Summary
Background
Prevention and control of non-communicable diseases (NCDs) become a policy priority in Universal Health Coverage (UHC) in China, while NCD management has never been comprehensively estimated at national and subnational levels. We aimed to assess NCD management in China nationally and in key subpopulations, investigate inequalities from multidimensions, and further examine its association with health financing and resources.
Methods
Data included were from China Chronic Disease and Risk Factors Surveillance (CCDRFS) and China Health and Nutrition Survey (CHNS). Following the WHO recommended frameworks, we selected eight NCD health service and risk management indicators and used meta-analysis to construct the composite NCD index. We explored the trends in and projections of NCD management index and indicators at national and subnational levels by using Bayesian regression models with average annual percentage change (AAPC) from 2004 to 2018 and probability of reaching the UHC target by 2030. We further conducted comprehensive inequality analyses of NCD indicators from multidimensions with patterns of changes over time using absolute difference and relative ratio. Finally, we quantified the associations between NCD management performance with health financing and resources using stochastic frontier analysis.
Findings
In China, the NCD management index increased slowly from 62.0% (95% CI 36.0 to 84.0) in 2004 to 64.3% (95% CI 44.0 to 82.2) in 2018, with lagging performance being observed in prevention domain (AAPC −0.1%, 95% CrI −1.0 to 0.8). And all management indicators presented low probabilities of accomplishing 2030 targets in China. Notably, based on subnational analysis, diverse tendency and magnitude of inequalities in multiple NCD indicators were identified with widening gaps between genders (non-overweight, diabetes treatment), age groups (non-use of tobacco), urban-rural areas (non-use of alcohol, non-use of tobacco), regions (sufficient physical activity), and wealth quintiles (non-overweight, sufficient physical activity). Additionally, it was observed that compared with urban area, rural area had constantly lower health resources and presented 2.2% lower NCD management performance in 2018. Importantly, we found that health financing and resources especially distributed in primary health care (PHC) facilities were closely and positively associated with NCD management performance. A 1000 yuan increase of government health expenditure (GHE) per capita and a 10 increase of medical beds per 1000 capita in PHC facilities were associated with a 4.0% (95% CI 2.0 to 6.0) and 6.8% (95% CI 0.2 to 13.5) increase of NCD management index, respectively.
Interpretation
The progress towards NCD management is slow at national level and in key subpopulations in China, with great challenges of existing and widening inequalities between genders, age groups, urban-rural areas, regions and socioeconomic groups. Rural and old people were still vulnerable populations who were lagging behind in NCD prevention and control. Optimising resource allocation by strengthening PHC especially in rural area, developing tailor-made programmes targeting specific populations such as old individuals, simultaneously integrating gender, education, and economic interventions to reduce inequalities should be prioritised to help China tackle NCDs during the progress towards UHC.
Funding
National Natural Science Foundation of China.
Keywords: Non-communicable disease management, Universal health coverage, Inequalities, Primary health care, China
Research in context.
Evidence before this study
We searched PubMed for articles published in any language before September 26, 2023, using the terms ((non-communicable disease) OR (chronic diseases)) AND (inequality) OR (inequity) OR (disparity) AND (Universal Health Coverage). Of these 1564 records identified, 131 papers were about China. We determined 6 papers that assessed non-communicable disease (NCD) in China after screening the title, abstract, and 4 papers were finally determined after screening full text. Previously, four studies reported NCD prevention and control in China, provided valuable information about the major NCDs and related risk factors, and widely discussed related policies, practices, and incentives. However, work to date has only examined individual NCD indicators in isolation with restricted captured interventions and none of them measured overall NCD management using comprehensive index from WHO recommended frameworks, which cannot be internationally compared. NCD management has never been comprehensively estimated at national and subnational levels in China and whether China can reach the 2030 global targets is also unknown. Also, we found no study conducted comprehensive inequality analyses in NCD management indicators in China, encompassing estimations, trends, and patterns of disparities between geographic, demographic, and socioeconomic groups. Moreover, some studies have suggested that an economic perspective is critical to the design and implementation of effective policies in addressing NCDs. However, no studies have investigated the associations between NCD management performance with health financing and resources, and such quantifiable evidence in low-income and middle-income countries (LMICs) including China are very scarce.
Added value of this study
To the best of our knowledge, this study provides the most comprehensive assessment of NCD management in China at national and subnational levels following WHO frameworks. Our results demonstrated that China showed slow progress in NCD management with the majority of NCD indicators failing to reach the 2030 targets at either national or sub-national levels. Notably, our findings highlighted existing and even increasing geographic, demographic, and socioeconomic inequalities in NCD management indicators with different trends and patterns, which may impede China's progress towards achieving UHC. Individuals in rural area still presented low availability of essential treatment services, and old people were lagged behind in several indicators in prevention domain, indicating that rural and old people were left behind in NCD prevention and control. Furthermore, our study quantified the associations between health financing and resources and NCD management performance, which first provided essential evidence of the role that health financing and resources distributed in primary health care (PHC) could play in promoting NCD management, filling the aforementioned knowledge gaps and provided valuable insights for approach to NCD prevention and control worldwide.
Implications of all the available evidence
China showed slow progress in NCD management at both national and subnational levels. Existing and increasing inequalities indicated unignorable challenges, requiring effective national-to-local strategy. Equity-oriented and contextualised interventions should be focused on least coverage indicators and greatest needed populations such as rural and old populations. Optimising resource allocation and improving efficacy of financial investment by promoting high-quality primary health care should be priorities for preventing and coping with NCDs in China.
Introduction
Non-communicable diseases (NCDs) contributed the largest portion of the global burden of disease, causing 41.1 million deaths (73.4%) and 874,500 (53.0%) years of life lost (YLL) in 2017, which is also becoming an essential issue of equity.1, 2, 3 Prevention and control of NCDs are prioritised in the Sustainable Development Goals (SDGs) and have been a health policy priority for countries worldwide during the progress moving towards Universal Health Coverage (UHC).4, 5, 6 Specifically, UHC targeting that at least 80% of the population having access to quality health services by 2030 irrespective of geographic area or economic status, including providing universal access to essential NCD interventions.5,6 On basis of the NCD best-buys strategy and global monitoring framework (GMF),7, 8, 9 WHO further identified a set of NCD intervention coverage indicators in the context of UHC for prevention and treatment.5,6 In the past decades, many countries have made efforts to enhance NCD management by preventing risk factors, improving treatment services, and reducing inequalities.10, 11, 12 However, many low- and middle-income countries (LMICs) still struggle to address NCDs and bear a disproportionate NCD burden, where 76% of NCD deaths (31.4 million) occur but only 1% of health funding is dedicated.12, 13, 14, 15 In this situation, it is crucial to monitor progress towards global targets, evaluate NCD management, identify high risk people, as well as understand how to distribute limited inputs more effectively for NCD control in LMICs. As the most populous LMIC in the world, data from China would be useful to fill the gap in incomplete information from LMICs around the world, and provide valuable insights and approach for NCD prevention and control worldwide.
China has been undergoing the increasing NCD burden due to economic development, accelerating urbanisation, and population ageing, with cardiovascular diseases, cancer, and chronic respiratory diseases accounting for 80.7% of the total deaths in 2019.16, 17, 18 Since the comprehensive healthcare reform in 2009, Chinese government has put place a wide range of strategies to tackle NCDs, such as the “Health China 2030” plan, the national Medium-to-Long Term Plan for the Prevention and Treatment of Chronic Diseases (2017–2025), and the Healthy Life Style for All 2017–2025 Action Protocol,19, 20, 21 which predominantly centralised prevention activities, treatment management, and capacity enhancement. Previously, one study has comprehensively analysed the trends in major NCDs and related risk factors in China, providing valuable information of NCD burden.22 Additionally, several studies have tried to report NCD prevention and control in China, but works to date has only examined individual NCD indicators in isolation with restricted captured interventions.23,24 None of them measured overall NCD management using comprehensive index from WHO recommended frameworks, which cannot be internationally compared and whether China can accomplish the 2030 global targets is also unknown. Moreover, health problems remain heterogeneous across populations as demonstrated in our previous work on UHC assessment in China.25 Few studies have systematically investigated the disparities of NCD management across populations by sociodemographic and regional characteristics from subnational level analysis, which may potentially mask the true dimensions of a problem. Reducing NCD burden without considering these disparities will further leave behind already-vulnerable people in disadvantages. Moreover, how to transform limited health resources to promote NCD management is also an essential question, while such evidence-based information in LMICs including China are very scarce.26
As China rapidly experiences epidemiological and demographic transitions, closely monitoring the progress in NCD management at national and subnational levels, identifying major NCD problems and most vulnerable people, and further understanding how to distribute limited health resource for better NCD management performance have far-reaching policy implications for prioritising health strategies. In this study, we aimed to provide the most comprehensive assessment of NCD management in China at national and subnational levels with probability of achieving 2030 UHC targets. We conducted a comprehensive analysis of inequality in NCD management in China with trends and patterns across populations by gender, age groups, residence, region, education, and income to capture the demographic, geographic, and socioeconomic disparities. Moreover, we further quantified the associations between NCD management performance with health financing and resources, which would be crucial for informing policymakers in LMICs to develop effective health strategies for NCD prevention and control.
Methods
Data sources
Our study based on data from nationally representative household survey (China Chronic Disease and Risk Factors Surveillance, CCDRFS) and large-scale longitudinal survey (China Health and Nutrition Survey, CHNS). The CCDRFS, carried out by the Chinese Centre for Disease Control and Prevention (China CDC) every three years since 2004, is serial national cross-sectional surveys to monitor the prevalence of major NCDs and their risk factors in China.27, 28, 29 Multistage stratified cluster sampling was employed to select subjects on the basis of the adjusted National Disease Surveillance Points (DSPs) covering all 31 provinces in mainland of China. The CHNS is an ongoing large-scale, longitudinal survey launched in 1989 by University of North Carolina at Chapel Hill and Chinese Center for Disease Control and Prevention to monitor Chinese residents’ health, nutritional status, and lifestyle behaviours.30,31 Multistage random-cluster sampling was used to choose samples from 15 provinces across China. Details on these two household surveys and data sources can be seen in Appendix (pp 2–7), and more information about the study design have been described elsewhere.27, 28, 29, 30, 31
Individuals aged 18 years or above from the latest five rounds data of CCDRFS (2004, 2007, 2010, 2013, and 2018) and the latest four waves of CHNS (2004, 2009, 2011, and 2015) were included for analysis in this study. Notably, the survey time of each round across these two surveys was not identical. Such differences in the timing of survey waves were not rare in studies that included numerous indicators spanning long timeframe. And to address this inconsistency, adjacent years as the same survey time have been usually used previously.31, 32, 33 Therefore, we followed this approach in our analysis considering that the NCD management progress was seldom a discontinuous and sudden change.10,22 Besides, we collected the health financing and resources data in each survey year (2004, 2009, 2013, and 2018) from the statistical yearbook of the National Bureau of Statistics and of China and China Health Statistics Yearbook.34,35
Ethical approval was not required for this study because only secondary datasets were used.
Measurement of NCD management indicators
NCD management is defined as preventing and controlling major noncommunicable diseases and their key risk factors. Following WHO's global monitoring frameworks and indicators (NCD framework, “best-buys”, UHC framework, and global health indicator),5,8,9,36 we measured the NCD management progress with the coverages for a set of tracer interventions from prevention and treatment domains. Considering varieties in indicators, it is important to take into account a country's epidemiology, health system, and data availability when choosing indicators. Based on the selection criteria involving relevance, quality, and availability of the indicators and previous studies (Appendix pp 8–9), we finally selected eight NCD risk management and health service indicators. Six prevention indicators (sufficient physical activity (SPA), non-use of alcohol (NUA), non-use of tobacco (NUT), non-overweight (NOW), sufficient fruit and vegetable intake (SFVI), and non-hypercholesterolemia (NHC)) were included in WHO NCD Monitoring Framework, UHC framework, “best-buys”, and global health indicator, and two treatment indicators (hypertension treatment (HTNT), and diabetes treatment (DBT)) were included in UHC framework for NCD treatment services assessment. The choice and rationale of indicators selection, details of estimated indicators with data source and definition can be seen in Appendix pp 8–13. To track the overall progress, we construct the composite NCD management indices of management (all indicators), prevention (six prevention indicators), treatment (two treatment indicators) using random-effect meta-analysis (Appendix p 14). As illustrated in previous studies,10,31 the advantage of meta-analysis was its repeatability and transparency compared with other methods.
Statistical analysis
The coverages of composite NCD management indices and indicators were estimated with 95% confidence intervals (CIs). As widely applied in previous work,10,25,31 we conducted Bayesian linear regression models with non-informative prior to explore trends in and projections of NCD indicators (Appendix p 15). The logit transformed proportions of NCD indicators were the dependent variables and survey year was the covariate. Posterior predictive distributions were extracted from the fitted Bayesian models to compute the average annual percentage of change (AAPC) over time and probability of reaching UHC target (as of 80% coverage) for NCD management indicators. A Markov chain Monte Carlo (MCMC) algorithm was used to obtain 1000 samples from the posterior distributions of the parameter of interest with two chains. We discarded the initial 5000 iterations as burn-in for each model and continued the iterations until the output confirmed convergence. We used the trace plots and potential scale reduction factor for convergence diagnosis of Bayesian models.37 Additionally, in models that were stratified by subgroups (household annual income, educational level, geographic region, residence, gender, and age group), we included and tested the interaction terms between these variables and survey year using the deviance information criterion (Appendix p 27).
Further, we conducted a comprehensive inequality analysis in NCD management indicators from multidimensions as well as examined the changes. Data were stratified by gender (men and women), age (18–44 years, 45–59 years, and 60 years or above), residence (urban and rural), geographic region (east, central, and west), educational level (primary school or below, middle school, high school, and college or above), and household annual income (quartile 1 [Q1, the poorest] to quartile 4 [Q4, the wealthiest]). To evaluate the degree of income inequality in an NCD indicator, we calculated the difference and ratio of an indicator based on the level of household income in the top (Q4) and bottom (Q1).25,38 The difference suggests an absolute inequality (Q4-Q1), where 0 implies no inequality. The ratio expresses a relative inequality (Q4/Q1), where 1 implies no inequality. The same analysis was conducted to investigate multiple dimensions of inequalities of NCD indicators in gender, age, residence, geographic region, and educational level. For composite NCD indices, inequality analyses were only conducted within the dimensions of gender, residence, and geographic region due to constraints in the availability of certain NCD indicators in subgroups. Additionally, we calculated the changes in difference and ratio between two time points (ie, the year 2013 and 2018) to estimate the tendency in absolute and relative inequalities over the period.10
Macroeconomic perspective is critical to the NCD management, which requires health financing systems that provide prepaid pooled resources for key health services.26,39 As in our work and other previous studies on financial analysis,25,40,41 to better understand the impact of economic and resource investment in NCD prevention and control, we further did stochastic frontier analysis (SFA) to investigate the associations between national NCD management index performance with health financing and resources (Appendix p 16). Health financing and resources were measured by government health expenditure (GHE) per capita and medical beds per 1000 capita, which were further stratified by different medical institutions including primary health care (PHC) facilities and large hospitals. In addition to the overall relationships, we also compared the different effects of health financing and resources distributed in hospitals and primary health-care institutions on NCD management.
All statistical analyses were performed in Stata 16.0 and R (version 4.2.3).
Sensitivity analysis
Sensitivity analyses were performed to test the robustness of our results. First, we tested the linear assumption of Bayesian models by employing a generalised additive model with three degrees of freedom. We then compared the adjusted R-squares of this model with those obtained from the linear model. Moreover, to further validate the extrapolation, we projected the trends based on observed data from 2004 to 2013, and compared the predicted values with observed data. And we also compared projections for NCD management indicators in 2030 using the overall trends (all data points 2004 to 2018) and recent trends (the last 3 years 2009–2018). Second, we conducted a sensitivity analysis of composite indices by using two other aggregate methods of geometric and arithmetic average with individual indicators equally-weighted. These indices were integrated into Bayesian models for trend and projection analysis, and the results were compared with those from random-effect meta-analysis. Third, we examined if the composite NCD management indices in the meta-analysis were influenced by a limited number of indicators. Specifically, we removed an indicator every time and then recalculated the composite NCD management indices to observe any significant changes in the results. Forth, following previous study,10 we used multiple imputation approach for handling missing values in household income information of some indicators to test the robustness of our results (Appendix p 17). Fifth, we also investigated whether inconsistencies in the timing of survey waves would significantly affect our results. More details of sensitivity analyses can be seen in Appendix pp 20–26.
Role of the funding source
The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Trends in and projections of NCD management indicators
Table 1 reports the national NCD management indices and indicators in China with both observed coverages (2004–2018) and projections (2030). Overall, the composite NCD management index presented slow increase from 62.0% (95% CI 36.0 to 84.0) in 2004 to 64.3% (95% CI 44.0 to 82.2) in 2018, and was projected to reach 66.5% (95% CrI 52.1 to 79.1) in 2030 at national level (Table 1). In terms of different domains, a substantial increase of 12.5% was found in the treatment index over time, while lagging change was observed in prevention index (AAPC −0.1%, 95% CrI −1.1 to 0.9). Notably, most NCD management indicators presented very low probabilities of accomplishing 2030 targets, and different indicators demonstrated various patterns and trends (Table 1). For lifestyle behaviours indicators, sufficient fruit and vegetable intake (SFVI) increased largely (AAPC, 2.1%, 95% CrI 0.1 to 4.4) but was projected to be still far below the target in 2030 (67.5%, 95% CrI 48.3 to 83.4), the improvements of non-use of alcohol (NUA) and non-use of tobacco (NUT) were not substantial (AAPC 0.5, 95% CrI −1.2 to 2.2; 0.5, 95% CrI −0.3 to 1.5), while sufficient physical activity (SPA) even presented constantly decreasing trend from 82.2% (95% CI 81.3 to 83.1) to 78.5% (95% CI 77.5 to 79.5) between 2004 and 2018. Although the coverage of non-hypercholesterolemia (NHC) exceeded 90%, decreasing trend was observed (AAPC, −0.5%, 95% CrI −0.9 to −0.2) and remarkable decrease in non-overweight (NOW) was also found with unacceptably high AAPC (−1.4%, 95% CrI −2.6 to −0.2). Within treatment domain, hypertension treatment (HTNT) and diabetes treatment (DBT) presented large improvements between 2004 and 2018 (AAPC 3.3%, 95% CrI −0.5 to 6.9; 3.9%, 95% CrI 0.0 to 7.6), and were projected to reach 49.0% (95% CrI 26.7 to 72.4) and 52.6% (95% CrI 27.7 to 75.3) in 2030 respectively.
Table 1.
Trends in and projections of national Non-communicable disease management in China from 2004 to 2030.
| Observed coverage (95% CI) |
AAPC (95% CrI) |
Predicted coverage (95% CrI) |
Probability of reaching targeta (%) | ||||
|---|---|---|---|---|---|---|---|
| 2004 | 2009 | 2013 | 2018 | 2004–2018 | 2030 | ||
| Non-use of tobacco | 71.5 (70.6 to 72.4) | 72.3 (71.4 to 73.2) | 73.8 (73.0 to 74.6) | 76.5 (75.7 to 77.2) | 0.5 (−0.3 to 1.5) | 79.4 (66.9 to 88.6) | 47.9 |
| Non-use of alcohol | 67.6 (66.7 to 68.5) | 66.9 (66.0 to 67.8) | 66.2 (65.4 to 67.0) | 72.5 (71.7 to 73.3) | 0.5 (−1.2 to 2.2) | 73.5 (54.6 to 89.0) | 20.5 |
| Sufficient physical activity | 82.2 (81.3 to 83.1) | 84.8 (83.9 to 85.7) | 81.6 (80.8 to 82.4) | 78.5 (77.5 to 79.5) | −0.4 (−1.4 to 0.7) | 74.3 (52.4 to 88.9) | 26.2 |
| Sufficient fruit and vegetable intake | 41.5 (41.0 to 42.0) | 47.2 (46.9 to 47.5) | 53.2 (53.0 to 53.4) | 55.3 (55.1 to 55.5) | 2.1 (0.1 to 4.4) | 67.5 (48.3 to 83.4) | 4.6 |
| Non-hypercholesterolemia | 96.9 (96.6 to 96.6) | 96.7 (92.8 to 92.8) | 92.9 (91.7 to 91.7) | 91.8 (91.7 to 91.7) | −0.5 (−0.9 to −0.2) | 78.9 (56.8 to 92.8) | 50.8 |
| Non-overweight | 74.4 (73.5 to 75.3) | 70.9 (70.0 to 71.8) | 66.7 (65.8 to 67.5) | 60.7 (59.8 to 61.6) | −1.4 (−2.6 to −0.2) | 47.8 (31.7 to 64.4) | 0.1 |
| Hypertension treatment | 23.1 (22.6 to 23.6) | 23.7 (23.3 to 24.1) | 32.5 (32.3 to 32.7) | 34.9 (34.7 to 35.1) | 3.3 (−0.5 to 6.9) | 49.0 (26.7 to 72.4) | 0.5 |
| Diabetes treatment | 20.7 (20.4 to 21.1) | 25.8 (25.5 to 26.1) | 35.6 (35.4 to 35.8) | 34.1 (33.9 to 34.3) | 3.9 (0.0 to 7.6) | 52.6 (27.7 to 75.3) | 0.9 |
| Composite NCD prevention index | 74.0 (50.0 to 92.0) | 75.1 (47.6 to 94.6) | 73.6 (51.4 to 90.8) | 73.6 (53.3 to 89.7) | −0.1 (−1.1 to 0.9) | 72.8 (56.2 to 85.1) | 9.8 |
| Composite NCD treatment index | 22.0 (22.0 to 22.0) | 24.7 (24.6 to 24.9) | 34.0 (33.9 to 34.2) | 34.5 (34.3 to 34.7) | 3.5 (−0.1 to 7.3) | 50.8 (28.5 to 72.5) | 0.6 |
| Composite NCD management index | 62.0 (36.0 to 84.0) | 63.0 (36.4 to 85.9) | 64.2 (43.1 to 82.7) | 64.3 (44.0 to 82.2) | 0.2 (−1.1 to 1.4) | 66.5 (52.1 to 79.1) | 2.3 |
WHO's targets of at least 80% health service coverage for the entire population by 2030 for Universal Health Coverage. NCD = Non-communicable disease. 95% CI = 95% Confidence Interval. 95% CrI = 95% Credible Intervals. AAPC = Average annual percentage change.
Estimations and changes in inequalities in NCD management indicators
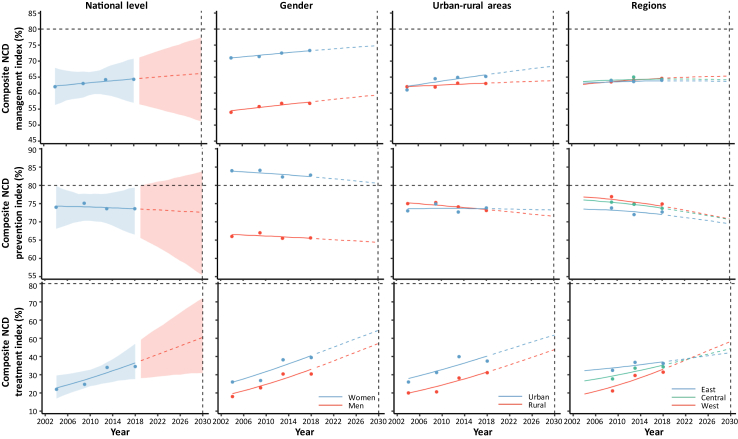
Fig. 1 demonstrates the trends in and projections of composite NCD indices stratified by gender, urban-rural area, and region. Constantly sizeable gender discrepancies were observed in NCD management index with large difference presenting in prevention index (Fig. 1). The prevention index in women was consistently high exceeding 80% while it in men was constantly far below the target (Fig. 1). Women have achieved the 2030 target in NUT and NUA but were left behind in SPA, men were lagging in most NCD indicators with no chance of achieving 80% target by 2030 (Appendix p 18). Notably, we observed expanding urban-rural disparity in NCD management index with large gap remaining in treatment domain (Fig. 1), and rural people would be left behind in most indicators such as HTNT, DBT, NUT, and SFVI (Appendix p 18). Significant narrowing regional disparities were observed in both prevention and treatment indices and the gap was small in NCD management index (Fig. 1). Nevertheless, differences in coverages of some NCD indicators across regions were still remain. West region showed lower coverage in most indicators such as NUT, SFVI, HTNT, and DBT, while east region presented lower coverage in NOW, SPA, and NHC (Appendix p 18).
Fig. 1.
Trends in, projections of, and inequalities in composite Non-communicable disease management indices in China from 2004 to 2030. Dots represented recorded mean estimates. Lines show the posterior mean estimates (dashed lines represent projected future values). The shaded area represents the 95% credible intervals. The dotted line represents the 80% coverage target for NCD management indicators by year 2030. NCD = Non-communicable disease.
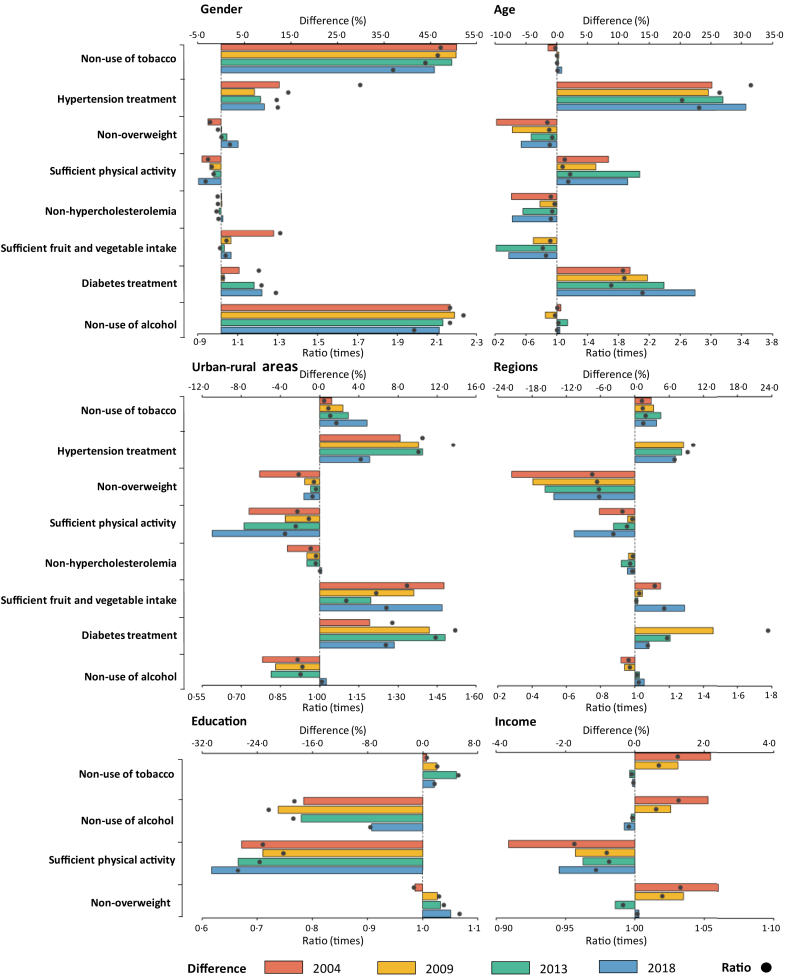
Fig. 2 further presents the absolute and relative inequality in all NCD management indicators in 2004, 2009, 2013, and 2018 by age group, gender, region, urban-rural area, education, and income. Notably, we found diversities in the magnitude and tendency of inequalities between different subgroups (Fig. 2). Gender inequality presented the largest disparity in NUA and NUT with differences of 45.8% and 46.9%, and ratios as high as 1.9 and 2.0 in 2018, respectively. Age inequality was observed with old people lagging behind in SFVI, NOW, and NHC, while younger people presented lower coverage in lifestyle behaviours indicators like SPA, NUA, and NUT. Notably, urban-rural and regional inequalities presented similar patterns and large gaps were observed in SFVI (difference 12.5%, ratio 1.3 for urban-rural areas; difference 8.7%, ratio 1.2 for regions), HTNT (difference 5.1%, ratio 1.6 for urban-rural areas; difference 7.1%, ratio 1.2 for regions), SPA (difference −10.9%, ratio 0.8 for urban-rural areas; difference −10.6%, ratio 0.8 for regions) and NOW (difference −1.6%, ratio 0.9 for urban-rural areas; difference −14.2%, ratio 0.7 for regions). Additionally, low coverages of SFVI, NUT, NUA, HTNT, and DBT in rural population and west people, and low coverages of SPA and NOW in urban population and east people. Additionally, both education and wealth inequalities presented the highest gap in SPA (difference −30.6%, ratio 0.6 for education; difference −2.2%, ratio 0.9 for income), with no statistically significant inequality in NUT.
Fig. 2.
Absolute and relative inequality for Non-communicable disease management indicators in China. The bar indicates the difference and the point indicates the ratio, which present the absolute and relative inequality between two subgroups (women vs men, 60 years or above vs 18–44 years, urban vs rural, east vs west, high educational level vs low educational level, and Q4 vs Q1). Difference = 0 or ratio = 1 indicates non-disparities between each subgroup in NCD management indicators. Difference >0 or ratio >1 suggests higher coverage in NCD management indicators in women, 60 years or above, urban, east, high educational level, and Q4 income subgroups. Difference <0 or ratio <1 suggests lower coverage NCD management indicators in women, 60 years or above, urban, east, high educational level, and Q4 income subgroups.
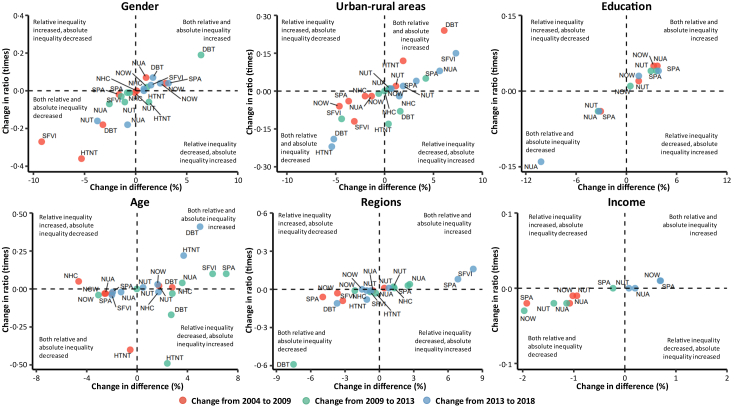
Moreover, NCD management indicators presented different trends in inequalities from multiple dimensions, and two major patterns of changes were further identified (Fig. 3). The first pattern was characterised by an improving trend in both absolute and relative inequalities, which indicates narrowing gaps over time (bottom-left corner). The bottom-left corner presents the indicators with significant improvements in absolute and relative inequalities between genders (NUT, NUA, SFVI), regions (NOW, HTNT, DBT), educational levels (NUT, NUA) and wealth quintiles (NUA). Conversely, the top-right corner shows the indicators with worsening trends in inequality with widening gaps, which can be observed in gender inequality (NOW, DBT), age inequality (NUT, DBT), urban-rural inequality (NUT, NUA, SPA), regional inequality (SPA), and wealth inequality (SPA, NOW).
Fig. 3.
Changes in inequalities in Non-communicable disease management indicators in China from 2004 to 2018. The horizontal axis shows change in difference indicating change in absolute inequality between two time points. The vertical axis shows change in ratio indicating change in relative inequality between two time points. The top-left corner indicates the relative inequality increased and the absolute inequality decreased, the top-right corner indicates both the relative and absolute inequality increased, the bottom-left corner indicates both the relative and absolute inequality decreased, and the bottom-right corner indicates the relative inequality decreased and the absolute inequality increased. NUT = non-use of tobacco use. NUA = non-use of alcohol. SPA = sufficient physical activity. NHC = non-hypercholesterolemia. SFVI = sufficient fruit and vegetable intake. NOW = non-overweight. HTNT = hypertension treatment. DBT = diabetes treatment.
Associations between NCD management performance with health financing and resources
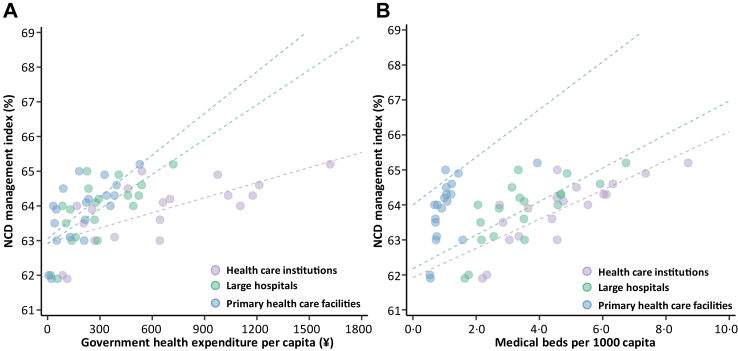
It was noted that rural area had constantly lower health resources than urban area in China during the survey years and presented 2.2% lower NCD management performance in 2018 (Appendix p 14). Further, we found that the upward and significant (p < 0.05) slopes of the NCD management frontiers show positive relationships between the NCD index with health financing and resources: a 1000 yuan increase of GHE per capita and a 10 increase of medical beds per 1000 capita were associated with the NCD management index increase of 1.5% (95% CI 0.8 to 2.1) and 4.2% (95% CI 2.7 to 5.6) respectively (Fig. 4). Notably, these relationships varied by health expenditure and resource in different medical institutions in large hospitals and primary health care (PHC) facilities. Higher NCD management performance was associated with health financing and resources allocated in PHC facilities than in hospitals: GHE per capita of 100 yuan and one medical beds per 1000 capita in PHC facilities can reach 63.5% and 64.7% on the NCD management index respectively, which were 0.3% and 2.0% higher than the same health spending and medical beds allocated in hospitals. Additionally, a 1000 yuan increase of GHE per capita and a 10 increase of medical beds per 1000 capita in PHC facilities were associated with the NCD management index increase of 4.0% (95% CI 2.0 to 6.0) and 6.8% (95% CI 0.2 to 13.5) respectively.
Fig. 4.
Associations between Non-communicable disease management performance with health financing and resources. (A) Relationship between NCD management index and government health spending per capita (B) Relationship between NCD management index and medical beds per 1000 capita. Data are based on the four round surveys. Datapoints represent residence regions or urban-rural areas in each survey year. Datapoints are colour-coded by different level of healthcare institutions. The line represents the fitted value of the NCD management index. Medical and healthcare institutions refer to primary health care facilities, hospitals, professional public health institutions, etc. Primary health care facilities refer to town and township health centres, community health centres (stations) and village medical rooms, outpatients, clinics, etc. Hospitals refer to general hospitals, traditional Chinese medicine hospitals, integrated traditional Chinese and western medicine hospitals, national hospitals, various specialised hospitals and nursing homes. NCD = Non-communicable disease.
Sensitivity analysis
The results of robustness tests and sensitivity analysis can be seen in Appendix pp 20–26. First, the adjusted R squares of the Bayesian linear model and generalised additive model are similar (Appendix p 20), indicating the validity of the Bayesian linear model in our study. Moreover, the small differences in predicted and observed coverage for most indicators suggested the validity of extrapolation (Appendix p 21). And for most indicators, small differences were observed between the projections in 2030 based on the overall and recent trends (Appendix p 22). Second, the values of composite NCD management index almost unchanged in sensitivity analysis of meta-analysis, indicating that the value of composite index were not driven by a specific indicator (Appendix p 23). Third, there is little difference in composite NCD indices using methods of random-effect meta-analysis, geometric average, and arithmetic average, which indicated the robustness of our results in meta-analysis (Appendix p 24). Forth, we found small differences of the projections before and after multiple imputation (Appendix p 25), suggesting that the robustness of our results and missing data would not be a great concern in our study. Fifth, differences in the time of survey waves have limited impacts on our results and conclusions (Appendix p 26).
Discussion
This study provides a comprehensive nationwide assessment of NCD management in China using major indicators following the WHO frameworks. Overall, despite notable improvement, the progress towards NCD management was still slow in China and most NCD indicators were predicted to fail to achieve the global target by 2030. Notably, our findings revealed existing even increasing gender, age, urban-rural, regional, educational, and socioeconomic inequalities in several NCD indicators with different trends and patterns, impeding the progress towards UHC in China. Importantly, by further quantifying the relationship between NCD management performance with health financing and resources, our results highlighted the essential role of PHC can play in NCD prevention and control, which could help identify tractable policy pathways to addressing NCDs. Therefore, continued efforts to develop more equitable and effective policies in NCD management should be made to achieve the 2030 targets.
Over the past decades, China has experienced a rapid epidemiological transition shifting from the infectious to the chronic diseases during demographic and social changes.16,22,23 Since major health-care reform in 2009, China has issued a series of national and local policies that are responsive to the country's increasing NCD burden.19, 20, 21 The composite NCD index in our study capturing a wide range of interventions presented increasing trend, suggesting these initiatives have already had some effects. Importantly, based on WHO-recommended frameworks, the results in our study were internationally comparable and our findings showed that improvements occurred in China over time with NCD management score exceeding many LMICs like Vietnam (63.6% in 2020).10 Particularly, we observed that remarkable achievements were mainly in treatment domain with substantial increase and narrowing regional disparity in hypertension and diabetes treatment. Such improvement can be largely attributed to the healthcare reform when diabetes and hypertension management were included in the National Basic Public Health Service Project,42 which in line with the aim of UHC to promote essential health service capacity and access for all. And remarkable improvement in treatment performance in the western region also indicated the positive impacts of transfer payment mechanism in public health spending in China.43 Nevertheless, as demonstrated in this study and other research, the rate of hypertension and diabetes treatment in China were lower than those in developed countries.28,44,45 Additionally, although China has attempted to change the emphasis of the healthcare principle from “treatment first” to “prevention first”,25 the progress towards NCD management was still challenging with lagging performance in prevention domain. The slow progress in NCD management in China may be attributed to a multitude of complex social, environmental, individual, and healthcare system factors, along with their interplay.16,22,23 Prominent social factors encompassed rapid urbanisation, an aging population, and heightened life expectancy.23,24 Environmental elements included air pollution, an obesogenic environment, and a generally low health literacy level.16 Individual aspects involved prevalent unfavorable lifestyles, such as smoking, physical inactivity, and poor dietary habits.22,23 Furthermore, a fragmented healthcare delivery system centred around hospitals, coupled with escalating healthcare expenses, has hindered China's capacity to efficiently mitigate and manage chronic diseases.31,43 There is still a long way to go for NCD prevention and control in China.
Of particular concern was the existing and even increasing inequalities in NCD prevention and control across populations, which poses huge hindrance to the whole nation's progress. Notably, different patterns regarding NCD risk factors and services access were identified among people with varying demographic, geographic, and socioeconomic characteristics. Specifically, while a high level of nutritional awareness might lead to high coverage of sufficient fruit and vegetable consumption, urban population was more likely to experience hypercholesterolemia and overweight with low activity level, possibly resulting from greater occupational pressures and prevalent sedentary behaviour.29 And rural people had much lower accessibility of hypertension and diabetes treatment. Young people had high risks of unhealthy behaviours especially tobacco and alcohol use, while old people were left behind in sufficient fruit and vegetable intake. Additionally, men were lagging in almost all NCD indicators with no chance of reaching targets by 2030. Moreover, the COVID-19 pandemic may exacerbate these inequality issues, leading to vulnerable populations especially rural and old people further in disadvantages in future. This concern found in our study provides an early warning for LMICs where the problems may also exist in these countries during the process of rapid economic development, accelerated urbanization and population aging.10,46, 47, 48 Reducing NCD and improving health equity has long been a government priority included in Healthy China 2030,19,25 while equity can only be achieved if specific and targeted intervention programmes can be developed at subnational or even more granular levels with full consideration of discrepancies. Our findings emphasised the necessity of developing tailor-made, well-designed, population-specific public health programs simultaneously integrating gender, education, and economic interventions. Particularly, improving diabetes and hypertension management services targeting vulnerable people in rural area, promoting physical activity programs with daily-activity, workplace-based, and city-design integrated interventions focused on urban populations, strengthening comprehensive school-based health education for young adults to reduce tobacco and alcohol use, providing adequate community supports for old people to improve health should be priorities.
Globally, NCDs impose huge economic losses that fall heavy on the LMICs.15,26 The imperative to address NCDs has become evident worldwide, while substantial challenges remain in implementation and the constraints of financing and resources with competing priorities are core issues.13,39,49,50 Our study first provided quantifiable evidence for relationships between health financing and resources and NCD performance, revealing that PHC could play an essential role. In fact, Chinese government invested massive funding into basic public health services including for NCD management with GHE per person tripling from ¥343 in 2008 to ¥1086 in 2017.50 However, the resources are not well allocated to where they would have the greatest benefit currently and health system was still hospital-centric and weak in PHC in China.25,31 Considering enormous challenges and pervasive inequalities in NCD management in China, improving the equity, efficiency, and effectiveness of policy is essential and one crucial solution is adopting national-to-local strategy. Additionally, establishing health information system in PHC facilities and developing Internet + Health initiatives would likely to be a more efficient way to promote the accessibility, availability, and acceptability of NCD management services especially for remote rural area in China.51,52
To tackle challenges of the slow progress and widespread inequalities in NCD management in China, vigorous multilevel efforts are needed to strengthen the current policy and practical measures by addressing various social, environmental, individual and healthcare system factors. For future NCD prevention and control, we recommend: 1) adopt national-to-local strategy by elevating efficacy of financial investment and optimizing resource allocation; 2) develop effective public health programs simultaneously integrating gender, education, and economic interventions; 3) reduce widespread inequalities by supporting the vulnerable population groups such as those with low socioeconomic status and those living in areas with limited resources; 4) reorient the healthcare system towards primary care, enhance community engagement, and promote digital health technologies use to improve access to healthcare services in NCDs.
From the perspective of NCD management, this study discussed realistic approaches to sustainably optimise NCD prevention and control in China. Our study had several strengths. First, our study included all major indicators following the WHO-recommended well-accepted frameworks. The developed composite NCD management indices offer the advantage of consolidating a wide range of information and facilitating comparisons within countries, between countries, and over time. Second, this study provided comprehensive estimation of NCD management in China including trends and projections at national and subnational levels, revealing patterns of changes in geographic, demographic, and socioeconomic inequalities, which identified least coverage indicators and greatest needed people. Such evidence-based information is crucial in developing tailored, population-specific, and equality-oriented policies and facilitate priority setting, which provides a valuable insight for future studies looking at these inequalities in other regions or contexts worldwide. Last, we quantified the association between health financing and resources and NCD management performance and highlighted the essential role PHC facilities can play in promoting NCD management, which shows potential opportunity to better leverage these resources for health priorities during progress towards UHC.
Nevertheless, our study also had some limitations. First, all our models were constructed under the assumption of unchanged future policies, relying on current trends, which may be too strict. Nevertheless, our primary aim was to forecast NCD management based on current trends to provide insights for future policymaking. Therefore, the assumption of stable policies was crucial for achieving the objectives of this study. Second, some critical indicators, such as cancer screening and chronic respiratory disease, were not available in our study. The lack of these indicators may have limited impacts on our results of the composition NCD management indices. Third, the non-nationally representative nature of the CHNS data is a limitation. However, we maintain that the multi-stage random cluster sampling strategy employed in the survey allows for an insightful exploration of NCD management inequalities across gender, age groups, residence, region, education, and income. Fourth, although our study reveals widespread inequalities in NCD management in China, quantitative analysis of the link between inequalities and underlying causes are needed in future work. Fifth, the investigation of inequality in NCD management indices was constrained by the availability of certain NCD indicators in subgroups, such as education and income. Last, it is essential to note that the observed associations between NCD performance with health financing and resources do not imply causality. Further investigations are necessary to explore alternative mechanisms that may underlie this relationship.
Conclusion
China still face many daunting challenges in NCD management. Our study indicated the slow progress in NCD management nationally, lagging performance in prevention domain, companied with existing and expanding inequalities between genders, urban-rural areas, and socioeconomic groups. Prevention and control of NCDs is a large and complex task, which requires public health programs made at both national and local levels to reduce widespread inequalities, simultaneously integrating gender, education, and economic interventions. Strengthening primary health care to address major risk factors for NCDs, focusing on vulnerable populations such as rural and old people, developing tailor-made, well-designed, population-specific public health programs, elevating efficacy of financial investment and optimising resource allocation would serve as a substantial contributor to enhance NCD management during China's progress towards UHC.
Contributors
LD and YZ conceived the idea for the study and managed the project. YZ, CL, PM, and LD designed the study. YZ, CL, and QW collected the data. YZ, CL, and QW did the statistical analyses, and wrote the statistical analysis plan. CL and QW drafted the manuscript. YZ and CL edited the manuscript. All authors discussed the results, contributed to revisions of the manuscript, and approved the final version.
Data sharing statement
Data included in this study were sourced from the China Chronic Disease and Risk Factors Surveillance (CCDRFS) and China Health and Nutrition Survey (CHNS). CHNS data files are available at [https://www.cpc.unc.edu/projects/china]. CCDRFS data used in our study can be obtained from national reports on chronic disease risk factors surveillance in China released by the National Center for Chronic and Noncommunicable Disease Control and Prevention of Chinese Center for Disease Control and Prevention.
Declaration of interests
All authors declare no competing interests.
Acknowledgements
This study is supported by the National Natural Science Foundation of China (grant No. 72122007, 72071089, 71732001, received by Ying Zhou and Lieyun Ding).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100989.
Contributor Information
Ying Zhou, Email: ying_zhou@hust.edu.cn.
Lieyun Ding, Email: dly@hust.edu.cn.
Appendix A. Supplementary data
References
- 1.GBD 2017 Causes of Death Collaborators Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO . World Health Organization; Geneva: 2014. Global status report on noncommunicable diseases 2014. [Google Scholar]
- 3.WHO . World Health Organization; Geneva: 2023. Advancing the global agenda on prevention and control of noncommunicable diseases 2000 to 2020: looking forwards to 2030. [Google Scholar]
- 4.WHO . World Health Organization; Geneva: 2020. Strengthening NCD service delivery through UHC benefit package: technical meeting report. [Google Scholar]
- 5.WHO, World Bank Group . 2014. Monitoring progress towards universal health coverage at country and global levels: framework, measures, and targets.https://www.who.int/publications/i/item/monitoring-progress-towards-universal-health-coverage-at-country-and-global-levels-framework-measures-and-targets [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boerma T., AbouZahr C., Evans D., et al. Monitoring intervention coverage in the context of universal health coverage. PLoS Med. 2014;11(9) doi: 10.1371/journal.pmed.1001728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO . World Health Organization; Geneva: 2013. Global action plan for the prevention and control of noncommunicable diseases 2013-2020. [Google Scholar]
- 8.World Health Organization . World Health Organization; Geneva, Switzerland: 2017. Tackling NCDs: ‘best buys' and other recommended interventions for the prevention and control of noncommunicable diseases. CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 9.WHO . World Health Organization; Geneva: 2014. Noncommunicable diseases global monitoring framework: indicator definitions and specifications. [Google Scholar]
- 10.Nguyen P.T., Gilmour S., Le P.M., et al. Trends in, projections of, and inequalities in non-communicable disease management indicators in Vietnam 2010-2030 and progress toward universal health coverage: a Bayesian analysis at national and sub-national levels. eClinicalMedicine. 2022;51 doi: 10.1016/j.eclinm.2022.101550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hambleton I.R., Caixeta R., Jeyaseelan S.M., et al. The rising burden of non-communicable diseases in the Americas and the impact of population aging: a secondary analysis of available data. Lancet Reg Health Am. 2023;21 doi: 10.1016/j.lana.2023.100483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allen L.N., Wigley S., Holmer H. Implementation of non-communicable disease policies from 2015 to 2020: a geopolitical analysis of 194 countries. Lancet Glob Health. 2021;9:e1528–e1538. doi: 10.1016/S2214-109X(21)00359-4. [DOI] [PubMed] [Google Scholar]
- 13.Allen L., Cobiac L., Townsend N. Quantifying the global distribution of premature mortality from non-communicable diseases. J Public Health. 2017;39:698–703. doi: 10.1093/pubmed/fdx008. [DOI] [PubMed] [Google Scholar]
- 14.WHO . World Health Organization; Geneva: 2021. Saving lives, spending less: the case for investing in noncommunicable diseases. [Google Scholar]
- 15.Ali M.K., Rabadán-Diehl C., Flanigan J., Blanchard C., Narayan K.M., Engelgau M. Systems and capacity to address noncommunicable diseases in low- and middle-income countries. Sci Transl Med. 2013;5:181. doi: 10.1126/scitranslmed.3005121. [DOI] [PubMed] [Google Scholar]
- 16.Zhou M., Wang H., Zeng X., et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394:1145–1158. doi: 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Health Commission of the People’s Republic of China . People’s Medical Publishing House; Beijing: 2022. Report on Chinese residents’ chronic diseases and nutrition 2020. [Google Scholar]
- 18.Liu S., Chen Z., Han L., et al. Integrated multisectoral non-communicable disease prevention and control in China: a review of agencies and policies. J Glob Health. 2020;10 doi: 10.7189/jogh.10.020304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Central Committee of Communist Party of China and the State Council . 2016. The “Healthy China 2030” blueprint.http://english.gov.cn/policies/latest_releases/2016/10/25/content_281475475062678.htm [Google Scholar]
- 20.Office of the State Council of China . 2017. Notice of the general office of the state council on printing and distributing China's Medium and long-term plan for prevention and treatment of chronic diseases (2017-2025)http://www.gov.cn/zhengce/content/201702/14/content_5167886.htm [Google Scholar]
- 21.National Health Commission . 2017. On the Health life style in the general population (2017-2025)http://www.nhc.gov.cn/jkj/s5878/201704/e73c1934c7f84c709e445f01bf832b17.shtml [Google Scholar]
- 22.Peng W., Chen S., Chen X., et al. Trends in major non-communicable diseases and related risk factors in China 2002–2019: an analysis of nationally representative survey data. Lancet Reg Health West Pac. 2023 doi: 10.1016/j.lanwpc.2023.100809. published online June 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang C., Yu H., Koplan J.P. Can China diminish its burden of non-communicable diseases and injuries by promoting health in its policies, practices, and incentives? Lancet. 2014;384:783–792. doi: 10.1016/S0140-6736(14)61214-9. [DOI] [PubMed] [Google Scholar]
- 24.Yang G., Kong L., Zhao W., et al. Emergence of chronic non-communicable diseases in China. Lancet. 2008;372:1697–1705. doi: 10.1016/S0140-6736(08)61366-5. [DOI] [PubMed] [Google Scholar]
- 25.Zhou Y., Li C., Wang M., et al. Universal health coverage in China: a serial national cross-sectional study of surveys from 2003 to 2018. Lancet Public Health. 2022;7:e1051–e1063. doi: 10.1016/S2468-2667(22)00251-1. [DOI] [PubMed] [Google Scholar]
- 26.Smith R. Why a macroeconomic perspective is critical to the prevention of noncommunicable disease. Science. 2012;337:1501–1503. doi: 10.1126/science.1222569. [DOI] [PubMed] [Google Scholar]
- 27.Zhang M., Wang L., Wu J., et al. Data resource profile: China chronic disease and risk factor surveillance (CCDRFS) Int J Epidemiol. 2022;51:e1–e8. doi: 10.1093/ije/dyab255. [DOI] [PubMed] [Google Scholar]
- 28.Wang L., Peng W., Zhao Z., et al. Prevalence and treatment of diabetes in China, 2013-2018. JAMA. 2021;326:2498–2506. doi: 10.1001/jama.2021.22208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang L., Zhou B., Zhao Z., et al. Body-mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004-18. Lancet. 2021;398:53–63. doi: 10.1016/S0140-6736(21)00798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Popkin B.M., Du S., Zhai F., et al. Cohort profile: the China health and nutrition survey--monitoring and understanding socio-economic and health change in China, 1989-2011. Int J Epidemiol. 2010;39:1435–1440. doi: 10.1093/ije/dyp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li Y., Zhang C., Zhan P., et al. Trends and projections of universal health coverage indicators in China, 1993-2030: an analysis of data from four nationwide household surveys. Lancet Reg Health West Pac. 2022;31 doi: 10.1016/j.lanwpc.2022.100646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Han S.M., Rahman M.M., Rahman M.S., et al. Progress towards universal health coverage in Myanmar: a national and subnational assessment. Lancet Glob Health. 2018;6:e989–e997. doi: 10.1016/S2214-109X(18)30318-8. [DOI] [PubMed] [Google Scholar]
- 33.Rahman M.S., Rahman M.M., Gilmour S., et al. Trends in, and projections of, indicators of universal health coverage in Bangladesh, 1995-2030: a Bayesian analysis of population-based household data. Lancet Glob Health. 2018;6:e84–e94. doi: 10.1016/S2214-109X(17)30413-8. [DOI] [PubMed] [Google Scholar]
- 34.National Bureau of Statistics of China Statistical yearbook of China. http://www.stats.gov.cn/tjsj/ndsj/
- 35.National Health Commission China health Statistics yearbook. http://www.nhc.gov.cn/mohwsbwstjxxzx/tjtjnj/new_list.shtml
- 36.WHO . World Health Organization; Geneva: 2018. 2018 Global reference list of 100 core health indicators (plus health-related SDGs) [Google Scholar]
- 37.Gelman A., Carlin J.B., Stern H.S., et al. 3rd ed. Chapman & Hall/CRC Press; London: 2013. Bayesian data analysis. [Google Scholar]
- 38.Hosseinpoor A.R., Bergen N., Schlotheuber A., et al. State of inequality in diphtheria-tetanus-pertussis immunisation coverage in low-income and middle-income countries: a multicountry study of household health surveys. Lancet Glob Health. 2016;4:e617–e626. doi: 10.1016/S2214-109X(16)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bertram M.Y., Sweeny K., Lauer J.A., et al. Investing in non-communicable diseases: an estimation of the return on investment for prevention and treatment services. Lancet. 2018;391:2071–2078. doi: 10.1016/S0140-6736(18)30665-2. [DOI] [PubMed] [Google Scholar]
- 40.Global Burden of Disease Health Financing Collaborator Network Trends in future health financing and coverage: future health spending and universal health coverage in 188 countries, 2016-40. Lancet. 2018;391:1783–1798. doi: 10.1016/S0140-6736(18)30697-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.GBD 2019 Universal Health Coverage Collaborators Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1250–1284. doi: 10.1016/S0140-6736(20)30750-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.China PEACE Collaborative Group. Zhou T., Wang Y., et al. Primary care institutional characteristics associated with hypertension awareness, treatment, and control in the China PEACE-Million Persons Project and primary health-care survey: a cross-sectional study. Lancet Glob Health. 2023;11:e83–e94. doi: 10.1016/S2214-109X(22)00428-4. [DOI] [PubMed] [Google Scholar]
- 43.Yip W., Fu H., Chen A.T., et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet. 2019;394:1192–1204. doi: 10.1016/S0140-6736(19)32136-1. [DOI] [PubMed] [Google Scholar]
- 44.Wang Z., Chen Z., Zhang L., et al. Status of hypertension in China: results from the China hypertension survey, 2012-2015. Circulation. 2018;137:2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 45.Lu J., Lu Y., Wang X., et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE Million Persons Project) Lancet. 2017;390:2549–2558. doi: 10.1016/S0140-6736(17)32478-9. [DOI] [PubMed] [Google Scholar]
- 46.Anjana R.M., Unnikrishnan R., Deepa M., et al. Metabolic non-communicable disease health report of India: the ICMR-INDIAB national cross-sectional study (ICMR-INDIAB-17) Lancet Diabetes Endocrinol. 2023;11:474–489. doi: 10.1016/S2213-8587(23)00119-5. [DOI] [PubMed] [Google Scholar]
- 47.Kraef C., Juma P.A., Mucumbitsi J., et al. Fighting non-communicable diseases in East Africa: assessing progress and identifying the next steps. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-003325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Niessen L.W., Mohan D., Akuoku J.K., et al. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda. Lancet. 2018;391:2036–2046. doi: 10.1016/S0140-6736(18)30482-3. [DOI] [PubMed] [Google Scholar]
- 49.Murphy A., Palafox B., Walli-Attaei M., et al. The household economic burden of non-communicable diseases in 18 countries. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2019-002040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kazibwe J., Tran P.B., Annerstedt K.S. The household financial burden of non-communicable diseases in low- and middle-income countries: a systematic review. Health Res Policy Syst. 2021;19:96. doi: 10.1186/s12961-021-00732-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xiong S., Cai C., Jiang W., et al. Primary health care system responses to non-communicable disease prevention and control: a scoping review of national policies in Mainland China since the 2009 health reform. Lancet Reg Health West Pac. 2022;31 doi: 10.1016/j.lanwpc.2022.100390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Meng Q., Mills A., Wang L., et al. What can we learn from China's health system reform? BMJ. 2019;365:l2349. doi: 10.1136/bmj.l2349. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.