Abstract
PURPOSE:
This article provides an update to the 2018 Spina Bifida Association’s Transition to Adult Care Guidelines.
METHODS:
A workgroup of topic experts was convened including authors from the initial guideline workgroup. The workgroup reviewed and updated the primary, secondary, and tertiary outcome goals, clinical questions, and guideline recommendations based on a literature review.
RESULTS:
Twenty-two additional articles were identified from the literature search. Updated references included observational studies describing transition to adult care outcomes, transition care model initiatives, and a validated self-management assessment tool.
CONCLUSION:
Structured transition initiatives increase the likelihood of establishing with adult care, decrease acute care use for young adults with spina bifida, and have the potential to improve quality of life and optimize chronic condition management. However, there is still a need to implement structure transition practices more broadly for this population using these recommended guidelines.
Keywords: Spina bifida, myelomeningocele, transition to adult care, adolescent care, care guidelines
1. Introduction
The primary goal of health care transition (henceforth referred to as transition) is to maximize lifelong functioning through the provision of high quality, developmentally appropriate health care that continues uninterrupted as the individual moves from adolescence to adulthood [1]. Collaboration and coordination between the individual, family, pediatric and adult health care providers, allied health services, and school systems are essential to navigate the complexities of transition to adult care and life [2–4]. Fostering the gradual, developmentally appropriate acquisition of independent skills through goal setting and coaching enables adolescents and young adults with spina bifida (SB) to optimize their independence and participation in adult roles and activities throughout transition [5–8].
While transition focuses on adolescent and young adult age groups, the trajectory to maximize adult function and independence is fostered throughout the lifespan by setting expectations early for adult independence and the eventual transition of care [3, 9]. Transition to adulthood and health care planning with the individual and their family is a lifelong process that begins at birth. However, the essential steps of the health care transition (i.e., preparation, hand-off, and completion) primarily take place in adolescent and young adult age groups. Transition preparation should begin between the ages of 12–14 [6, 10] and involves supporting the adolescent in the gradual, developmentally appropriate assumption of increased independence and responsibility for self-care and condition management through coaching in home, school, and clinic settings [5]. Transition hand-off involves transferring care plans and responsibilities from pediatric to adult providers as the individual establishes care in the adult setting. Secondary to the structure of contemporary health care systems, transfer usually occurs between the ages of 18–21, but timing can be variable based on care needs and health care settings [6, 7, 11]. Transition completion refers to the establishment of the individual in the adult healthcare setting, with adult care providers, and with needed community supports to optimize their adult life [10].
Survival to adulthood for individuals with SB now exceeds 85%, but the degree of adult independence in the population varies [12]. In general, individuals with higher lesions (i.e., above the L2 sensory level) and hydrocephalus are more dependent on others for bowel and bladder management, mobility, self-care, transfers, and activities of daily living [13, 14]. Additionally, adolescents with SB may experience a two- to five-year delay in developing autonomy skills compared with their typically-developing peers and may overestimate their abilities [15–17]. By age 30, approximately one-third of individuals with SB report independence, one-third need supervision and occasional help, and one-third routinely require assistance for daily care needs [18]. Also concerning, young adults with SB are less likely to achieve emerging adult milestones such as leaving home, attending college, finding employment, developing romantic relationships, and having multiple friendships compared to their peers without SB [19, 20]. Executive function, socioeconomic status, intrinsic motivation, parental fostering of independence, and bowel continence are significant predictors of successful transition to adult participation [20–22]. Young adults with SB also may experience increased health risks during transition. Many young adults with SB have increased hospitalizations for chronic condition exacerbations, such as urinary tract infections, shunt complications, and skin ulcers, and more difficulty accessing health care services than their age-matched peers [23, 24]. Thus, lifelong assessment and gradual, iterative interventions to maximize chronic condition management, family function, socialization, cognitive function and school performance, mental health, and self-management/self-care are foundational to their optimal participation, function, and quality of life in adulthood [3, 5, 6, 25–28].
2. Guideline goals and outcomes
2.1. Primary
– Maximize health and participation in emerging adult milestones throughout the transition process for individuals with SB.
2.2. Secondary
– Provide person-centered, comprehensive transition care that includes transition planning and care coordination beginning by age 14; self-management coaching; decision-making support; education and employment resources; and independent-living support.
2.3. Tertiary
– Promote access to uninterrupted, developmentally appropriate SB condition management and preventative care throughout transition – specifically, ages 14–21.
3. Methods
This manuscript provides an update to the 2018 Spina Bifida Health Care Transition Guidelines [29]. These updates include more recent publication references, assessment tools, and resources to inform spina bifida health care transition clinical practice. The scientific methodology for guideline development has been described by Dicianno et al [30]. To update the previous guidelines, a workgroup of topic experts was convened including authors from the initial workgroup. Table 1 includes the clinical question framing these guidelines.
Table 1.
Clinical questions that informed the transition to adult care guidelines
| Age group | Clinical questions |
| 0–12 years 11 months | 1. How can a child’s probable trajectory regarding future adult function and independence be identified? 2. What are barriers and facilitators to participating in emerging adult milestones for children with SB? 3. What are the essential transition planning elements to promote uninterrupted access to care once children with SB need adult care? |
| 13–17 years 11 months | 1. How can a child’s probable trajectory regarding future independence be identified? 2. What are barriers and facilitators to participating in emerging adult milestones for children with SB? 3. What are child-centered perceptions of a successful transition experience? 4. What are the systems level barriers to successful transition and strategies that have effectively mitigated them? 5. What are the key transition readiness parameters for patients with SB that can be measured over time? 6. What are the preventative and chronic condition management considerations in the transition age group, ages 14–21? 7. What are the essential transition planning elements to promote uninterrupted access to care once children with SB need adult care? |
| 18 + years | 1. What are barriers and facilitators to participating in emerging adult milestones for individuals with SB? 2. What are the preventative and chronic condition management considerations in the transition age group? 3. What are the essential transition planning elements to promote uninterrupted access to care once children with SB need adult care? 4. What are the best strategies to find and engage adult providers? |
The following updated key term list was developed by the authoring group: “myelomeningocele”, “lipomyelomeningocele”, “meningocele”, “neural tube defects”, “spinal dysraphism”, “spina bifida” AND “young adult”, “transition of care”, “functional independence”, “autonomy,” “adult healthcare”, “transition to adult care”, “adolescent”, and “self-care”. Medline, PubMed, Web of Science, Cochrane Library, PsycInfo and CINAHL databases were searched for peer-reviewed articles published between January 1, 2016, and November 1, 2020. Additional articles were identified by the authoring group. When applicable, the evidence from the literature search was used to develop these guidelines and, where it was limited, general health care transition guidelines were provided with additional expert clinical recommendations for SB. Each article was reviewed by at least two authors for applicability to the identified outcome goals and to determine needed updates to the recommendations and/or citations for each of the original aged-basedguidelines.
4. Results
Twenty-two additional articles were identified with the updated search. Of these, eight were cross-sectional studies [6, 31–37], one was a cohort study [38], one was an assessment tool validation study [39], three were qualitative [8, 17, 40], five were literature reviews [41–45], and four were descriptive articles summarizing SB transition clinic models [2, 3, 7, 46].
Of the cross-sectional studies, four were single center studies. Regarding transition preparation, Hopson et al. described common individualized transition plan goals amongst 32 adolescents with SB including completing career interest surveys or exploration opportunities, working on bowel continence, and documenting medical history [6]. Three single-center, cross-sectional studies evaluated transfer and integration to adult care. Shepard et al. found that children engaged in a multidisciplinary SB clinic had more outpatient clinic use than transitioned adults and that adults who did not successfully transition had more emergency care and inpatient utilization than those who did establish with an adult provider [31]. Hettel et al. found that provider preference and communication were the most cited barriers to establishing adult care amongst 27 surveyed adults with SB [34]. Finally, Aguilera et al. surveyed ten young adults with SB established with an adolescent and young adult transition clinic, finding that all had routine primary care follow up, only two had emergency care visits in the last year, and seven reported good to excellent quality of life [36].
The other four cross-sectional studies involved multiple SB clinics. One international study found that amongst young adults who had transitioned to adult care from Brazil, Germany, and the United States, 76.5% of those requiring bladder catheterization were independent in intermittent catheterization, and there was no difference in self-catheterization amongst the nationalities [32]. Three studies focused on transition preparation. Wood et al. tested the predictive validity of the Transition Readiness Assessment Questionnaire-SB (TRAQ-SB) in 90 youth with SB, determining that higher TRAQ-SB scores were associated with urinary continence but not bowel continence or skin breakdown [37]. Wajchendler et al. surveyed 28 Canadian pediatric urologists regarding their SB transition practices and found that 78% did not provide ongoing care after 18 years but only 14% assessed transition readiness [35]. Similarly, Kelly et al. surveyed 34 pediatric SB clinics finding that most discussed the concept of transition but did not routinely evaluate their transition process or discuss insurance changes, and only 30% communicated with adult providers [33].
The cohort study focused on transfer success, revealing only 40% of young adults successfully transferred from a pediatric multidisciplinary clinic to an adult urology clinic. There were no identified predictors of successful transfer, potentially due to low study size [38]. The validity study assessed the TRAQ-SB, finding good internal reliability and strong age correlation for scores [39].
Qualitative studies addressed transition preparation and support topics in single centers. Betz et al. explored understanding of Individualized Education Plans (IEPs) among youth with SB. They found several IEP knowledge gaps and that self-management skills were not included on IEPs [8]. Lindsay et al. interviewed clinicians and young adults with SB regarding the implementation of a single center transition program in Canada, finding that the program facilitated care coordination but accessibility to adult care services and difficulties with adult clinic communication remained barriers [40]. Finally, Stromfors et al. interviewed eight adolescents from Sweden, finding that adolescents overestimated their independence and needed support for independence development as well as social and emotional health [17].
Reviews summarized SB adult care needs as well as SB transition preparation needs. Mukherjee and Pasulka summarized the health and psychosocial needs of adults and the need for primary care access and routine follow-up, structured transition, and strategies to address potentially preventable complications that lead to hospitalization (e.g., sepsis, skin ulcers, infective arthritis, and urinary tract infections) [41]. Similarly, Patel et al. summarized the lifelong multi-organ system SB-related conditions affecting adolescents and adults with SB that need to be addressed during transition [45]. De Kort summarized the literature addressing urological SB transition and recognized the need for dedicated transition staff, addressing readiness, and discussing sexuality and relationship health [44]. A Cochrane Review by Campbell et al. evaluating the effectiveness of transition interventions for youth with chronic conditions found only four randomized controlled trials, including one study that compared adolescents with SB who did and did not attend a two-day transition workshop [42]. The three non-SB studies showed improved patient knowledge and self-efficacy, but the SB-specific study did not find significant results. Finally in a mixed-methods review, Choi et al. cited eight studies addressing SB transition programs and found that quantitative studies reported positive outcomes regarding independence and satisfaction whereas qualitative studies reported negative experiences such as barriers to communication with providers [43].
Descriptive articles summarized various strategies to address structured transition for SB. Betz described perspectives on fostering comprehensive self-management competencies as part of transition, particularly regarding navigating relationships, the community, and adult health care [46]. Seeley and Lindeke described a quality improvement pediatric nurse care coordination intervention that improved TRAQ scores [2]. Fremion et al. described a comprehensive SB transition preparation clinic model that partners with a pediatric multidisciplinary SB clinic and an adult medical home clinic to address transition planning and chronic condition management [7]. Finally, Hopson et al. described the implementation of a lifetime model to provide comprehensive care to individuals with SB using a pediatric and adult hospital system partnership [3].
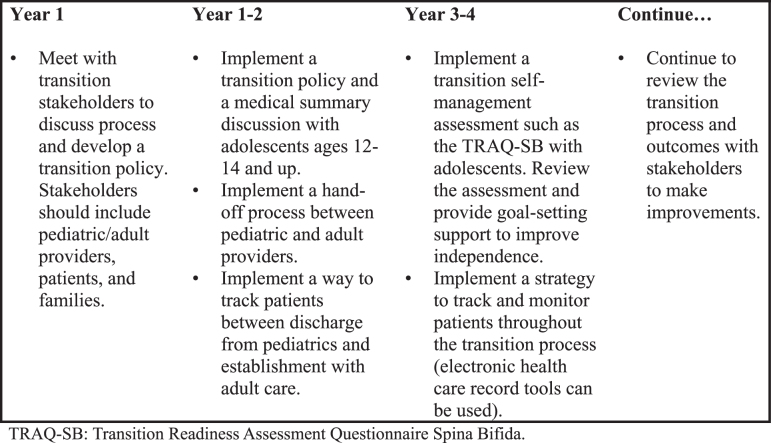
Using these articles, the authors updated the SB Transition Guidelines as listed in Table 2 with previous references from the 2018 guidelines also included [47–84]. Recognizing the challenge of initiating a comprehensive health care transition process, the workgroup also developed a stepwise strategy for implementing these guidelines into clinical practice based upon expert opinion (Fig. 1).
Table 2.
Summary of transition to adult care guidelines
| Age Group | Guidelines | Evidence |
| 0–5 years 11 months | 1. Provide families with a realistic, long-term orientation that includes a probable trajectory for adult function and expectations to promote life-long optimal independence according to the child’s abilities. | [3, 5, 12–15, 18, 31, 45, 48, 49, 62, 68–70] |
| 2. Provide information for families regarding long-term financial, insurance, and supportive living planning based on the child’s probable trajectory into adult function. | [54, 64, 68] | |
| 3. Consider regular evaluation of social determinants of health and immigration status (when applicable). Offer resources and navigation support if needs are identified as barriers can impact the individual’s long term functional trajectory and access to care. | [31, 50] | |
| 4. Discuss plans regarding where individuals with SB can access comprehensive care throughout the lifespan including the transition to adult care. | [3, 56, 63] | |
| 6 years–12 years 11 months | In addition to the above,1. Review the clinic’s transition policy with patients and families between ages 12–14. | [1, 10] |
| 13–17 years 11 months | 1. Consider having a designated transition clinic or care coordinator to support transition planning and coordination acknowledging that young adults may need ongoing support throughout hand-off and transfer to adult care. | [2–4, 6, 7, 26, 52, 71, 76, 78, 82, 84] |
| 2. Provide families with a realistic, long-term orientation that includes a probable trajectory for adult function and expectations to promote life-long optimal independence according to the child’s abilities. | [3, 12–18, 21, 45, 46, 49, 51, 55, 56, 68–70] | |
| 3. Promote participation in self-advocacy opportunities such as IEP meetings. Consider neurocognitive assessment to identify cognitive, adaptive, or learning support needs if knowledge or skill gaps are identified. | [8, 34, 48, 57, 65, 66] | |
| 4. Consider regular evaluation of social determinants of health and immigration status (when applicable). Offer resources and increased navigation support if needs are identified as barriers can impact the individual’s long term functional trajectory and access to care. | [14, 26, 43, 47, 51–56, 68] | |
| 5. Discuss transition planning with adolescent and family throughout adolescence ensuring that the adolescent’s and family’s views and preferences are considered in transition planning. Transition planning should include: | ||
| a. Expectations of when the transfer to adult care will occur based on the individual’s health condition, insurance/funding, cognitive development, and personal/family needs. | [1, 3, 7, 26, 34, 71] | |
| b. Expectations of who will provide care throughout the transition process. Often multidisciplinary clinics are not available for adults; thus, a primary care medical home or physiatrist practice may be best to provide comprehensive SB management for adults. Urologists often play an important role in facilitating transition to adult-centered care as well. | [3, 7, 33–41] | |
| c. Long-term financial, insurance, and supportive living (housing and transportation) plans, based on the individual’s current needs and probable trajectory of adult function. Information regarding the Social Security Administration’s Disability Determination Services before age 18, as applicable. | [14, 56] | |
| d. Information regarding the adolescent’s education and employment needs, such as vocational rehabilitation services, school transition planning as part of the IEP, and adaptive vocational needs. | [5–7, 20, 30, 50, 57–59] | |
| e. Preparation for decision-making supports and modalities that maximize the individual’s ability to participate in decisions for themselves once they are age 18, such as a medical power of attorney, supportive decision-making, or guardianship. Referral to medical legal partnerships may be needed. | [24, 34, 49, 58, 60] | |
| 6. Create medical summary including past medical and surgical history, current care plans, medications, allergies, vaccines, and current providers | [1, 10] | |
| 7. Regularly assess self-management independence throughout transition using a validated tool such as the TRAQ-SB. Discuss the results with the adolescent and family and set realistic goals to improve independence. Emphasize that self-management development is a gradual, iterative process. | [17, 26, 37, 42, 43, 46, 60, 66, 67] | |
| 8. Optimize bowel and bladder continence and independent management as continence is a major factor in promoting life-long social participation, quality of life, and education and employment opportunities. | [11, 31, 36, 42–45, 58, 59, 72] | |
| 9. Designate time alone with the adolescent for at least part of their visit, if developmentally appropriate. | [1, 10] | |
| 10. Ensure patient-centered and developmentally appropriate preventative and chronic condition management services are provided throughout transition. Topics to particularly address in this age group include bowel/bladder management, skin health, sexual health and function, mental health, healthy weight, and adaptive equipment/supplies to maximize independent function. | [10, 61, 73] | |
| 11. Patients and families should know the signs, symptoms, and action steps to manage these common SB-related complications: shunt malfunction, urinary tract infection, constipation, and skin ulcers. These management plans should be included along with a medical summary to hand-off to adult providers. | [24, 41, 61, 72] | |
| 12. Prepare a hand-off packet that includes the medical summary, action plans, supply/equipment, and other important care coordination information to handoff to adult providers. Adult providers should include a primary care physician, neurosurgeon (if shunt or other neurosurgery history), urology if neurogenic bladder, and physiatrist if ongoing mobility management needs. | [1, 10, 79, 80, 83] | |
| Ages 18+ | 1. Provide families with a realistic, long-term orientation that includes a probable trajectory for adult function and expectations to promote life-long optimal independence according to the individual’s abilities. | [3, 12–15, 18, 52, 53, 68–70] |
| 2. Consider regular evaluation of social determinants of health and immigration status (when applicable). Offer resources and increased navigation support if needs are identified as barriers can impact the individual’s long term functional trajectory and access to care. | [31, 55, 68] | |
| 3. Optimize bowel and bladder continence and independent management as continence is a major factor in promoting life-long social participation, quality of life, and education and employment opportunities. | [6, 27, 31, 32, 57–59, 72, 74] | |
| 4. Regularly assess self-management independence throughout transition using a validated tool such as the TRAQ-SB (validated up to age 25). Discuss the results with the adolescent and family and set realistic goals to improve independence. Emphasize that self-management development is a gradual, iterative process. | [17, 37, 42, 43, 46, 57, 60, 66, 67, 75] | |
| 5. Promote on-going collaboration between pediatric/adult care providers and patients/families to improve the transition process and promote best care practices. Often multidisciplinary clinics are not available for adults; thus, a primary care medical home or physiatrist practice may be best to provide comprehensive SB management for adults. Urologists often play an important role in facilitating transition to adult-centered care as well. Also important is identifying an adult neurosurgeon for ventricular shunt concerns. | [3, 7, 31, 34–36, 38, 44, 50, 61, 62, 79, 80] | |
| 6. Continue to assist with transition coordination as applicable including:a. Assistance in identifying adult providers who accept the patient’s insurance and can assume their care.b. Counselling regarding long-term financial, insurance, and supportive living plans (housing, transportation, etc.) based on the individual’s current needs and probable trajectory of adult function.c. Information for education/employment transition support as applicable to the individual’s need such as vocational rehabilitation services, school transition planning, as part of the IEP, and adaptive vocational needs.d. Decision-making supports and modalities that maximize the individual’s ability to participate in decisions for themselves, such as a medical power of attorney, supportive decision-making, or guardianship. Referral to medical legal partnerships may be needed.e. Adult disability determination information if applicable.f. Updating a medical summary including past medical and surgical history, current care plans, medications, allergies, vaccines, and current providers. | [2, 4, 11, 63–68, 77] | |
| 7. Ensure patient-centered and developmentally appropriate preventative and chronic condition management services are provided throughout transition. Topics to particularly address in this age group include bowel/bladder management, skin health, sexual health and function, mental health, healthy weight, and adaptive equipment/supplies to maximize independent function | [24, 50, 53, 58, 60, 61, 66, 69, 70] |
IEP: individualized education plan. SB: spina bifida. TRAQ-SB: Transition Readiness Assessment Questionnaire Spina Bifida.
Fig. 1.
Suggested timeline for implementing a structured transition to adult care clinical process.
5. Discussion
These updated guidelines provide additional references for the recommended SB Health Care Transition practices throughout the lifespan. Notably, they include a reference for the TRAQ-SB, a validated measure for transition readiness including specific questions regarding independence SB-care topics that can be used to direct self-management goal setting and measure intervention success during transition preparation [2, 37, 39].
The updated literature search found additional studies addressing the three topics of health care transition: transition preparation, transfer, and completion/integration into adult care for adolescents and young adults with SB. Most studies were single center and descriptive. Studies addressing transition preparation described the need to support self-management independence and adolescent health including mental health and reproductive health [8, 17, 43, 44, 46]. While several publications described single center, clinic-based transition initiatives to improve care coordination and transition readiness skills [2, 3, 6, 7, 40], there is still a need to implement structured transition practices more broadly in pediatric clinics in partnership with adult care clinics [35, 82]. Publications addressing transfer to adult care identified gaps in establishing adult care, particularly around communication with providers and the need to ensure care transfer as well as the benefits of assuring access to adult primary care including decreased acute care utilization [31, 33–36, 38, 40]. Lastly, publications regarding transition completion and integration into adult care consisted of one study evaluating adult catheterization independence and two literature reviews of adult care needs [9, 32, 45]. As evidence shows that time spent facilitating a successful transition can have significant health impact in the future, transition planning and care coordination are health care priorities for individuals with SB.
5.1. Limitations
Overall, there is limited literature evaluating outcomes of transition intervention at each stage: preparation, transfer, and completion. Most studies are single center with small sample sizes. These limitations highlight the need to further evaluate transition preparation and hand-off implementation strategies and patient outcomes as well as adult SB care models that support integration into the adult healthcare system and ongoing comprehensive care.
6. Conclusions
In summary, general transition to adult care guidelines as well as limited SB-specific studies support the recommendation that transition discussions should begin at birth. Early childhood transition planning should focus on developing long-term goals and expectations to promote optimal health and independence, lifelong care access, and financial planning. During the adolescent years, transition preparation should include developing a care plan (i.e., medical summary, financial plan, care team hand-off plan, decision-making supports, and care supports needed), supporting self-management development, addressing adolescent health topics, and care coordination. Transfer to adult care is an opportunity for proactive care coordination to ensure that individuals establish with adult providers and that adult providers receive a care summary. Finally, adults with SB establishing with adult health care need ongoing, comprehensive, coordinated care to address their SB-related conditions, mental health, general preventive care needs, and self-management supports needs. Further studies are needed to evaluate transition interventions to inform best practices and future guideline updates.
Acknowledgments
Timothy J. Brei, MD, Spina Bifida Association Medical Director; Developmental Pediatrician, Professor, Seattle Children’s Hospital.
Sara Struwe, MPA, Spina Bifida Association President & Chief Executive Officer.
Patricia Beierwaltes, DPN, CPNP, Guideline Steering Committee Co-Chair; Assistant Professor, Nursing, Minnesota State University, Mankato.
Brad E. Dicianno, MD, Guideline Steering Committee Co-Chair; Associate Medical Director and Chair of Spina Bifida Association’s Professional Advisory Council; Associate Professor, Department of Physical Medicine and Rehabilitation, University of Pittsburgh School of Medicine.
Nienke Dosa MD, MPH, Guideline Steering Committee Co-Chair; Upstate Foundation Professor of Child Health Policy; SUNY Upstate Medical University.
Lisa Raman, RN, MScANP, MEd, former Spina Bifida Association Director, Patient and Clinical Services.
Jerome B. Chelliah, MD, MPH, Johns Hopkins Bloomberg School of Public Health.
Julie Bolen, PhD, MPH, Lead Health Scientist, Rare Disorders Health Outcomes Team, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention.
Adrienne Herron, PhD Behavioral Scientist, Intervention Research Team, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention.
Judy Thibadeau, RN, MN, Spina Bifida Association Director, Research and Services; former Health Scientist, National Spina Bifida Program, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention.
Conflict of interest
Ellen Fremion and Kathrine Smith are unpaid board members and provider advisory committee members of the Spina Bifida Association.
Funding
The development of these Guidelines was supported in part by Cooperative Agreement UO1DD001077, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
References
- [1]. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110(Supplement 3):1304–6. doi: 10.1542/peds.110.S3.1304. [DOI] [PubMed] [Google Scholar]
- [2]. Seeley A, Lindeke L. Developing a Transition Care Coordination Program for Youth with Spina Bifida. J Pediatr Health Care. 2017;31(6):627–33. doi: 10.1016/j.pedhc.2017.04.015. [DOI] [PubMed] [Google Scholar]
- [3]. Hopson B, Rocque BG, Joseph DB, et al. The development of a lifetime care model in comprehensive spina bifida care. J Pediatr Rehabil Med. 2018;11(4):323–34. doi: 10.3233/PRM-180548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Lindsay S, Cruickshank H, Mcpherson AC, Maxwell J. Implementation of an inter-agency transition model for youth with spina bifida. Child Care Health Dev. 2016;42(2):203–12. doi: 10.1111/cch.12303. [DOI] [PubMed] [Google Scholar]
- [5]. Holmbeck GN, Kritikos TK, Stern A, Ridosh M, Friedman CV. The Transition to Adult Health Care in Youth with Spina Bifida: Theory, Measurement, and Interventions. J Nurs Scholarsh. 2021;53(2):198–207. doi: 10.1111/jnu.12626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Hopson B, Alford EN, Zimmerman K, et al. Development of an evidence-based individualized transition plan for spina bifida. Neurosurg Focus. 2019;47(4):7–12. doi: 10.3171/2019.7.FOCUS19425. [DOI] [PubMed] [Google Scholar]
- [7]. Fremion E, Morrison-Jacobus M, Castillo J, et al. A chronic care model for spina bifida transition. J Pediatr Rehabil Med. 2017;10(3-4):243–7. doi: 10.3233/PRM-170451. [DOI] [PubMed] [Google Scholar]
- [8]. Betz CL, Hudson SM, Lee JJ, et al. An exploratory study of adolescents and emerging adults with spina bifida knowledge of their individual education program: Implications for health care transition planning. J Pediatr Rehabil Med. 2019;12(4):393–403. doi: 10.3233/PRM-180578. [DOI] [PubMed] [Google Scholar]
- [9]. Mukherjee S, Pasulka J. Care for Adults with Spina Bifida: Current State and Future Directions. Top Spinal Cord Inj Rehabil. 2017;23(2):155–67. doi: 10.1310/sci2302-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Got Transition [homepage on the internet]. Washington, DC: The National Alliance to Advance Adolescent Health; 2014-2023 [cited 2023 October 1]. Available from: https://www.gottransition.org/
- [11]. Binks JA, Barden WS, Burke TA, Young NL. What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Arch Phys Med Rehabil. 2007;88(8):1064–73. doi: 10.1016/j.apmr.2007.04.018. [DOI] [PubMed] [Google Scholar]
- [12]. Dillon CM, Davis BE, Duguay S, Seidel KD, Shurtleff DB. Longevity of patients born with myelomeningocele. Eur J Pediatr Surg. 2000;10 Suppl:33-4. doi: 10.1055/s-2008-1072412. [DOI] [PubMed] [Google Scholar]
- [13]. Verhoef M, Barf HA, Post MWM, et al. Functional independence among young adults with spina bifida, in relation to hydrocephalus and level of lesion. Dev Med Child Neurol. 2006;48(2):114–9. doi: 10.1017/S0012162206000259. [DOI] [PubMed] [Google Scholar]
- [14]. Hetherington R, Dennis M, Barnes M, Drake J, Gentili F. Functional outcome in young adults with spina bifida and hydrocephalus. Childs Nerv Syst. 2006;22(2):117–24. doi: 10.1007/s00381-005-1231-4. [DOI] [PubMed] [Google Scholar]
- [15]. Davis BE, Shurtleff DB, Walker WO, et al. Acquisition of autonomy skills in adolescents with myelomeningocele. Dev Med Child Neurol. 2006;48(4):253–8. doi: 10.1017/S0012162206000569. [DOI] [PubMed] [Google Scholar]
- [16]. Psihogios AM, Holmbeck GN. Discrepancies in mother and child perceptions of spina bifida medical responsibilities during the transition to adolescence: Associations with family conflict and medical adherence. J Pediatr Psychol. 2013;38(8):859–70. doi: 10.1093/jpepsy/jst047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17]. Strömfors L, Wilhelmsson S, Falk L, Höst GE. Experiences among children and adolescents of living with spina bifida and their visions of the future. Disabil Rehabil. 2017;39(3):261–71. doi: 10.3109/09638288.2016.1146355. [DOI] [PubMed] [Google Scholar]
- [18]. Oakeshott P, Hunt GM. Long-term outcome in open spina bifida. Br J Gen Pract. 2003;53(493):632–6. [PMC free article] [PubMed] [Google Scholar]
- [19]. Liptak GS, Kennedy JA, Dosa NP. Youth with spina bifida and transitions: health and social participation in a nationally represented sample. J Pediatr. 2010;157(4):584–8, 588.e1. doi: 10.1016/j.jpeds.2010.04.004. [DOI] [PubMed] [Google Scholar]
- [20]. Liu T, Ouyang L, Walker WO, et al. Education and employment as young adults living with spina bifida transition to adulthood in the USA: A study of the National Spina Bifida Patient Registry. Dev Med Child Neurol. 2022;65(6):821–830. doi: 10.1111/dmcn.15456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21]. Liptak GS, Garver K, Dosa NP. Spina bifida grown up. J Dev Behav Pediatr. 2013;34(3):206–15. doi: 10.1097/DBP.0b013e31828c5f88. [DOI] [PubMed] [Google Scholar]
- [22]. Davis MC, Hopson BD, Blount J, et al. Predictors of permanent disability among adults with spinal dysraphism. J Neurosurg Spine. 2017;27(2):169–77. doi: 10.3171/2017.1.SPINE161044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23]. Wilson R, Lewis SA, Dicianno BE. Targeted preventive care may be needed for adults with congenital spine anomalies. PM&R. 2011;3(8):730–8. doi: 10.1016/j.pmrj.2011.05.021. [DOI] [PubMed] [Google Scholar]
- [24]. Young NL, Anselmo LA, Burke TA, et al. Youth and young adults with spina bifida: Their utilization of physician and hospital services. Arch Phys Med Rehabil. 2014;95(3):466–71. doi: 10.1016/j.apmr.2013.09.015. [DOI] [PubMed] [Google Scholar]
- [25]. Thibadeau JK, Alriksson-Schmidt AI, Zabel TA. The National Spina Bifida Program Transition Initiative: The People, the Plan, and the Process. Pediatr Clin North Am. 2010;57(4):903–10. doi: 10.1016/j.pcl.2010.07.010.26. [DOI] [PubMed] [Google Scholar]
- [26]. Sawin KJ, Buran CF, Brei TJ, Fastenau PS. Correlates of functional status, self-management, and developmental competence outcomes in adolescents with spina bifida. SCI Nurs. 2003;20(2):72–85. [PubMed] [Google Scholar]
- [27]. Rocque BG, Bishop ER, Scogin MA, et al. Assessing health-related quality of life in children with spina bifida. J Neurosurg Pediatr. 2015. Feb;15(2):144–9. doi: 10.3171/2014.10.PEDS1441. [DOI] [PubMed] [Google Scholar]
- [28]. Logan LR, Sawin KJ, Bellin MH, Brei T, Woodward J. Self-management and independence guidelines for the care of people with spina bifida. J Pediatr Rehabil Med. 2020;13(4):583–600. doi: 10.3233/PRM-200734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29]. Fremion EJ, Dosa NP. Spina bifida transition to adult healthcare guidelines. J Pediatr Rehabil Med. 2019;12(4):423–9. doi: 10.3233/PRM-190633. [DOI] [PubMed] [Google Scholar]
- [30]. Dicianno BE, Beierwaltes P, Dosa N, et al. Scientific methodology of the development of the Guidelines for the Care of People with Spina Bifida: An initiative of the Spina Bifida Association. Disabil Health J. 2020;13(2):100816. doi: 10.1016/j.dhjo.2019.06.005. [DOI] [PubMed] [Google Scholar]
- [31]. Shepard C, Doerge E, Eickmeyer A, et al. Ambulatory Care Utilization Among Patients with Spina Bifida: Change in Care from Childhood to Adulthood. J Urol. 2018;199(4):1050–1055. doi: 10.1016/j.juro.2017.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32]. Faleiros F, Warschausky S, Käppler C, et al. Bladder Self-management in the Transition to Adulthood With Spina Bifida in 3 Countries: A Comparative Study. Journal of Wound, Ostomy and Continence Nursing. 2019;46(4):321–326. doi: 10.1097/WON.0000000000000545. [DOI] [PubMed] [Google Scholar]
- [33]. Kelly MS, Thibadeau J, Struwe S, et al. Evaluation of spina bifida transitional care practices in the United States. J Pediatr Rehabil Med. 2017;10(3-4):275–81. doi: 10.3233/PRM-170455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34]. Hettel D, Tran C, Szymanski K, et al. Lost in transition: Patient-identified barriers to adult urological spina bifida care. J Pediatr Urol. 2018;14(6):535.e1–535.e4. doi: 10.1016/j.jpurol.2018.06.009. [DOI] [PubMed] [Google Scholar]
- [35]. Wajchendler A, Anderson P, Koyle MA. The transition process of spina bifida patients to adult-centred care: An assessment of the Canadian urology landscape. Can Urol Assoc J. 2017;11(1-2Suppl1):S88–S91. doi: 10.5489/cuaj.4338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36]. Aguilera AM, Wood DL, Keeley C, et al. Young adults with spina bifida transitioned to a medical home: A survey of medical care in Jacksonville, Florida. J Neurosurg Pediatr. 2016;17(2):203–207. doi: 10.3171/2015.7.PEDS14694. [DOI] [PubMed] [Google Scholar]
- [37]. Wood D, Rocque B, Hopson B, et al. Transition Readiness Assessment Questionnaire Spina Bifida (TRAQ-SB) specific module and its association with clinical outcomes among youth and young adults with spina bifida. J Pediatr Rehabil Med. 2019;12(4):405–13. doi: 10.3233/PRM-180595. [DOI] [PubMed] [Google Scholar]
- [38]. Szymanski KM, Cain MP, Hardacker TJ, Misseri R. How successful is the transition to adult urology care in spina bifida? A single center 7-year experience. J Pediatr Urol. 2017;13(1):40.e1–40.e6. doi: 10.1016/j.jpurol.2016.09.020. [DOI] [PubMed] [Google Scholar]
- [39]. Johnson K, Rocque B, Hopson B, Barnes K, Omoike OE, Wood D. The reliability and validity of a newly developed spina bifida-specific Transition Readiness Assessment Questionnaire: Transition Readiness Assessment Questionnaire-supplement (TRAQ-SB). J Pediatr Rehabil Med. 2019;12(4):415–22. doi: 10.3233/PRM-180599. [DOI] [PubMed] [Google Scholar]
- [40]. Lindsay S, Cruickshank H, McPherson AC, Maxwell J. Implementation of an inter-agency transition model for youth with spina bifida. Child Care Health Dev. 2016;42(2):203–12. doi: 10.1111/cch.12303. [DOI] [PubMed] [Google Scholar]
- [41]. Mukherjee S, Pasulka J. Care for adults with spina bifida: Current state and future directions. Top Spinal Cord Inj Rehabil. 2017;23(2):155–167. doi: 10.1310/sci2302-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42]. Campbell F, Biggs K, Aldiss SK, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev. 2016;4(4):CD009794. doi: 10.1002/14651858.CD009794.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43]. Choi EK, Bae E, Jang M. Transition programs for adolescents and young adults with spina bifida: A mixed-methods systematic review. J Adv Nurs. 2021;77(2):608–21. doi: 10.1111/jan.14651. [DOI] [PubMed] [Google Scholar]
- [44]. De Kort LMO. Transition from childhood to adolescence: Steps to be taken. Curr Opin Urol. 2020;30(4):491–5. doi: 10.1097/MOU.0000000000000771. [DOI] [PubMed] [Google Scholar]
- [45]. Patel SK, Staarmann B, Heilman A, et al. Growing up with spina bifida: Bridging the gaps in the transition of care from childhood to adulthood. Neurosurg Focus. 2019;47(4):E16. doi: 10.3171/2019.7.FOCUS19441. [DOI] [PubMed] [Google Scholar]
- [46]. Betz CL. Self-management and health care transition: Trials, tribulations and triumphs. J Pediatr Rehabil Med. 2017;10(3-4):177–83. doi: 10.3233/PRM-170446. [DOI] [PubMed] [Google Scholar]
- [47]. Fremion EJ, Dosa NP. Spina bifida transition to adult healthcare guidelines. J Pediatr Rehabil Med. 2019;12(4):423–9. doi: 10.3233/PRM-190633. [DOI] [PubMed] [Google Scholar]
- [48]. Castillo J, Ostermaier KK, Fremion E, et al. Urologic self-management through intermittent self-catheterization among individuals with spina bifida: A journey to self-efficacy and autonomy. J Pediatr Rehabil Med. 2017;10(3-4):219–26. doi: 10.3233/PRM-170447. [DOI] [PubMed] [Google Scholar]
- [49]. Yun HJ, Kim HS. Self-Management Behaviors of Children With Spina Bifida. J Neurosci Nurs. 2017;49(1):15–21. doi: 10.1097/JNN.0000000000000223. [DOI] [PubMed] [Google Scholar]
- [50]. Cooper J, Chisolm D, McLeod DJ. Sociodemographic Characteristics, Health Literacy, and Care Compliance in Families With Spina Bifida. Glob Pediatr Health. 2017 Dec 6:4:2333794X17745765. doi: 10.1177/2333794X17745765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51]. Brewer K, Pollock N, Wright FV. Addressing the challenges of collaborative goal setting with children and their families. Phys Occup Ther Pediatr. 2014;34(2):138–52. doi: 10.3109/01942638.2013.794187. [DOI] [PubMed] [Google Scholar]
- [52]. Stubberud J, Langenbahn D, Levine B, Stanghelle J, Schanke A-K. Goal Management Training of Executive Functions in Patients with Spina Bifida: A Randomized Controlled Trial. J Int Neuropsychol Soc. 2013;19(6):672–85. doi: 10.1017/S1355617713000209. [DOI] [PubMed] [Google Scholar]
- [53]. Kulesz PA, Treble-Barna A, Williams VJ, et al. Attention in spina bifida myelomeningocele: Relations with brain volume and integrity. Neuroimage Clin. 2015;8:72–8. doi: 10.1016/j.nicl.2015.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54]. Zabel TA, Jacobson LA, Zachik C, et al. Parent- and self-ratings of executive functions in adolescents and young adults with spina bifida. Clin Neuropsychol. 2011;25(6):926–41. doi: 10.1080/13854046.2011.586002. [DOI] [PubMed] [Google Scholar]
- [55]. Ryan P, Sawin KJ. The Individual and Family Self-Management Theory: Background and perspectives on context, process, and outcomes. Nurs Outlook. 2009;57(4):217–225.e6. doi: 10.1016/j.outlook.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56]. Zukerman JM, Devine KA, Holmbeck GN. Adolescent predictors of emerging adulthood milestones in youth with spina bifida. J Pediatr Psychol. 2011;36(3):265–76. doi: 10.1093/jpepsy/jsq075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57]. Holbein CE, Lennon JM, Kolbuck VD, Zebracki K, Roache CR, Holmbeck GN. Observed differences in social behaviors exhibited in peer interactions between youth with spina bifida and their peers: Neuropsychological correlates. J Pediatr Psychol. 2015;40(3):320–35. doi: 10.1093/jpepsy/jsu101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58]. Tapia CI, Khalaf K, Berenson K, Globe D, Chancellor M, Carr LK. Health-related quality of life and economic impact of urinary incontinence due to detrusor overactivity associated with a neurologic condition: a systematic review. Health Qual Life Outcomes. 2013;11(1):13. doi: 10.1186/1477-7525-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59]. Schechter MS, Liu T, Soe M, Swanson M, Ward E, Thibadeau J. Sociodemographic Attributes and Spina Bifida Outcomes. Pediatrics. 2015;135(4):e957–64. doi: 10.1542/peds.2014-2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60]. Mahmood D, Dicianno B, Bellin M. Self-management, preventable conditions and assessment of care among young adults with myelomeningocele. Child Care Health Dev. 2011;37(6):861–5. doi: 10.1111/j.1365-2214.2011.01299.x. [DOI] [PubMed] [Google Scholar]
- [61]. Dicianno BE, Gaines A, Collins DM, Lee S. Mobility, assistive technology use, and social integration among adults with spina bifida. Am J Phys Med Rehabil. 2009;88(7):533–41. doi: 10.1097/PHM.0b013e3181aa41d4. [DOI] [PubMed] [Google Scholar]
- [62]. Roebroeck ME, Jahnsen R, Carona C, Kent RM, Chamberlain MA. Adult outcomes and lifespan issues for people with childhood-onset physical disability. Dev Med Child Neurol. 2009;51(8):670–8. doi: 10.1111/j.1469-8749.2009.03322.x. [DOI] [PubMed] [Google Scholar]
- [63]. Kinsman SL, Levey E, Ruffing V, Stone J, Warren L. Beyond multidisciplinary care: a new conceptual model for spina bifida services. Eur J Pediatr Surg. 2000. Dec:10 Suppl 1:35-8. doi: 10.1055/s-2008-1072413. [DOI] [PubMed] [Google Scholar]
- [64]. Lotstein DS, Inkelas M, Hays RD, Halfon N, Brook R. Access to Care for Youth with Special Health Care Needs in the Transition to Adulthood. J Adolesc Health. 2008;43(1):23–9. doi: 10.1016/j.jadohealth.2007.12.013. [DOI] [PubMed] [Google Scholar]
- [65]. Coakley RM, Holmbeck GN, Bryant FB. Constructing a Prospective Model of Psychosocial Adaptation in Young Adolescents with Spina Bifida: An Application of Optimal Data Analysis. J Pediatr Psychol. 2006;31(10):1084–99. doi: 10.1093/jpepsy/jsj032. [DOI] [PubMed] [Google Scholar]
- [66]. Bellin MH, Dosa N, Zabel TA, et al. Self-Management, Satisfaction With Family Functioning, and the Course of Psychological Symptoms in Emerging Adults With Spina Bifida. J Pediatr Psychol. 2013;38(1):50–62. doi: 10.1093/jpepsy/jss095. [DOI] [PubMed] [Google Scholar]
- [67]. Beal SJ, Riddle IK, Kichler JC, et al. The Associations of Chronic Condition Type and Individual Characteristics with Transition Readiness. Acad Pediatr. 2016;16(7):660–7. doi: 10.1016/j.aca2016.06.007. [DOI] [PubMed] [Google Scholar]
- [68]. Loomis JW, Javornisky JG, Monahan JJ, Burke G, Lindsay A. Relations between family environment and adjustment outcomes in young adults with spina bifida. Dev Med Child Neurol. 1997. Sep;39(9):620–7. doi: 10.1111/j.1469-8749.1997.tb07498.x. [DOI] [PubMed] [Google Scholar]
- [69]. Hunt GM, Oakeshott P. Outcome in people with open spina bifida at age Prospective community-based cohort study. Br Med J. 2003;326(7403):1365–6. doi: 10.1136/bmj.326.7403.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70]. Bowman RM, McLone DG, Grant JA, et al. Spina bifida outcome: A 25-year prospective. Pediatr Neurosurg. 2001;34(3):114–20. doi: 10.1159/000056005. [DOI] [PubMed] [Google Scholar]
- [71]. White PH, Cooley WC. Supporting the Health Care Transition from Adolescence to Adulthood in the Medical Home. Pediatrics. 2018;142(5):20182587. doi: 10.1542/peds.2018-2587. [DOI] [PubMed] [Google Scholar]
- [72]. Wiener JS, Suson KD, Castillo J, et al. Bowel management and continence in adults with spina bifida: Results from the National Spina Bifida Patient Registry 2009-15. J Pediatr Rehabil Med. 2017;10(3-4):335–43. doi: 10.3233/PRM-170466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73]. King G, Shultz I, Steel K, Gilpin M, Cathers T. Self-evaluation and self-concept of adolescents with physical disabilities. Am J Occup Ther. 1993;47(2):132–40. doi: 10.5014/ajot.47.2.132. [DOI] [PubMed] [Google Scholar]
- [74].Healthy and Ready to Work Transition Models Project Summary of Effective Approaches. Boston, MA: John Snow, Inc; 2008.
- [75]. Woodward JF, Swigonski NL, Ciccarelli MR. Assessing the health, functional characteristics, and health needs of youth attending a noncategorical transition support program. J Adolesc Health. 2012;51(3):272–8. doi: 10.1016/j.jadohealth.2011.12.016. [DOI] [PubMed] [Google Scholar]
- [76]. Rauen KK, Sawin KJ, Bartelt T, Waring WP, Orr M, O’Connor RC. Transitioning adolescents and young adults with a chronic health condition to adult healthcare - An exemplar program. Rehabil Nurs. 2013;38(2):63–72. doi: 10.1002/rnj.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77]. West C, Brodie L, Dicker J, Steinbeck K. Development of health support services for adults with spina bifida Development of health support services for adults with spina bifida. Disabil Rehabil. 2011;33(23-24):2381–8. doi: 10.3109/09638288.2011.568664. [DOI] [PubMed] [Google Scholar]
- [78]. Le JT, Mukherjee S. Transition to Adult Care for Patients with Spina Bifida. Phys Med Rehabil Clin N Am. 2015;26(1):29–38. doi: 10.1016/j.pmr.2014.09.007. [DOI] [PubMed] [Google Scholar]
- [79]. Grimsby GM, Burgess R, Culver S, Schlomer BJ, Jacobs MA. Barriers to transition in young adults with neurogenic bladder. J Pediatr Urol. 2016;12(4):258.e1–258.e5. doi: 10.1016/j.jpurol.2016.04.015. [DOI] [PubMed] [Google Scholar]
- [80]. Timberlake MD, Corbett ST, Costabile RA, Herndon CDA. Identification of adolescent and adult patients receiving pediatric urologic care and establishment of a dedicated transition clinic. J Pediatr Urol. 2015;11(2):62.e1–6. doi: 10.1016/j.jpurol.2014.11.013. [DOI] [PubMed] [Google Scholar]
- [81]. Lindsay S, Hartman LR, Fellin M. A systematic review of mentorship programs to facilitate transition to post-secondary education and employment for youth and young adults with disabilities. Disabil Rehabil. 2016;38(14):1329–49. doi: 10.3109/09638288.2015.1092174. [DOI] [PubMed] [Google Scholar]
- [82]. Betz CL, O’Kane LS, Nehring WM, Lobo ML. Systematic review: Health care transition practice service models. Nurs Outlook. 2016;64(3):229–43. doi: 10.1016/j.outlook.2015.12.011. [DOI] [PubMed] [Google Scholar]
- [83]. Summers SJ, Elliott S, Mcadams S, et al. Urologic Problems in Spina Bifida Patients Transitioning to Adult Care. Urology. 2014;84(2):440–4. doi: 10.1016/j.urology.2014.03.041. [DOI] [PubMed] [Google Scholar]
- [84]. Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128(1):182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]