Abstract
Open-globe injuries (OGI) can lead to significant visual impairment. The Ocular Trauma Score (OTS) is the most widely recognized tool for predicting visual outcomes. This review aimed to identify prognostic factors and assess the effectiveness of the OTS in predicting visual outcomes. Twenty-one articles published on PubMed and Google Scholar were analyzed. Initial visual acuity and the zone of injury were found to be the most significant prognostic factors for OGI. Other significant prognostic factors include retinal detachment/involvement, relative afferent pupillary defect, vitreous hemorrhage, vitreous prolapse, type of injury, hyphema, lens involvement, and duration from incidence of OGI to vitrectomy. Of the 21 studies evaluated, 11 investigated the effectiveness of OTS. Four studies concluded that OTS was effective overall, while six studies suggested that it was only useful in certain OGI categories. Thus, there is a need for further research to develop an optimized ocular trauma prognosticating system.
Keywords: Ocular trauma, open globe injury, prognostic factors
Open-globe injuries (OGI) are a significant public health problem worldwide and a leading cause of monocular blindness.[1,2,3] OGI refers to full-thickness injuries to the eye wall, caused by either blunt or sharp objects, including penetrating or perforating injuries, lacerations, and intraocular foreign bodies. OGI is classified under the Birmingham Eye Trauma Terminology (BETT) system, which is widely recognized as a standard classification system for ocular injuries. In contrast, closed-globe injuries are injuries that do not penetrate the eye wall.[4]
Although the incidence rate of OGI is relatively low, at 3.5 per 100,000 people globally, the consequences can be devastating, leading to significant morbidity and even permanent disability.[5] The potential for vision loss is a primary concern as OGI tend to have poorer visual outcomes than closed-globe injuries.[6] Early diagnosis and management are critical in preventing vision loss.
The Ocular Trauma Score (OTS) helps clinicians predict the final visual acuity of patients with ocular trauma.[7] OTS is calculated using several factors, including initial visual acuity, presence of globe rupture, endophthalmitis, perforating injury, retinal detachment, and relative afferent pupillary defect (RAPD).[8] The OTS classifies the injury into five OTS categories and prognosticates the injury based on the derived OTS score. A higher OTS score correlates to a better predicted prognosis, whereas a lower OTS score correlates to a worse predicted prognosis. The OTS enables clinicians to make informed decisions regarding the management of ocular trauma patients and provides valuable guidance for counseling patients and their families.[9]
Numerous studies have been conducted to identify the prognostic factors for OGI and evaluate the predictive value of the OTS.[6,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28] Among the factors identified in these studies, initial visual acuity and the zone of injury are the most significant prognostic factors for OGI. Other prognostic factors include retinal detachment or involvement, RAPD, vitreous hemorrhage, vitreous prolapse, type of injury, hyphema, and lens involvement.
In addition, the predictive value of the OTS has been extensively studied.[12,14,18,19,20,21,22,23,24,26,28] While some studies have concluded overall effectiveness, others have suggested usefulness only in certain categories. These findings suggest that the OTS has variable predictive value, and there is a need for further research to develop an optimized prognosticating system for ocular trauma.
Therefore, it is crucial to identify prognostic factors that can help healthcare providers deliver efficient and effective care to OGI patients. By examining studies from various locations and contexts, the hope is to identify factors that are broadly applicable and can inform best practices for OGI care. In addition to a literature review, this article explores the predictive value of the OTS. By analyzing the effectiveness of the OTS in different contexts, this article aims to provide further guidance for healthcare providers in caring for OGI patients.
This article aims to support healthcare providers in delivering the best possible care to patients with OGI. By identifying prognostic factors and evaluating predictive tools such as the OTS, it aims to improve outcomes and quality of life for those affected by OGI. Early diagnosis, prompt treatment, and appropriate follow-up are critical for maximizing visual outcomes and improving the quality of life for patients with ocular trauma.
Methods
Search strategy: The literature search was conducted using the electronic databases PubMed and Google Scholar. The search was conducted using the keywords “prognostic factors” and “open globe injuries.”
Inclusion criteria: The papers that were considered for review had to be from/published in peer-reviewed journals. The review was limited to papers published in the year 2010 or later to ensure that the findings were current. The titles and abstracts were also screened to ensure that they were relevant to the topic. Only articles that focused on the prognostic factors of OGI were selected for review.
Exclusion criteria: Non-English language literature was excluded. Papers that did not meet the inclusion criteria were also excluded.
Data extraction: Information was extracted from each selected paper, including the study type, country of study, sample size, mean or median age of subjects, gender proportion of subjects, and significant findings. These data were then compiled into a table for ease of comparison and analysis.
Review of articles: After compiling the data, significant findings from each paper were reviewed in detail. In particular, prognostic factors identified by the studies and their potential impact on visual outcomes were noted. In addition, studies that investigated the predictive value of the OTS were reviewed to determine the effectiveness of this tool in different contexts.
Synthesis of results: Finally, the results of the studies were synthesized to identify common themes and factors that were consistently associated with poor visual outcomes in OGI. These findings were then used to develop recommendations for healthcare providers in managing patients with these types of injuries.
The study design is shown in Fig. 1.
Figure 1.
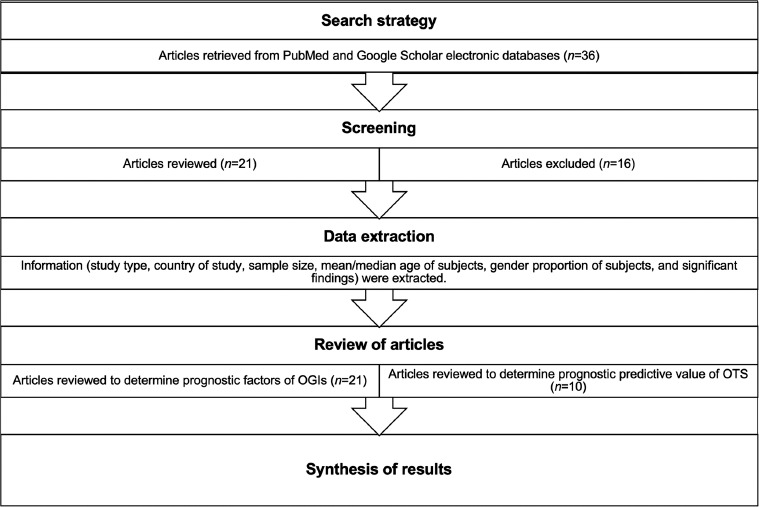
Study design
Results
In total, 21 articles (n = 21) were reviewed. These comprised two prospective cohort studies and 19 retrospective cohort studies. In 19 of these studies, data on eyes from all age groups were analyzed, while two studies investigated the pediatric population specifically. In these studies, the visual outcome was assessed in terms of the final best correct visual acuity (BCVA) of the subjects post treatment.
Prognostic factors of OGI
The key findings from the papers are summarized in Table 1.
Table 1.
Findings from cohort studies (n=21) elaborating on the prognostic factors of OGI
| Study | Study type | Country | Sample size | Age (years) | Gender | Findings (Prognostic factors of OGI) |
|---|---|---|---|---|---|---|
| Toh ZH et al. (2022)[11] | Retrospective | India | 791 | Mean 23.9±19.4 | Male 70.6% Female 29.4% |
Initial visual acuity (VA), Zone III injuries, corneoscleral wound, large wound size, presence of post-traumatic infections |
| Bruce CN et al. (2022)[12] | Retrospective | USA | 15 | Mean 6.97 | NIL | Relative afferent pupillary defect (RAPD), zone of injury |
| Hoskin AK et al. (2021)[13] | Retrospective | India, Nepal, Singapore, Australia, Argentina, Malaysia, China, Indonesia and USA | 746 | Median 35.9±20.0 | Male 85.8% Female 14.2% |
Poor prognosis: female gender, presence of RAPD, eyelid injury |
| Wang SY et al. (2021)[14] | Retrospective | Malaysia | 39 | Mean 34.9±21.7 | Male 84.6% Female 15.4% |
Initial VA, OTS |
| Mayer CS et al. (2021)[15] | Retrospective | Germany | 147 | Mean 42.9±22.2 | Male 78.2% Female 21.8% |
Poor prognosis: posterior segment involvement, retinal/optic nerve involvement Good prognosis: Good initial corrected distance visual acuity (CDVA), OGI affecting only Zones I and II |
| Puodžiuvienė E et al. (2021)[16] | Retrospective | Lithuania | 160 | Mean 41.9 | Male: female ratio 8.4:1 | Initial VA, iris dialysis, hypotony, vitreous hemorrhage, vitreous prolapse at presentation |
| Ng HR et al. (2021)[17] | Retrospective | Malaysia | 118 | Predominant age group: 21-30 | Male 88.1% Female 11.9% |
Preoperative VA, presence of RAPD, vitreous loss |
| Demir M et al. (2021)[18] | Retrospective | Finland | 118 | Mean 33.4±4.8 | Male: female ratio 4.6:1 | Poor prognosis: best corrected visual acuity (BCVA) <1/10, ocular trauma score category 1, perforating OGI, wound location of Zone II and III, additional vitreoretinal surgery required, retinal detachment, vitreous hemorrhage, lens damage |
| Toh ZH et al. (2020)[19] | Prospective | India | 42 | Mean 22.81 (males), 28.6 (females) | Male 76.2% Female 23.8% |
Preoperative VA, involvement of visual axis, hyphema, retinal detachment |
| Guzmán-Almagro E et al. (2020)[20] | Retrospective | Spain | 104 | Median 41 | Male 79.8% Female 20.2% |
Preoperative VA, OTS |
| He Y et al. (2020)[10] | Prospective | China | 53 | Mean 46.7±11.4 years in the early surgery group Mean 42.3±10.3 in the late surgery group |
Early surgery group – Male 100%; Female 0% Late surgery group – Male 92.0%; Female 8.0% |
Good prognosis: early vitrectomy after presentation of OGI |
| Fujikawa A et al. (2018)[6] | Retrospective | Japan | 59 | Mean 56.7±21.8 years in the light perception (LP) group; 62.3±21.7 years in the no light perception (NLP) group | Male 66.1% Female 33.9% |
Poor prognostic factors: Zone III injuries Globe rupture Poor VA at first visit History of penetrating keratoplasty Retinal detachment Vitreous hemorrhage Dislocation of crystalline lens Good prognostic factor: pars plana vitrectomy (PPV) performed if posterior segment involved |
| Guven S et al. (2019)[21] | Retrospective | Turkey | 633 | Mean 24.37±11.1 | Male: female ratio 18.6:1 | Poor prognosis: OTS category 1, initial VA, zone of injury, additional surgeries (PPV), initial lens damage |
| Okamoto et al. (2018)[22] | Retrospective | Japan | 374 | Mean 56.8±22.1 | Male 73.5% Female 26.5% |
Initial visual acuity, type of injury (rupture), retinal detachment, proliferative vitreoretinopathy |
| Page RD et al. (2016)[23] | Retrospective | USA | 103 | Mean 41.8±22 | Male 78.1% Female 21.9% |
Pre-op BCVA, OTS |
| Yu M et al. (2015)[24] | Retrospective | China | 298 | Mean 45.46±17.48 | Male 83.56% Female 16.44% |
Independent risk factors: initial VA, relative afferent papillary defect (RAPD), zone of injury Other risk factors: vitreous haemorrhage, lens injury, endophthalmitis, hyphema, retinal detachment |
| Liu X et al. (2014)[25] | Retrospective | China | 137 | Mean 11.57±4.19 | Male 84.7% Female 15.3% |
Independent risk factors: poor presenting VA, posterior wound location Other risk factors: younger age at presentation, injuries caused by blunt or missile objects, hyphema, vitreous haemorrhage, and surgical intervention of pars plana vitrectomy (PPV) (However, with the advances in technology, PPV has an important role in management of injured eyes and improving visual outcomes.) |
| Agrawal R et al. (2013)[26] | Retrospective | Singapore | 172 | Mean 36.67 | Male 96.5% Females 3.5% |
Poor prognostic factors: poor initial VA, presence of RAPD, posterior extent of wound, vitreous loss, vitreous haemorrhage, traumatic cataract, hyphema IOFB had no impact on final VA regardless of zone of injury |
| Bauza AM et al. (2012)[27] | Retrospective | USA | 148 | Mean 35.9±14.3 | Male 81.8% Female 18.2% |
Poor prognosis: initial VA of NLP, Zone III injury Good prognosis: penetrating injuries have better prognosis than rupture or perforating injuries |
| Tök OY et al. (2011)[33] | Retrospective | Turkey | 313 | Mean 32.01±21.04 | Male 73.2% Female 26.8% |
Initial VA, retinal detachment, vitreous prolapse |
| Han SB et al. (2010)[28] | Retrospective | Korea | 194 | Mean 38.2±17.8 | Male 82.5% Female 17.5% |
Initial visual acuity, presence of retinal detachment, relative afferent papillary defect, and wound length (>10 mm is considered large) |
Out of the 21 articles reviewed, 85.7% of them cited initial visual acuity as a prognostic factor for OGI. In addition, 47.6% of the studies found that the zone of injury is a prognostic factor for OGI – with zone III injuries being a poor prognostic factor. Furthermore, 33.3% of the studies identified retinal detachment/involvement as a prognostic factor for OGI, while 28.6% of them identified RAPD and/or vitreous hemorrhage as prognostic factors. Moreover, 23.8% of the studies also identified vitreous prolapse, type of injury, hyphema, and/or lens involvement as prognostic factors. One study (4.8%) also identified duration from incidence of OGI to vitrectomy as a prognostic factor. In relation to the type of injury, globe ruptures were found to be a poor prognostic factor in OGI.
Other prognostic factors identified include the need for additional surgeries, wound size, associated infection(s), hypotony, visual axis involvement, and the presence of post-OGI complications of proliferative vitreoretinopathy. With regard to the need for additional surgeries, the study by Fujikawa et al. (2018)[6] found that the execution of pars plana vitrectomy (PPV) is a good prognostic factor if the posterior segment is involved. The study by He Y et al. (2020)[10] also found that early PPV conducted <10 days from the onset of OGI is a good prognostic factor.
In particular, the studies by Yu M et al. (2015)[24] and Liu X et al. (2014)[25] cited initial visual acuity and zone of injury as independent prognostic factors for OGI. In addition, the paper by Yu M et al. (2015)[24] also identified RAPD as an independent prognostic factor for OGI.
The breakdown of the findings is presented in Table 2.
Table 2.
Breakdown of the prognostic factors identified by the 20 reviewed articles
| Prognostic factor identified | Number of studies |
|---|---|
| Initial visual acuity | 18 (90%) |
| Zone of injury | 10 (50%) |
| Retinal detachment/involvement | 7 (35%) |
| RAPD | 6 (30%) |
| Vitreous hemorrhage | 6 (30%) |
| Vitreous prolapse | 4 (25%) |
| Type of injury | 4 (25%) |
| Hyphaema | 4 (25%) |
| Lens involvement | 4 (25%) |
| Need for additional surgeries | 3 (12%) |
| Wound size | 2 (10%) |
| Associated infection(s) | 2 (10%) |
| Hypotony | 1 (5%) |
| Visual axis involvement | 1 (5%) |
| Proliferative vitreoretinopathy | 1 (5%) |
The findings above apply to the general population and are not limited to any demographic.
Prognostic predictive value of OTS
Of the 21 articles reviewed, 10 investigated the prognostic predictive value of the OTS (n = 10).
The OTS developed by Kuhn et al. (2002) calculates a raw score for the injured eye based on certain prognostic factors – initial visual acuity, presence of globe rupture, endophthalmitis, perforating injury, retinal detachment, and RAPD[7,8] These factors were also identified by the papers analyzed in this review as prognostic for OGI. The scoring system is elaborated on in Tables 3 and 4.
Table 3.
Computational method to obtain the raw score sum of OTS
| Initial visual factor | Raw points |
|---|---|
| Initial raw score | NPL=60 |
| PL/HM=70 | |
| 1/200 to 19/200=80 | |
| 20/200 to 20/50=90 ≥20/40=100 | |
| Globe rupture | -23 |
| Endophthalmitis | -17 |
| Perforating injuries | -14 |
| Retinal detachment | -11 |
| RAPD | -10 |
Raw score sum=Sum of raw points above
Table 4.
Probability of achieving respective visual acuity category at 6 months follow-up based on OTS score[8]
| Raw score sum | OTS Score | NPL | PL/HM | 1/200-19/200 | 20/200-20/50 | ≥20/40 |
|---|---|---|---|---|---|---|
| 0-44 | 1 | 73% | 17% | 7% | 2% | 1% |
| 45-65 | 2 | 28% | 26% | 18% | 13% | 15% |
| 66-80 | 3 | 2% | 11% | 15% | 28% | 44% |
| 81-91 | 4 | 1% | 2% | 2% | 21% | 74% |
| 92-100 | 5 | 0% | 1% | 2% | 5% | 92% |
NPL: NIL perception of light; PL: Perception of light; HM: Hand movements
Four studies, namely Bruce CN et al. (2022),[12] Guzmán-Almagro E et al. (2020),[20] Page RD et al. (2016),[23] and Yu M et al. (2015),[24] concluded that the OTS is generally effective in predicting the final visual acuity of the subjects.
In contrast, six studies concluded that the prognostic predictive value of the OTS score is limited to certain categories. Studies by Wang SY et al. (2021),[14] Demir M et al. (2021),[18] Guven S et al. (2019),[21] and Han SB et al. (2010)[28] showed that the OTS is effective in predicting the final visual acuity of subjects with a higher OTS score. The study by Agrawal R et al. (2013)[26] concluded that the OTS score only has predictive value in OTS categories 2, 4, and 5. In contrast, the study by Toh ZH et al. (2020)[19] found that the OTS score has predictive value in subjects with a lower OTS score.
The findings derived from the reviewed studies are further elaborated on in Table 5.
Table 5.
Findings from cohort studies elaborating on the prognostic predictive value of the Ocular Trauma Score (OTS) by Kuhn et al. (2002)[7]
| Study | Study design | Country | Sample size | Age (years) | Gender | Findings (Predictive value of OTS) |
|---|---|---|---|---|---|---|
| Bruce CN et al. (2022)[12] | Retrospective | USA | 15 | Mean 6.97 | NIL | OTS is effective in predicting final VA even outside of the age ranges for which they have been created. |
| Wang SY et al. (2021)[14] | Retrospective | Malaysia | 39 | Mean 34.9±21.7 | Male 84.6% Female 15.4% |
A higher OTS category correlates with better final VA, consistent with the OTS study. |
| Demir M et al. (2021)[18] | Retrospective | Finland | 118 | Mean 33.4±4.8 | Male: female ratio 4.6:1 | Considerable outcome in the prediction of final visual acuity (FVA) was seen only in OTS categories 4 and 5, which might be due to relatively larger sample sizes in OTS category 1 and 2. Cases in OTS category 1 showed a poor prognosis on FVA. |
| Toh ZH et al. (2020)[19] | Prospective | India | 42 | Mean 22.81 (males), 28.6 (females) | Males 76.2% Females 23.8% |
For OTS scores 1 and 2, the percentage differences between the observed and expected proportions were not statistically significant. For OTS score 3, the difference in frequencies was statistically significant (P=0.0004). For the remaining categories, the numbers of eyes were too small for comparison analysis. |
| Guzmán-Almagro E et al. (2020)[20] | Retrospective | Spain | 104 | Median 41 | Males 79.8% Females 20.2% |
OTS is a useful indicator in predicting final visual outcome. |
| Guven S et al. (2019)[21] | Retrospective | Turkey | 633 | Mean 24.37±11.1 | Male: female ratio 18.6:1 | The prediction of final VA with OTS was not valuable except for OTS category 5, possibly due to relatively higher (69.3%) rates of OTS category 1 and 2 cases – which already have a poor functional prognosis – in this study. |
| Page RD et al. (2016)[23] | Retrospective | USA | 103 | Mean 41.8±22 | Male 78.1% Female 21.9% |
This study adds to the evidence in the literature that the OTS predicts VA outcome |
| Yu M et al. (2015),[24] | Retrospective | China | 298 | Mean 45.46±17.48 | Male 83.56% Female 16.44% |
The OTS correlated with final VA (r=0.988, P=0.000). |
| Agrawal R et al. (2013)[26] | Retrospective | Singapore | 172 | Mean 36.67 | Male 96.5% Females 3.5% |
In most of the table, there was complete agreement between OTS in this study with USEIR OTS but with the following exceptions: OTS 1: Recovery of 20/200 or better was predicted in 23% of patients in USEIR data as against 6% in this study OTS 3: Vision outcome was LP/HM in 11% of patients in USEIR whereas it was 0% in this study |
| Han SB et al. (2010)[28] | Retrospective | Korea | 194 | Mean 38.2±17.8 | Male 82.5% Female 17.5% |
Final VA assessed were comparable with those of the OTS study. Moreover, three of the four predictive factors of final VA demonstrated in multivariate analysis in this study were included in the parameters of OTS – showing the reliability of the system. Final VA outcomes of categories 1 and 2 were better in this study compared to those in OTS study, possibly due to aggressive surgical intervention. |
Discussion
The analysis of 21 articles on OGI revealed several significant prognostic factors. This study highlights that initial visual acuity and the zone of injury are key indicators for predicting the prognosis of OGI. The presence of retinal detachment, retinal artery occlusion, vitreous hemorrhage, and RAPD are also identified as important factors that can be used to prognosticate OGI. Furthermore, other possible factors, such as vitreous prolapse, type of injury, hyphema, lens involvement, and duration from incidence of OGI to vitrectomy can be studied further to gain a better understanding of their prognostic value.
In addition, the review of ten articles on the OTS revealed differing conclusions about its effectiveness. There is no consensus about which OTS score categories have significant prognostic value based on the data analyzed in the respective studies.
In this review, only 2 out of 21 articles were based on prospective data. The heavy reliance on retrospective data limits the accuracy of the results due to a lack of information as described by Nagurney JT et al. (2008).[29] For example, the treatment options that the patients received might not have been properly documented as cited by Mayer CS et al. (2021),[15] Puodžiuvienė E et al. (2021),[16] Ng HR et al. (2021),[17] and Bauza AM et al. (2012).[27] In addition, the lack of standardization could have led to discrepancies in data collection and subsequently analysis, thus compromising on data quality and accuracy of results.
Furthermore, only 2 out of 21 articles focused on the pediatric population,[12,25] and there are no other papers that had a specific focus on other age groups. It should be noted that there could be other underlying factors affecting the outcomes of OGI in different demographics;[30] hence, the different demographic groups (e.g., age and ethnicity) should be studied in detail in future studies. Moreover, the different mechanisms of injury have not been well explored. Different mechanisms of injury could lead to different visual outcomes, and this could lead to variation in the conclusions drawn.[31]
Apart from the study by Hoskin AK et al. (2021),[13] all other studies were confined to the scope of a single country; therefore, conclusions were specific to certain demographics. This could have led to misrepresented results because the epidemiology of OGI tends to vary in different geographic regions. In future studies, data can be drawn from larger databases such as the International Globe and Adnexal Trauma Epidemiology Study (IGATES), which is a multinational collaborative data registry reaching 86 institutions worldwide.[32]
Lastly, the discrepancies in the cutoff criteria for prognostic factors could have led to inaccuracies in the conclusions drawn. For example, the differences in the cutoff criteria for wound size leading to poor prognosis in studies by Toh ZH et al. (2022)[11] and Han SB et al. (2010)[28] can hinder the prognostic value of wound size in predicting the outcome of OGI.
With regards to the study design, the exclusion of articles published before the year 2010 and non-English language literature may have limited the scope of the review.
Nonetheless, this review has managed to draw findings from articles written globally and synthesize the findings. The global nature of the review lends breadth and scope to the findings of this review, adding to its reliability.
Although there are largely unanimous findings on the prognostic factors of OGI, there is debate when it comes to the prognostic predictive value of the OTS. Given that the recognition of the prognostic factors of OGI can help in clinical management and counseling, it is imperative to conduct a study on the prognostic factors of OGI based on a larger international database and to make use of the findings to derive an improved OTS scoring system. The larger international database can offer a larger sample size, varied demographics, and prospective data, which will add to the objectivity of the study.
Conclusion
Initial visual acuity and zone of injury are the most significant prognostic factors of OGI, among others, which include retinal detachment/involvement, RAPD, vitreous hemorrhage, vitreous prolapse, type of injury, hyphema, lens involvement, and duration from incidence of OGI to vitrectomy.
Although there is consensus on the prognostic predictive value of the OTS in general, there is variation on the prognostic predictive value of specific OTS categories. To improve the understanding of the prognostic factors of OGI and the predictive value of the OTS, further research is necessary. The limitations of current studies should be recognized to improve the outcomes of future research. By conducting additional studies, clinicians can gain a better understanding of the predictive value of the OTS and other prognostic factors, leading to more accurate predictions and improved patient outcomes.
Financial support and sponsorship:
Nil.
Conflicts of interest:
There are no conflicts of interest.
References
- 1.Aghadoost D. Ocular trauma: An overview. Arch Trauma Res. 2014;3:e21639. doi: 10.5812/atr.21639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thylefors B. Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol. 1992;20:95–8. doi: 10.1111/j.1442-9071.1992.tb00718.x. [DOI] [PubMed] [Google Scholar]
- 3.Pizzarello LD. Ocular trauma: Time for action. Ophthalmic Epidemiol. 1998;5:115–6. doi: 10.1076/opep.5.3.115.8366. [DOI] [PubMed] [Google Scholar]
- 4.Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Graefes Arch Clin Exp Ophthalmol. 1996;234:399–403. doi: 10.1007/BF00190717. [DOI] [PubMed] [Google Scholar]
- 5.Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5:143–69. doi: 10.1076/opep.5.3.143.8364. [DOI] [PubMed] [Google Scholar]
- 6.Fujikawa A, Mohamed YH, Kinoshita H, Matsumoto M, Uematsu M, Tsuiki E, et al. Visual outcomes and prognostic factors in open-globe injuries. BMC Ophthalmol. 2018;18:138. doi: 10.1186/s12886-018-0804-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuhn F, Maisiak R, Mann L. OTS: Prognosticating the final vision of the seriously injured eye. Ocular Trauma: Principles and Practice. 2002:9–13. [Google Scholar]
- 8.Scott R. The ocular trauma score. Community Eye Health. 2015;28:44–5. [PMC free article] [PubMed] [Google Scholar]
- 9.Lima-Gómez V, Razo Blanco Hernández D, Rojas-Dosal J. Ocular trauma score at the initial evaluation of ocular trauma. Cir Cir. 2010;78:209–13. [PubMed] [Google Scholar]
- 10.He Y, Zhang L, Wang F, Zhu M, Wang Y, Liu Y. Timing influence on outcomes of vitrectomy for open-globe injury: A prospective randomized comparative study. Retina. 2020;40:725–34. doi: 10.1097/IAE.0000000000002447. [DOI] [PubMed] [Google Scholar]
- 11.Toh ZH, Shah SM, Chua CH, Hoskin AK, Agrawal R, Shah M. International Globe and Adnexal Trauma Epidemiology Study (IGATES): Visual outcomes in open globe injuries in rural West India. Eye. 2023;37:88–96. doi: 10.1038/s41433-021-01895-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bruce CN, Beal CJ, Zou B. Visual outcomes and prognostic factors for pediatric open globe injuries. Pediatr Emerg Care. 2022;38:e439–42. doi: 10.1097/PEC.0000000000002624. [DOI] [PubMed] [Google Scholar]
- 13.Hoskin AK, Low R, Sen P, Mishra C, Kamalden TA, Woreta F, et al. Epidemiology and outcomes of open globe injuries: The international globe and adnexal trauma epidemiology study (IGATES) Graefes Arch Clin Exp Ophthalmol. 2021;259:3485–99. doi: 10.1007/s00417-021-05266-1. [DOI] [PubMed] [Google Scholar]
- 14.Shir Yen W, Siu Wan F, Che Hamzah J, Khoo Kah Luen K. Epidemiology and visual outcome of open globe injury cases in hospital Pulau Pinang. Cureus. 2021;13:e19648. doi: 10.7759/cureus.19648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mayer CS, Reznicek L, Baur ID, Khoramnia R. Open globe injuries: Classifications and prognostic factors for functional outcome. Diagnostics (Basel) 2021;11:1851. doi: 10.3390/diagnostics11101851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Puodžiuvienė E, Valeišaitė G, Žemaitienė R. Clinical characteristics, visual outcomes, and prognostic factors of open globe injuries. Medicina (Kaunas) 2021;57:1198. doi: 10.3390/medicina57111198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ng HR, Chee SF, Chai KS, Chong MF, Mustapha M. The Epidemiological profile of open globe injuries and prognostic factors in a tertiary care centre. Cureus. 2021;13:e15846. doi: 10.7759/cureus.15846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Demir M, Akpolat Ç, Akar S, Muftuoglu G, Ozkan S. Prognostic factors affecting functional and anatomical outcome in globe injuries. Med Sci. 2021;10:804–11. [Google Scholar]
- 19.Toh ZH, Agrawal S, Raje D, Hoskin A, Agrawal R, Khandelwal R. International globe and adnexal trauma epidemiology study (IGATES): A report from Central India on visual outcome in open globe injuries and correlation with ocular trauma score. Int Ophthalmol. 2020;40:2797–806. doi: 10.1007/s10792-020-01429-x. [DOI] [PubMed] [Google Scholar]
- 20.Guzmán-Almagro E, Fernandez-Sanz G, Herrero-Escudero D, Contreras I, González Martín-Moro J. Open-globe-injury: A single center Spanish retrospective 5-year cohort study. Eur J Ophthalmol. 2021;31:2710–6. doi: 10.1177/1120672120962039. [DOI] [PubMed] [Google Scholar]
- 21.Guven S, Durukan AH, Erdurman C, Kucukevcilioglu M. Prognostic factors for open-globe injuries: Variables for poor visual outcome. Eye (Lond) 2019;33:392–7. doi: 10.1038/s41433-018-0218-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Okamoto Y, Morikawa S, Okamoto F, Inomoto N, Ishikawa H, Ueda T, et al. Clinical characteristics and outcomes of open globe injuries in Japan. Jpn J Ophthalmol. 2019;63:109–18. doi: 10.1007/s10384-018-0638-x. [DOI] [PubMed] [Google Scholar]
- 23.Page RD, Gupta SK, Jenkins TL, Karcioglu ZA. Risk factors for poor outcomes in patients with open-globe injuries. Clin Ophthalmol. 2016;10:1461–6. doi: 10.2147/OPTH.S108901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meng Y, Yan H. Prognostic factors for open globe injuries and correlation of ocular trauma score in Tianjin, China. J Ophthalmol. 2015;2015:345764. doi: 10.1155/2015/345764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu X, Liu Z, Liu Y, Zhao L, Xu S, Su G, et al. Determination of visual prognosis in children with open globe injuries. Eye (Lond) 2014;28:852–6. doi: 10.1038/eye.2014.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agrawal R, Wei HS, Teoh S. Prognostic factors for open globe injuries and correlation of ocular trauma score at a tertiary referral eye care centre in Singapore. Indian J Ophthalmol. 2013;61:502–6. doi: 10.4103/0301-4738.119436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bauza AM, Emami P, Soni N, Holland BK, Langer P, Zarbin M, et al. A 10-year review of assault-related open-globe injuries at an urban hospital. Graefes Arch Clin Exp Ophthalmol. 2013;251:653–9. doi: 10.1007/s00417-012-2136-z. [DOI] [PubMed] [Google Scholar]
- 28.Han SB, Yu HG. Visual outcome after open globe injury and its predictive factors in Korea. J Trauma. 2010;69:E66–72. doi: 10.1097/TA.0b013e3181cc8461. [DOI] [PubMed] [Google Scholar]
- 29.Nagurney JT, Brown DFM, Sane S, Weiner JB, Wang AC, Chang Y. The accuracy and completeness of data collected by prospective and retrospective methods. Acad Emerg Med. 2005;12:884–95. doi: 10.1197/j.aem.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 30.Schrader WF. [Epidemiology of open globe eye injuries: Analysis of 1026 cases in 18 years] Klin Monbl Augenheilkd. 2004;221:629–35. doi: 10.1055/s-2004-813254. [DOI] [PubMed] [Google Scholar]
- 31.Framme C, Roider J. [Epidemiology of open globe injuries] Klin Monbl Augenheilkd. 1999;215:287–93. doi: 10.1055/s-2008-1034716. [DOI] [PubMed] [Google Scholar]
- 32.Ng SMS, Low R, Hoskin AK, Rousselot A, Gunasekeran DV, Natarajan S, et al. The application of clinical registries in ophthalmic trauma-the International Globe and Adnexal Trauma Epidemiology Study (IGATES) Graefes Arch Clin Exp Ophthalmol. 2022;260:1055–67. doi: 10.1007/s00417-021-05493-6. [DOI] [PubMed] [Google Scholar]
- 33.Yalcin Tök O, Tok L, Eraslan E, Ozkaya D, Ornek F, Bardak Y. Prognostic factors influencing final visual acuity in open globe injuries. J Trauma. 2011;71:1794–800. doi: 10.1097/TA.0b013e31822b46af. [DOI] [PubMed] [Google Scholar]


