Abstract
Spontaneous pneumothorax is a common presentation, and there has been a recent surge of research into the condition. With the recent publication of the new British Thoracic Society guidelines and the upcoming European Respiratory Society guidelines, we provide a concise up-to-date summary of clinical learning points. In particular we focus on the role of conservative or ambulatory management, as well as treatment options for persistent air leak and guidance for when to refer to thoracic surgeons for the prevention of the recurrence of pneumothorax.
Educational aims
To give up-to-date guidance on the acute management of spontaneous pneumothorax, including the role of conservative or ambulatory management
To discuss the different treatment options for persistent air leak.
To guide physicians on when to refer patients to thoracic surgeons for the prevention of the recurrence of pneumothorax.
Tweetable abstract
This educational review gives up-to-date guidance on the acute management of spontaneous pneumothorax, including the role of conservative or ambulatory management. It also discusses persistent air leak and the role of surgery for recurrence prevention. https://bit.ly/3M0njaT
Introduction
Spontaneous pneumothorax is a common clinical presentation, with 14.1 admissions per year per 100 000 population aged ≥15 years [1]. The management of pneumothorax has been debated for decades, with some advocating conservative management [2] and others championing a more interventional approach [3]. With the advent of readily available Seldinger devices providing bespoke catheters for pleural procedures, research and therefore guidelines have since favoured intervention, with either needle aspiration or intercostal drain (ICD) insertion [4]. However, recent research has brought the debate surrounding conservative management back to the fore. In addition, there remain questions over the optimum management of persistent air leak (PAL) and pneumothorax recurrence prevention. This article reviews current guidelines and the emerging evidence, which is changing practice.
Definition of pneumothoraces
A pneumothorax occurs when air accumulates between the visceral and parietal pleura, and can be defined as spontaneous, iatrogenic or traumatic [4]. This review focuses on spontaneous pneumothoraces. These are further classified as primary or secondary, depending on whether the patient has normal underlying lung parenchyma. Primary spontaneous pneumothoraces (PSPs) occur in the absence of underlying lung disease, and make up ∼40% of spontaneous pneumothoraces [1]. They are more common in men and in younger patients [1], and are associated with smoking [5]. Although generally believed to occur in patients with normal lungs, there is convincing evidence that there are underlying subpleural abnormalities within the lungs of people who develop PSPs [6].
Secondary spontaneous pneumothoraces (SSPs) occur in the presence of underlying lung disease, most commonly COPD [7]. The definition of SSP also typically includes older smokers (patients aged >50 years with a significant smoking history), as a subgroup analysis of a case series showed that patients with either one of these characteristics had a poor response to needle aspiration [8]. The distinction between PSP and SSP is based on data demonstrating a difference in outcomes to treatment, duration of air leak and suitability for surgical resection. However, spontaneous pneumothorax exists as a spectrum, and better phenotyping of patients remains an important research goal.
There are five main treatment approaches for the management of spontaneous pneumothorax:
1) Conservative approach, with a period of monitoring.
2) Ambulatory device such as a flutter valve.
3) Needle aspiration using a small-bore cannula or aspiration kit.
4) ICD attached to a drainage system.
5) Surgery for either acute or preventative treatment.
The most appropriate course of action will depend on numerous factors, including the patient's background and current clinical condition, the size of pneumothorax and its amenability to intervention, and patient preference.
Initial management of primary spontaneous pneumothorax
Learning points 1
PSP may not need immediate intervention.
Asymptomatic or minimally symptomatic patients may be managed conservatively, taking into account patient preference and local services.
If intervention is required, needle aspiration or placement of ICD should be considered.
In selected patients, ambulatory devices may be used if local services are in place to facilitate this.
There have been significant advances in evidence for the management of PSP over the past decade, which is reflected in the recently published British Thoracic Society (BTS) guideline for pleural disease [9]. The previous BTS guidelines, published in 2010 [4], based their guidance on the size of the pneumothorax at the level of the hilum on a plain posteroanterior radiograph. The guidance specified that patients with PSP <2 cm could generally be managed conservatively, but greater than this would prompt consideration of intervention. Additionally, these guidelines discussed high-risk characteristics (figure 1) that would have led to the insertion of an ICD. However, this guidance has now changed, as discussed later.
FIGURE 1.

High-risk characteristics for spontaneous pneumothorax.
Since these guidelines were published, more recent evidence has shown that conservative management is safe and effective in minimally symptomatic PSP, and studies have explored the use of novel technologies such as pleural vents. In a recent randomised controlled trial (RCT), Brown et al. [10] demonstrated that 94% of patients with large but minimally symptomatic PSPs treated conservatively had complete re-expansion within 8 weeks, which was statistically noninferior to the 98% in patients managed with an ICD. In addition, they found that there were significantly lower rates of recurrence in patients managed conservatively, with 12-month recurrence of 8.8% in the conservative arm compared to 16.8% if patients had ICD placement [10]. Additionally, 85% of patients managed conservatively did not require further pleural intervention. While these data are encouraging, there are reasons why this approach hasn't been universally adopted [11]. These include questions about the choice of a radiological primary outcome, the comparator arm (ICD insertion) not truly representing standard care and the generalisability of its findings [12]. For example, the study had a relatively high screen failure rate (∼90%) and the patients had lower symptom scores compared to other PSP studies. The currently recruiting Conservative versus Standard Care for Primary Spontaneous Pneumothorax (CONSEPT) study will compare conservative to standard care for patients with large symptomatic PSPs in United Kingdom (UK) hospitals (www.isrctn.com identifier ISRCTN75384510).
If intervention is required for a patient, the initial interventions available have either been needle aspiration or placement of an ICD. Evidence suggests that patients with a PSP undergoing needle aspiration have a shorter length of stay and fewer complications, although the rates of immediate success are lower [13]. While needle aspiration is better tolerated than ICD [14], 40% will require further pleural intervention due to needle aspiration failure [15], and 50% may still need admitting to hospital [16]. If needle aspiration is successful, patients should be followed-up in 2–4 weeks, although the exact length and any more immediate follow-up will be guided by local protocols. However, emerging evidence around the role of ambulatory devices means that a different intervention could be considered. These devices can be a one-way valve that attaches to the end of an ICD in place of the tubing to the underwater seal or a self-contained device (e.g. Rocket Pleural Vent; Rocket Medical, Watford, UK) [17–19]. The recent multicentre Randomised Ambulatory Management of Primary Pneumothorax (RAMPP) trial examined the use of self-contained devices for the management of PSP [19]. In the ambulatory arm, both initial hospitalisation and the overall length of hospitalisation (including re-admission times) were significantly lower. However, there were significantly more adverse effects, defined as requiring re-hospitalisation, in this arm. Additionally, they found that the length of time until treatment was complete (removal of the device or ICD) was significantly longer in ambulatory management, which may have been due to lack of clinician confidence in removing the device due to less frequent reviews as an outpatient compared to inpatient, as well as a lack of familiarity with the device [19]. Similar results were found in a Canadian study, and notably, neither study found a difference in total time off work [20].
Figure 2 shows the outcomes for the different management options for PSP [10, 13, 16, 19, 21, 22].
FIGURE 2.
Management options for primary spontaneous pneumothorax.
The results of these studies have led to a shift in priorities for physicians when treating a PSP from size-based criteria to greater focus on patient preference and symptoms. The recently published BTS guidance reflects this [9], as will the upcoming European Respiratory Society (ERS) guidance. The first question in any spontaneous pneumothorax is whether there are signs of physiological compromise, such as hypotension or severe hypoxia. In such cases an ICD should be inserted (after needle decompression in extreme circumstances). Further treatment decisions should focus on degree of symptoms and each patients’ preferences.
In patients for whom immediate intervention is not required, the management options largely depend on the patient's priorities and local services available. For patients with limited symptoms who are keen to avoid intervention, or those with a pneumothorax that is not sufficiently large enough to intervene, conservative management may be the most appropriate strategy. For others, relief of symptoms or more rapid resolution of the pneumothorax may be their priority, and therefore they may prefer management with needle aspiration or an ambulatory device, depending on size of pneumothorax, provision of local services to provide appropriate follow-up and the availability of clinicians familiar with ambulatory devices and trained in their insertion [9]. It is also important to consider specific factors that may be influencing a patient. For example, a patient may need to take a flight in the near future. The current advice is that you should not fly until 7 days after resolution on a chest radiograph [23], and so clearly a conservative approach may not be appropriate. Figure 3 gives a schema for how to incorporate patient wishes when considering the management of PSP.
FIGURE 3.
Management of primary spontaneous pneumothorax incorporating patient preferences.
In conclusion, the management of patients presenting with PSP is a rapidly developing area, and hospitals will need to assess whether they are able to provide the less invasive approaches that are becoming available.
Initial management of secondary spontaneous pneumothorax
Learning points 2
Patients with SSP generally require intervention, as they are at higher risk of deterioration.
ICD insertion remains the first-line treatment if it is safe to intervene.
Needle aspiration or conservative management can be considered on a case-by-case basis.
In contrast to the management of PSP, the mainstay of managing SSP is with the insertion of an ICD, as long as the pneumothorax is large enough to intervene [4], largely because patients with underlying lung disease are more likely to be symptomatic and hypoxic, presumed secondary to reduced physiological reserve to withstand pneumothoraces, and are at higher risk of prolonged air leak, thought to be due to the presence of larger visceral pleural defects [24].
Needle aspiration is not routinely used in SSP, due to lack of high-quality evidence, together with concerns about efficacy of needle aspiration based on two small (n<15) case series reports [8, 25]. This has been challenged by the findings of a recent randomised study which recruited 48 SSP patients as part of a larger cohort of patients, which also included 79 patients with PSP [21]. In the SSP subgroup, median (interquartile range) length of hospital stay in the needle aspiration arm was 2.5 (1.2–7.8) days versus 5.5 (3.6–9.2) days in the chest drain arm (p=0.049). Needle aspiration was also associated with higher rates of immediate success in the SSP subgroup: 59% for needle aspiration compared to 23% in chest drain group (p=0.011). Importantly, complication rates across all patients were much higher in the chest drain arm than needle aspiration (15 serious complications versus none). Needle aspiration versus chest drain is now being studied in a full UK RCT (PRINCE study; www.isrctn.com identifier: ISRCTN12644940).
Several studies have explored the role of conservative and ambulatory management in SSP. A retrospective analysis of a case series of 82 patients presenting with SSP to a single centre in Australia over a 7-year period found that patients managed conservatively had a shorter length of stay [26] and that none required further pleural intervention. However, due to the retrospective design and lack of randomisation, there was inevitable selection bias, as patients managed conservatively had smaller pneumothoraces than those who received an intervention. There was incomplete documentation about time to re-expansion.
An RCT published in 2021 investigating the role of ambulatory devices as the initial management of SSP found that this was not an optimum approach [27]. Patients were randomised to standardised care with an ICD and an underwater seal, or ambulatory management with either a self-contained device (i.e. Rocket Pleural Vent) or a flutter valve attached to an ICD, if an ICD was already in place. Overall, there was no difference in length of hospital stay, but a higher rate of treatment failure was observed in the ambulatory care group managed with the ambulatory device, postulated to be secondary to a larger air leak than could be managed with the narrower gauge Rocket Pleural Vent. The higher treatment failure rate was not observed in patients with a standard ICD and flutter valve, suggesting that this may be a safer ambulatory approach, but the study was not powered to show this.
In summary, patients presenting with SSP should have an ICD inserted provided it is safe to proceed. There may be some select cases where needle aspiration or conservative management is suitable (for example if the pneumothorax is too small to intervene and the patient is asymptomatic), but these patients would require a period of close observation as an inpatient. An ambulatory approach should typically be avoided in the initial management of patients with SSP.
Management of persistent air leak
Learning points 3
Management conundrum, with numerous interventions available, but limited concrete evidence to support one over another.
Interventions should be decided on a case-by-case basis depending on local experience.
Surgical referral should be considered early in a patient's admission (i.e. after 48 h).
Despite the recent surge in pneumothorax research, there remain ongoing questions regarding the best management for patients with PAL. These are patients with pneumothorax with ongoing air leak after initial management, occurring both post-surgically and in spontaneous pneumothorax. Patients with spontaneous pneumothorax are often considered to have PAL 48 h after intervention [28]. While most PAL will settle spontaneously, with a mean duration of PSP and SSP of 5.19 and 9.9 days, respectively [24], this leads to long hospital stays, with its associated complications. The traditional underwater seal provides crude measurement by the rate of bubbles being produced, but more accurate measurement of the size of the air leak can be achieved by newer digital devices. Evidence from surgical patients suggests that these can reduce the length of hospital stay in patients presenting with post-surgical air leak, but there is currently limited evidence supporting their use in spontaneous pneumothorax [29, 30].
Guidelines for both PSP and SSP suggest early discussion with thoracic surgeons for intervention via video-assisted thoracic surgery (VATS) [4] as early as 48 h into their admission, especially if they have respiratory compromise. However, many patients presenting with SSP are not fit enough for surgery. These patients present a conundrum, as the various management options available have a limited evidence base. Much of the evidence has been extrapolated from studies of PAL following thoracic surgery rather than in spontaneous pneumothorax [31]. We discuss each management strategy briefly, but their use should be dependent on local experience and availability.
One of the most widely used interventions is placing the ICD on suction at −10 to −20 cmH2O, which can be achieved with both standard underwater seals and digital devices. Its aim is to increase the speed of air removal from the pleural space and to appose the pleura, sealing the defect. However, there is very little evidence for whether this reduces the time to re-expansion or the requirement for surgery [32] and some have suggested that suction may perpetuate the air leak [33]. However, it is usually well tolerated and may be used for patients with PAL while considering other treatment options. A trial has recently opened in the UK investigating whether suction is safe and reduces treatment duration in PSP (RASPER; www.isrctn.com identifier ISRCTN18017504).
The intervention with perhaps the strongest evidence base in spontaneous pneumothorax is the use of an autologous blood patch (ABP), achieved by instilling a patient's own blood through the ICD [34]. It is postulated to work by both causing a pleurodesis reaction and forming a clot over the visceral defect. A study in 2012 showed that the weight-related dosing of a blood patch achieves up to 82% success after 13 days, compared to 9% with saline injection [35]. A more recent study showed that early use of an ABP reduces time to sealing from 10.5 days to 5.4 days [36]. Some clinicians are concerned that ABP may increase the risk of pleural infection. The first of the studies mentioned did not report any pleural infection, and the second study found 16.7% of patients with standard care developed empyema, possibly related to the duration of chest tube insertion, compared to 8.7% with early ABP. Therefore, this intervention should be considered in patients with PAL as long as local experience with the procedure is available. However, care should be taken, as these studies were done using large-bore chest drains; there remains concern that smaller bore chest drains may block, and further research is required to ensure the safety of this approach.
As with initial management of spontaneous pneumothorax, another possible approach to PAL is the use of ambulatory devices. The 2021 study mentioned earlier investigating the use of ambulatory devices in SSP found that the pleural vents had a higher complication rate than standard care. However, in patients treated with a large-bore chest drain and a Heimlich valve failure, complication rate was similar to standard care [27]. Therefore, this option may be possible in selected patients, and could be an option in PAL, although further investigation is required to establish safety and efficacy.
The final management option we will discuss is the insertion of endobronchial valves (EBVs). These are placed using flexible bronchoscopy, and can be in lobar, segmental or subsegmental bronchi, ensuring that air moves only out of the lung, and not back into it. Primarily these valves have been used in patients with emphysema as lung volume reduction therapy [37], but their use has also been investigated in PAL. In PAL, the location of the air leak first needs to be determined using endoscopic balloon occlusion, and the placement of an EBV aims to stop the air leak to allow the area of defective lung to heal.
In a prospective case series in the 2000s, 40 patients with PAL had an EBV inserted; 20 of these patients had initially presented with spontaneous pneumothorax. The authors found that 47.5% of patients had resolution of the pneumothorax, with a median time of 21 days from EBV insertion to ICD removal, but had no control arm for comparison [38]. In a retrospective case series of patients with PAL following spontaneous pneumothorax, 37 patients were identified who had either refused or been deemed unsuitable for surgery and were subsequently offered EBV insertion [39]. Of these, 46% were unable to have the EBV as the location of the air leak could not be identified, and only 40% (eight in total) of the remaining patients were successful in stopping the air leak. Conversely, a study in the United States reported that 80% of patients had successful resolution of their PAL following EBV insertion, although the average length of time between ICD insertion and EBV insertion was 10 days, by which time the majority of PAL will have resolved spontaneously [40]. Alternative endobronchial interventions have been trialled, such as an endobronchial silicon spigot occlusion device, which showed 84% resolution at 14 days compared to 60% for ICD alone [41]. Given the lack of large randomised trials, there is ongoing concern that referring for EBV delays definitive surgical intervention, and identifying which patients are suitable is difficult to determine. It is only currently available in specialist centres, whereas other treatment strategies for PAL can be carried out locally.
In summary, the management of PAL remains a difficult problem. Patients should be discussed with thoracic surgeons early in their admission, especially if they present with any significant compromise. Those patients for whom surgery is not possible require case-by-case discussion, with the potential for interventions such as ABP and EBV insertion. The use of suction remains controversial, and can be used with care, although more evidence regarding this should emerge over the coming years.
Prevention of recurrence
Learning points 4
Lifetime recurrence rate is ∼30% in PSP.
Chronic lung disease and female sex are significant predictors of recurrence.
VATS can be offered to patients in whom recurrence prevention is a priority, after informed discussion.
Smoking cessation should be encouraged in all patients with spontaneous pneumothorax.
A patient who has had one spontaneous pneumothorax is at risk of developing further pneumothoraces, and questions remain on the optimum management to reduce recurrence, as well as patient selection. It is estimated that ∼30% of patients with PSP will develop a further pneumothorax [42]. The highest rate is within the first year (18.8% in males and 19.5% in females) and younger patients have a higher risk of recurrence [1]. In general, females with PSP demonstrate higher recurrence rates, which may be explained by the presence of gender-specific diseases such as lymphangioleiomyomatosis and catamenial pneumothoraces [42]. However, the group with the highest incidence of recurrence is male patients aged 15–34 years with chronic lung disease, and chronic lung disease in general significantly increases risk of recurrence [1]. Other factors that may predispose patients to recurrence are low body mass index and radiological evidence of a combination of blebs and bullae.
Smoking is a significant risk factor for developing a pneumothorax [5], although the evidence base for its contribution to recurrence is less clear. However, there is evidence that the cessation of smoking reduces the rate of recurrence of PSP from 70% to 40% [43]. In addition, smoking cannabis has been associated with developing pneumothorax [44]. Patients should be encouraged to stop smoking tobacco and other illicit substances to reduce their recurrence rate.
Within the acute phase of treatment, there is evidence that using chemical pleurodesis with sterile talc can reduce recurrence rates [45]. A meta-analysis completed by the BTS concluded that 179 per 1000 patients will have a recurrence after pleurodesis compared to 320 per 1000 with chest drainage only, and this has been reflected in the recent BTS guidance [9]. However, pleurodesis is less effective than surgery, so should be reserved for those who are not suitable for or decline surgery [22].
Once a patient's pneumothorax has resolved, physicians must decide whether they should be referred for surgery to reduce the risk of recurrence. The ERS task force statement [46] and the BTS guidelines [9] suggest that patients should be referred if they present with their first contralateral pneumothorax, second ipsilateral pneumothorax or synchronous bilateral pneumothoraces or work in at-risk professions, such as pilots and scuba divers [47]. The surgical options available for patients with pneumothorax are generally achieved via VATS, and usually involve removal of blebs via a wedge resection with or without other procedures such as pleurectomy or chemical pleurodesis [48]. The merits of the different approaches are beyond the scope of this review.
Some clinicians advocate a more interventional approach to reduce recurrence risk with early surgical intervention at first presentation with spontaneous pneumothorax. An RCT of 181 patients presenting with PSP demonstrated recurrence in 13% treated with an early VATS procedure compared to 34% of patients with chest tube treatment [49]. This difference was significant when patients had bullae of >1 cm on high-resolution computed tomography, with highest benefit occurring for patients with bullae >2 cm. However, this study was limited by lack of patient-reported outcome measures such as pain score. Additionally, with a number needed to treat of 4.8, first-line surgery subjects many patients to unnecessary surgery to prevent a minority of recurrences [50].
Patient preference should play a significant role in decision making after they have been fully informed of the risks and benefits. This includes discussing their profession or high-risk activities. As mentioned previously, patients cannot fly until 7 days after complete radiological resolution, and so a pilot may want surgery to reduce their risk of recurrence and therefore risk of taking more time off work. Similarly, patients should not scuba dive at all following a spontaneous pneumothorax [47], but they can do so after bilateral pleurectomy with normal computed tomography and lung function after surgery [51], and therefore patients wishing to undergo these high-risk activities should be referred for surgery.
In summary, all patients presenting with a spontaneous pneumothorax should be followed-up by a respiratory physician to discuss ongoing disease recurrence. The simplest intervention is to counsel smoking cessation, but referral for surgery will be necessary for many patients, especially if they are presenting with a recurrence of their pneumothorax.
Conclusion
Spontaneous pneumothoraces present a significant burden on hospitals, and how they are managed has changed over the past decade. Selected patients with PSP may now be safely managed with conservative or ambulatory care, reducing their length of hospital stay. Patients presenting with SSP still generally require insertion of an ICD at first presentation, except in select cases, due to their higher risk of deterioration. PAL remains difficult to manage, especially in patients who are unable to undergo surgery. Several techniques are being used, although none have shown definitively that they reduce the need to progress to surgery, length of hospital stay or mortality. Therefore, local experience and availability will drive which methods are used. Following presentation with spontaneous pneumothorax, patients require follow up to discuss recurrence prevention, with young patients and patients with chronic lung disease most likely to have recurrence. For both PAL and recurrence, surgery plays a large role in treatment.
Self-evaluation questions
-
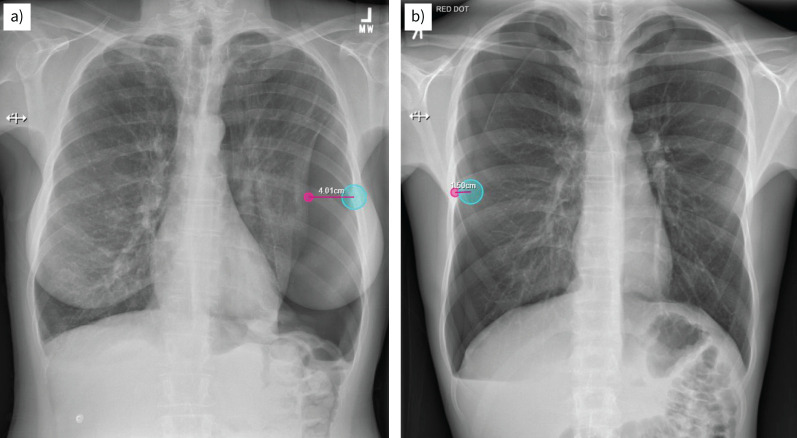
A 54-year-old woman with a background of COPD presents with sudden-onset left-sided chest pain and breathlessness. She was treated the previous week for an exacerbation of her COPD with antibiotics and steroids. Her oxygen saturations are 91% on 1 L oxygen via nasal specs, systolic blood pressure is 130 mmHg, heart rate is 85 beats per min and she is afebrile. Her chest radiograph is shown in figure 4a.
What is the most appropriate initial management in this patient's case?- Admit for observation and repeat chest radiography in 12 h.
- Immediate needle decompression in 2nd intercostal space, midclavicular line.
- Insert small-bore (8–14 Fr) Seldinger chest drain in 4th intercostal space, midaxillary line, attach to underwater seal and admit.
- Insert large-bore (16–20 Fr) Seldinger chest drain in 4th intercostal space, midaxillary line, attach to underwater seal and admit.
- Needle aspiration of up to 2.5 L and repeat chest radiography post-procedure. If stable in appearance, discharge home with outpatient follow-up.
-
A 17-year-old male presents to the emergency department with a <24-h history of right-sided chest pain. He has no past medical history or family history, but does smoke five cigarettes per day. His oxygen saturations are 99% on room air, systolic blood pressure is 115 mmHg, heart rate is 64 beats per min and he is afebrile. He is able to mobilise around the department without significant breathlessness and feels his pain is manageable. Chest radiography shows a right-sided pneumothorax measuring 1.5 cm at the hilum (figure 4b).
What is the most appropriate management initial in this patient's case?- Admit, give high-flow oxygen and observe for 24 h.
- Admit, insert small-bore (8–14 Fr) Seldinger chest drain.
- Consider discharge with no intervention and follow-up in the outpatient clinic in 2–4 weeks.
- Insert pleural vent and review in clinic in 1 week.
- Needle aspiration of up to 2.5 L and repeat chest radiography.
-
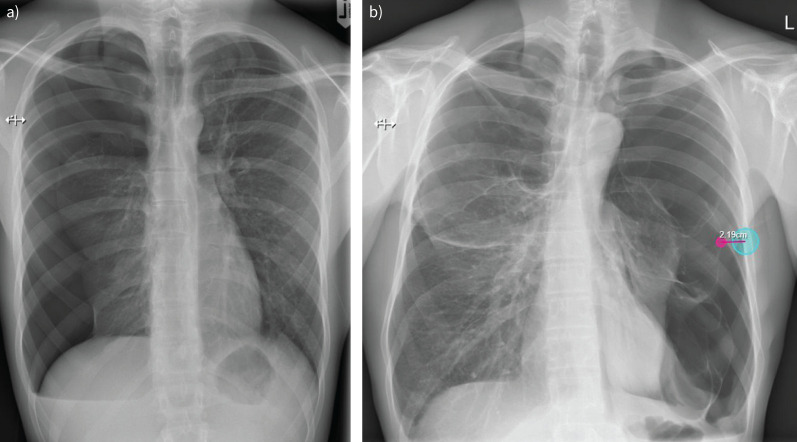
A 19-year-old male presents with sudden-onset right-sided chest tightness and pain. His observations are stable; he is not breathless; and the pain is manageable with simple analgaesia. Chest radiography shows a right-sided pneumothorax measuring 3.3 cm at the hilum (figure 5a). You discuss management options with him, including needle aspiration, ambulatory management with a pleural vent and conservative management. He is keen to avoid admission to hospital, but is due to fly to Spain in 3 months’ time.
What is the most appropriate advice to give him regarding management of his pneumothorax?- 30% of conservatively managed pneumothoraces will require further intervention prior to resolution.
- He will be safe to fly in 7 days’ time.
- Length of hospital stay is similar whether he has a needle aspiration or a pleural vent.
- Needle aspiration is successful in 75% of pneumothoraces and no further intervention is required.
- With conservative management, 94% of primary spontaneous pneumothoraces will resolve within 8 weeks and recurrence rates are lower.
-
A 47-year-old man with no past medical history presented with left-sided back pain and dyspnoea. He used to smoke heroin and continues to smoke cannabis regularly. He is haemodynamically stable with normal oxygen saturations. His chest radiography is shown in figure 5b.
What is the most appropriate initial management in this patient's case?- Admit for observation and repeat chest radiography in 12 h.
- Consider discharge without intervention and follow-up in clinic in 2–4 weeks.
- Immediate needle decompression in 2nd intercostal space, midclavicular line.
- Insert small-bore (8–14 Fr) Seldinger chest drain in 4th intercostal space, midaxillary line, attach to underwater seal and admit.
- Needle aspiration of up to 2.5 L and repeat chest radiography post-procedure. If stable in appearance, discharge home with outpatient follow-up.
FIGURE 4.
a) Chest radiograph for self-evaluation question 1. b) Chest radiograph for self-evaluation question 2.
FIGURE 5.
a) Chest radiograph for self-evaluation question 3. b) Chest radiograph for self-evaluation question 4.
FIGURE 4.
a) Chest radiograph for self-evaluation question 1. b) Chest radiograph for self-evaluation question 2.
FIGURE 5.
a) Chest radiograph for self-evaluation question 3. b) Chest radiograph for self-evaluation question 4.
Suggested answers
c. This woman is aged >50 years with an underlying diagnosis of COPD. She is therefore at high risk of deterioration and requires intervention rather than conservative management (a). There is no evidence of haemodynamic instability to suggest tension pneumothorax, so immediate needle decompression is not warranted (b). A needle aspiration would be inappropriate in the context of her underlying lung disease, breathlessness and hypoxia (e). There is no evidence to support the use of wider bore chest drains in patients with SSP (d), so insertion of a 8–14 Fr Seldinger chest drain (c) is the most appropriate answer.
c. This patient has a primary spontaneous pneumothorax and is clinically well. His low symptom burden and stable observations make him an excellent candidate for conservative management (c). A pleural vent (d) or needle aspiration (e) would also be appropriate if the patient had a desire for rapid resolution of his symptoms, but his symptoms do not warrant this. Intercostal chest drain insertion (b) is reserved for those who have failed more conservative options. There is limited evidence to suggest benefit from giving high-flow oxygen and this patient does not need to be admitted to hospital (a).
e. In Brown et al.’s [10] study published in 2020, 94% of conservatively managed patients showed full radiographic resolution at 8 weeks (e), but only 15% of those managed conservatively went on to require further intervention (a). The current BTS guidelines advise that patients who have had a pneumothorax are considered safe to fly 7 days post-radiographic resolution of their pneumothorax, so this patient needs further radiography in due course to ensure that his pneumothorax has resolved before clinicians can decide whether he is fit to fly (b). Evidence suggests that 40–50% of those who undergo needle aspiration require a further procedure to resolve their pneumothorax (d). The RAMPP study showed that patients managed with an ambulatory device had a shorter length of stay than those managed with standard care (c). (e) is therefore the most accurate statement.
d. Although this man is aged <50 years, he has a significant history of smoking both tobacco and illicit substances. His chest radiograph shows clear bullous disease bilaterally, worse on the left. Therefore, he should be managed as a secondary spontaneous pneumothorax; his pneumothorax is of sufficient size to intervene and he is breathless so he should have an 8–14 Fr ICD inserted (d). There is no evidence of tension, so needle decompression is not warranted (c). Needle aspiration is not currently advised for SSP (e), nor is conservative management appropriate as he is symptomatic (a/b).
Footnotes
Conflict of interest: The authors declare no conflicts of interest related to this manuscript.
References
- 1.Hallifax RJ, Goldacre R, Landray MJ, et al. . Trends in the incidence and recurrence of inpatient-treated spontaneous pneumothorax, 1968–2016. JAMA 2018; 320: 1471–1480. doi: 10.1001/jama.2018.14299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stradling P, Poole G. Conservative management of spontaneous pneumothorax. Thorax 1966; 21: 145–149. doi: 10.1136/thx.21.2.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruckley CV, McCormack RJ. The management of spontaneous pneumothorax. Thorax 1966; 21: 139–144. doi: 10.1136/thx.21.2.139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacDuff A, Arnold A, Harvey J. Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline 2010. Thorax 2010; 65: Suppl. 2, ii18–ii31. doi: 10.1136/thx.2010.136986 [DOI] [PubMed] [Google Scholar]
- 5.Bense L, Eklund G, Wiman LG. Smoking and the increased risk of contracting spontaneous pneumothorax. Chest 1987; 92: 1009–1012. doi: 10.1378/chest.92.6.1009 [DOI] [PubMed] [Google Scholar]
- 6.Grundy S, Bentley A, Tschopp J-M. Primary spontaneous pneumothorax: a diffuse disease of the pleura. Respiration 2012; 83: 185–189. doi: 10.1159/000335993 [DOI] [PubMed] [Google Scholar]
- 7.Guo Y, Xie C, Rodriguez RM, et al. . Factors related to recurrence of spontaneous pneumothorax. Respirology 2005; 10: 378–384. doi: 10.1111/j.1440-1843.2005.00715.x [DOI] [PubMed] [Google Scholar]
- 8.Ng AW, Chan KW, Lee SK. Simple aspiration of pneumothorax. Singapore Med J 1994; 35: 50–52. [PubMed] [Google Scholar]
- 9.Roberts M, Rahman NM, Maskell NA, et al. . British Thoracic Society guideline for pleural disease. Thorax 2023; 78: s1–s42. 10.1136/thorax-2022-219784 [DOI] [PubMed] [Google Scholar]
- 10.Brown SGA, Ball EL, Perrin K, et al. . Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med 2020; 382: 405–415. doi: 10.1056/NEJMoa1910775 [DOI] [PubMed] [Google Scholar]
- 11.Hallifax RJ, Roberts M, Russell N, et al. . Pneumothorax management: current state of practice in the UK. Respir Res 2022; 23: 23. doi: 10.1186/s12931-022-01943-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hallifax RJ, Walker S, Walters J, et al. . Management of primary spontaneous pneumothorax: less is more – authors’ reply. Lancet 2020; 396: 1973–1974. doi: 10.1016/S0140-6736(20)32676-3 [DOI] [PubMed] [Google Scholar]
- 13.Carson-Chahhoud KV, Wakai A, van Agteren JE, et al. . Simple aspiration versus intercostal tube drainage for primary spontaneous pneumothorax in adults. Cochrane Database Syst Rev 2017; 9: CD004479. doi: 10.1002/14651858.CD004479.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marx T, Joly L-M, Parmentier A-L, et al. . Simple aspiration versus drainage for complete pneumothorax: a randomized noninferiority trial. Am J Respir Crit Care Med 2023; 207: 1475–1485. doi: 10.1164/rccm.202110-2409OC [DOI] [PubMed] [Google Scholar]
- 15.Harvey J, Prescott RJ. Simple aspiration versus intercostal tube drainage for spontaneous pneumothorax in patients with normal lungs. British Thoracic Society Research Committee. BMJ 1994; 309: 1338–1339. doi: 10.1136/bmj.309.6965.1338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Noppen M, Alexander P, Driesen P, et al. . Manual aspiration versus chest tube drainage in first episodes of primary spontaneous pneumothorax: a multicenter, prospective, randomized pilot study. Am J Respir Crit Care Med 2002; 165: 1240–1244. doi: 10.1164/rccm.200111-078OC [DOI] [PubMed] [Google Scholar]
- 17.Brims FJH, Maskell NA. Ambulatory treatment in the management of pneumothorax: a systematic review of the literature. Thorax 2013; 68: 664–669. doi: 10.1136/thoraxjnl-2012-202875 [DOI] [PubMed] [Google Scholar]
- 18.Aujayeb A. Ambulatory pneumothorax management with 8FG Rocket® Pleural VentTM. Eur Respir J 2019; 54: Suppl. 63, PA3127. doi: 10.1183/13993003.congress-2019.PA3127 [DOI] [Google Scholar]
- 19.Hallifax RJ, McKeown E, Sivakumar P, et al. . Ambulatory management of primary spontaneous pneumothorax: an open-label, randomised controlled trial. Lancet 2020; 396: 39–49. doi: 10.1016/S0140-6736(20)31043-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marcotte A, de Champlain F. Is ambulatory management of primary spontaneous pneumothorax safe and effective? CJEM 2021; 23: 750–751. doi: 10.1007/s43678-021-00183-y [DOI] [PubMed] [Google Scholar]
- 21.Thelle A, Gjerdevik M, SueChu M, et al. . Randomised comparison of needle aspiration and chest tube drainage in spontaneous pneumothorax. Eur Respir J 2017; 49: 1601296. doi: 10.1183/13993003.01296-2016 [DOI] [PubMed] [Google Scholar]
- 22.Ayed AK, Chandrasekaran C, Sukumar M. Aspiration versus tube drainage in primary spontaneous pneumothorax: a randomised study. Eur Respir J 2006; 27: 477–482. doi: 10.1183/09031936.06.00091505 [DOI] [PubMed] [Google Scholar]
- 23.Coker RK, Armstrong A, Church AC, et al. . BTS clinical statement on air travel for passengers with respiratory disease. Thorax 2022; 77: 329–350. doi: 10.1136/thoraxjnl-2021-218110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chee CB, Abisheganaden J, Yeo JK, et al. . Persistent air-leak in spontaneous pneumothorax – clinical course and outcome. Respir Med 1998; 92: 757–761. doi: 10.1016/S0954-6111(98)90008-7 [DOI] [PubMed] [Google Scholar]
- 25.Archer GJ, Hamilton AA, Upadhyay R, et al. . Results of simple aspiration of pneumothoraces. Br J Dis Chest 1985; 79: 177–182. doi: 10.1016/0007-0971(85)90028-2 [DOI] [PubMed] [Google Scholar]
- 26.Gerhardy BC, Simpson G. Conservative versus invasive management of secondary spontaneous pneumothorax: a retrospective cohort study. Acute Med Surg 2021; 8: e663. doi: 10.1002/ams2.663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walker SP, Keenan E, Bintcliffe O, et al. . Ambulatory management of secondary spontaneous pneumothorax: a randomised controlled trial. Eur Respir J 2021; 57: 2003375. doi: 10.1183/13993003.03375-2020 [DOI] [PubMed] [Google Scholar]
- 28.Lazarus DR, Casal RF. Persistent air leaks: a review with an emphasis on bronchoscopic management. J Thorac Dis 2017; 9: 4660–4670. doi: 10.21037/jtd.2017.10.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ruigrok D, Kunst PWA, Blacha MMJ, et al. . Digital versus analogue chest drainage system in patients with primary spontaneous pneumothorax: a randomized controlled trial. BMC Pulm Med 2020; 20: 136. doi: 10.1186/s12890-020-1173-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Evans JM, Ray A, Dimmock P. Thopaz+ portable digital system for managing chest drains: a NICE Medical Technologies Guidance. Appl Health Econ Health Policy 2019; 17: 285–294. doi: 10.1007/s40258-019-00461-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dugan KC, Laxmanan B, Murgu S, et al. . Management of persistent air leaks. Chest 2017; 152: 417–423. doi: 10.1016/j.chest.2017.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Deng B, Tan Q-Y, Zhao Y-P, et al. . Suction or non-suction to the underwater seal drains following pulmonary operation: meta-analysis of randomised controlled trials. Eur J Cardiothorac Surg 2010; 38: 210–215. doi: 10.1016/j.ejcts.2010.01.050 [DOI] [PubMed] [Google Scholar]
- 33.Walker SP, Hallifax R, Rahman NM, et al. . Challenging the paradigm of persistent air leak: are we prolonging the problem? Am J Respir Crit Care Med 2022; 206: 145–149. doi: 10.1164/rccm.202109-2149PP [DOI] [PubMed] [Google Scholar]
- 34.Pathak V, Quinn C, Zhou C, et al. . Use of autologous blood patch for prolonged air leak in spontaneous pneumothoraces in the adolescent population. Lung India 2018; 35: 328–331. doi: 10.4103/lungindia.lungindia_462_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cao GQ, Kang J, Wang F, et al. . Intrapleural instillation of autologous blood for persistent air leak in spontaneous pneumothorax in patients with advanced chronic obstructive pulmonary disease. Ann Thorac Surg 2012; 93: 1652–1657. doi: 10.1016/j.athoracsur.2012.01.093 [DOI] [PubMed] [Google Scholar]
- 36.Ibrahim IM, Elaziz MEA, El-Hag-Aly MA. Early autologous blood-patch pleurodesis versus conservative management for treatment of secondary spontaneous pneumothorax. Thorac Cardiovasc Surg 2019; 67: 222–226. doi: 10.1055/s-0038-1642028 [DOI] [PubMed] [Google Scholar]
- 37.Kemp SV, Slebos D-J, Kirk A, et al. . A multicenter randomized controlled trial of zephyr endobronchial valve treatment in heterogeneous emphysema (TRANSFORM). Am J Respir Crit Care Med 2017; 196: 1535–1543. doi: 10.1164/rccm.201707-1327OC [DOI] [PubMed] [Google Scholar]
- 38.Travaline JM, McKenna RJ, De Giacomo T, et al. . Treatment of persistent pulmonary air leaks using endobronchial valves. Chest 2009; 136: 355–360. doi: 10.1378/chest.08-2389 [DOI] [PubMed] [Google Scholar]
- 39.Yu WC, Yu EL, Kwok HC, et al. . Endobronchial valve for treatment of persistent air leak complicating spontaneous pneumothorax. Hong Kong Med J 2018; 24: 158–165. [DOI] [PubMed] [Google Scholar]
- 40.Bermea RS, Miller J, Wilson WW, et al. . One-way endobronchial valves as management for persistent air leaks: a preview of what's to come? Am J Respir Crit Care Med 2019; 200: 1318–1320. doi: 10.1164/rccm.201904-0761LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang H-T, Xie Y-H, Gu X, et al. . Management of persistent air leaks using endobronchial autologous blood patch and spigot occlusion: a multicentre randomized controlled trial in China. Respiration 2019; 97: 436–443. doi: 10.1159/000495298 [DOI] [PubMed] [Google Scholar]
- 42.Walker SP, Bibby AC, Halford P, et al. . Recurrence rates in primary spontaneous pneumothorax: a systematic review and meta-analysis. Eur Respir J 2018; 52: 1800864. doi: 10.1183/13993003.00864-2018 [DOI] [PubMed] [Google Scholar]
- 43.Sadikot RT, Greene T, Meadows K, et al. . Recurrence of primary spontaneous pneumothorax. Thorax 1997; 52: 805–809. doi: 10.1136/thx.52.9.805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Feldman AL, Sullivan JT, Passero MA, et al. . Pneumothorax in polysubstance-abusing marijuana and tobacco smokers: three cases. J Subst Abuse 1993; 5: 183–186. doi: 10.1016/0899-3289(93)90061-F [DOI] [PubMed] [Google Scholar]
- 45.Hallifax RJ, Yousuf A, Jones HE, et al. . Effectiveness of chemical pleurodesis in spontaneous pneumothorax recurrence prevention: a systematic review. Thorax 2017; 72: 1121–1131. doi: 10.1136/thoraxjnl-2015-207967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tschopp JM, Bintcliffe O, Astoul P, et al. ERS task force statement: diagnosis and treatment of primary spontaneous pneumothorax. Eur Respir J 2015; 46: 321–335. 10.1183/09031936.00219214 [DOI] [PubMed] [Google Scholar]
- 47.Villela MA, Dunworth S, Harlan NP, et al. . Can my patient dive after a first episode of primary spontaneous pneumothorax? A systematic review of the literature. Undersea Hyperb Med 2018; 45: 199–208. doi: 10.22462/03.04.2018.7 [DOI] [PubMed] [Google Scholar]
- 48.Sudduth CL, Shinnick JK, Geng Z, et al. . Optimal surgical technique in spontaneous pneumothorax: a systematic review and meta-analysis. J Surg Res 2017; 210: 32–46. doi: 10.1016/j.jss.2016.10.024 [DOI] [PubMed] [Google Scholar]
- 49.Olesen WH, Katballe N, Sindby JE, et al. . Surgical treatment versus conventional chest tube drainage in primary spontaneous pneumothorax: a randomized controlled trial. Eur J Cardiothorac Surg 2018; 54: 113–121. doi: 10.1093/ejcts/ezy003 [DOI] [PubMed] [Google Scholar]
- 50.Cardillo G, Ricciardi S, Rahman N, et al. . Primary spontaneous pneumothorax: time for surgery at first episode? J Thorac Dis 2019; 11: S1393–S1397. doi: 10.21037/jtd.2019.03.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Godden D. British Thoracic Society guidelines on respiratory aspects of fitness for diving. Thorax 2003; 58: 3–13. doi: 10.1136/thorax.58.1.3 [DOI] [PMC free article] [PubMed] [Google Scholar]