.1111/apa.16603. [DOI] [PubMed] [Google Scholar]
- 15.Petursdottir A.B., Haraldsdottir E., Svavarsdottir E.K. The impact of implementing an educational intervention to enhance a family-oriented approach in specialised palliative home care: a quasi-experimental study. Scand J Caring Sci. 2019;33:342–350. doi: 10.1111/scs.12628. [DOI] [PubMed] [Google Scholar]
- 16.Bos-van den Hoek D.W., Thodé M., Jongerden I., van Laarhoven H.W.M., Smets E.M.A., Tange D., et al. The role of hospital nurses in shared decision-making about life-prolonging treatment: a qualitative interview study. J Adv Nurs. 2021;77:296–307. doi: 10.1111/jan.14549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murugesu L., Heijmans M., Fransen M., Rademakers J. NIVEL; Utrecht: 2018. Beter omgaan met beperkte gezondheidsvaardigheden in de curatieve zorg: kennis, methoden en tools. [Google Scholar]
- 18.Saveman B.I., Benzein E.G., Engström A.H., Årestedt K. Refinement and psychometric reevaluation of the instrument: Families’ Importance In Nursing Care--Nurses’ Attitudes. J Fam Nurs. 2011;17:312–329. doi: 10.1177/1074840711415074. [DOI] [PubMed] [Google Scholar]
- 19.Hagedoorn E.I., Paans W., Jaarsma T., Keers J.C., Van Der Schans C.P., Luttik M.L.A., et al. Translation and psychometric evaluation of the Dutch families importance in nursing care: Nurses’ attitudes scale based on the generalized partial Credit model. J Fam Nurs. 2018;24:538–562. doi: 10.1177/1074840718810551. [DOI] [PubMed] [Google Scholar]
- 20.Hengeveld B., Maaskant J.M., Lindeboom R., Marshall A.P., Vermeulen H., Eskes A.M. Nursing competencies for family-centred care in the hospital setting: a multinational Q- methodology study. J Adv Nurs. 2020;10:1783–1799. doi: 10.1111/jan.14719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blöndal K., Zoëga S., Hafsteinsdottir J.E., Olafsdottir O.A., Thorvardardottir A.B., Hafsteinsdottir S.A., et al. Attitudes of registered and licensed practical nurses about the importance of families in surgical hospital units: findings from the Landspitali University Hospital family nursing implementation project. J Fam Nurs. 2014;20:355–375. doi: 10.1177/1074840714542875`. [DOI] [PubMed] [Google Scholar]
- 22.Younas A., Khan R.A., Yasmin R. Entrustment in physician-patient communication: a modified Delphi study using the EPA approach. BMC Med Educ. 2021;21:497. doi: 10.1186/s12909-021-02931-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shamali M., Esandi Larramendi N., Østergaard B., Barbieri-Figueiredo M., Brødsgaard A., Canga-Armayor A., et al. Nurses' attitudes towards family importance in nursing care across Europe. J Clin Nurs. 2023;32:4574–4585. doi: 10.1111/jocn.16456. [DOI] [PubMed] [Google Scholar]
- 24.Michie S., van Stralen M.M., West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maurer M., Dardess P., Carman K.L., Frazier K., Smeeding L., Rockville M.D. AHRQ Publication; 2012. Guide to Patient and Family Engagement: Environmental Scan Report. 12–0042-EF. [Google Scholar]
- 26.McCabe C. Nurse-patient communication: an exploration of patients’ experiences. J Clin Nurs. 2004;13:41–49. doi: 10.1111/j.1365-2702.2004.00817.x. [DOI] [PubMed] [Google Scholar]
- 27.Naef R., Kläusler-Troxler M., Ernst J., Huber S., Dinten-Schmid B., Karen T., et al. Translating family systems care into neonatology practice: a mixed method study of practitioners’ attitudes, practice skills and implementation experience. Int J Nurs Stud. 2020;102 doi: 10.1016/j.ijnurstu.2019.103448. [DOI] [PubMed] [Google Scholar]
- 28.Dyson J., Cowdell F. How is the theoretical domains framework applied in designing interventions to support healthcare practitioner behaviour change? A systematic review. International J Qual Health Care. 2021;33:mzab106. doi: 10.1093/intqhc/mzab106. [DOI] [PubMed] [Google Scholar]
- 29.Kruger J., Dunning D. Unskilled and unaware of it: how difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J Pers Soc Psychol. 1999;77:1121–1134. doi: 10.1037/0022-3514.77.6.1121. [DOI] [PubMed] [Google Scholar]
- 30.Vallée A., Blacher J., Cariou A., Sorbets E. Blended learning compared to traditional learning in medical education: systematic review and Meta-analysis. J Med Internet Res. 2020;22 doi: 10.2196/16504. [DOI] [PMC free article] [PubMed] [Google Scholar]