Abstract
Purpose:
Body image is a major psychosocial concern for all cancer patients but can affect the adolescent and young adult (AYA) population in distinct ways. Similarly, the prospect of infertility and the fertility preservation process can create additional stress during cancer treatment. Discussions regarding infertility inherently implicate the body and its reproductive function, but downstream effects on self-perception have not been previously described. The aim of this study was to explore the experiences of AYAs as they considered their risk of infertility and options for fertility preservation (FP), specifically the ways in which this impacted body image and FP decision-making.
Methods:
AYA cancer patients (n = 27) aged 12–25 years whose cancer and treatment conferred risk of infertility were recruited through electronic health record query at an NCI-Designated Comprehensive Cancer Center. Participants completed semi-structured interviews, which were recorded, transcribed, and deductively coded for themes related to information needs, knowledge of treatment effects on fertility, and reproductive concerns after cancer. Emergent, inductive themes related to body image were identified.
Results:
Body image concerns, related to both physical appearance and body functioning emerged. Common concerns included anticipating change as it pertains to the body and its functions, physical discomfort, fear of judgment, and meeting expectations of the body. While these themes are broad in nature, they have been previously explored in relation to body image in general and their emergence in the oncofertility space provides guidance for further optimization of infertility and fertility preservation discussions.
Conclusions:
AYA cancer patients experience a multitude of body image related disturbances when faced with the possibility of infertility and fertility preservation. In identifying and exploring these themes, future opportunities for improving oncofertility practice and discussions among AYAs with a focus on body image positivity are called upon.
Keywords: adolescent, body image, fertility preservation, oncofertility, young adult
Introduction
Body image has been recognized as a major psychosocial concern for cancer patients and encompasses views on physical appearance as well as thoughts and feelings related to how one’s body functions.1 Significant alterations in appearance and body function can emerge with disease progression or with cancer-directed treatment and supportive measures. One’s body image is largely developed in adolescence and young adulthood with implications for self-identity and social relationships.2 As such, it is unsurprising that body image concerns affect adolescent and young adult (AYA) cancer patients in distinct ways when compared to an older cancer patient population.3
The risk of infertility due to diagnosis or prescribed curative treatment causes distress and uncertainty among AYA cancer patients.4 Concerns related to fertility can be present at the time of a cancer diagnosis and may persist into survivorship. In addition, increased reproductive concerns may portend increased depression and reduced quality of life.5 Fear of infertility is just one reproductive concern; the negative impact of infertility on romantic relationships and the ability to successfully parent and raise children are also considerations for cancer patients, including AYAs.6
The community of oncology providers recognizes the risk of infertility in the AYA population and this possibility is often included in the consent process and ideally further addressed by a reproductive specialist.7 Unfortunately, barriers to this specialized care exist and include time constraints, either during clinic visits specifically or due to an urgency to initiate treatment.8 To mitigate these barriers and to efficiently provide information regarding fertility, validated measures have been developed to better assess cancer-related reproductive concerns in the hopes of meeting the needs of AYAs.9 While recognition of these concerns is necessary, the subsequent discussions regarding infertility and potential fertility preservation (FP) will inherently implicate the body and its reproductive capability. As such, body image disturbances – related to both physical changes and changes in the body’s functional capacity – may arise.
The relationship between reproductive concerns, infertility, fertility preservation, and body image in AYAs with cancer is largely unknown. Cancer-directed therapy, including chemotherapy, radiation therapy and surgical intervention, can alter appearance and therefore body image, especially in the AYA population. It is therefore important to consider the additional and possibly exacerbating factor of infertility when assessing body image in the AYA cancer population. This study aimed to explore the experiences of AYAs as they considered their own risk of infertility and learned of the options for fertility preservation, specifically the ways in which this may have impacted body image and ultimately decisions to pursue FP.
Methods
Sample10
Participant recruitment occurred in adult and pediatric oncology units within an NCI-Designated Comprehensive Cancer Center from October 2019 to August 2020 (Figure 1). Eligibility criteria included: age 12 to 25 years, diagnosed with a malignancy in the previous 2 to 12 months, and at-risk for infertility due to prescribed curative treatment regimens that qualified them for referral to the institution’s fertility preservation program. Participants were identified via electronic health record (EHR) query based upon ICD-10 codes. Query results (n = 590) were screened by medical personnel and 521 patients were deemed ineligible. 69 patients were deemed potentially eligible. Study staff contacted the treating oncologist of potential patients via email and offered a 7-day opt-out period to decline participation on behalf of their patient if this was felt to be warranted. 9 patients were excluded based on their oncologist’s recommendation. As such, the 60 remaining eligible patients were contacted by phone one time per week for up to three weeks. Active non-respondents who declined to participate (n = 16), and passive non-respondents who did not respond after three contact attempts were eliminated (n = 17). Reasons for nonparticipation from the active non-responders were not systemically collected. A total of 27 participants were included in the final sample.
Figure 1.
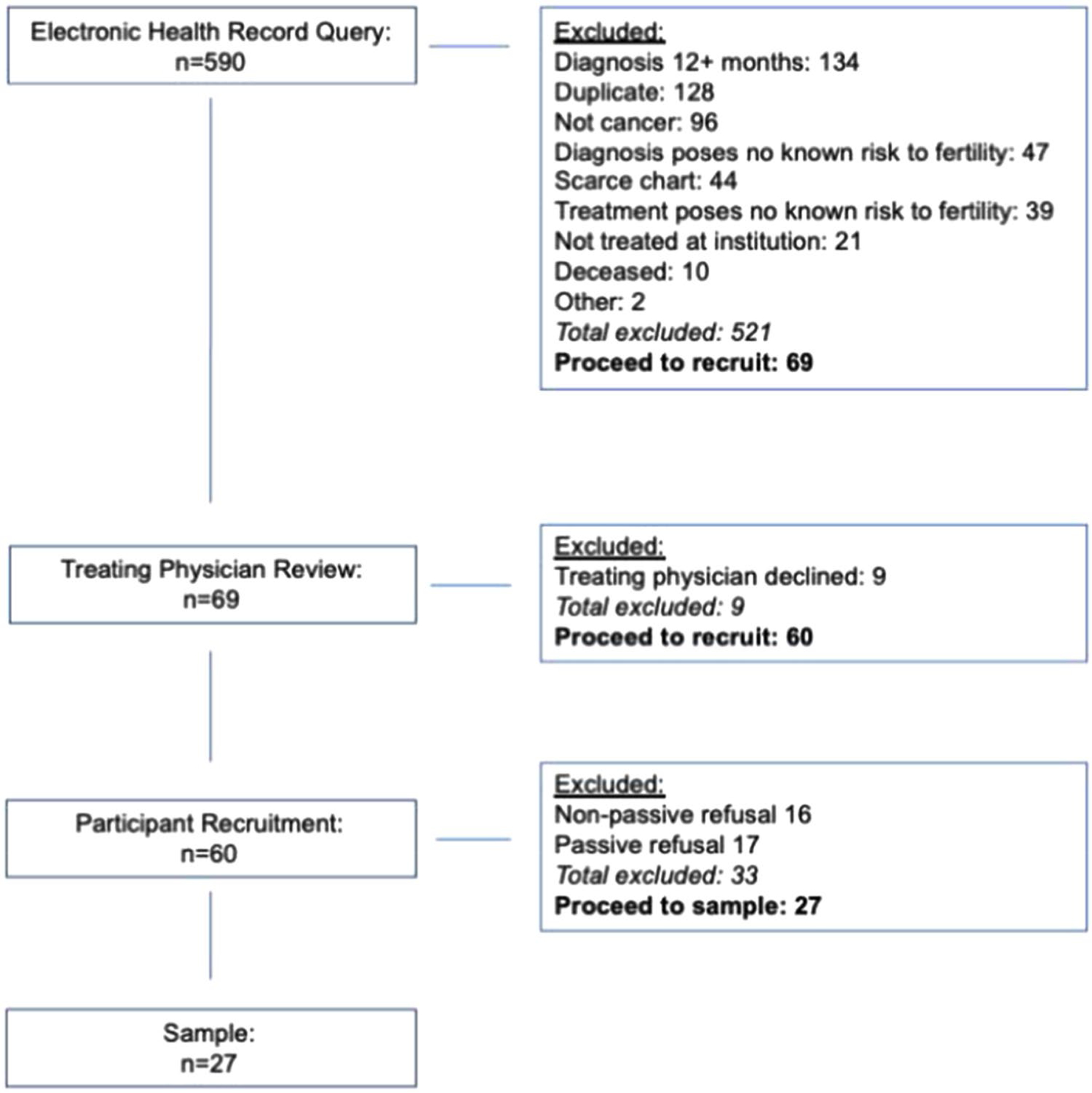
Recruitment of adolescents and young adults. Participants were recruited within an NCI-Designated Comprehensive Cancer Center and were identified via EHR query based upon ICD-10 codes. Query results (n = 590) were screened by medical personnel who eliminated n = 521 ineligible patients. N = 69 individuals were deemed eligible for recruitment. Study staff contacted eligible patients’ treating oncologists by email and offered a 7-day opt-out period. Nine eligible individuals were excluded in this manner. Remaining eligible patients (n = 60) were contacted by phone. Active non-respondents (n = 16), and passive nonrespondents were eliminated (n = 17). A total of n = 27 participants comprise the final sample. EHR, electronic health record.
Procedure10
Participants over 18 years were emailed/mailed copies of informed consent documents. Guardian consent/minor assent were sent to participants below the age of 18. Interviews were scheduled with one of four authors (NJL, DS, NI, AZ). Interviews consisted of administration of a battery of standardized instruments9,11–16 immediately followed by a semi-structured interview via HIPAA-approved confidential video-conferencing software, by telephone, in person on-site at the outpatient clinic. Interviews were audio-recorded. Semi-structured interviews were comprised of three major sections that addressed general cancer experience, goals and dreams for the future including desire to have a family someday, and experiences with FP. Examples of specific probes used by the authors conducting the interviews included the identification of any physical or emotional changes as a result of cancer-directed treatment, discussing the disclosure of infertility risk to romantic partners and addressing emotional reactions to learning about infertility risk and fertility preservation. Following conclusion of the interview, participants were provided with a $25 gift card. The local Institutional Review Board approved this study (HUM#00157267).
Data analysis
Demographic information collected from EHR and self-report included sex, race, age at diagnosis, clinical unit, cancer type, and whether FP occurred. In this study, qualitative findings from the semi-structured interviews are reported exclusively while quantitative findings from the questionnaires are not discussed in this analysis. Interviews were professionally transcribed by a HIPAA-compliant transcription service. Research assistants reviewed transcriptions for accuracy and de-identified transcripts. The authors CYT and DS independently coded 27 transcripts using a deductive coding schema derived from the empirical literature addressing information needs,11,12 knowledge about treatment effects,12–14 and reproductive concerns after cancer.9,15,16 Coders met monthly to discuss and resolve discrepancies. Final codes were compiled into a master document and the first author reviewed and extracted inductive codes which were then grouped into themes related to body image. An example of the deductive and inductive coding process is illustrated in Figure 2.
Figure 2.
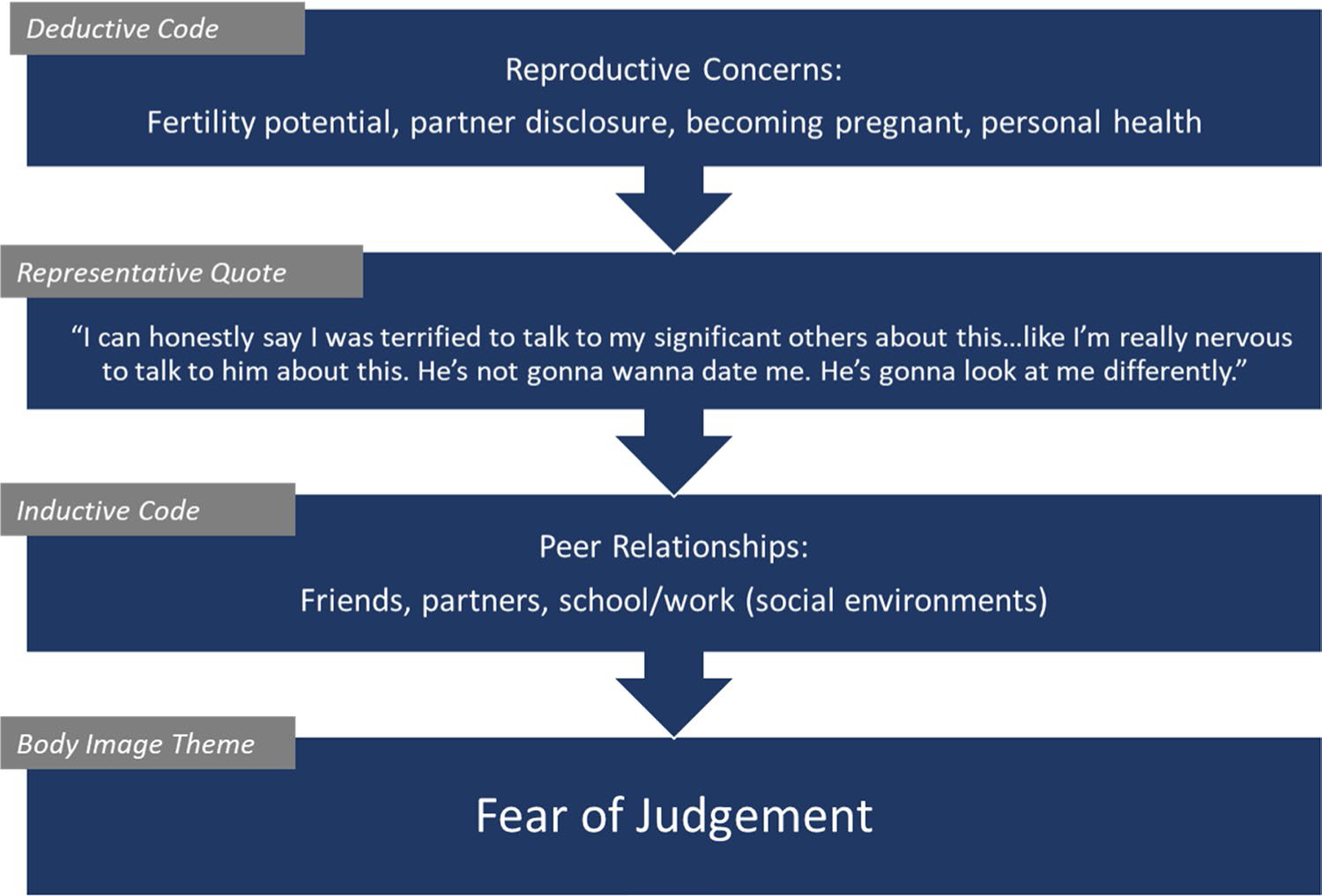
Example of deductive and inductive coding schema.
Results
Demographics
The sample included 63% male and 37% female respondents. At age of diagnosis, participants were 18–25 years (59%) and 12–17 years (41%). Racially, white participants comprised 78% and nonwhite participants comprised 22%. Roughly half of the sample (n = 14) received treatment in the adult clinical unit. Non-solid cancers constituted 52% of the cancer types. Most participants ages 18–25 (n = 11) elected to pursue FP, as did most participants ages 12–17 (n = 6) (Table 1).
Table 1.
Demographics of the adolescent and young adult cancer patient sample.
| # | % | |
|---|---|---|
| Sex | ||
| Male | 17 | 63 |
| Female | 10 | 37 |
| TOTAL | 27 | 100 |
| Age at diagnosis (years) | ||
| 18–25 | 16 | 59 |
| 12–17 | 11 | 41 |
| TOTAL | 27 | 100 |
| Race | ||
| White | 21 | 78 |
| Nonwhite | 6 | 22 |
| TOTAL | 27 | 100 |
| Clinical unit | ||
| Adult | 14 | 52 |
| Pediatric | 13 | 48 |
| TOTAL | 27 | 100 |
| Cancer type * | ||
| Non-solid tumor | 14 | 52 |
| Solid tumor | 13 | 48 |
| TOTAL | 27 | 100 |
| Preserved fertility (Yes/No) | ||
| 18–25 Yes | 11 | 41 |
| 18–25 No | 7 | 26 |
| 12–17 Yes | 6 | 22 |
| 12–17 No | 3 | 11 |
| TOTAL | 27 | 100 |
Cancer types: Hodgkin’s lymphoma n = 9; synovial sarcoma n = 3; osteosarcoma n = 3; acute lymphocytic leukemia, n = 3; acute myeloid leukemia n = 2; testicular n = 2; ovarian tumor n = 1; pineoblastoma n = 1; laryngeal n = 1; nasopharyngeal n = 1; nerve sheath tumor n = 1.
Emergent themes
Anticipating body changes
Recognizing and coping with anticipated changes to the body, both physically and in terms of function, emerged as a theme. One 23-year-old female participant discussed her process and realization of impending changes to her fertility during cancer treatment. She stated that “going back to when I was younger, I wasn’t sure if I wanted kids…As I’ve gotten older, I’m like, ‘Yeah, I think I do want kids.’ When I found out how this medicine [chemotherapy] can affect a woman’s body, I did start asking questions.” Another 24-year-old female participant receiving cancer treatment and potentially a stem cell transplant was surprised to learn “how things can change, and your whole anatomy can change, basically.”
For some, learning about the risk of infertility and FP prompted thoughts regarding future options and decision-making. When recalling initial FP discussions, one 17-year-old male respondent stated, “Yeah, I was a little bummed when I heard it ‘cause any loss of your body’s function…sucks ‘cause then you can—you have less options…I wanted to keep my options open.” Another 22-year-old female participant was struck by these conversations regarding reproduction and the way this altered her perception of her body’s functions and its potential to change. She noted that “you rarely think about your body other than as a machine to do things for you” and that learning about fertility risks “was a very big part” of treatment decision-making.”
A 17-year-old female participant was surprised to learn about the risk of infertility, stating that this prospect was “kind of crazy to think about. I would have never thought, being so young, to think about my future so heavily, something so crazy and life changing, I wouldn’t have thought I’d ever think about that.”
Discomfort
Discomfort in both experiencing one’s own body and discussing one’s body was noted by multiple participants in their conversations regarding reproductive concerns. This discomfort was largely reported when participants shared their experiences during the FP process. A 17-year-old male participant recalled the sperm banking procedure which took place in the hospital, stating that “Yeah, it was a little weird…They drew the curtain, but yeah, it was a little uncomfortable especially ‘cause it was a pretty small wing, and there’s other people, and there’s stuff goin’ on everywhere.” Another 16-year-old male had a similar experience during sperm banking due to a lack of privacy, recalling that he “just wanted to leave as quickly as possible…it was such a weird place.”
One 17-year-old female respondent noticed that “you gained a lot of weight for [FP]. I felt like I just weighed a lot more than what I originally did.” Another 17-year-old female respondent described FP as “very up and down” and explained the process in more detail, noting that:
It was a lot at first. All the medicines, giving yourself a shot, two shots every night…At the end, I actually had the ovarian hyper-stimulation thing, whatever it’s called. I didn’t feel good from that. I actually went into my first round of chemo right after that, and it’s not good. That was a lot to deal with, having that.
A sense of discomfort also extended to modesty or a lack thereof when discussing reproductive concerns. One 21-year-old male participant noted as much when thinking about the presence of his parents during these discussions. When asked if it was uncomfortable to have his parents present, he reported: “I guess a tiny bit uncomfortable, but basically, I threw out all modesty out the window when I had—when I knew something was wrong after the first surgery. I guess I’m starting to get my modesty back, but I basically just threw it all out the window.”
Fear of judgement
Participants described a fear of judgment when discussing both the possibility of infertility and the prospect of fertility preservation. A 23-year-old female respondent expressed concern regarding her potential infertility as she described her dating future, stating, “How am I gonna find a boy that likes me that’s okay with not having his own kids…He’s not gonna wanna date me. He’s gonna look at me differently.” Another 24-year-old male participant felt similarly, role-playing how a future discussion regarding fertility with a romantic partner may occur: “All right, if this becomes serious, if we get married, and we decide we wanna have a family, this is what my status is at. I know this ‘cause I’ve had medical issues, and I want you to know that, so that way you’re not disappointed.” A 16-year-old male participant noted that while he “was hoping to have kids sometime in the future,” a conversation with his girlfriend of six months and her expectations played a role in his decision to pursue sperm banking: “She really wants to have kids in the future. It’s weird thinking about that. We’re not probably gonna be having kids for multiple, multiple years.”
Other participants noted a fear of judgment for their decision to pursue fertility preservation. One 22-year-old female participant recalled the reactions of others, specifically family and friends, reporting:
They were like, ‘Why are you freezing your eggs? That’s gonna take another two to three weeks. You should just go to treatment right away. You’re risking her life.’ Then that made me parents not sure if I should freeze my eggs or not or if I should just go straight to chemo…I feel like it’s just so important for me to have children.
Failing to meet expectations of the body
Many participants discussed the expectations of the body’s ability to reproduce and their own ability to meet those expectations either naturally or with fertility preservation. These expectations were often held by AYAs themselves and they expressed sentiments of disappointment and inadequacy upon recognizing the possibility that these expectations may not be fulfilled. When considering adoption as an alternative option, one 22-year-old female participant noted that “there’s something so special about passing on parts of your personality and genes and appearance on to another human being.” Another 24-year-old female participant considered fertility and the ability to reproduce to be a “big part of yourself that everyone should have [a] right to” and lamented that with cancer treatment “it’s just being taken from you.” Another 20-year-old female respondent felt similarly when thinking about reproductive options, stating that “if it came down to it where I couldn’t [conceive], tried and tried the in vitro and natural and everything, and I still couldn’t [conceive], I would be open to adoption or something else…when I imagine my family, I imagine it being children of my own that I have.”
For some participants, including a 19-year-old male, the expectation to reproduce was held by others and the prospect of infertility and discussions regarding FP caused friction between family members:
He [my father] cared more about me producing a child than me not having cancer. That was something I fundamentally understood in that moment. It was so clear. It was so clear that for him me having children is just so much more important than me getting rid of the cancer in my body.
A 20-year-old-male participant also remarked upon interactions with family members as his parents relayed to him that “‘yeah, you should probably do it [FP] just in case—you never know’ …I mean, I think they want grandkids someday.”
Some participants discussed the general physical expectations of the body during reproduction and with fertility preservation more specifically. A 20-year-old-female respondent described the unpredictability associated with the FP process, stating that it “was up in the air on when my actual retrieval would be because it depended on my blood levels and the way my eggs looked and all that. It was just two weeks straight of, I don’t know, of worry and stuff.” This sentiment of meeting expectations was shared by a 17-year-old female participant undergoing fertility preservation. She shared that “my age is when I should be having kids…My body is at its peak right now for having kids.”
Discussion
This study makes a unique contribution to the existing empirical knowledge about the multiple aspects of body image that are affected when AYAs with cancer confront the possibility of infertility and the prospect of fertility preservation. Infertility has been described as an “identity shock” in which affected individuals have an alteration in their concept of self upon realizing a failure of the body to reproduce.17 This perception is based on both personal expectations as well as a societal expectation for natural reproduction.18 Furthermore, fertility preservation methods present their own unique challenges that impact body image, including physical changes such as weight gain, and emotional changes related to the unpredictability of the body’s response to these methods.19
Four major themes were identified among participants and these themes incorporated both physical and psychosocial components of body image. Common concerns included anticipating body changes, discomfort, fear of judgment, and failing to meet expectations of the body. While these themes are broad in nature, they have been previously explored in relation to body image and their emergence in terms of oncofertility provides novel guidance for further optimization of infertility and fertility preservation discussions.
Participants described their concerns regarding the failure to meet expectations of the body when faced with possible infertility and the resultant sense of failure should the goal of producing a genetically related family not occur. The sense of guilt and loss associated with the prospect of infertility is not uncommon and can lead to altered perceptions of one’s body and its capabilities.9 The reproductive expectations were held by AYAs, family members and society writ large. It may be that AYA patients with these expectations enter fertility preservation discussions with pre-conceived notions about what one’s body “should” be able to do, including reproduction. While these views may not have previously caused body image disturbances, confronting the risk of infertility may result in a negative perception of self and the body’s ability to reproduce. In addition, it may be that underlying body image disturbances not related to reproduction or a cancer diagnosis exist and shape reactions to possible infertility or FP. Both scenarios inform the need for a more complete assessment of overall psychosocial health, including thoughts about reproductive expectations and body image, may allow more tailored infertility and fertility preservation approaches that are sensitive to these concerns.
A new diagnosis of cancer in an AYA patient is certainly an emotionally challenging scenario but from a practical perspective, there are critical and time-sensitive medical decisions to be made to ensure the best opportunity for successful treatment outcomes. To this end, discussions of fertility preservation and their implications for body image disturbances and psychosocial health may be rushed or even omitted. Cancer clinic and visit restructuring may help alleviate these concerns. For example, a “dual clinic” with both medical oncology and reproductive medicine visits for new AYA cancer patients at the time of initial consultation could eliminate any delays due to the referral and scheduling process for a separate infertility and FP visit. In this model, treatment decisions would inform the FP discussions taking place on the same day and upon conclusion of this “dual visit,” a plan for both treatment and FP would be in place and known to all relevant providers. While such a workflow presents the risk for information overload for patients and families, involvement of a social worker in this setting may alleviate acute distress. While it is expected that patients will continue to follow with their medical oncologist as they continue their cancer-directed therapy or surveillance, it may not be routine for appointments to occur with a reproductive specialist, especially if fertility preservation is not immediately chosen. A short-term follow-up visit with a reproductive specialist or their support staff, whether in-person or virtual, may allow for a knowledge retention assessment regarding infertility risk and fertility preservation options and if performed within 1–2 wk, would likely not delay the initiation of cancer-directed therapy.
Participants also expressed concerns about anticipating body changes during cancer treatment. Preparing for body changes has been identified as a source of body image disturbances outside of both cancer and reproductive concerns. For example, puberty represents a period of rapid physical change for both male and female adolescents. These changes in body weight, height, and composition, along with the development of primary and secondary sex characteristics, have been associated with negative body image.20,21 The changes that come with both infertility and the process of fertility preservation can be difficult to both predict and accept in the AYA cancer population. Faced with these unknown scenarios, peer-support programs specifically focused on oncofertility may be useful in providing examples of positive outcomes.
General peer-support programs for patients with cancer have been shown to improve satisfaction with medical care, personal relationships, and overall mood.22 The American Cancer Society’s Reach to Recovery program has been in place for over 50 years for patients with breast cancer.23 Through an online matching system, interested patients are matched with a volunteer who has experienced a similar type of breast cancer and both parties can engage in telephone calls or online messaging. Peer support for infertility has also been investigated. A pilot study to assess the use and benefits of an online fertility-related peer support forum led to a positive experience for many participants, especially those participants who experienced higher psychological distress related to fertility concerns.24 With this preliminary success, it is reasonable to consider a similar program in the unique AYA cancer population. In the setting of AYA cancer and fertility concerns, such an intervention may take on a mentor/mentee structure in which mentors can address the changes to the body as well as the physical discomfort they endured and provide context for AYA cancer patients facing similar challenges.
Finally, AYA cancer patients expressed a fear of judgment; for some, this was related to a fear of future partners judging their infertility as a defect of the body. For others, there was a fear of being judged for prioritizing fertility preservation and the body’s ability to reproduce over more prompt cancer-directed therapy. Body image disturbances are closely linked to the perception of others and concern for their approval, and this is especially true in the AYA population. For example, many AYAs feel a need to present their best self in terms of appearance and ability on social media platforms and failing to do so can lead to both self-criticism and fear of judgment from others.25 This fear may impact engagement in romantic relationships and dating, especially in the younger segment of the AYA population. In relation to oncofertility, concerns about judgment of the body are not without merit as infertility-related stress has been shown to negatively impact relationships and marital satisfaction.26,27 This is largely due to the emotional distress that accompanies infertility-related stress, and body image concerns and subsequent judgment can affect both entities. Oncofertility teams are generally comprised of medical oncologists, reproductive medicine specialists and their respective nursing support.28 Incorporating a mental health provider, such as a social worker, into these teams may provide AYA patients with communication skills to discuss infertility with current loved ones and future romantic or sexual partners.
AYAs are an under-represented group in medical literature and their thoughts on infertility and fertility preservation in the setting of a cancer diagnosis are relatively unknown. A strength of this study is that it identifies real-world, granular concerns directly from AYA cancer patients. Limitations include a small number of patients that, as a result, does not allow for specific analysis of sub-populations that may experience body image differently, including the spectrum of gender identify and sexual orientation.29 While reasons for non-responders in our study were not systematically collected, further studies exploring the reasons for AYA active non-response are needed to better tailor recruitment strategies to gain a representative sample of a vulnerable population. Our study population includes AYA cancer patients ages 12–25. We note that the AYA population definition includes patients up to age 39. Our goal with this study was to capture a group of participants at a similar life stage and hopefully similar thought processes. In doing so, however, the concerns of the 26–39-year-old AYA population are not addressed. Also of note, body image disturbance emerged as an inductive theme post hoc as our interview protocol was not designed to incorporate specific measures related to body image disturbance. Future studies are advised to include validated measures of body image disturbance in studies addressing oncofertility.
This study underscores the varied body image concerns that arise in the AYA cancer population when facing infertility and the prospect of fertility preservation. Furthermore, it also provides an opportunity for further investigation into improving both the informational discussions and supportive interventions surrounding infertility and fertility preservation in a way that allows for body image positivity.
Acknowledgments
The authors thank the anonymous reviewers for their supportive feedback. The authors also thank Lisa Kelley, Anca Tilea, Kenneth Piehl, Julie Tumbarello, Dr. Erin Peregrine Antalis and the Master of Social Work research assistants for their contributions to the study. The authors thank our study participants for sharing their experiences to advance health care for adolescent and young adult cancer patients and survivors.
Funding
B.Z., R.C., E.B.W., L.H., E.E., A.Z., N.I., C.Y.T., D.S., and N.L.J. received funding from a Research Award (Innovation Grant) from the University of Michigan Rogel Cancer Center, under the National Cancer Institute Cancer Center Support Grant Award Number P30-CA-046592. N.J.L. received research support from the National Cancer Institute institutional training grant T32-CA-236621. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the National Cancer Institute. N.J.L was also supported by a Research Assistantship and by the Bobbe and Jon Bridge Award for Engaged Scholarship from the University of Michigan School of Social Work. A.Z. and N.J.L. received research support from the University of Michigan Vivian A. and James L. Curtis School of Social Work Center for Health Equity Research and Training, Signature Programs Initiatives.
Footnotes
Disclosure statement
The authors declare no conflict of interest.
References
- 1.Cash Thomas F, Linda Smolak, eds. Body Image: A Handbook of Science, Practice, and Prevention. New York: Guilford Press; 2011. [Google Scholar]
- 2.Lehmann V, Hagedoorn M, Tuinman MA. Body image in cancer survivors: a systematic review of case-control studies. J Cancer Surviv. 2015;9(2):339–348. doi: 10.1007/s11764-014-0414-y [DOI] [PubMed] [Google Scholar]
- 3.Moore JB, Canzona MR, Puccinelli-Ortega N, et al. A qualitative assessment of body image in adolescents and young adults (AYAs) with cancer. Psychooncol. 2021;30(4):614–622.doi: 10.1002/pon.5610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Irene Su H, Lee YT, Barr R. Oncofertility: meeting the fertility goals of adolescents and young adults with cancer. Cancer J. 2018;24(6):328–335. doi: 10.1097/PPO.0000000000000344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benedict C, Thom B, Friedman DN, Pottenger E, Raghunathan N, Kelvin JF. Fertility information needs and concerns post-treatment contribute to lowered quality of life among young adult female cancer survivors. Support Care Cancer. 2018;26(7):2209–2215. doi: 10.1007/s00520-017-4006-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gorman JR, Bailey S, Pierce JP, Su HI. How do you feel about fertility and parenthood? The voices of young female cancer survivors. J Cancer Surviv. 2012;6(2):200–209. doi: 10.1007/s11764-011-0211-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murpy D, et al. The need for reproductive and sexual health discussions with adolescent and young adult cancer patients. Contraception. 2013;88:215–220. [DOI] [PubMed] [Google Scholar]
- 8.Flink DM, Sheeder J, Kondapalli LA. A review of the oncology patient’s challenges for utilizing fertility preservation services. J Adolesc Young Adult Oncol. 2017;6(1):31–44. doi: 10.1089/jayao.2015.0065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gorman JR, Pan-Weisz TM, Drizin JH, Su HI, Malcarne VL. Revisiting the reproductive concerns after cancer (RCAC) scale. Psychooncol. 2019;28(7):1544–1550. doi: 10.1002/pon.5130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levin J, et al. Banking on fertility preservation: financial concern for adolescent and young adult cancer patients considering oncofertility services. J Adolesc Young Adult Oncol. 2023. Jan 5. doi: 10.1089/jayao.2022.0055. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oosterhuis BE, Goodwin T, Kiernan M, Hudson MM, Dahl GV. Concerns about infertility risks among pediatric oncology patients and their parents. Pediatr Blood Cancer. 2008;50(1):85–89. doi: 10.1002/pbc.21261 [DOI] [PubMed] [Google Scholar]
- 12.Johnson AC, Mays D, Rehberg K, Shad A, Tercyak KP. Knowledge and beliefs about oncofertility and associations with quality of life among adolescent and young adult survivors of pediatric cancer. J Adolesc Young Adult Oncol. 2018;7(4):424–429. doi: 10.1089/jayao.2018.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meneses K, McNees P, Azuero A, Jukkala A. Development of the fertility and cancer project: an internet approach to help young cancer survivors. Oncol Nurs Forum. 2010;37(2):191–197. doi: 10.1188/10.ONF.191-197 [DOI] [PubMed] [Google Scholar]
- 14.Jukkala A, Meneses K, Azuero A, Cho J, McNees P. Development of the knowledge of fertility and fertility preservation scale. Nursing: Research and Reviews. 2012; 2:1–7. doi: 10.2147/NRR.S28248 [DOI] [Google Scholar]
- 15.Gorman JR, Su I, Hsieh M. Measuring reproductive concerns among young adult male cancer survivors: preliminary results. Fertility Sterility. 2017;108(3):e185–e186. doi: 10.1016/j.fertnstert.2017.07.551 [DOI] [Google Scholar]
- 16.Gorman JR, Su HI, Pierce JP, Roberts SC, Dominick SA, Malcarne VL. A multidimensional scale to measure the reproductive concerns of young adult female cancer survivors. J Cancer Surviv. 2014;8(2):218–228. doi: 10.1007/s11764-013-0333-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clarke LH, et al. The continuity and discontinuity of the embodied self in infertility. Can Rev Sociol. 2006;43(1):95–113. doi: 10.1111/j.1755-618X.2006.tb00856.x [DOI] [Google Scholar]
- 18.Behruzi R, Hatem M, Goulet L, et al. Understanding childbirth practices as an organizational cultural phenomenon: a conceptual framework. BMC Pregnancy Childbirth. 2013;13:205. doi: 10.1186/1471-2393-13-205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumar P, Sait SF, Sharma A, Kumar M. Ovarian hyperstimulation syndrome. J Hum Reprod Sci. 2011;4(2):70–75. doi: 10.4103/0974-1208.86080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee JM, Appugliese D, Kaciroti N, Corwyn RF, Bradley RH, Lumeng JC. Weight status in young girls and the onset of puberty. Pediatrics. 2007;119(3):e624–e630. doi: 10.1542/peds.2006-2188 [DOI] [PubMed] [Google Scholar]
- 21.McCabe MP, Ricciardelli LA. A Longitudinal study of pubertal timing and extreme body change behaviors among adolescent boys and girls. Adolescence. 2004;39(153):145–166. [PubMed] [Google Scholar]
- 22.Ashbury FD, Cameron C, Mercer SL, et al. One-on-one peer support and quality of life for breast cancer patients. Patient Educ Couns. 1998;35(2):89–100. doi: 10.1016/s0738-3991(98)00035-4 [DOI] [PubMed] [Google Scholar]
- 23.“How does the Reach to Recovery program support people facing breast cancer?”. American Cancer Society. https://www.cancer.org/support-programs-and-services/reach-to-recovery.html. [Google Scholar]
- 24.Grunberg PH, Da Costa D, Dennis C-L, O’Connell S, Lahuec A, Zelkowitz P. ‘How did you cope with such concerns?’: insights from a monitored online infertility peer support forum. Human Fertility (Camb). 2023. Feb; 26(1):69–83. doi: 10.1080/14647273.2021.1959952. Epub 2021 Aug 4. [DOI] [PubMed] [Google Scholar]
- 25.Young G, Smith M, Batten J. “Social media makes it inevitable to feel bad about your body”: examining self-presentation and body image of young collegiate females. Youth. 2022;2(3):217–235. doi: 10.3390/youth2030016 [DOI] [Google Scholar]
- 26.Gana K, Jakubowska S. Relationship between infertility-related stress and emotional distress and marital satisfaction. J Health Psychol. 2016;21(6):1043–1054. doi: 10.1177/1359105314544990 [DOI] [PubMed] [Google Scholar]
- 27.Anderson KM, Sharpe M, Rattray A, et al. Distress and concerns in couples referred to a specialist infertility clinic. J Psychosom Res. 2003;54(4):353–355. doi: 10.1016/s0022-3999(02)00398-7 [DOI] [PubMed] [Google Scholar]
- 28.Woodruff TK. Oncofertility: a grand collaboration between reproductive medicine and oncology. Reproduction. 2015;150(3):S1–S10. doi: 10.1530/REP-15-0163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sampson A, Block R, Lake PW, et al. “No one size fits all” a multi-method survey of oncology allied health professionals experiences with lesbian, gay, bisexual, transgender/queer questioning adolescent, and young adult patients with cancer and reproductive and sexual health. J Adolesc Young Adult Oncol. 2023;12(2):250–258. doi: 10.1089/jayao.2021.0208 [DOI] [PMC free article] [PubMed] [Google Scholar]


