Abstract
Objective:
To examine prospectively associations of neighborhood opportunity with the presence of dampness or pests in the home environment during early adolescence.
Study Design:
We geocoded residential addresses from 831 children (mean age 7.9 years, 2007–2011) in the Project Viva cohort. We linked each address with census tract-level Child Opportunity Index scores, which capture neighborhood conditions and resources influencing child heath including educational, health, environmental, and socioeconomic factors. Our primary outcome was presence of dampness or pests in the home in early adolescence (mean age 13.2 years, 2013–2016). Secondary outcomes included current asthma and lung function testing results. Mixed-effects regression models estimated longitudinal associations of Child Opportunity Index scores with outcomes, adjusting for individual and family sociodemographics.
Results:
Children residing in neighborhoods with higher overall opportunity were less likely to live in homes with dampness or pests approximately 5 years later (adjusted odds ratio = 0.85 per 20-unit increase in Child Opportunity Index percentile rank, 95% confidence interval 0.73, 0.998). We observed no significant associations in adjusted models of overall neighborhood opportunity with current asthma or lung function. Lower school poverty or single-parent households and higher access to healthy food or economic resource index were associated with lower odds of a home environment with dampness or pests.
Conclusions:
More favorable neighborhood conditions in mid-childhood were associated with lower likelihood of living in a home with dampness or pests in the early adolescence.
Keywords: asthma, neighborhoods, household asthma triggers, health inequities
Striking health inequities exist in the prevalence and severity of childhood asthma, driven by structural factors including poverty and racism.[1–7] Asthma is a leading indication for emergency department visits and hospitalizations in children.[8,9] Asthma is a major driver of pediatric health inequity, with marked disparities and widespread prevalence.
There is growing recognition that social and environmental conditions in which children reside influence their health, both in homes and neighborhoods.[10] Community poverty manifests as limited neighborhood resources and adverse physical conditions, harming children’s health and deepening health inequities.[11,12] “Neighborhood opportunity” describes the conditions and resources in the community that influence child development and long-term health.[13–17] These neighborhood conditions include educational, health, environmental, and socioeconomic factors. [16,17] The Child Opportunity Index is a surveillance tool that incorporates traditional (e.g., median household income) and novel (e.g., access to healthy food choices or green space) attributes of neighborhood conditions and resources important for child health and development.[16–19]
Children living in neighborhoods with less favorable opportunities, defined by lower Child Opportunity Index scores, have higher rates of emergency department visits and hospitalizations for asthma.[20–22] The ways in which neighborhood conditions and resources for children influence asthma symptoms and severity, however, is not clear. Establishing the mechanisms of this relationship would inform interventions and policies to improve health for vulnerable children with asthma and advance health equity in children.
To address these knowledge gaps, we examined associations of neighborhood opportunity for children (defined by the Child Opportunity Index) with the presence of dampness or pests in the home, as well as with respiratory outcomes including lung function and current asthma. We hypothesized that children residing in neighborhoods with less favorable opportunity in mid-childhood and early adolescence would be more likely to live in home environments with dampness or pests in early adolescence.
Methods
Study Sample
Project Viva is a study of prenatal and postnatal factors affecting maternal and child health.[23] We recruited eligible pregnant women at their first prenatal visit between April 1999 and November 2002. Participants were recruited from obstetric practices at Atrius Harvard Vanguard Medical Associates in eastern Massachusetts. Mothers provided written informed consent at enrollment and follow-up study visits. Children provided verbal assent at study visits beginning in mid-childhood. The Institutional Review Board at Harvard Pilgrim Health Care approved the project.
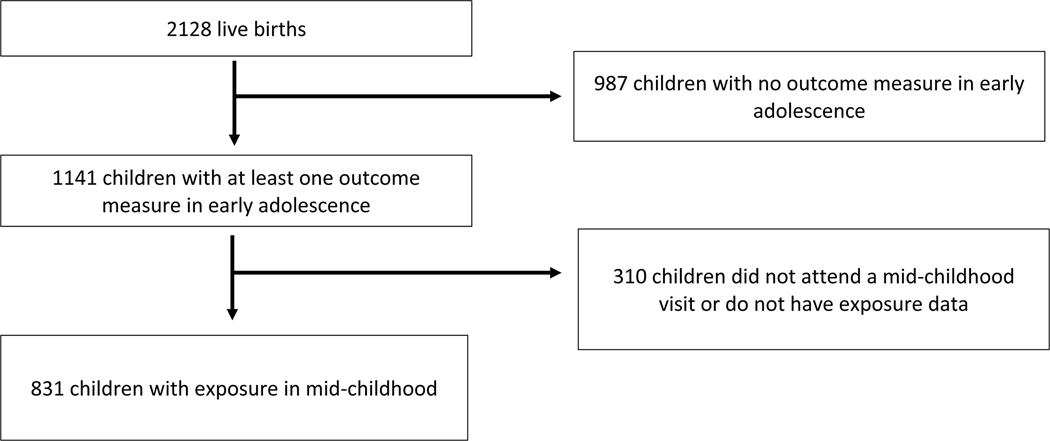
Of 2128 live singleton births, we excluded 987 children with no outcome measures in early adolescence (2013–2016) and an additional 310 children who did not attend a mid-childhood visit or do not have exposure data (2007–2011), leaving 831 participants in our sample (Figure 1; online).
Figure 1. Flowchart of study sample from Project Viva cohort.
Exposure: Child Opportunity Index
We geocoded each participant’s residential address at mid-childhood (mean age 7.9 years, SD 0.8) and early adolescence (mean age 13.1 years, SD 0.9) using ArcGIS (Esri, Redlands, CA). We linked the census tract location at mid-childhood (2007–2011) to Child Opportunity Index data for the year 2010, while census tract locations in early adolescence (2013–2016) were linked to data for the year 2015.
The Child Opportunity Index as a summary measure of the quality of neighborhoods in which children live across the US developed by researchers.[17] Briefly, the index includes 29 indicators of neighborhood quality – drawn from public sources including the Census Bureau, the National Center for Education Statistics, the Department of Agriculture, and the Environmental Protection Agency – and grouped into 3 domains: education, health and environment, and social and economic (Table 1; online).
Table 1.
Child Opportunity Index indicators and sources of data
| Indicators | Definition (Data source and Year) |
|---|---|
| Education domain | |
| 1. Early Childhood Education (ECE) centers | Number of ECE centers within a 5-mile radius (own data collection from state and federal sources; 2010) |
| 2. High-quality ECE centers | Number of National Association for the Education of Young Children accredited centers within a 5-mile radius (own data collection from state and federal sources; 2010) |
| 3. ECE enrollment | Percent 3- and 4-year-olds enrolled in nursery school, preschool or kindergarten (ACS; 2008–2012) |
| 4. Third grade reading proficiency | Percent third graders scoring proficient on standardized reading tests, converted to NAEP scale score points (EDFacts, GS and SEDA; 2010) |
| 5. Third grade math proficiency | Percent third graders scoring proficient on standardized math tests, converted to NAEP scale score points (EDFacts, GS and SEDA; 2010) |
| 6. High school graduation rate | Percent ninth graders graduating from high school on time (EDFacts and GS; 2010) |
| 7. Advanced Placement (AP) course enrollment | Ratio of students enrolled in at least one AP course to the number of 11th and 12th graders (CRDC; 2011) |
| 8. College enrollment in nearby institutions | Percent 18–24 year-olds enrolled in college within 25-mile radius (ACS; 2008–2012) |
| 9. School povertyb | Percent students in elementary schools eligible for free or reduced-price lunches, reversed (NCES CCD; 2010) |
| 10. Teacher experienceb | Percent teachers in their first and second year (CRDC; 2011) |
| 11. Adult educational attainment | Percent adults ages 25 and over with a college degree or higher (ACS; 2008–2012) |
| Health and Environment domain | |
| 1. Access to healthy foodb | Percent households without a car located further than a half-mile from the nearest super-market, reversed (USDA; 2010) |
| 2. Access to green spaceb | Percent impenetrable surface areas such as rooftops, roads or parking lots (CDC; 2011) |
| 3. Walkability | EPA Walkability Index (EPA; 2010–2012) |
| 4. Housing vacancy rateb | Percent housing units that are vacant (ACS; 2008–2012) |
| 5. Hazardous waste dump sitesb | Average number of Superfund sites within a 2-mile radius (EPA; 2010) |
| 6. Industrial pollutants in air, water or soilb | Index of toxic chemicals released by industrial facilities (EPA; 2010) |
| 7. Airborne microparticlesb | Mean estimated microparticle (PM2.5) concentration (CDC; 2010) |
| 8. Ozone concentrationb | Mean estimated 8-hour average ozone concentration (EPA; 2011) |
| 9. Extreme heat exposureb | Summer days with maximum temperature above 90 degrees Fahrenheit (CDC; 2009–2011) |
| 10. Health insurance coverage | Percent individuals ages 0–64 with health insurance coverage (ACS; 2008–2012) |
| Social and Economic domain | |
| 1. Employment rate | Percent adults ages 25–54 who are employed (ACS; 2008–2012) |
| 2. Commute durationb | Percent workers commuting more than one hour one way (ACS; 2008–2012) |
| 3. Poverty rateb | Percent individuals living in households with incomes below 100% of the federal poverty threshold (ACS; 2008–2012) |
| 4. Public assistance rateb | Percent households receiving cash public assistance or Food Stamps/Supplemental |
| Nutrition Assistance Program (ACS; 2008–2012) | |
| 5. Home ownership rate | Percent owner-occupied housing units (ACS; 2008–2012) |
| 6. High-skill employment | Percent individuals ages 16 and over employed in management, business, financial, computer, engineering, science, education, legal, community service, health care practitioner, health technology, arts and media occupations (ACS; 2008–2012) |
| 7. Median household income | Median income of all households (ACS; 2008–2012) |
| 8. Single-headed householdsb | Percent family households that are single-parent headed (ACS; 2008–2012) |
Adapted from the Child Opportunity Index: Technical Documentation.
Scores are reversed so higher scores reflect higher opportunity levels.
ACS: American Community Survey; CDC: Center for Disease Control and Prevention; CRDC: U.S. Department of Education Office for Civil Rights Data Collection; EDFacts: U.S. Department of Education Data Files; EPA: Environmental Protection Agency; GS: Great Schools data; NAEP: National Assessment of Educational Progress; NCES CCD: National Center for Education Statistics Common Core of Data; SEDA: Stanford Education Data Archive; USDA: U.S. Department of Agriculture
The developers generated z-scores (mean 0, SD 1) for each of the 29 indicators for 72,195 census tracts across 50 US states and Washington D.C. These scores were standardized at the national level such that higher scores reflect more favorable neighborhood opportunities, such as higher median household income, better access to early childhood education, and more green spaces, relative to other neighborhoods across the US. Additionally, the developers derived a domain-specific and overall Child Opportunity Index score, and generated percentile ranks for each census tract based on domain-specific and overall Child Opportunity Index scores, ranging from 1st (lowest opportunity) to 100th percentile (highest opportunity). In accordance with prior literature,[17] we further grouped census tract rankings into quintiles: very low (<20th percentile), low (20th–<40th percentile), moderate (40th–<60th percentile), high (60th–<80th percentile), or very high opportunity (≥80th percentile). Detailed methods are published.[16,17,24]
Outcomes
Presence of Dampness or Pests in the Home
In early adolescence (mean age 13.1 years), we used parental reports of presence of dampness or pests in the home, obtained from study questionnaires derived from the International Study of Asthma and Allergies in Childhood.[25] We considered dampness or pests to be present in the home if the parent answered “yes” to any of the following questions: (1) “Is there any moisture or mildew in your home on the ceiling, walls, or windows?”, (2) In the past 12 months, has there been water damage to the building or its contents (for example, broken pipes, leaks, or a flood)?”, (3) “In the past 12 months, has water collected on the basement floor?”, (4) “In the past 12 months, have you seen or noticed signs of any of the following in your home? a) cockroaches, b) rats or mice.”
Lung Function
Trained research assistants obtained lung function measurements in early adolescence, including forced expiratory volume (FEV1) and forced vital capacity (FVC). Measurements were obtained using the Easy One Spirometer (NDD Medical Technologies, Andover, MA).[26] The study participant produced three acceptable spirograms, of which two had to be reproducible.[27] For this study, lung function was captured using FEV1/FVC ratio.
Current Asthma
A participant was considered to have a current diagnosis of asthma in early adolescence if the parent reported ever having a diagnosis of asthma from a doctor on the study questionnaire and also one of the following: (1) parental report of wheeze in the last 12 months or (2) asthma medication use in the last 12 months. Parental report of wheeze was considered positive if they answered “yes” to the question, “In the past 12 months, has your child ever had wheezing (or whistling in the chest)?”.
Covariates
Mothers enrolled in Project Viva reported their highest education level, smoking history, asthma history, household income, and their partner’s asthma history via questionnaires and interviews at the time of recruitment. We categorized maternal education as having obtained a college degree, smoking history as never smoked, smoked before pregnancy, or smoked during pregnancy, and household income as above or below $70,000 per year. Mothers reported their child’s race and ethnicity, which we categorized as White, Black, Hispanic, Asian, or other. We viewed race and ethnicity as societal constructs rather than deterministic biological causes of risk and considered it as a proxy measure of racism that can affect both residence in high opportunity neighborhoods and asthma.[28] We obtained child sex at birth from hospital medical records from the delivery. We chose these covariates based on existing literature on the relationship between the Child Opportunity Index and child health.[21,29]
Statistical Analyses
We used mixed-effect logistic models to estimate the associations of census tract-level Child Opportunity Index scores and the following outcomes in early adolescence: (1) presence of dampness or pests in the home, (2) current asthma versus never having a diagnosis of asthma and (3) lung function.
The primary analyses examined longitudinal associations for overall and domain-specific Child Opportunity Index scores in mid-childhood as continuous variables and the outcomes in early adolescence, using national-level Child Opportunity index scores. To identify specific indicators potentially driving these associations, we performed secondary analyses that examined the associations of the 29 specific indicators with the outcomes.
We conducted sensitivity analyses examining the cross-sectional associations for overall and domain-specific Child Opportunity Index scores and outcomes in early adolescence. We estimated the associations for overall and domain-specific Child Opportunity Index scores in early adolescence as continuous variables using national-level Child Opportunity Index scores.
For all analyses, we included the following variables as fixed effects: Child Opportunity Index percentile ranks, sex at birth, and race and ethnicity, maternal education, smoking history, household income, and parental history of asthma prior to the child’s birth. For models with lung function as the outcome, we additionally included child age and height in early adolescence. We included a random effect term for census tract to account for clustering of children residing within the same neighborhood. We did not adjust for multiple comparisons, consistent with the literature on the Child Opportunity Index,[18–22,30] which reflects this common practice in multiple regression analyses.[31] We performed all analyses using SAS version 9.4 (SAS Institute, Inc, Cary, NC).
Results
Among the 831 participants, 10% (n=87) resided in neighborhoods with very low overall opportunity and 55% (n=453) resided in neighborhoods with very high overall opportunity in mid-childhood, based on national distributions of the Child Opportunity Index (Table 2). Children in areas of very low opportunity (versus very high) were more likely to be Black or Hispanic, had parents with lower income and educational attainment, and were more likely to born to mothers who smoked tobacco during pregnancy (Table 2).
Table 2.
Individual and Family Characteristics of Children in Project Viva in Early Adolescence by Quintiles of Neighborhood Child Opportunity Index Scores Assessed in Mid-Childhood
| All Participants | Quintiles of Overall Neighborhood Child Opportunity Index Percentile Ranks |
|||||
|---|---|---|---|---|---|---|
| Very Low Opportunity | Low Opportunity | Moderate Opportunity | High Opportunity | Very High Opportunity | ||
| n (% of cohort) | n=831 | n=87 (10%) | n=38 (5%) | n=74 (9%) | n=179 (22%) | n=453 (55%) |
|
| ||||||
| Neighborhood Child Opportunity Index Percentile Ranks in Mid-Childhood | ||||||
|
| ||||||
| Overall score, mean (SD) | 72.5 (27.4) | 10.2 (5.1) | 32.6 (4.3) | 49.9 (5.6) | 72.5 (5.9) | 91.4 (5.4) |
| Educational domain, mean (SD) | 74.5 (26.4) | 17.5 (10.1) | 38.5 (14.1) | 52.5 (18.0) | 77.9 (12.6) | 90.8 (6.9) |
| Health and environment domain, mean (SD) | 77.6 (22.7) | 40.9 (21.7) | 42.5 (22.8) | 67.4 (22.5) | 77.5 (17.1) | 89.2 (10.3) |
| Social and economic domain, mean (SD) | 67.9 (27.4) | 8.7 (5.6) | 30.9 (6.3) | 45.0 (8.2) | 65.2 (9.8) | 87.1 (8.6) |
|
| ||||||
| Parental Characteristics | ||||||
|
| ||||||
| Maternal education: college graduate, n (%) | 594 (72%) | 29 (34%) | 17 (45%) | 35 (47%) | 126 (70%) | 387 (86%) |
| Maternal pregnancy smoking status, n (%) | ||||||
| Never smoker | 576 (70%) | 64 (74%) | 23 (61%) | 57 (77%) | 121 (68%) | 311 (69%) |
| Former smoker | 172 (21%) | 7 (8%) | 7 (18%) | 12 (16%) | 38 (21%) | 108 (24%) |
| Smoker during pregnancy | 80 (10%) | 15 (17%) | 8 (21%) | 5 (7%) | 18 (10%) | 34 (8%) |
| Household annual income >$70,000, n (%) | 492 (64%) | 13 (21%) | 8 (27%) | 27 (41%) | 102 (59%) | 342 (79%) |
| Parental asthma (prior to child’s birth), n (%) | 102 (14%) | 16 (22%) | 5 (18%) | 13 (21%) | 21 (14%) | 47 (12%) |
|
| ||||||
| Child Characteristics | ||||||
|
| ||||||
| Age (years) in early adolescence, mean (SD) | 13.1 (0.9) | 13.1 (0.8) | 13.3 (1.1) | 13.4 (1.0) | 13.3 (1.0) | 13.1 (0.8) |
| Race/ethnicity, n (%) | ||||||
| White | 549 (66%) | 3 (3%) | 10 (26%) | 34 (46%) | 132 (74%) | 370 (82%) |
| Black | 126 (15%) | 57 (66%) | 16 (42%) | 23 (31%) | 10 (6%) | 20 (4%) |
| Hispanic | 32 (4%) | 10 (12%) | 5 (13%) | 5 (7%) | 5 (3%) | 7 (2%) |
| Asian | 26 (3%) | 1 (1%) | 1 (3%) | 0 (0%) | 9 (5%) | 15 (3%) |
| Other | 97 (12%) | 15 (17%) | 6 (16%) | 12 (16%) | 23 (13%) | 41 (9%) |
| Female sex at birth, n (%) | 420 (51%) | 40 (46%) | 16 (42%) | 40 (54%) | 80 (45%) | 244 (54%) |
|
| ||||||
| Outcomes in Early Adolescence | ||||||
|
| ||||||
| Dampness or pests in the home, n (%) | 430 (52%) | 51 (59%) | 24 (63%) | 34 (47%) | 90 (51%) | 231 (51%) |
| Moisture or mildew | 156 (20%) | 12 (15%) | 6 (17%) | 14 (21%) | 41 (24%) | 83 (19%) |
| Water damage | 252 (32%) | 33 (40%) | 13 (36%) | 20 (30%) | 58 (34%) | 128 (29%) |
| Cockroaches, rats, or mice | 214 (26%) | 25 (29%) | 13 (34%) | 17 (24%) | 39 (22%) | 120 (27%) |
| Asthma status, n (%) | ||||||
| Current asthma | 102 (12%) | 16 (19%) | 5 (13%) | 13 (18%) | 21 (12%) | 47 (11%) |
| Previous asthma | 111 (14%) | 14 (16%) | 10 (26%) | 12 (16%) | 26 (15%) | 49 (11%) |
| Never asthma | 608 (74%) | 56 (65%) | 23 (61%) | 48 (66%) | 130 (73%) | 351 (79%) |
| Lung Function Testing | ||||||
| FEV1/FVCa, mean (SD) | 0.85 (0.06) | 0.84 (0.06) | 0.84 (0.08) | 0.84 (0.07) | 0.85 (0.07) | 0.85 (0.06) |
FEV1, forced expiratory volume in the first second; FVC, forced vital capacity
Associations of Overall and Domain-specific Child Opportunity Index Scores in Mid-childhood with Outcomes in Early Adolescence
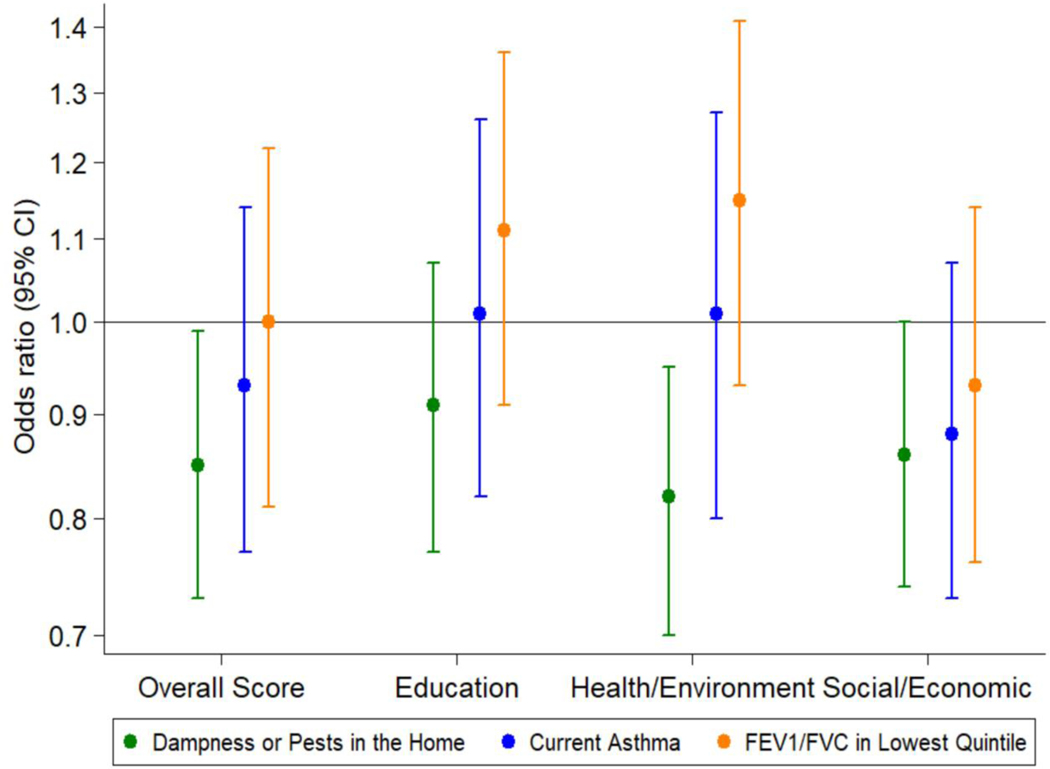
After adjusting for individual and family characteristics, children residing in neighborhoods with higher overall opportunity in mid-childhood were less likely to live in homes with dampness or pests in early adolescence (odds ratio [OR] = 0.85 per 20-unit increase in Child Opportunity Index percentile rank, 95% confidence interval [CI] 0.73, 0.998). We detected no associations of overall Child Opportunity Index scores with current asthma or lung function, as measured by FEV1/FVC (Table 3, Figure 2).
Table 3.
Unadjusted and adjusted longitudinal associations of neighborhood Child Opportunity Index scores in mid-childhood (overall and domain-specific) with the presence of dampness or pests in the home, current asthma, and lung function (FEV1/FVC) in early adolescence.
| Neighborhood Child Opportunity Index Score | Dampness or Pests in the Home | Current Asthma | FEV1/FVC (*100) | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | β (95% CI) | ||||
| Unadjusted | Adjusteda | Unadjusted | Adjusteda | Unadjusted | Adjustedb | |
| Overall | 0.92 (0.84, 1.02) | 0.85 (0.73, 1.00) | 0.81 (0.70, 0.92) | 0.93 (0.77, 1.14) | 0.35 (0.01, 0.69) | 0.23 (−0.25, 0.71) |
| Education Domain | 0.95 (0.86, 1.05) | 0.91 (0.77, 1.07) | 0.83 (0.72, 0.97) | 1.01 (0.82, 1.26) | 0.19 (−0.17, 0.54) | −0.08 (−0.58, 0.42) |
| Health and Environment Domain | 0.87 (0.77, 0.98) | 0.82 (0.70, 0.95) | 0.84 (0.71, 1.00) | 1.01 (0.80, 1.27) | 0.29 (−0.12, 0.70) | 0.06 (−0.41, 0.53) |
| Social and Economic Domain | 0.93 (0.84, 1.02) | 0.86 (0.74, 1.00) | 0.79 (0.69, 0.90) | 0.88 (0.73, 1.07) | 0.42 (0.08, 0.76) | 0.36 (−0.10, 0.82) |
Odds ratios and effect estimates reflect a per 20-unit increase in Child Opportunity Index scores. OR = odds ratio; CI = confidence interval, FEV1 = forced expiratory volume in the first second, FVC = forced vital capacity.
Mixed effects logistic regression models adjusted for sex at birth, race/ethnicity, maternal education, pregnancy smoking status, household income, parental asthma prior to the child’s birth, and for clustering by census tract.
Mixed effects linear regression models adjusted for sex at birth, race/ethnicity, age and height at the early adolescent visit, maternal education, pregnancy smoking status, household income, parental asthma prior to the child’s birth, and clustering by census tract.
Figure 2. Longitudinal associations of overall and domain-specific neighborhood Child Opportunity Index scores in mid-childhood with presence of dampness or pests in the home, current asthma, and FEV1/FVC in the lowest quintile in early adolescence.
Odds ratios and effect estimates reflect a per 20-unit increase in Child Opportunity Index scores. All models are adjusted for sex at birth, race/ethnicity, maternal education, prenatal smoking exposure, household income, parental asthma prior to the child’s birth, and clustering by census tract. Models predicting FEV1/FVC in the lowest quintile are additionally adjusted for age and height at the early adolescent visit. OR = odds ratio; CI = confidence interval, FEV1 = forced expiratory volume in the first second, FVC = forced vital capacity.
Children residing in neighborhoods with higher health and environment opportunity were less likely to live in a home with dampness or pests in unadjusted and adjusted models (unadjusted OR = 0.87 per 20-unit increase in Child Opportunity Index percentile rank, 95% CI 0.77, 0.98, adjusted OR = 0.82 per 20-unit increase in Child Opportunity Index percentile rank, 95% CI 0.70, 0.95). Estimates for the social and economic domain scores with the presence of dampness or pests in the home were similar to those for the health and environment domain, but minimally exceeded statistical significance; no associations were noted for the education domain (Table 3, Figure 2).
Children residing in neighborhoods with higher overall opportunity, higher educational opportunity, and higher social and economic opportunity were less likely to have current asthma in unadjusted models. Children in neighborhoods with higher social and economic opportunity had better lung function in unadjusted models. These associations were attenuated in adjusted models (Table 3, Figure 2).
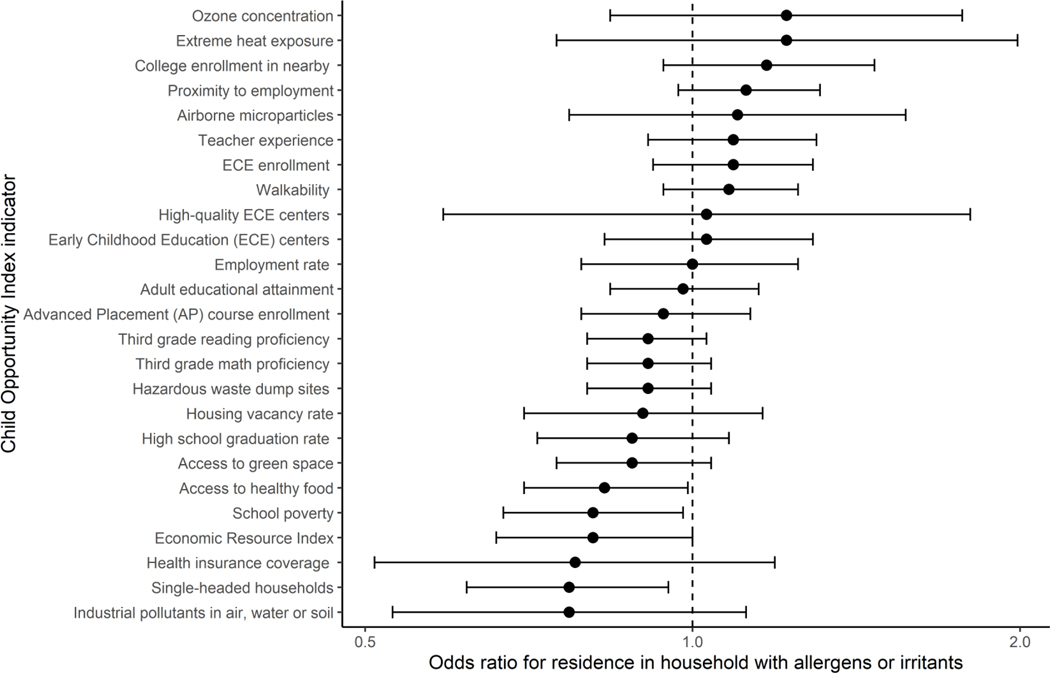
Associations of Each Indicator of Neighborhood Opportunity in Mid-childhood with Outcomes in Early Adolescence
After adjusting for individual and family characteristics, children who resided in neighborhoods with lower levels of school poverty (OR = 0.81 per 1-SD increase, 95% CI 0.67, 0.98), better access to healthy foods (OR = 0.83 per 1-SD increase, 95% CI 0.70, 0.99), higher economic resource index scores (OR = 0.81 per 1-SD increase, 95% CI 0.66, 0.99), and lower rate of single parent households (OR = 0.77 per 1-SD increase, 95% CI 0.62, 0.95) in mid-childhood were less likely to live in homes with dampness or pests in early adolescence (Figure 3).
Figure 3. Longitudinal associations of specific indicators of Child Opportunity Index scores in mid-childhood with the presence of dampness or pests in the home in early adolescence.
Odds ratios and effect estimates reflect a per z-score increase in Child Opportunity Index scores. All models are adjusted for sex at birth, race/ethnicity, maternal education, prenatal smoking exposure, household income, parental asthma prior to the child’s birth, and clustering by census tract. Higher scores reflect higher opportunity levels for all items.
Sensitivity Analysis
Our cross-sectional analysis in early adolescence revealed similar associations between neighborhood opportunity and homes with dampness or pests, current asthma, or lung function. The association of the social and economic domain scores with the presence of dampness or pests in the home was statistically significant in this model (Table 4; online).
Table 4.
Unadjusted and adjusted cross-sectional associations of neighborhood Child Opportunity Index scores (overall and domain-specific) with presence of dampness or pests in the home, current asthma, and lung function (FEV1/FVC) in early adolescence.
| Neighborhood Child Opportunity Index Score | Dampness or Pests in the Home | Current Asthma | FEV1/FVC (*100) | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | β (95% CI) | ||||
| Unadjusted | Adjusteda | Unadjusted | Adjusteda | Unadjusted | Adjustedb | |
| Overall | 0.89 (0.81, 0.98) | 0.84 (0.73, 0.96) | 0.81 (0.72, 0.91) | 0.98 (0.82, 1.17) | 0.33 (0.01, 0.65) | 0.27 (−0.16, 0.70) |
| Education Domain | 0.90 (0.80, 1.01) | 0.85 (0.72, 1.00) | 0.84 (0.72, 0.98) | 1.09 (0.87, 1.36) | 0.23 (−0.15, 0.61) | 0.06 (−0.45, 0.57) |
| Health and Environment Domain | 0.94 (0.84, 1.07) | 0.91 (0.78, 1.05) | 0.84 (0.72, 0.99) | 0.95 (0.77, 1.16) | 0.45 (0.03, 0.87) | 0.36 (−0.13, 0.84) |
| Social and Economic Domain | 0.90 (0.83, 0.99) | 0.87 (0.76, 0.99) | 0.80 (0.71, 0.91) | 0.94 (0.80, 1.11) | 0.32 (0.01, 0.63) | 0.26 (−0.13, 0.65) |
Odds ratios and effect estimates reflect a per 20-unit increase in Child Opportunity Index scores. OR = odds ratio; CI = confidence interval, FEV1 = forced expiratory volume in the first second, FVC = forced vital capacity.
Mixed effects logistic regression models adjusted for sex at birth, race/ethnicity, maternal education, pregnancy smoking status, household income, biparental asthma prior to the child’s birth, and for clustering by census tract.
Mixed effects linear regression models adjusted for sex at birth, race/ethnicity, age and height at the early adolescent visit, maternal education, pregnancy smoking status, household income, parental asthma prior to the child’s birth, and clustering by census tract.
Discussion
We found longitudinal and cross-sectional associations of neighborhoods with more favorable opportunities for children with lower likelihood of residence in a home with dampness or pests. These associations were independent of individual and family social characteristics. We noted certain indicators of neighborhood opportunity – i.e., lower school poverty rate, better access to healthy food, lower economic resource index, and lower rate of single-parent households – were associated with lower likelihood of residing in a home with dampness or pests. However, we found no associations in adjusted analyses for neighborhood opportunity and asthma or lung function.
A recent study suggested a link between neighborhood conditions at birth and childhood wheezing and asthma, which is consistent with the body of literature on neighborhoods and asthma.[32] We did not detect associations with asthma likely due to limited power in this smaller sample size that was primarily from high opportunity communities, or potentially because we examined the exposure in a different life stage at mid-childhood and not at birth. We do not believe these findings indicate that a relationship between community conditions and asthma does not exist.
Prior literature utilizing the Child Opportunity Index has highlighted marked inequities in asthma severity for children who live in communities with less favorable neighborhood opportunities.[20–22,33] Hospitalizations for asthma in children in Kansas City and Cincinnati were more than five times higher in neighborhoods with very low opportunity compared with those with very high opportunity.[20] In a study of one Ohio county, children in neighborhoods with very low opportunity also had greater than five times the rate of hospitalizations for asthma compared with children with very high opportunity.[22] Children in neighborhoods with very low opportunity had five times greater rates of hospital or emergency department utilization for asthma.[22] In San Francisco, children living in neighborhoods with very low opportunity have higher odds of seeking acute or emergency care for asthma.[21] Geographic hotspots in Atlanta for pediatric intensive care unit admissions for asthma requiring mechanical ventilation had substantially lower neighborhood opportunity compared with other neighborhoods.[33]
Despite strong evidence for a relationship between lower neighborhood opportunity for children and more severe asthma, the pathways by which neighborhood conditions affect outcomes in asthma are not well-defined. In this study, we provide evidence of both longitudinal and cross-sectional relationships between neighborhood opportunity for children and the presence of dampness or pests in the home in childhood. In the context of the extant literature, we speculate household exposures may be a potential driver of higher hospitalizations and emergency visits for asthma among children who reside in neighborhoods with less favorable conditions from mid-childhood to early adolescence.
Potential explanations for the observed association between less favorable neighborhood conditions and the presence of dampness or pests in the home may include poor housing stock, challenges to repairing homes, and effects of climate change.[34,35] Systematic reviews of the literature have demonstrated a link between dampness and pests in the home and asthma in children, as well as improving asthma severity with interventions to reduce exposure to these irritants in the home environment.[36–38] In this analysis, the longitudinal association is driven by the health and environment domain, yet the cross-sectional association is driven by the education domain, suggesting a dynamic vulnerability to neighborhood factors over the life course. Further investigation is required to confirm these findings and evaluate the possible mechanisms.
Interventions to improve the prevalence and severity of asthma in children through the reduction of allergens and irritants have been effective in individual homes and schools.[38–41] The use of neighborhood opportunity to predict exposure to presence of dampness and pests in the home extends the potential for interventions beyond the individual-level. The value of this study is in the identification of the Child Opportunity Index as (1) a potential neighborhood-level target for identifying and targeting high-risk children and (2) a means to tailor interventions to address disparities in high-risk communities. The Child Opportunity Index may serve as the foundation for location-based initiatives[42] to improve asthma outcomes in children by supporting healthy environments and reducing exposures to dampness and pests in homes. Future research is needed to characterize and evaluate interventions aimed at specific neighborhood conditions that may be important in promoting health equity in pediatric asthma.
Strengths of this study include the prospective design and outcomes captured using standardized protocols by trained research staff. We used neighborhood indices that not only captured both physical (e.g., access to green space) and social attributes (e.g., access to health care services) but also have been validated for a range of health outcomes.[18,19,43] We also assessed neighborhood opportunity at life stages when children were unlikely to select their place of residence, which reduces the likelihood of self-selection and potential reverse causation bias. We controlled for parental history of asthma, which reduces the likelihood of residential self-selection by parental factors that might influence child respiratory health.
Limitations of the study include the limits to generalizability imposed by the composition of the cohort, which is largely white, high-income, and well-educated. Limited variation in Child Opportunity Index scores may account for the lack associations between the neighborhood opportunity and asthma or lung function. However, with 15% of the cohort residing in very low or low opportunity neighborhoods, we believe there was sufficient variation in the exposure. Furthermore, we defined current diagnosis of asthma and the presence of dampness and pests in the home using parent-reported questionnaires, which are prone to measurement errors. We excluded 61% of the original cohort for lack of residential addresses or outcome measures. Differences between children included and excluded may have led to selection bias. Lastly, we used census tracts as a marker for exposure, which may not capture other areas where children may spend significant time, such as in schools or with secondary caregivers.
Our findings suggest that more favorable neighborhood opportunity for children predicts lower likelihood of residence in homes with dampness or pests. The data suggest that this relationship exists both longitudinally, between mid-childhood and early adolescence, as well as cross-sectionally in early adolescence. These associations appear to be driven by specific indicators in each of the domains of the Child Opportunity Index. Understanding the mechanisms that drive exposure to dampness and pests in the home among children living in low opportunity neighborhoods is critical to inform interventions and policies to improve health in vulnerable populations and advance health equity in children. Further investigation is needed to confirm these associations and characterize neighborhood-based interventions aimed to improve asthma severity utilizing evidence from the Child Opportunity Index.
Funding/Support:
Project Viva is supported by NICHD R01HD034568 and NIH UH3OD023286. Dr. James is supported by NHLBI R01HL150119. Dr. Gold is supported by NIEHS P30ES000002.
Footnotes
Conflicts of Interest: There are no potential conflicts of interest, real or perceived. The listed sponsors had no role in study design, the collection, analysis and interpretation of data, the writing of the report, or the decision to submit the paper for publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Sullivan K, Thakur N. Structural and Social Determinants of Health in Asthma in Developed Economies: a Scoping Review of Literature Published Between 2014 and 2019. Curr Allergy Asthma Rep 2020;20. 10.1007/s11882-020-0899-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Assari S, Lankarani MM. Poverty status and childhood asthma in white and black families: National survey of children’s health. Healthc 2018;6. 10.3390/healthcare6020062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Thakur N, Barcelo NE, Borrell LN, Singh S, Eng C, Davis A, et al. Perceived Discrimination Associated With Asthma and Related Outcomes in Minority Youth The GALA II and SAGE II Studies n.d. 10.1016/j.chest.2016.11.027. [DOI] [PMC free article] [PubMed]
- [4].Gaffney AW, Himmelstein DU, Christiani DC, Woolhandler S. Socioeconomic Inequality in Respiratory Health in the US from 1959 to 2018. JAMA Intern Med 2021;181:968–76. 10.1001/jamainternmed.2021.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Brumberg HL, Karr CJ. Ambient air pollution: Health hazards to children. Pediatrics 2021;147. 10.1542/peds.2021-051484. [DOI] [PubMed] [Google Scholar]
- [6].Nkoy FL, Stone BL, Knighton AJ, Fassl BA, Johnson JM, Maloney CG, et al. Neighborhood Deprivation and Childhood Asthma Outcomes, Accounting for Insurance Coverage. Hosp Pediatr 2018;8:59. 10.1542/hpeds.2017-0032. [DOI] [PubMed] [Google Scholar]
- [7].Keet CA, Matsui EC, McCormack MC, Peng RD. Urban residence, neighborhood poverty, race/ethnicity, and asthma morbidity among children on Medicaid. J Allergy Clin Immunol 2017;140:822–7. 10.1016/j.jaci.2017.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Pelletier JH, Rakkar J, Au AK, Fuhrman D, Clark RSB, Horvat CM. Trends in US Pediatric Hospital Admissions in 2020 Compared with the Decade before the COVID-19 Pandemic. JAMA Netw Open 2021;4:e2037227–e2037227. 10.1001/jamanetworkopen.2020.37227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].McDermott KW, Stocks C, Freeman WJ. Overview of Pediatric Emergency Department Visits, 2015: Statistical Brief #242. Agency Healthc Res Qual; Rockville, MD: n.d. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb242-Pediatric-ED-Visits-2015.pdf (accessed March 8, 2022). [PubMed] [Google Scholar]
- [10].Pediatrics AC on C. Poverty and child health in the United States. Pediatrics 2016;137:e20160339. 10.1542/peds.2016-0339. [DOI] [PubMed] [Google Scholar]
- [11].Christian H, Zubrick SR, Foster S, Giles-Corti B, Bull F, Wood L, et al. The influence of the neighborhood physical environment on early child health and development: A review and call for research 2015. 10.1016/j.healthplace.2015.01.005. [DOI] [PubMed]
- [12].Krieger N. Epidemiology and the web of causation: Has anyone seen the spider? Soc Sci Med 1994;39:887–903. 10.1016/0277-9536(94)90202-X. [DOI] [PubMed] [Google Scholar]
- [13].Galster GC, Killen SP. The Geography of Metropolitan Opportunity: A Reconnaissance and Conceptual Framework. Hous Policy Debate 1995;6:7–43. 10.1080/10511482.1995.9521180. [DOI] [Google Scholar]
- [14].Galster G. The Geography of Opportunity 20 Years Later. Hous Policy Debate 2017;27:941–3. 10.1080/10511482.2016.1216745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Galster G, Sharkey P. Spatial foundations of inequality: A conceptual model and empirical overview. RSF 2017;3:1–33. 10.7758/rsf.2017.3.2.01.29780882 [DOI] [Google Scholar]
- [16].Acevedo-Garcia D, McArdle N, Hardy EF, Crisan UI, Romano B, Norris D, et al. The child opportunity index: Improving collaboration between community development and public health. Health Aff 2014;33:1948–57. 10.1377/hlthaff.2014.0679. [DOI] [PubMed] [Google Scholar]
- [17].Acevedo-Garcia D, Noelke C, McArdle N, Sofer N, Hardy EF, Weiner M, et al. Racial and ethnic inequities in children’s neighborhoods: Evidence from the new child opportunity index 2.0. Health Aff 2020;39:1693–701. 10.1377/hlthaff.2020.00735. [DOI] [PubMed] [Google Scholar]
- [18].Aris IM, Rifas-Shiman SL, Jimenez MP, Li LJ, Hivert MF, Oken E, et al. Neighborhood child opportunity index and adolescent cardiometabolic risk. Pediatrics 2021;147:e2020018903. 10.1542/peds.2020-018903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Bouchard ME, Kan K, Tian Y, Casale M, Smith T, De Boer C, et al. Association Between Neighborhood-Level Social Determinants of Health and Access to Pediatric Appendicitis Care. JAMA Netw Open 2022;5. 10.1001/JAMANETWORKOPEN.2021.48865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Krager MK, Puls HT, Bettenhausen JL, Hall M, Thurm C, Plencner LM, et al. The Child Opportunity Index 2.0 and Hospitalizations for Ambulatory Care Sensitive Conditions. Pediatrics 2021;148:e2020032755. 10.1542/peds.2020-032755. [DOI] [PubMed] [Google Scholar]
- [21].Kersten EE, Adler NE, Gottlieb L, Jutte DP, Robinson S, Roundfield K, et al. Neighborhood child opportunity and individual-level pediatric acute care use and diagnoses. Pediatrics 2018;141. 10.1542/peds.2017-2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Beck AF, Huang B, Wheeler K, Lawson NR, Kahn RS, Riley CL. The Child Opportunity Index and Disparities in Pediatric Asthma Hospitalizations Across One Ohio Metropolitan Area, 2011–2013. J Pediatr 2017;190:200–206.e1. 10.1016/j.jpeds.2017.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Oken E, Baccarelli AA, Gold DR, Kleinman KP, Litonjua AA, De Meo D, et al. Cohort profile: project viva. Int J Epidemiol 2015;44:37–48. 10.1093/IJE/DYU008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Noelke C, Mcardle N, Baek M, Huntington N, Huber R, Hardy E, et al. Child Opportunity Index 2.0 Technical Documentation 2020. diversitydatakids.org/research-library/research-brief/how-we-built-it (accessed March 8, 2020).
- [25].Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J 1995;8:483–91. 10.1183/09031936.95.08030483. [DOI] [PubMed] [Google Scholar]
- [26].Man Tse S, Gold DR, Sordillo JE, Hoffman EB, Gillman MW, Rifas-Shiman SL, et al. Diagnostic accuracy of the bronchodilator response in children n.d. 10.1016/j.jaci.2013.03.031. [DOI] [PMC free article] [PubMed]
- [27].Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J 2005;26:319–38. 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- [28].Flanagin A, Frey T, Christiansen SL. Updated Guidance on the Reporting of Race and Ethnicity in Medical and Science Journals. JAMA - J Am Med Assoc 2021;326:621–7. 10.1001/jama.2021.13304. [DOI] [PubMed] [Google Scholar]
- [29].Roubinov DS, Hagan MJ, Boyce WT, Adler NE, Bush NR. Family socioeconomic status, cortisol, and physical health in early childhood: The role of advantageous neighborhood characteristics. Psychosom Med 2018;80:492–501. 10.1097/PSY.0000000000000585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Shanahan KH, Subramanian SV, Burdick KJ, Monuteaux MC, Lee LK, Fleegler EW. Association of Neighborhood Conditions and Resources for Children with Life Expectancy at Birth in the US. JAMA Netw Open 2022;5:E2235912. 10.1001/jamanetworkopen.2022.35912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Streiner DL. Best (but oft-forgotten) practices: The multiple problems of multiplicity-whether and how to correct for many statistical tests. Am J Clin Nutr 2015;102:721–8. 10.3945/ajcn.115.113548. [DOI] [PubMed] [Google Scholar]
- [32].Zanobetti A, Ryan PH, Coull B, Brokamp C, Datta S, Blossom J, et al. Childhood Asthma Incidence, Early and Persistent Wheeze, and Neighborhood Socioeconomic Factors in the ECHO/CREW Consortium. JAMA Pediatr 2022. 10.1001/JAMAPEDIATRICS.2022.1446. [DOI] [PMC free article] [PubMed]
- [33].Najjar N, Opolka C, Fitzpatrick AM, Grunwell JR. Geospatial Analysis of Social Determinants of Health Identifies Neighborhood Hot Spots Associated With Pediatric Intensive Care Use for Life-Threatening Asthma. Pediatr Crit Care Med 2022. 10.1097/PCC.0000000000002986. [DOI] [PMC free article] [PubMed]
- [34].Xu Z, Crooks JL, Davies JM, Khan AF, Hu W, Tong S. The association between ambient temperature and childhood asthma: a systematic review. Int J Biometeorol 2018;62:471–81. 10.1007/S00484-017-1455-5. [DOI] [PubMed] [Google Scholar]
- [35].Xu Z, Huang C, Hu W, Turner LR, Su H, Tong S. Extreme temperatures and emergency department admissions for childhood asthma in Brisbane, Australia. Occup Environ Med 2013;70:730–5. 10.1136/oemed-2013-101538. [DOI] [PubMed] [Google Scholar]
- [36].Dick S, Friend A, Dynes K, AlKandari F, Doust E, Cowie H, et al. A systematic review of associations between environmental exposures and development of asthma in children aged up to 9 years. BMJ Open 2014;4. 10.1136/BMJOPEN-2014-006554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Kanchongkittiphon W, Gaffin JM, Phipatanakul W. The indoor environment and inner-city childhood asthma. Asian Pacific J Allergy Immunol 2014;32:103–10. [PMC free article] [PubMed] [Google Scholar]
- [38].Wu F, Takaro TK. Childhood asthma and environmental interventions. Environ Health Perspect 2007;115:971–5. 10.1289/EHP.8989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Eggleston PA, Butz A, Rand C, Curtin-Brosnan J, Kanchanaraksa S, Swartz L, et al. Home environmental intervention in inner-city asthma: a randomized controlled clinical trial. Ann Allergy Asthma Immunol 2005;95:518–24. 10.1016/S1081-1206(10)61012-5. [DOI] [PubMed] [Google Scholar]
- [40].Morgan WJ, Crain EF, Gruchalla RS, O’Connor GT, Kattan M, Evans R, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med 2004;351:1068–80. 10.1056/NEJMOA032097. [DOI] [PubMed] [Google Scholar]
- [41].Vesper SJ, Wymer L, Coull BA, Koutrakis P, Cunningham A, Petty CR, et al. HEPA filtration intervention in classrooms may improve some students’ asthma. J Asthma 2022. 10.1080/02770903.2022.2059672. [DOI] [PMC free article] [PubMed]
- [42].Chan M, Gray M, Burns C, Owens L, Woolfenden S, Lingam R, et al. Community-based interventions for childhood asthma using comprehensive approaches: a systematic review and meta-analysis. Allergy Asthma Clin Immunol 2021;17. 10.1186/S13223-021-00522-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Bergmann KR, Nickel A, Hall M, Cutler G, Abuzzahab MJ, Bretscher B, et al. Association of Neighborhood Resources and Race and Ethnicity With Readmissions for Diabetic Ketoacidosis at US Children’s Hospitals. JAMA Netw Open 2022;5:e2210456–e2210456. 10.1001/JAMANETWORKOPEN.2022.10456. [DOI] [PMC free article] [PubMed] [Google Scholar]