Abstract
Hemangiomas, benign vascular masses, occasionally occur in the kidneys, presenting as rare, small, unilateral, and solitary growths. Venous hemangiomas, a renal subtype, are atypical. While clinically nonspecific, they are typically asymptomatic and may be incidentally discovered during unrelated clinical workups. Diagnosing renal hemangioma preoperatively is challenging due to rarity, lacking standard radiographic criteria, and poor differentiation from aggressive renal neoplasms on contrast-enhanced imaging. These tumors commonly follow a benign course, with no documented recurrence. This video article showcases the robot-assisted excision of a renal vein hemangioma, addressing the expertise needed in managing this uncommon condition robotically.
Keywords: Robotic, Hemangioma, Renal neoplasm, Nephron-sparing
1. Introduction
Hemangiomas are vascular benign masses that develop in various body parts, including the kidneys, where they are rare, solitary, small, and usually unilateral. Venous hemangiomas are an unusual subtype of the renal ones.1 The clinical presentation is non-specific. Hematuria can be the presenting symptom, although venous hemangiomas are typically asymptomatic.2
Usually, hemangiomas are discovered as incidental findings during the workup for other clinical conditions (as observed in the herein reported patient).
Due to the rarity of the condition, the preoperative diagnosis of renal hemangiomas represents a challenge for the clinician. Indeed, there are no standard radiographic criteria. Moreover, contrast-enhanced computed tomography scans cannot reliably differentiate benign hemangiomas of the renal vein from other aggressive renal neoplasms such as renal cell carcinoma with tumor thrombi.3
Notwithstanding the challenges in the diagnosis, such tumors run a benign course without evidence of recurrences or metastatic potential reported in the literature.
The aim of the present video article was to report on the surgical treatment of a suspect neoplasm of the renal vein, which was found to be a benign hemangioma of the renal vein at final pathology.
2. Case presentation
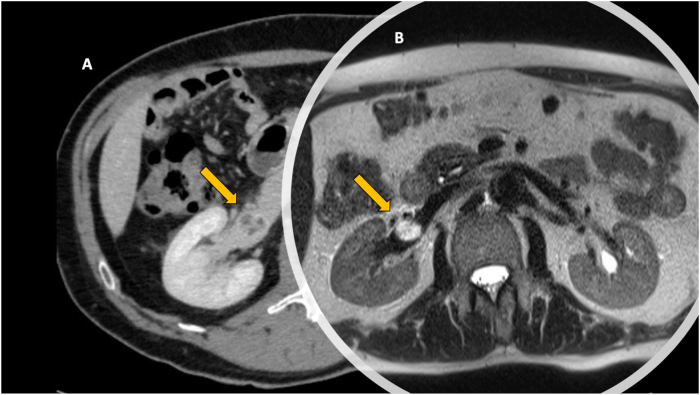
We describe the case of a 62-year-old Caucasian man with a long story of lower urinary tract symptoms and recurrent renal colic who underwent abdominal computed tomography with urography which incidentally found a 2 cm hypodense filling defect in the lumen of the right renal vein. The finding was compatible with venous thrombosis (Fig. 1A).
Fig. 1.
Contrast-enhanced computed tomography scan A) and Magnetic Resonance Imaging B) showing the hypodense filling defect in the lumen of the right renal vein and the solid, round shaped mass, in the lumen of the right renal vein, hyperintense on T2-weighted images, respectively.
The patient's medical history was negative for gross hematuria and significant weight loss. Physical examination was negative for any palpable mass or skin lesions.
Abdominal magnetic resonance imaging confirmed the presence of a 3.3 cm solid mass, round shaped, in the lumen of the right renal vein, hyperintense on T2-weighted images (Fig. 1B). The morphology addressed towards the suspect of a papillary renal cell carcinoma.
Staging was completed with chest computed tomography and was negative for either lymph-nodal localizations or other metastases.
Moreover, the patient did not show any alteration of the coagulative profile. The renal function was normal with estimated glomerular filtration rate (eGFR) of 98 ml/min/1.73 m2.
Considering the radiological findings, the differential diagnosis included conditions such as primitive neoplasm of the renal vein versus a “pedunculated” renal cell carcinoma.
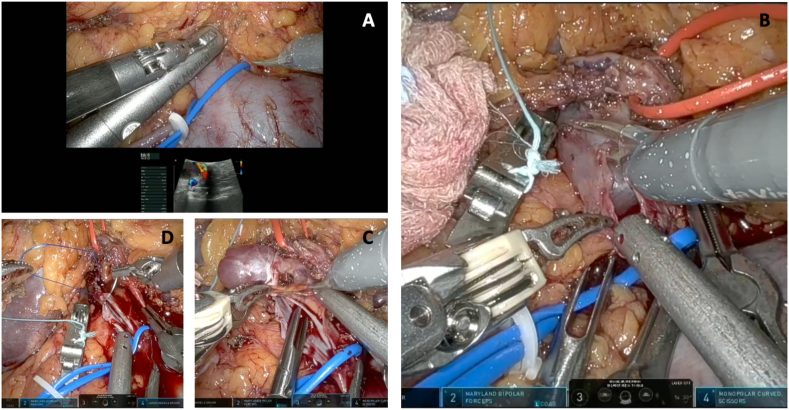
We performed a robotic transperitoneal excision of the mass, detailed in the accompanying Video 1. Briefly, after isolation of the right kidney, attention was moved towards the renal hilum. All the vascular structures were dissected free. Intraoperative ultrasound was performed to identify the limits of the known mass inside the lumen of the renal vein (Fig. 2A). The renal vein, the renal artery, and its upper branches were clamped, and then the indocyanine green (ICG) was injected to evaluate the kidney perfusion. A radial venotomy was performed to expose the mass removed en-bloc (Fig. 2B and C). A dedicated suture of the renal vein defect was performed with 4-0 Prolene (Fig. 2D). After removing the robotic bulldogs, no blood spillage was noticed, and the restored kidney perfusion was confirmed by ICG fluorescence. Warm ischemia time was just below 15 minutes. Blood losses were negligible. Console time was 90 minutes. The surgery was uneventful. Length of stay was 4 days. The patient had a regular postoperative course. He has been followed-up for three months. He no longer complained of flank pain. His renal function remained unchanged.
Fig. 2.
After the vascular structures were dissected free, A) intraoperative ultrasound was performed to identify the limits of the known mass inside the lumen of the renal vein; B) radial venotomy was performed to expose the mass, C) which was removed en-bloc. D) A dedicated suture of the renal vein defect was performed with 4-0 Prolene.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.eucr.2024.102651
The following is the supplementary data related to this article.
Video summarizing the case report and the surgical intervention.1
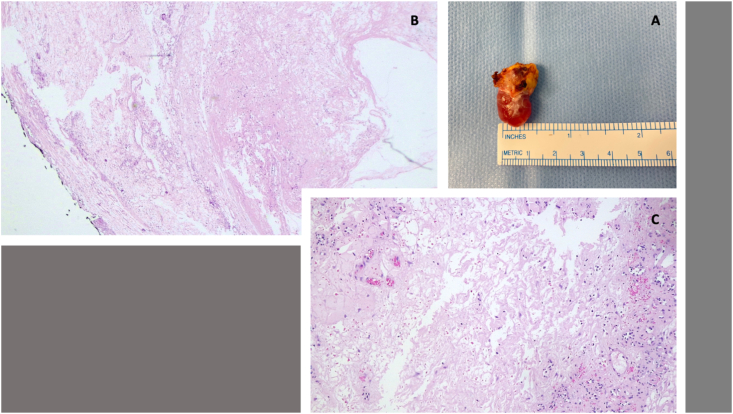
The final pathology reported a hemangioma of the renal vein, 3.3 × 2 cm in maximum sizes. Immunohistochemistry showed positivity for CD34 and ML-actin (Fig. 3).
Fig. 3.
Final pathology specimen: A) Macroscopic specimen: hemangioma of the renal vein, 3.3 × 2 cm in maximum sizes; B, C) Microscopic slices with immunohistochemistry showing the positivity for CD34 and ML-actin.
3. Discussion
Our case report underlines how primary vascular tumors of the kidney may pose diagnostic difficulties because of their rarity and their clinical and morphological presentation similar to tumor thrombosis.4
Due to the lack of specific clinical and radiologic manifestations, such diseases can be easily misdiagnosed preoperatively. Anecdotal reports are available in the literature. Previous experiences had the final benign pathology in common, but many authors approached the suspect tumor with radical nephrectomy.5,6
We believe that the present experience will help raise awareness of such rare diseases. Definitely, the preoperative workout can be improved. On the other hand, the expertise in minimally-invasive robotic kidney surgery matured at our institution was paramount in achieving a successful nephron sparing intent. This was particularly satisfactory once the final pathology resulted to be benign.
Finally, the reader should remember that such lesions are generally seen as isolated but may be part of a congenital disorder. We further investigated the patient once we got the final diagnosis, but we discovered that the patient's family history was negative for any hemangioma-related genetic disorders such as Klippel-Trenaunay-Weber syndrome or Sturge-Weber syndrome.7
4. Conclusion
The preoperative diagnosis of hemangioma of the renal vein is challenging because there are neither radiographic nor clinical criteria to reference. The most effective management of this condition has not yet been standardized. The optimal treatment should be tailored case-by-case, considering location, size, growth over time, and symptoms. In our experience, robotics was a safe and effective approach, particularly at a referral institution with consolidated expertise in minimally-invasive nephron-sparing surgery.
Fundings
None.
CRediT authorship contribution statement
Francesca Montanaro: Writing – original draft, Validation, Data curation. Riccardo Bertolo: Writing – review & editing, Validation, Supervision, Software, Project administration, Methodology, Conceptualization. Sonia Costantino: Validation, Software, Resources, Data curation. Nicola De Maria: Validation, Resources, Data curation. Alessandro Veccia: Validation, Resources, Methodology, Investigation. Filippo Migliorini: Visualization, Validation, Resources, Data curation. Anna Caliò: Validation, Resources, Formal analysis. Matteo Brunelli: Validation, Resources, Formal analysis. Stefania Montemezzi: Visualization, Validation, Software, Resources. Maria Angela Cerruto: Validation, Supervision, Resources. Alessandro Antonelli: Writing – review & editing, Validation, Supervision, Resources, Project administration, Conceptualization.
Declaration of competing interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
References
- 1.Elek A., Kwon J.W., Ertugrul S., et al. Radiologic and pathologic correlation of a renal venous hemangioma. Int Canc Conf J. 2023;12:227–232. doi: 10.1007/s13691-023-00626-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao X., Zhang J., Zhong Z., Koh C.J., Xie H.W., Hardy B.E. Large renal cavernous hemangioma with renal vein thrombosis: case report and review of literature. Urology. 2009 Feb;73(2):443.e1–443.e3. doi: 10.1016/j.urology.2008.02.049. Epub 2008 Apr 14. PMID: 18407336. [DOI] [PubMed] [Google Scholar]
- 3.Hull G.W., 3rd, Genega E.M., Sogani P.C. Intravascular capillary hemangioma presenting as a solid renal mass. J Urol. 1999 Sep;162(3 Pt 1):784–785. doi: 10.1097/00005392-199909010-00045. [DOI] [PubMed] [Google Scholar]
- 4.Omiyale A.O. Primary vascular tumours of the kidney. World J Clin Oncol. 2021 Dec 24;12(12):1157–1168. doi: 10.5306/wjco.v12.i12.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zheng L.P., Shen W.A., Wang C.H., et al. Anastomosing hemangioma arising from the left renal vein: a case report. World J Clin Cases. 2020 Oct 26;8(20):4986–4992. doi: 10.12998/wjcc.v8.i20.4986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Omiyale A.O., Golash A., Mann A., Kyriakidis D., Kalyanasundaram K. Anastomosing haemangioma of the kidney involving a segmental branch of the renal vein. Case Rep Surg. 2015;2015 doi: 10.1155/2015/927286. Epub 2015 Sep. 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prasad S.R., Surabhi V.R., Menias C.O., Raut A.A., Chintapalli K.N. Benign renal neoplasms in adults: cross-sectional imaging findings. AJR Am J Roentgenol. 2008 Jan;190(1):158–164. doi: 10.2214/AJR.07.2724. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video summarizing the case report and the surgical intervention.1