Abstract
Pleural infection remains a medical challenge. Although closed tube drainage revolutionised treatment in the 19th century, pleural infection still poses a significant health burden with increasing incidence. Diagnosis presents challenges due to non-specific clinical presenting features. Imaging techniques such as chest radiographs, thoracic ultrasound and computed tomography scans aid diagnosis. Pleural fluid analysis, the gold standard, involves assessing gross appearance, biochemical markers and microbiology. Novel biomarkers such as suPAR (soluble urokinase plasminogen activator receptor) and PAI-1 (plasminogen activator inhibitor-1) show promise in diagnosis and prognosis, and microbiology demonstrates complex microbial diversity and is associated with outcomes. The management of pleural infection involves antibiotic therapy, chest drain insertion, intrapleural fibrinolytic therapy and surgery. Antibiotic therapy relies on empirical broad-spectrum antibiotics based on local policies, infection setting and resistance patterns. Chest drain insertion is the mainstay of management, and use of intrapleural fibrinolytics facilitates effective drainage. Surgical interventions such as video-assisted thoracoscopic surgery and decortication are considered in cases not responding to medical therapy. Risk stratification tools such as the RAPID (renal, age, purulence, infection source and dietary factors) score may help guide tailored management. The roles of other modalities such as local anaesthetic medical thoracoscopy and intrapleural antibiotics are debated. Ongoing research aims to improve outcomes by matching interventions with risk profile and to better understand the development of disease.
Tweetable abstract
Pleural fluid analysis is the gold standard for pleural infection diagnosis. Current management is by antibiotic therapy, therapeutic pleural aspirations, chest drains, IPFT and surgery; the future includes targeted treatment by RAPID risk categorisation. https://bit.ly/49PtBEH
Introduction
Pleural infection, which is defined as bacterial entry and replication in the pleural space [1], is a common medical condition that was described nearly 5000 years ago by the ancient Egyptians [2]. Historically, the recommended treatment was open thoracic drainage, which was associated with a very high mortality of approximately 70% [3]. This dramatically improved with the introduction of closed tube drainage in the 19th century, which remains the main principle of management to this day [3]. However, despite recent advances in our understanding of the aetiopathogenesis and management of pleural infection, this condition continues to be associated with poor outcomes.
Approximately 20–57% of patients with pneumonia have an associated pleural effusion at presentation, of which 5–7% progress to pleural infection [4, 5]. Terms such as “simple” and “complicated” parapneumonic effusion are used to describe the stages of evolution of pneumonia to pleural infection, but these suggest that pleural infection is always a consequence of complications arising from an associated pneumonia. We now know that about 30% of cases of pleural infection have no associated pneumonic illness on radiological assessment [6]. The term “empyema” denotes the presence of purulent fluid in the pleural space and represents one end of the spectrum of pleural infection [7]. Therefore, “pleural infection” is an all-encompassing term that is preferred in modern literature and includes both complicated parapneumonic effusion and empyema.
Pleural infection has a combined incidence of over 80 000 cases per annum in the USA and UK, thereby causing a significant health burden [8]. Moreover, several recent studies have shown that the incidence of pleural infection is increasing across the Western World, but the cause for this, particularly in the elderly population, is unclear [9–11]. Worryingly, clinical outcomes remain poor, with a 30-day mortality of 10% [12] and 12-month mortality as high as 32% after an episode of pleural infection [6]. It is important to note that the so-called “simple parapneumonic effusion” is also associated with a higher 30-day mortality and more prolonged hospital stay than pneumonia without effusion [13], and the reasons for this are unclear. The average length of hospital stay for pleural infection is 14 days [11], which contributes to the significant healthcare costs associated with this condition.
This review aims to provide an overview of the diagnosis and management of pleural infection with a focus on recent developments in these two areas. We have also attempted to highlight current knowledge gaps and possible future research directions in each section.
Diagnosis of pleural infection
Clinical presentation
Clinical presentation of pleural infection is non-specific and variable; therefore, early diagnosis can be challenging. Patients with pleural infection usually present in one of two ways. The classical presentation is that of a relatively young patient with few comorbidities, with fever, rigors, symptoms of an acute respiratory illness, and a non-resolving pneumonia with associated pleural effusion on chest radiography. In contrast, patients with several comorbidities, particularly in the elderly age group, often present insidiously with non-specific symptoms such as weight loss, anorexia and malaise. These symptoms mimic those of malignancy, and often these patients are enrolled in malignancy investigation pathways, thereby causing delays in diagnosis and treatment, which may contribute to poor outcomes [14].
Several risk factors, such as immunosuppression, diabetes, poor oral hygiene, gastro-oesophageal reflux, alcohol excess and intravenous drug use, are known to independently predict increased risk of progression of pneumonia to pleural infection [5, 15, 16]. However, there are currently no validated clinical risk prediction tools that predict the development of pleural infection from pneumonia. A reliable prediction tool for parapneumonic effusion and pleural infection in patients with pneumonia would allow identification of patients that are at high risk of developing these conditions, thereby allowing close monitoring of this group and, therefore, early detection and management to improve outcomes.
Imaging
Chest radiography
The first line of investigation for suspected pleural infection is usually a chest radiograph, which can detect the presence of pleural effusion, consolidative change and any other underlying lung parenchymal pathology that might be contributing to symptoms. However, chest radiographs have poor sensitivity for pleural effusion [17] and can miss more than 10% of significant parapneumonic effusions, particularly in the presence of lower lobe consolidation [18].
Thoracic ultrasound
Thoracic ultrasound is a readily available bedside radiological modality that is used in guiding safe sampling of pleural fluid [19]. It also has a role in detecting features suggestive of a diagnosis of pleural infection prior to fluid sampling, such as septations, loculations and echogenic swirling (figure 1) [20]. However, the role of thoracic ultrasound in predicting outcomes in pleural infection is less clear. Previous studies have indicated that the presence of septations is associated with poor outcomes [21], but these studies were retrospective and unblinded, and more recent better designed studies suggest no association of baseline radiographic septations with outcome [22]. Therefore, the ability of septations (or any other thoracic ultrasound features for that matter) to predict outcomes in pleural infection remains to be seen and requires prospective evaluation.
FIGURE 1.
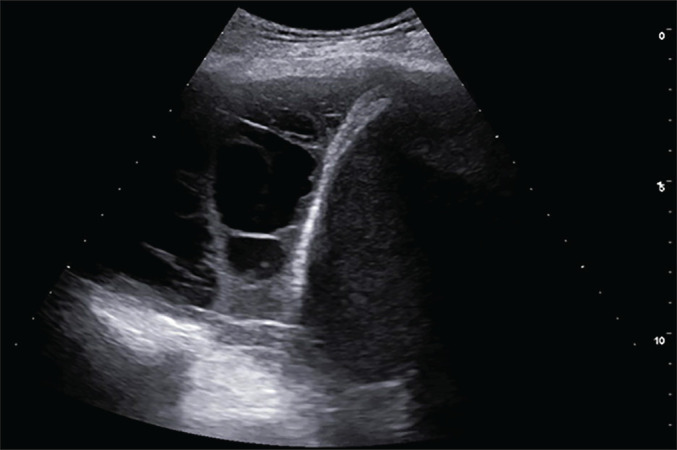
Right thoracic cavity ultrasound scan showing echogenic effusion with coarse septations.
Computed tomography
Computed tomography (CT) of the chest, although not as specific as thoracic ultrasound in diagnosing pleural infection, is useful in providing information on pleural abnormalities. In a retrospective review of 150 patients, CT of the chest was found to accurately predict the need for chest drainage [23]. The authors developed a CT scoring system, as detailed in table 1. However, this scoring system would require prospective validation prior to use in clinical settings. Another retrospective study of 83 patients found the presence of the “split pleura sign” (figure 2) and pleural fluid volume as the only CT features that were predictive of pleural infection [24]. Therefore, CT features may be a useful tool in predicting a diagnosis of pleural infection and need for drainage, but need further prospective studies before being recommended for use in clinical practice.
TABLE 1.
Chest computed tomography scoring system developed by Porcel et al. [23] to predict need for chest drainage in pleural infection
| Pleural contrast enhancement |
| Pleural microbubbles |
| Increased extrapleural fat attenuation |
| Pleural fluid volume ≥400 mL |
FIGURE 2.
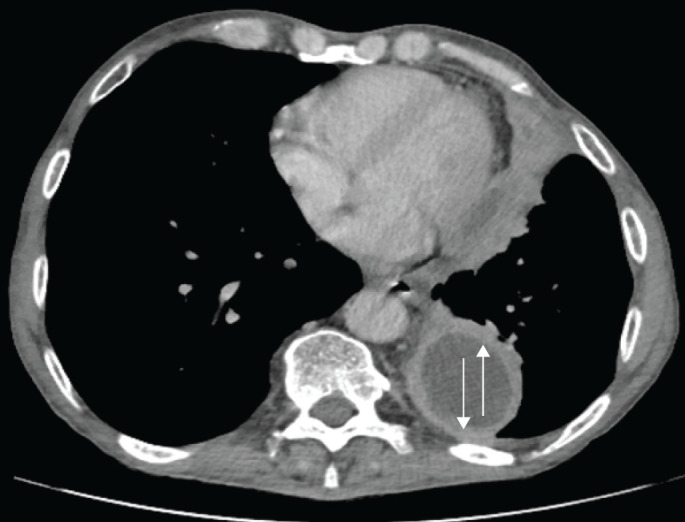
Computed tomography of the chest with a pleural-phase contrast axial cut showing left parietal and visceral pleural enhancement: the split sign (arrows).
Pleural fluid
Pleural fluid sampling remains the gold standard for diagnosis of pleural infection.
Gross appearance
Macroscopically purulent pleural fluid, or empyema, is diagnostic of pleural infection and no further pleural fluid analysis is required. Immediate management with intercostal drainage is recommended [8]. The presence of purulence is said to be associated with better outcomes as indicated by the RAPID (renal, age, purulence, infection source and dietary factors) score [25], which is a prognostic risk model devised specifically for patients with pleural infection. Although this score has been prospectively validated [26], its utility in the clinical setting is yet to be established.
Pleural fluid biochemistry
When pleural fluid is non-purulent, it can be challenging to determine which patients require intercostal drainage. In these situations, biochemical surrogates of pleural infection, including pleural fluid pH, lactate dehydrogenase and glucose, can help guide management. Pleural fluid pH has continued to be the single most useful indicator of the need for drainage of parapneumonic effusion [27]. Previous guidelines have suggested a cut-off of 7.2 to aid management in the everyday clinical setting [2]. However, studies have shown that this criterion is not absolute and a higher pH of up to 7.37 may require drainage [28]. Pleural fluid pH can also be prone to instability and contamination [29]. Therefore, in situations where the pH readings are uncertain or unreliable, pleural fluid glucose (<2.2 mmol·L−1), which has been shown to have high concordance with pH, can be utilised to guide management [15].
The recommendations provided by the newly released British Thoracic Society guidelines [8] on the management of suspected pleural infection based on pleural fluid biochemistry are outlined in table 2.
TABLE 2.
Categorisation of likelihood of pleural infection on the basis of pleural fluid pH and recommended actions as suggested by the 2023 British Thoracic Society guidelines [8]
| Pleural fluid pH | Likelihood of pleural infection | Recommended actions |
| ≤7.2 | High | Intercostal drain insertion |
| >7.2 and <7.4 | Intermediate | 1) Check pleural fluid LDH and glucose; 2) consider intercostal drain if LDH >900 IU·L−1 and glucose ≤4 mmol·L−1 |
| ≥7.4 | Low | Intercostal drain insertion not indicated |
Blood biochemical markers such as white cell count and C-reactive protein are well established biomarkers of infection and have been shown to reliably predict a diagnosis of pleural infection [5, 15]. A large prospective study of 1269 patients with pneumonia has also shown that an elevated platelet count, low serum albumin and a low serum sodium are independent predictors of pleural infection [5]. Conversely, serum procalcitonin has not been shown to be superior to white cell count and C-reactive protein [15, 30].
New pleural fluid biomarkers
Recent investigative research into pleural fluid biomarkers has revealed two promising novel entities, namely soluble urokinase plasminogen activator receptor (suPAR) and plasminogen activator inhibitor (PAI)-1.
suPAR plays a role in the dysregulation of the fibrinogenesis/fibrinolysis cascade that results in the development of loculations [31]. It has been shown to be elevated in infected ascitic and pleural fluid [32, 33]. A single-centre prospective observational study of 93 patients demonstrated that raised pleural fluid suPAR was higher in effusions that were loculated and was predictive of need for intercostal drain insertion [34]. suPAR was also found to be superior to a combination of conventional pleural biomarkers when predicting need for intrapleural fibrinolysis and referral for thoracic surgery. Further large multicentre prospective studies are required to support this finding and delineate the role of suPAR in the diagnosis and management of pleural infection.
PAI-1 is a major inhibitor of fibrinolysis in the injured pleural space and, therefore, promotes pleural septation, which has implications for pleural fluid drainage [35]. It is known to be markedly elevated in infected pleural fluid [36]. A prospective clinical outcome study of 214 samples of pleural fluid showed that higher pleural fluid PAI-1 levels were associated with greater degree of septations in patients with pleural infection [22]. This study also demonstrated a relationship between PAI-1 and clinical outcomes, with higher concentrations of PAI-1 being associated with increased length of hospital stay and increased 12-month mortality, which has never been shown before with a pleural biomarker. Therefore, PAI-1 is the first pleural fluid biomarker that appears to be an independent predictor of mortality in patients with pleural infection.
Pleural fluid culture
Pleural fluid culture, to date, is the recommended modality for microbiology. Although it has a yield of 30–40%, this increases to 60% when inoculated into blood culture bottles [37]. Peripheral blood cultures are important and may be the only positive source of culture (as seen in about 12% of cases in the MIST-1 study (First Multicentre Intrapleural Sepsis Trial)) [2]. Nucleic acid amplification testing can amplify and detect DNA/RNA in clinical samples, and is therefore potentially useful in detecting multiple pathogens, in particular those that are too fastidious to grow [38]. The 16S ribosomal RNA gene, which is present in all bacteria, is one such example [39]. There are several retrospective studies that indicate the utility of 16S ribosomal RNA PCR in detecting the aetiology of pleural infection, particularly when pleural fluid culture is negative, but it is yet to be incorporated into usual clinical practice [40, 41] and may be an oversensitive technique.
Despite being the optimal sampling method, pleural fluid culture is negative in 40% of cases, making one wonder if we are looking for pathogens in the right place. The AUDIO (Advanced Ultrasound in Pleural Infection) feasibility study demonstrated that ultrasound-guided pleural biopsies conducted prior to intercostal drain insertion increased the microbiological yield by 25% with no increased risk of adverse events [42]. A further large prospective trial is required before this approach can be incorporated into clinical practice. Interestingly, in the AUDIO study, 75% of culture-positive pleural tissue had previous antibiotic administration, thereby alluding to the limited penetration of antibiotics into the pleural space or indicating other aspects of pathogenesis in this condition, such as biofilm formation.
Microbiology
The microbiology in pleural infection is different from that of pneumonia [16], with Staphylococcus aureus recently replacing viridans group streptococci as the most common causative pathogen [10, 43]. In addition, approximately 60% of S. aureus pleural infection episodes are due to methicillin-resistant S. aureus (MRSA). A recent systematic review found that the incidence of polymicrobial pleural space infections is approximately 23% but this may well be underestimated due to the use of standard culture techniques [43]. A metagenomics study has estimated that 60% of primary pleural infections (without contiguous pneumonia) are polymicrobial, as opposed to 25% of pneumonia-associated pleural infections [7]. Another recent metagenomics study, which aimed to investigate the entire microbiome of pleural infection using 16S RNA next-generation sequencing (NGS), discovered that pleural infection was predominantly polymicrobial, with an incidence as high as 79% in this cohort [44].
Traditionally, Gram-positive organisms are implicated in community-acquired infections and Gram-negative organisms in hospital-acquired ones [43]. Anaerobes continue to be important causative organisms in pleural infection but may be under-represented in the literature as they are difficult to grow using standard culture methods. The TORPIDS study (The Oxford Pleural Infection Metagenomics Studies), through the use of metagenomics, showed that diverse bacterial frequencies were observed in monomicrobial and polymicrobial disease in both community-acquired and hospital-acquired infections [44]. Mixed anaerobes and Gram-negative bacteria were predominant in community-acquired polymicrobial infection whereas Streptococcus pneumoniae prevailed in monomicrobial cases. Therefore, microbiology in pleural infection can be considered diverse and complex, and use of broad-spectrum antibiotics including anaerobic cover is recommended. Interestingly, although atypical organisms often cause pneumonia, they are rarely identified in pleural infection, possibly indicating an absence of tropism for the pleural space [45]. Atypical antibiotic cover is thus usually not required for pleural infection.
Identification of the causative organism in pleural infection not only has implications for antibiotic choice but also plays a role in predicting the clinical outcome. Analysis of the bacteriology of the participants of the MIST-1 study found a longer duration of hospital stay in patients with non-streptococcal pleural infection, and the 12-month mortality was higher in those with S. aureus infection [16]. The largest microbiology study to date using NGS (TORPIDS) confirmed this finding: the presence of anaerobes and bacteria from the Streptococcus anginosus group were associated with better survival [44]. Predominance of bacteria from the Enterobacteriaceae and Staphylococcus groups were associated with a higher risk of death. These findings suggest that in the future, with the use of metagenomics, it might be possible to risk stratify patients with pleural infection on the basis of their microbiology.
Management of pleural infection
Antibiotic therapy
Empirical broad-spectrum antibiotics have been advocated by all international guidelines once pleural infection is suspected [2, 46]. Appropriate antibiotic therapy for pleural infection is determined by the local institutes’ policies, the infection setting (community-acquired or hospital-acquired), the resistance patterns, and the pharmacological characteristics of the antibiotics.
In the community-acquired infection setting, treatment should target both Gram-positive aerobes and anaerobes until results of cultures become available. Overall, an aminopenicillin (e.g. amoxicillin) has been advocated to cover the likely culprit organisms (S. pneumoniae and Haemophilus influenzae). However, a β-lactamase inhibitor such as co-amoxiclav, and metronidazole, should also be given due to the frequent co-existence of penicillin-resistant aerobes (including S. aureus) and anaerobic bacteria, respectively. For patients that are penicillin-allergic, clindamycin alone, or in combination with ciprofloxacin or a cephalosporin, is likely to provide a good alternative [2, 46]. In monomicrobial infection, particularly with Streptococcus, anaerobic cover is rarely required, and this can help in narrowing antibiotic choice [16, 44].
In the hospital-acquired setting, pleural infection usually arises secondary to nosocomial pneumonia, trauma and surgery. It is therefore recommended that empirical antibiotics provide cover against Gram-positive and Gram-negative aerobes, as well as anaerobic organisms. Antipseudomonal antibiotics with anaerobic coverage are recommended. A reasonable empirical choice is cefepime–metronidazole, piperacillin–tazobactam, or a carbapenem with vancomycin or linezolid. The latter would also cover MRSA, the incidence of which has been rising in pleural infection in the hospital setting [43, 47].
The duration of antibiotic therapy in pleural infection has not been robustly assessed and is largely based on expert opinion and extrapolation from lung abscess treatment data. A minimum of 4 weeks of treatment including both oral and intravenous antibiotics is usually recommended [48]. There are two randomised studies addressing reduction in antibiotic treatment course in pleural infection, but both of these were underpowered [49, 50]. Current British Thoracic Society guidelines recommend stepping down from intravenous to oral antibiotics when there has been “clinical improvement”, which is defined as cessation of pyrexia, resolution of inflammatory markers, and radiological improvement. Usually, 5–7 days of intravenous antibiotics are sufficient to achieve these criteria in most cases [51].
Therapeutic pleural aspirations
Repeated therapeutic thoracentesis (TT) or iterative thoracentesis has been advocated as a modality of treatment for patients with pleural infection in some centres [51]. A literature review of case series comprising 250 patients with pleural infection showed that the treatment success rate of daily TT was 76% with a median of three procedures being required [51–55].
The use of intrapleural fibrinolytic therapy (IPFT) in combination with TT has been retrospectively studied in a comparative cohort study of 132 patients [56]. 81 patients were treated with a combination of intrapleural urokinase and DNase, and 52 were treated with intrapleural urokinase only. The TT failure rate was not found to be statistically significant between the two groups, although the former was associated with quicker fever defervescence, shorter hospital stay and increased volume of fluid drained. These findings would require prospective evaluation.
The ACTion trial (Aspiration versus Chest Tube drainage for pleural infectION), which is a feasibility study that randomised 10 patients with pleural infection to TT or chest tube insertion, with five patients in each arm, showed that the TT arm had a significantly shorter overall mean±sd hospital stay (5.4±5.1 days) compared to the chest tube control group (13±6.0 days; p=0.04) [57]. There was no difference in the total number of pleural procedures required per patient among both groups. The authors proposed that TT allows ambulation of the patient and, hence, reduces hospital stays and cost. Theoretically, this could represent a reasonable option for patients that have no evidence of systemic sepsis, and small to moderate volume effusions or a low RAPID score. However, all the evidence in this aspect of pleural infection management comes from retrospective data. To date, there are no sufficiently powered trial data to support TT as a first modality of treatment; therefore, this has not yet been recommended for pleural infection management by international guidelines.
Chest drain insertion
The use of open thoracic drainage to treat pleural infection dates back to the ancient Greeks, and indeed remained the standard of care for many centuries despite the high mortality rate owing to the presence of open pneumothorax [58, 59].
In 1891, a German physician, Gotthard Bülau, established “closed tube” drainage systems, but these only began to feature more consistently following the “Empyema Commission”, set up by Evarts A. Graham during World War I [60]. Closed thoracic drainage hugely altered the mortality rate of streptococcal pleural infection associated with the great H1N1 influenza pandemic in military hospitals from 30% to 3.4%. Several other measures, such as attention to patients’ nutritional status, rapid sterilisation, obliteration of the infected pleural cavity to prevent chronic empyema, and early avoidance of open pneumothorax, also aided in improving mortality [60].
Since then, closed tube drainage of the thoracic cavity has been the standard of care for patients with pleural infection, although several advances have been made in the tubes used as well as the technique of insertion. The drains used currently are made of plastic and have holes on the side to allow effective drainage of fluid or air. There are centimetre markings to measure the depth and they are easily visualised on chest radiography using a radiopaque tip and line. Drain insertion is usually done under image guidance using the Seldinger technique, which is better tolerated by patients than surgical drain insertion. The drains can also be used to apply fibrinolytics in the infected pleural space to enhance fluid drainage [61–63].
All guidelines advocate prompt chest drain insertion once pleural infection is established, but the appropriate chest tube size continues to be debated [64]. A recent expert consensus statement defined small-bore chest drains as ≤14 F and large-bore chest drains as ≥18 F [65]. It has been postulated that larger size drains may be more efficacious in draining pus from the pleural cavity, although this has been opposed by a number of retrospective studies, which favour a successful outcome with small-bore drains [66–73].
To date, there is only one study that directly compares differences in outcome between small and large chest drains in pleural infection [74]. The MIST-1 trial retrospectively analysed data from 405 patients and demonstrated that drain size does not affect clinical outcomes (mortality or need for surgery) or rate of adverse events. The drain displacement rate was 17–23% in this cohort. Interestingly, this study reported a marked difference in pain scores: large-bore drains (>14 F), particularly those inserted via blunt dissection, were associated with a significantly higher pain score compared to small-bore drains (<14 F) [74–76]. Furthermore, a subgroup analysis from the MIST-2 (Second MIST) trial data showed no difference in treatment outcomes between large- and small-bore drains, thereby echoing the previous result [61].
The rate of drain occlusion in empyema is approximately 63%, as suggested by retrospective data from case series; therefore, saline flushes have been advocated to reduce drain blockage [46, 70, 77, 78]. Hooper et al. [79] prospectively compared saline intrapleural irrigation (250 mL three times per day for 3 days) and best-practice management with best-practice management alone in patients with pleural infection requiring chest-tube drainage. This demonstrated improvement in the volume of pleural collection on CT and reduced surgery referral rate in the intervention arm. However, a multicentre study is required for further approval.
Intrapleural fibrinolytic therapy
It is well recognised that the presence of inflammatory mediators such as tissue plasminogen activator (tPA) inhibitors and tumour necrosis factor (TNF)-α in the infected pleural space in large quantities leads to deposition of fibrin clots and fibrin membranes. This causes increased pleural fluid viscosity and formation of loculations in the pleural cavity, thereby making drainage of the pleural fluid difficult [80, 81]. It is important to note that around 6–27% of patients with pleural infections treated with standard care (antibiotics plus chest drain insertion) require further surgical interventions [61, 74, 82, 83].
Over 70 years ago, Sherry and Tillett demonstrated that the use of a combination of streptokinase and DNase in patients with pleural infection aided in intrapleural fibrinolysis and drainage of viscous purulent pleural fluid [84–86]. Since then, IPFT has been an important aspect of pleural infection management. It has been noted that the use of streptokinase results in significant immunological side-effects and gives rise to an acute inflammatory response [72]. Its use, therefore, was abandoned until the late 1980s when purified urokinase and streptokinase became available for clinical use.
Subsequently, IPFT has been extensively studied through retrospective data and randomised controlled trials. However, the best evidence comes from a recent Cochrane review by Altman et al. [87], which included 993 patients from 12 randomised controlled trials. This demonstrated that there was no difference in overall mortality with fibrinolytic versus placebo (OR 1.16, 95% CI 0.71–1.91; 867 participants; I2=0%; moderate certainty of evidence) [86]. However, in the fibrinolytic group, there was evidence of reduction in surgical intervention (OR 0.37, 95% CI 0.21–0.68; eight studies, 897 participants; I2=51%; low certainty of evidence) and overall treatment failure (OR 0.16, 95% CI 0.05–0.58; seven studies, 769 participants; I2=88%; very low certainty of evidence, with evidence of significant heterogeneity). This “beneficial” effect of fibrinolysis disappeared in a sensitivity analysis that was confined to studies at low or unclear risk of bias. It is noteworthy that the largest trial, MIST-1, which randomised 427 participants to streptokinase versus placebo, also found that there was no benefit to streptokinase in terms of mortality, rate of surgery, radiographic outcomes or length of hospital stay [74].
The effect of IPFT on clinical outcomes was studied in the MIST-2 trial, which demonstrated that a combination of tPA and DNase led to improvements in radiographic clearance [61]. It also demonstrated statistically significant reductions in surgical referral (77%) and length of hospital stay (6.7 days) compared to placebo [61]. Currently, IPFT is the standard of care for non-draining infected pleural space in many centres, with an increasing body of evidence demonstrating both safety and efficacy. The IPFT dosing has been advocated empirically by the MIST-2 authors: intrapleural injection of 10 mg tPA followed by a 10-mL sodium chloride 0.9% flush, then 5 mg DNase, a further 10-mL sodium chloride 0.9% flush in a single setting, and then clamping for 1 h followed by unclamping to allow free drainage. This should be administered twice per day “12-hourly” to a maximum of six doses over three consecutive days [61]. Subsequently, this has been iterated in case series and observational studies using reduced alteplase dosing, including in the ADAPT-1 and ADAPT-2 studies (Alteplase Dose Assessment for Pleural infection Therapy). Moreover, once-daily dosing and concurrent dosing have demonstrated efficacy and safety. The risk of bleeding of IPFT is estimated at 3.8%, with a success rate of up to 90% [61, 88–92].
The risk of bleeding with IPFT has been specifically evaluated in a recent multicentre worldwide retrospective study of a large cohort of pleural infection patients (n=1825) [93]. This demonstrated an overall low bleeding risk (4.2%) and echoed the results reported in the original MIST-2 study [61]. Importantly, when bleeding events did occur, approximately 70% of these were managed with blood transfusion and did not require further intervention. Interestingly, factors such as a high RAPID score, the use of concurrent systemic anticoagulation, renal failure and a low platelet count (<100×109 per L) were independently associated with a higher risk of bleeding complications. It is worth noting that in certain cohorts of patients, such as those on dialysis or those with a recent diagnosis of acute venous thromboembolism in whom temporary cessation of systemic anticoagulation is deemed unsafe, halving the dose of tPA is an option to minimise the risk of bleeding. However, involving haematology and surgical colleagues is advisable [89].
Surgery in pleural infection
Although the MIST-2 trial demonstrated a 77% reduction in surgical referral after IPFT, about 15–20% of patients with pleural infection usually require surgical intervention (16% in the MIST-2 placebo group) [61]. This usually includes those with residual persistent fluid collection, ongoing sepsis [26, 61] or stage 2 or 3 empyema [61, 94]. A recent meta-analysis comparing surgical versus non-surgical management for pleural empyema included 391 patients from eight randomised controlled trials, of which six trials were from the paediatric population and two from adults [95]. The authors concluded that there is no statistically significant difference in mortality between primary surgical and non-surgical management of pleural empyema for all age groups. However, these results must be interpreted very cautiously as paediatric empyema is a clinically distinct entity from adult pleural infection, with very different outcomes and microbiology [94].
The principles of surgery in management of empyema focus on debridement and evacuation of the infected material from the pleural cavity. In advanced stages of pleural infection, the visceral pleura develops a thick rind; therefore, decortication is required to allow lung re-expansion and to maintain a sterile pleural space thereafter. Surgery for pleural infection ranges from the less invasive video-assisted thoracoscopic surgery (VATS) to the more invasive surgical procedures of open thoracotomy (decortication), thoracoplasty and open window thoracotomy [96, 97].
Advances in surgery have led to an increase in the use of VATS as the preferred approach in managing pleural infection. This is largely because of improved post-operative pain control, reduced operative time, shorter length of stay, less blood loss, less air leak, less respiratory compromise, and reduction in post-operative complications including 30-day mortality among VATS patients [98–106]. Another factor in favour of the VATS approach is its lower cost compared with open thoracotomy [100, 106, 107].
Recent robust data from the Society of Thoracic Surgeons’ database advocated early referral of patients with empyema for surgery, citing delay in intervention as associated with poor outcomes [102]. However, the appropriate timing of and candidates for surgery continue to be debated between physicians and surgeons. It is hoped that the RAPID score [25], which is the only prospectively validated mortality prediction tool in patients with pleural infection, might have a role in triaging patients for surgery and aggressive medical treatment. This, however, needs to be evaluated in future trials [26].
Other therapeutic options
Role of local anaesthetic medical thoracoscopy
Medical thoracoscopy has been the standard of care in management of patients with suspected malignant pleural effusion for over a decade [108]. However, the previous and current British Thoracic Society guidelines do not advocate its use for managing pleural infection in adults [2, 8]. Theoretically, medical thoracoscopy seems feasible in this group of patients. In the hands of a skilled physician, it would allow good direct visualisation of the pleural cavity, application of mechanical dissection and breaking up septations, optimisation of bacterial yield by obtaining pleural biopsies, and placement of a chest tube under direct vision. Indeed, the success rate of medical thoracoscopy in managing multiloculated infected pleural effusions has been estimated at 79.3–97.7% by several retrospective studies [109–112].
A recent systematic review on the efficacy of local anaesthetic medical thoracoscopy (LAT) in pleural infection included eight observational studies with sample sizes ranging from 16 to 430 patients [113]. The pooled treatment success rate of thoracoscopy was 85% (95% CI 80.0–90.0%; I2 61.8%) when used as a first-line intervention or after failure of chest tube insertion, whereas the pooled complication rate was 9.0% (95% CI 6.0–14.0%; I2 58.8%). The authors concluded that LAT is safe and effective in managing pleural infection; however, these data are drawn from observational studies and therefore must be interpreted with caution.
A small prospective multicentre trial including 32 patients was performed to compare the safety and efficacy of early LAT versus IPFT in selected patients with multiloculated pleural infection and empyema [114]. This demonstrated that LAT is safe and might shorten hospital stay; however, the authors used a biased end-point (counting time in hospital from the time of intervention rather than randomisation). A multicentre trial with a larger sample size is needed to establish the role of LAT in pleural infection management. The recent SPIRIT trial (Studying Pleuroscopy in Routine Pleural Infection Treatment; ISRCTN98460319) is a multicentre UK feasibility study that has demonstrated failure of feasibility of LAT in pleural infection management in UK centres.
Although evidence for the true role of LAT in pleural infection is lacking, a number of expert centres consider LAT as a treatment modality in patients with multiloculated pleural infection. This is particularly the case for elderly and frail patients who are considered high risk for surgery, and where there is local expertise including sufficient access to LAT, thoracic surgery and anaesthetic support [65].
Intrapleural antibiotics
Intrapleural antibiotics have been studied in the context of pleural infection following pneumonectomy, but the data are sparse and, to date, too inadequate to recommend outside of this specific context [115, 116].
Indwelling pleural catheter and other surgical options
In advanced cases of chronic pleural infection with trapped lung, and where surgical options might not be feasible, such as in patients with significant comorbidities or coincidental cancer, treatment is a real challenge. In these situations, the use of indwelling pleural catheters with prolonged antibiotics has been suggested as a management strategy [117, 118]. However, there is no robust evidence to recommend this approach.
As stated previously, VATS is usually the preferred surgical approach in the management of empyema. However, in clinical scenarios where chronic empyema and a bronchopleural fistula are present, and previous intervention has failed or candidates are deemed unfit for further intervention, open window thoracotomy and thoracoplasty are favoured approaches [119].
Uses of corticosteroid
It is worth noting that infected pleural fluid has a high content of numerous inflammatory mediators, including interleukin (IL)-6, IL-8, TNF-α, vascular endothelial growth factor (VEGF) and monocyte chemotactic protein (MCP). Therefore, theoretically, strategies that modulate the overexaggerated pleural inflammatory response, such as steroids, could attenuate this effect and improve outcomes. This was investigated in the STOPPE trial (Steroid Therapy and Outcome of Parapneumonic Pleural Effusions), which did not demonstrate preliminary benefits of steroids in the management of parapneumonic effusion [120], although this was a feasibility trial.
Risk stratification
Over the last 20 years, despite advances in pleural infection management, the morbidity and mortality of this condition has not changed significantly. The current “one-size-fits-all” approach to sequential management of pleural infection, from chest drain insertion to intrapleural enzyme treatment to surgical referral, which is recommended by all international guidelines, may not be appropriate. Risk stratification at the outset may help physicians tailor management accordingly and thereby improve clinical outcomes.
A large cohort study published by the Danish Pleural Empyema Group reported that a delay of pleural drainage by 2 days from time of diagnosis was associated with worse mortality at 30 and 90 days [14]. Importantly, it has been reported that a delay in surgical referral was associated with a poor outcome and resulted in an increased rate of conversion to open surgery and, therefore, increased mortality among this cohort of patients [102].
The RAPID score was derived and validated in the MIST-1 and MIST-2 cohort studies, respectively [25]. The score is based on five baseline parameters: serum urea (Renal), patient Age, pleural fluid Purulence, Infection source (community- versus healthcare-acquired infection) and serum albumin (Dietary) (table 3). This score has been validated prospectively and externally in the PILOT study (Pleural Infection Longitudinal OuTcome), which demonstrated that low-risk patients (RAPID score 0–2) had a 3-month mortality of 2.3%, medium-risk (RAPID score 3–4) had 9.2% mortality and high-risk (RAPID score 5–7) had 29.3% mortality [26].
TABLE 3.
RAPID score risk stratification
| Parameter | Measure | Score |
| Renal: urea, mmol·L−1 | <5 5–8 >8 |
0 1 2 |
| Age, years | <50 50–70 >70 |
0 1 2 |
| Purulence of fluid | Purulent Non-purulent |
0 1 |
| Infection source | Community-acquired Hospital-acquired |
0 1 |
| Dietary factors: albumin, mmol·L−1 | >27 <27 |
0 1 |
| Risk categories | Score 0–2 Score 3–4 Score 5–7 |
Low risk Moderate risk High risk |
Using baseline clinical parameters in patients with pleural infection, each patient scores from 0 to 7. Reproduced and modified from [25] with permission.
Data from Porcel et al. [121] reported that the RAPID score had been used in 1453 patients from different international centres retrospectively and showed results mirroring the PILOT study. The role of the RAPID score in routine clinical care and decision making, however, is yet to be defined. Current research aims to assess incorporation of the RAPID score into treatment paradigms by risk stratifying patients with pleural infection at the outset, potentially offering lower and higher aggression of therapy according to underlying risk.
Conclusion
In conclusion, pleural infection remains a formidable medical challenge. The increasing incidence and intricate clinical presentations make diagnosis complex. Imaging modalities and pleural fluid analysis aid in accurate diagnosis, with emerging biomarkers holding potential for enhanced diagnostic and prognostic precision. The multifaceted management approach encompasses antibiotic therapy, therapeutic pleural aspirations, chest drain insertion, IPFT and surgery. Empirical antibiotic regimens tailored to local resistance patterns play a pivotal role. Chest drain insertion remains a cornerstone, while the integration of IPFT facilitates efficient drainage. Surgical interventions, including VATS and decortication, are reserved for advanced cases. Risk stratification tools like the RAPID score may offer personalised guidance in management. Ongoing research endeavours seek to optimise outcomes by aligning interventions with individualised risk profiles. As our understanding evolves, a comprehensive and tailored approach holds the key to addressing the persistent challenges posed by pleural infections.
Key points
Pleural fluid analysis is the gold standard for diagnosis; novel biomarkers such as suPAR and PAI-1 hold promise in aiding diagnosis and prognosis in pleural infection.
The use of metagenomics in pleural infection shows a complex microbiome that differs from pneumonia, with polymicrobial infections being prevalent, which can influence antibiotic choice and clinical outcomes.
The management of pleural infection involves various strategies including antibiotic therapy, therapeutic pleural aspirations, chest drain insertion, IPFT and surgery.
Risk stratification through the RAPID score could guide tailored management approaches.
Footnotes
Conflict of interest: The authors have nothing to disclose.
References
- 1.Rosenstengel A. Pleural infection – current diagnosis and management. J Thorac Dis 2012; 4: 186–193. doi: 10.3978/j.issn.2072-1439.2012.01.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davies HE, Davies RJO, Davies CWH. Management of pleural infection in adults: British Thoracic Society pleural disease guideline 2010. Thorax 2010; 65: Suppl. 2, ii41–ii53. doi: 10.1136/thx.2010.137000 [DOI] [PubMed] [Google Scholar]
- 3.Peters RM. Empyema thoracis: historical perspective. Ann Thorac Surg 1989; 48: 306–308. doi: 10.1016/0003-4975(89)90100-8 [DOI] [PubMed] [Google Scholar]
- 4.Sahn SA. Diagnosis and management of parapneumonic effusions and empyema. Clin Infect Dis 2007; 45: 1480–1486. doi: 10.1086/522996 [DOI] [PubMed] [Google Scholar]
- 5.Chalmers JD, Singanayagam A, Murray MP, et al. . Risk factors for complicated parapneumonic effusion and empyema on presentation to hospital with community-acquired pneumonia. Thorax 2009; 64: 592–597. doi: 10.1136/thx.2008.105080 [DOI] [PubMed] [Google Scholar]
- 6.Brims F, Popowicz N, Rosenstengel A, et al. . Bacteriology and clinical outcomes of patients with culture-positive pleural infection in Western Australia: a 6-year analysis. Respirology 2019; 24: 171–178. doi: 10.1111/resp.13395 [DOI] [PubMed] [Google Scholar]
- 7.Dyrhovden R, Nygaard RM, Patel R, et al. . The bacterial aetiology of pleural empyema. A descriptive and comparative metagenomic study. Clin Microbiol Infect 2019; 25: 981–986. doi: 10.1016/j.cmi.2018.11.030 [DOI] [PubMed] [Google Scholar]
- 8.Roberts ME, Rahman NM, Maskell NA, et al. . British Thoracic Society Guideline for pleural disease. Thorax 2023; 78: Suppl. 3, s1–s42. doi: 10.1136/thorax-2022-219784 [DOI] [PubMed] [Google Scholar]
- 9.Finley C, Clifton J, FitzGerald JM, et al. . Empyema: an increasing concern in Canada. Can Respir J 2008; 15: 85–89. doi: 10.1155/2008/975312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grijalva CG, Zhu Y, Nuorti JP, et al. . Emergence of parapneumonic empyema in the USA. Thorax 2011; 66: 663–668. doi: 10.1136/thx.2010.156406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arnold DT, Hamilton FW, Morris TT, et al. . Epidemiology of pleural empyema in English hospitals and the impact of influenza. Eur Respir J 2021; 57: 2003546. doi: 10.1183/13993003.03546-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Søgaard M, Nielsen RB, Nørgaard M, et al. . Incidence, length of stay, and prognosis of hospitalized patients with pleural empyema: a 15-year Danish nationwide cohort study. Chest 2014; 145: 189–192. doi: 10.1378/chest.13-1912 [DOI] [PubMed] [Google Scholar]
- 13.Dean NC, Griffith PP, Sorensen JS, et al. . Pleural effusions at first ED encounter predict worse clinical outcomes in patients with pneumonia. Chest 2016; 149: 1509–1515. doi: 10.1016/j.chest.2015.12.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyer CN, Armbruster K, Kemp M, et al. . Pleural infection: a retrospective study of clinical outcome and the correlation to known etiology, co-morbidity and treatment factors. BMC Pulm Med 2018; 18: 160. doi: 10.1186/s12890-018-0726-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Falguera M, Carratalà J, Bielsa S, et al. . Predictive factors, microbiology and outcome of patients with parapneumonic effusion. Eur Respir J 2011; 38: 1173–1179. doi: 10.1183/09031936.00000211 [DOI] [PubMed] [Google Scholar]
- 16.Maskell NA, Batt S, Hedley EL, et al. . The bacteriology of pleural infection by genetic and standard methods and its mortality significance. Am J Respir Crit Care Med 2006; 174: 817–823. doi: 10.1164/rccm.200601-074OC [DOI] [PubMed] [Google Scholar]
- 17.Svigals PZ, Chopra A, Ravenel JG, et al. . The accuracy of pleural ultrasonography in diagnosing complicated parapneumonic pleural effusions. Thorax 2017; 72: 94–95. doi: 10.1136/thoraxjnl-2016-208904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brixey AG, Luo Y, Skouras V, et al. . The efficacy of chest radiographs in detecting parapneumonic effusions. Respirology 2011; 16: 1000–1004. doi: 10.1111/j.1440-1843.2011.02006.x [DOI] [PubMed] [Google Scholar]
- 19.Diacon AH, Brutsche MH, Soler M. Accuracy of pleural puncture sites: a prospective comparison of clinical examination with ultrasound. Chest 2003; 123: 436–441. doi: 10.1378/chest.123.2.436 [DOI] [PubMed] [Google Scholar]
- 20.Marchetti G, Arondi S, Baglivo F, et al. . New insights in the use of pleural ultrasonography for diagnosis and treatment of pleural disease. Clin Respir J 2018; 12: 1993–2005. doi: 10.1111/crj.12907 [DOI] [PubMed] [Google Scholar]
- 21.Bedawi EO, Hassan M, Harriss E, et al. . S57 Sonographic septations in pleural infection – what do they actually mean? Thorax 2018; 73: Suppl. 4, A35. doi: 10.1136/thorax-2018-212555.63 [DOI] [Google Scholar]
- 22.Bedawi EO, Kanellakis NI, Corcoran JP, et al. . The biological role of pleural fluid PAI-1 and sonographic septations in pleural infection: analysis of a prospectively collected clinical outcome study. Am J Respir Crit Care Med 2023; 207: 731–739. doi: 10.1164/rccm.202206-1084OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Porcel JM, Pardina M, Alemán C, et al. . Computed tomography scoring system for discriminating between parapneumonic effusions eventually drained and those cured only with antibiotics. Respirology 2017; 22: 1199–1204. doi: 10.1111/resp.13040 [DOI] [PubMed] [Google Scholar]
- 24.Tsujimoto N, Saraya T, Light RW, et al. . A simple method for differentiating complicated parapneumonic effusion/empyema from parapneumonic effusion using the split pleura sign and the amount of pleural effusion on thoracic CT. PLoS One 2015; 10: e0130141. doi: 10.1371/journal.pone.0130141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rahman NM, Kahan BC, Miller RF, et al. . A clinical score (RAPID) to identify those at risk for poor outcome at presentation in patients with pleural infection. Chest 2014; 145: 848–855. doi: 10.1378/chest.13-1558 [DOI] [PubMed] [Google Scholar]
- 26.Corcoran JP, Psallidas I, Gerry S, et al. . Prospective validation of the RAPID clinical risk prediction score in adult patients with pleural infection: the PILOT study. Eur Respir J 2020; 56: 2000130. doi: 10.1183/13993003.00130-2020 [DOI] [PubMed] [Google Scholar]
- 27.Heffner JE, Brown LK, Barbieri C, et al. . Pleural fluid chemical analysis in parapneumonic effusions. A meta-analysis. Am J Respir Crit Care Med 1995; 151: 1700–1708. doi: 10.1164/ajrccm.151.6.7767510 [DOI] [PubMed] [Google Scholar]
- 28.Jiménez Castro D, Díaz Nuevo G, Sueiro A, et al. . Pleural fluid parameters identifying complicated parapneumonic effusions. Respiration 2005; 72: 357–364. doi: 10.1159/000086248 [DOI] [PubMed] [Google Scholar]
- 29.Rahman NM, Mishra EK, Davies HE, et al. . Clinically important factors influencing the diagnostic measurement of pleural fluid pH and glucose. Am J Respir Crit Care Med 2008; 178: 483–490. doi: 10.1164/rccm.200801-062OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dixon G, Lama-Lopez A, Bintcliffe OJ, et al. . The role of serum procalcitonin in establishing the diagnosis and prognosis of pleural infection. Respir Res 2017; 18: 30. doi: 10.1186/s12931-017-0501-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Matzkies LM, Raggam RB, Flick H, et al. . Prognostic and diagnostic potential of suPAR levels in pleural effusion. J Infect 2017; 75: 465–467. doi: 10.1016/j.jinf.2017.07.002 [DOI] [PubMed] [Google Scholar]
- 32.Bakker OGM, Hemmes SNT, Backes Y, et al. . SuPAR in pleural fluid may function as a biological marker for infection in critically ill patients with pleural effusions. J Infect 2014; 68: 607–609. doi: 10.1016/j.jinf.2014.02.005 [DOI] [PubMed] [Google Scholar]
- 33.Zimmermann HW, Reuken PA, Koch A, et al. . Soluble urokinase plasminogen activator receptor is compartmentally regulated in decompensated cirrhosis and indicates immune activation and short-term mortality. J Intern Med 2013; 274: 86–100. doi: 10.1111/joim.12054 [DOI] [PubMed] [Google Scholar]
- 34.Arnold DT, Hamilton FW, Elvers KT, et al. . Pleural fluid suPAR levels predict the need for invasive management in parapneumonic effusions. Am J Respir Crit Care Med 2020; 201: 1545–1553. doi: 10.1164/rccm.201911-2169OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Komissarov AA, Rahman N, Lee YCG, et al. . Fibrin turnover and pleural organization: bench to bedside. Am J Physiol Lung Cell Mol Physiol 2018; 314: L757–L768. doi: 10.1152/ajplung.00501.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beckert L, Brockway B, Simpson G, et al. . Phase 1 trial of intrapleural LTI-01; single chain urokinase in complicated parapneumonic effusions or empyema. JCI Insight 2019; 5: e127470. doi: 10.1172/jci.insight.127470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Menzies SM, Rahman NM, Wrightson JM, et al. . Blood culture bottle culture of pleural fluid in pleural infection. Thorax 2011; 66: 658–662. doi: 10.1136/thx.2010.157842 [DOI] [PubMed] [Google Scholar]
- 38.Wrightson JM, Rahman NM, Crook DWM, et al. . Improving pathogen identification in pleural infection – application of molecular techniques. Am J Respir Crit Care Med 2012; 185: A5244. doi: 10.1164/ajrccm-conference.2012.185.1_MeetingAbstracts.A5244 [DOI] [Google Scholar]
- 39.Insa R, Marín M, Martín A, et al. . Systematic use of universal 16S rRNA gene polymerase chain reaction (PCR) and sequencing for processing pleural effusions improves conventional culture techniques. Medicine 2012; 91: 103–110. doi: 10.1097/MD.0b013e31824dfdb0 [DOI] [PubMed] [Google Scholar]
- 40.Hjertman J, Bläckberg J, Ljungquist O. 16S rRNA is a valuable tool in finding bacterial aetiology of community-acquired pleural empyema – a population-based observational study in South Sweden. Infect Dis 2022; 54: 163–169. doi: 10.1080/23744235.2021.1985165 [DOI] [PubMed] [Google Scholar]
- 41.Lampejo T, Ciesielczuk H, Lambourne J. Clinical utility of 16S rRNA PCR in pleural infection. J Med Microbiol 2021; 70: 001366. doi: 10.1099/jmm.0.001366 [DOI] [PubMed] [Google Scholar]
- 42.Psallidas I, Kanellakis NI, Bhatnagar R, et al. . A pilot feasibility study in establishing the role of ultrasound-guided pleural biopsies in pleural infection (the AUDIO study). Chest 2018; 154: 766–772. doi: 10.1016/j.chest.2018.02.031 [DOI] [PubMed] [Google Scholar]
- 43.Hassan M, Cargill T, Harriss E, et al. . The microbiology of pleural infection in adults: a systematic review. Eur Respir J 2019; 54: 1900542. doi: 10.1183/13993003.00542-2019 [DOI] [PubMed] [Google Scholar]
- 44.Kanellakis NI, Wrightson JM, Gerry S, et al. . The bacteriology of pleural infection (TORPIDS): an exploratory metagenomics analysis through next generation sequencing. Lancet Microbe 2022; 3: e294–e302. doi: 10.1016/S2666-5247(21)00327-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wrightson JM, Wray JA, Street TL, et al. . Absence of atypical pathogens in pleural infection. Chest 2015; 148: e102–e103. doi: 10.1378/chest.15-1130 [DOI] [PubMed] [Google Scholar]
- 46.Shen KR, Bribriesco A, Crabtree T, et al. . The American Association for Thoracic Surgery consensus guidelines for the management of empyema. J Thorac Cardiovasc Surg 2017; 153: e129–e146. doi: 10.1016/j.jtcvs.2017.01.030 [DOI] [PubMed] [Google Scholar]
- 47.Kollef MH, Shorr A, Tabak YP, et al. . Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest 2005; 128: 3854–3862. doi: 10.1378/chest.128.6.3854 [DOI] [PubMed] [Google Scholar]
- 48.Bedawi EO, George V, Rahman NM. A new approach to pleural infection: let it be? Curr Pulmonol Rep 2019; 8: 112–122. doi: 10.1007/s13665-019-00230-1 [DOI] [Google Scholar]
- 49.Porcel JM, Ferreiro L, Rumi L, et al. . Two vs. three weeks of treatment with amoxicillin-clavulanate for stabilized community-acquired complicated parapneumonic effusions. A preliminary non-inferiority, double-blind, randomized, controlled trial. Pleura Peritoneum 2020; 5: 20190027. doi: 10.1515/pp-2019-0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hassan M, Gad-Allah M, El-Shaarawy B, et al. . The Short versus Long Antibiotic Course for Pleural Infection Management (SLIM) randomised controlled open-label trial. ERJ Open Res 2023; 9: 00635-2022. doi: 10.1183/23120541.00635-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Porcel JM, Valencia H, Bielsa S. Adult patients with parapneumonic empyema who may not require pleural drainage. Rev Clin Esp 2016; 216: 172–174. doi: 10.1016/j.rce.2016.01.001 [DOI] [PubMed] [Google Scholar]
- 52.Letheulle J, Tattevin P, Saunders L, et al. . Iterative thoracentesis as first-line treatment of complicated parapneumonic effusion. PLoS One 2014; 9: e84788. doi: 10.1371/journal.pone.0084788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jouneau S, Letheulle J, Desrues B. Repeated therapeutic thoracentesis to manage complicated parapneumonic effusions. Curr Opin Pulm Med 2015; 21: 387–392. doi: 10.1097/MCP.0000000000000171 [DOI] [PubMed] [Google Scholar]
- 54.Simmers TA, Jie C, Sie B. Minimally invasive treatment of thoracic empyema. Thorac Cardiovasc Surg 1999; 47: 77–81. doi: 10.1055/s-2007-1013115 [DOI] [PubMed] [Google Scholar]
- 55.Storm HK, Krasnik M, Bang K, et al. . Treatment of pleural empyema secondary to pneumonia: thoracocentesis regimen versus tube drainage. Thorax 1992; 47: 821–824. doi: 10.1136/thx.47.10.821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Luque Paz D, Bayeh B, Chauvin P, et al. . Intrapleural use of urokinase and DNase in pleural infections managed with repeated thoracentesis: a comparative cohort study. PLoS One 2021; 16: e0257339. doi: 10.1371/journal.pone.0257339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Arnold DT, Tucker E, Morley A, et al. . A feasibility randomised trial comparing therapeutic thoracentesis to chest tube insertion for the management of pleural infection: results from the ACTion trial. BMC Pulm Med 2022; 22: 330. doi: 10.1186/s12890-022-02126-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Christopoulou-Aletra H, Papavramidou N. “Empyemas” of the thoracic cavity in the Hippocratic Corpus. Ann Thorac Surg 2008; 85: 1132–1134. doi: 10.1016/j.athoracsur.2007.11.031 [DOI] [PubMed] [Google Scholar]
- 59.Walcott-Sapp S, Sukumar M. A history of thoracic drainage: from ancient Greeks to wound sucking drummers to digital monitoring. CTSNet, 2015. www.ctsnet.org/article/history-thoracic-drainage-ancient-greeks-wound-sucking-drummers-digital-monitoring [Google Scholar]
- 60.Graham EA. Some Fundamental Considerations in the Treatment of Empyema Thoracis. St Louis, C.V. Mosby Company, 1925. [Google Scholar]
- 61.Rahman NM, Maskell NA, West A, et al. . Intrapleural use of tissue plasminogen activator and DNase in pleural infection. N Engl J Med 2011; 365: 518–526. doi: 10.1056/NEJMoa1012740 [DOI] [PubMed] [Google Scholar]
- 62.Mahmood K, Wahidi MM. Straightening out chest tubes: what size, what type, and when. Clin Chest Med 2013; 34: 63–71. doi: 10.1016/j.ccm.2012.11.007 [DOI] [PubMed] [Google Scholar]
- 63.Miller KS, Sahn SA. Chest tubes: indications, technique, management and complications. Chest 1987; 91: 258–264. doi: 10.1378/chest.91.2.258 [DOI] [PubMed] [Google Scholar]
- 64.Light RW. Pleural controversy: optimal chest tube size for drainage. Respirology 2011; 16: 244–248. doi: 10.1111/j.1440-1843.2010.01913.x [DOI] [PubMed] [Google Scholar]
- 65.Bedawi EO, Ricciardi S, Hassan M, et al. . ERS/ESTS statement on the management of pleural infection in adults. Eur Respir J 2023; 61: 2201062. doi: 10.1183/13993003.01062-2022 [DOI] [PubMed] [Google Scholar]
- 66.Klein JS, Schultz S, Heffner JE. Interventional radiology of the chest: image-guided percutaneous drainage of pleural effusions, lung abscess, and pneumothorax. AJR Am J Roentgenol 1995; 164: 581–588. doi: 10.2214/ajr.164.3.7863875 [DOI] [PubMed] [Google Scholar]
- 67.Crouch JD, Keagy BA, Delany DJ. “Pigtail” catheter drainage in thoracic surgery. Am Rev Respir Dis 1987; 136: 174–175. doi: 10.1164/ajrccm/136.1.174 [DOI] [PubMed] [Google Scholar]
- 68.Hunnam GR, Flower CDR. Radiologically-guided percutaneous catheter drainage of empyemas. Clin Radiol 1988; 39: 121–126. doi: 10.1016/S0009-9260(88)80006-0 [DOI] [PubMed] [Google Scholar]
- 69.O'Moore PV, Mueller PR, Simeone JF, et al. . Sonographic guidance in diagnostic and therapeutic interventions in the pleural space. AJR Am J Roentgenol 1987; 149: 1–5. doi: 10.2214/ajr.149.1.1 [DOI] [PubMed] [Google Scholar]
- 70.Horsley A, Jones L, White J, et al. . Efficacy and complications of small-bore, wire-guided chest drains. Chest 2006; 130: 1857–1863. doi: 10.1378/chest.130.6.1857 [DOI] [PubMed] [Google Scholar]
- 71.Keeling AN, Leong S, Logan PM, et al. . Empyema and effusion: outcome of image-guided small-bore catheter drainage. Cardiovasc Intervent Radiol 2008; 31: 135–141. doi: 10.1007/s00270-007-9197-0 [DOI] [PubMed] [Google Scholar]
- 72.Stavas J, Casola G, Wittich GR. Percutaneous drainage of infected and noninfected thoracic fluid collections. J Thorac Imaging 1987; 2: 80–87. doi: 10.1097/00005382-198707000-00011 [DOI] [PubMed] [Google Scholar]
- 73.Silverman SG, Mueller PR, Saini S, et al. . Thoracic empyema: management with image-guided catheter drainage. Radiology 1988; 169: 5–9. doi: 10.1148/radiology.169.1.3047789 [DOI] [PubMed] [Google Scholar]
- 74.Maskell N, Nunn A, Davies RJO. Intrapleural streptokinase for pleural infection. BMJ 2006; 332: 552. doi: 10.1136/bmj.332.7540.552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hallifax RJ, Psallidas I, Rahman NM. Chest drain size: the debate continues. Curr Pulmonol Rep 2017; 6: 26–29. doi: 10.1007/s13665-017-0162-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rahman NM, Maskell NA, Davies CWH, et al. . The relationship between chest tube size and clinical outcome in pleural infection. Chest 2010; 137: 536–543. doi: 10.1378/chest.09-1044 [DOI] [PubMed] [Google Scholar]
- 77.Cafarotti S, Dall'Armi V, Cusumano G, et al. . Small-bore wire-guided chest drains: safety, tolerability, and effectiveness in pneumothorax, malignant effusions, and pleural empyema. J Thorac Cardiovasc Surg 2011; 141: 683–687. doi: 10.1016/j.jtcvs.2010.08.044 [DOI] [PubMed] [Google Scholar]
- 78.Davies HE, Merchant S, McGown A. A study of the complications of small bore “Seldinger” intercostal chest drains. Respirology 2008; 13: 603–607. doi: 10.1111/j.1440-1843.2008.01296.x [DOI] [PubMed] [Google Scholar]
- 79.Hooper CE, Edey AJ, Wallis A, et al. . Pleural irrigation trial (PIT): a randomised controlled trial of pleural irrigation with normal saline versus standard care in patients with pleural infection. Eur Respir J 2015; 46: 456–463. doi: 10.1183/09031936.00147214 [DOI] [PubMed] [Google Scholar]
- 80.Simpson G, Roomes D, Heron M. Effects of streptokinase and deoxyribonuclease on viscosity of human surgical and empyema pus. Chest 2000; 117: 1728–1733. doi: 10.1378/chest.117.6.1728 [DOI] [PubMed] [Google Scholar]
- 81.Idell S, Florova G, Shetty S, et al. . Precision-guided, personalized intrapleural fibrinolytic therapy for empyema and complicated parapneumonic pleural effusions: the case for the fibrinolytic potential. Clin Pulm Med 2017; 24: 163–169. doi: 10.1097/CPM.0000000000000216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bouros D, Schiza S, Tzanakis N, et al. . Intrapleural urokinase versus normal saline in the treatment of complicated parapneumonic effusions and empyema: a randomized, double-blind study. Am J Respir Crit Care Med 1999; 159: 37–42. doi: 10.1164/ajrccm.159.1.9803094 [DOI] [PubMed] [Google Scholar]
- 83.Davies RJ, Traill ZC, Gleeson FV. Randomised controlled trial of intrapleural streptokinase in community acquired pleural infection. Thorax 1997; 52: 416–421. doi: 10.1136/thx.52.5.416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tillett WS, Sherry S. The effect in patients of streptococcal fibrinolysin (streptokinase) and streptococcal desoxyribonuclease on fibrinous, purulent, and sanguinous pleural exudations. J Clin Invest 1949; 28: 173–190. doi: 10.1172/JCI102046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tillett WS, Sherry S, Christensen LR. Streptococcal desoxyribonuclease: significance in lysis of purulent exudates and production by strains of hemolytic streptococci. Proc Soc Exp Biol Med 1948; 68: 184–188. doi: 10.3181/00379727-68-16429 [DOI] [PubMed] [Google Scholar]
- 86.Sherry S, Tillett WS, Christensen LR. Presence and significance of desoxyribose nucleoprotein in the purulent pleural exudates of patients. Proc Soc Exp Biol Med 1948; 68: 179–184. doi: 10.3181/00379727-68-16428 [DOI] [PubMed] [Google Scholar]
- 87.Altmann ES, Crossingham I, Wilson S, et al. . Intra-pleural fibrinolytic therapy versus placebo, or a different fibrinolytic agent, in the treatment of adult parapneumonic effusions and empyema. Cochrane Database Syst Rev 2019; 10: CD002312. doi: 10.1002/14651858.CD002312.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Majid A, Kheir F, Folch A, et al. . Concurrent intrapleural instillation of tissue plasminogen activator and DNase for pleural infection. A single-center experience. Ann Am Thorac Soc 2016; 13: 1512–1518. doi: 10.1513/AnnalsATS.201602-127OC [DOI] [PubMed] [Google Scholar]
- 89.Popowicz N, Ip H, Lau EPM, et al. . Alteplase Dose Assessment for Pleural infection Therapy (ADAPT) Study-2: use of 2.5 mg alteplase as a starting intrapleural dose. Respirology 2022; 27: 510–516. doi: 10.1111/resp.14261 [DOI] [PubMed] [Google Scholar]
- 90.Mehta HJ, Biswas A, Penley AM, et al. . Management of intrapleural sepsis with once daily use of tissue plasminogen activator and deoxyribonuclease. Respiration 2016; 91: 101–106. doi: 10.1159/000443334 [DOI] [PubMed] [Google Scholar]
- 91.McClune JR, Wilshire CL, Gorden JA, et al. . Safety and efficacy of intrapleural tissue plasminogen activator and DNase during extended use in complicated pleural space infections. Can Respir J 2016; 2016: 9796768. doi: 10.1155/2016/9796768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Piccolo F, Pitman N, Bhatnagar R, et al. . Intrapleural tissue plasminogen activator and deoxyribonuclease for pleural infection. An effective and safe alternative to surgery. Ann Am Thorac Soc 2014; 11: 1419–1425. doi: 10.1513/AnnalsATS.201407-329OC [DOI] [PubMed] [Google Scholar]
- 93.Akulian J, Bedawi EO, Abbas H, et al. . Bleeding risk with combination intrapleural fibrinolytic and enzyme therapy in pleural infection: an international, multicenter, retrospective cohort study. Chest 2022; 162: 1384–1392. doi: 10.1016/j.chest.2022.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Colice GL, Curtis A, Deslauriers J, et al. . Medical and surgical treatment of parapneumonic effusions: an evidence-based guideline. Chest 2000; 118: 1158–1171. doi: 10.1378/chest.118.4.1158 [DOI] [PubMed] [Google Scholar]
- 95.Redden MD, Chin TY, van Driel ML. Surgical versus non-surgical management for pleural empyema. Cochrane Database Syst Rev 2017; 3: CD010651. doi: 10.1002/14651858.CD010651.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Belcher E, Edwards JG. The role of surgery in pleural disease. In: Maskell NA, Laursen CB, Lee YCG, et al., eds. Pleural Disease (ERS Monograph). Sheffield, European Respiratory Society, 2020; pp. 263–281. [Google Scholar]
- 97.Molnar TF. Current surgical treatment of thoracic empyema in adults. Eur J Cardiothorac Surg 2007; 32: 422–430. doi: 10.1016/j.ejcts.2007.05.028 [DOI] [PubMed] [Google Scholar]
- 98.Farjah F, Backhus LM, Varghese TK, et al. . Ninety-day costs of video-assisted thoracic surgery versus open lobectomy for lung cancer. Ann Thorac Surg 2014; 98: 191–196. doi: 10.1016/j.athoracsur.2014.03.024 [DOI] [PubMed] [Google Scholar]
- 99.Muhammad MIA. Management of complicated parapneumonic effusion and empyema using different treatment modalities. Asian Cardiovasc Thorac Ann 2012; 20: 177–181. doi: 10.1177/0218492311435338 [DOI] [PubMed] [Google Scholar]
- 100.Chambers A, Routledge T, Dunning J, et al. . Is video-assisted thoracoscopic surgical decortication superior to open surgery in the management of adults with primary empyema? Interact Cardiovasc Thorac Surg 2010; 11: 171–177. doi: 10.1510/icvts.2010.240408 [DOI] [PubMed] [Google Scholar]
- 101.Höfken H, Herrmann D, Ewig S, et al. . Video-assisted thoracoscopic surgery of parapneumonic empyema – a 10-year single-centre experience. Pneumologie 2018; 72: 843–850. doi: 10.1055/a-0648-0145 [DOI] [PubMed] [Google Scholar]
- 102.Towe CW, Carr SR, Donahue JM, et al. . Morbidity and 30-day mortality after decortication for parapneumonic empyema and pleural effusion among patients in the Society of Thoracic Surgeons’ General Thoracic Surgery Database. J Thorac Cardiovasc Surg 2019; 157: 1288–1297. doi: 10.1016/j.jtcvs.2018.10.157 [DOI] [PubMed] [Google Scholar]
- 103.Scarci M, Abah U, Solli P, et al. . EACTS expert consensus statement for surgical management of pleural empyema. Eur J Cardiothorac Surg 2015; 48: 642–653. doi: 10.1093/ejcts/ezv272 [DOI] [PubMed] [Google Scholar]
- 104.Tong BC, Hanna J, Toloza EM, et al. . Outcomes of video-assisted thoracoscopic decortication. Ann Thorac Surg 2010; 89: 220–225. doi: 10.1016/j.athoracsur.2009.09.021 [DOI] [PubMed] [Google Scholar]
- 105.Casali C, Susanna Storelli E, Di Prima E, et al. . Long-term functional results after surgical treatment of parapneumonic thoracic empyema. Interact Cardiovasc Thorac Surg 2009; 9: 74–78. doi: 10.1510/icvts.2009.203190 [DOI] [PubMed] [Google Scholar]
- 106.Shahin Y, Duffy J, Beggs D, et al. . Surgical management of primary empyema of the pleural cavity: outcome of 81 patients. Interact Cardiovasc Thorac Surg 2010; 10: 565–567. doi: 10.1510/icvts.2009.215004 [DOI] [PubMed] [Google Scholar]
- 107.Shiraishi Y. Surgical treatment of chronic empyema. Gen Thorac Cardiovasc Surg 2010; 58: 311–316. doi: 10.1007/s11748-010-0599-6 [DOI] [PubMed] [Google Scholar]
- 108.Rahman NM, Ali NJ, Brown G, et al. . Local anaesthetic thoracoscopy: British Thoracic Society pleural disease guideline 2010. Thorax 2010; 65: Suppl. 2, ii54–ii60. doi: 10.1136/thx.2010.137018 [DOI] [PubMed] [Google Scholar]
- 109.Brutsche MH, Tassi GF, Györik S, et al. . Treatment of sonographically stratified multiloculated thoracic empyema by medical thoracoscopy. Chest 2005; 128: 3303–3309. doi: 10.1378/chest.128.5.3303 [DOI] [PubMed] [Google Scholar]
- 110.Ravaglia C, Gurioli C, Tomassetti S, et al. . Is medical thoracoscopy efficient in the management of multiloculated and organized thoracic empyema? Respiration 2012; 84: 219–224. doi: 10.1159/000339414 [DOI] [PubMed] [Google Scholar]
- 111.Tacconi F, Pompeo E, Fabbi E, et al. . Awake video-assisted pleural decortication for empyema thoracis. Eur J Cardiothorac Surg 2010; 37: 594–601. doi: 10.1016/j.ejcts.2009.08.003 [DOI] [PubMed] [Google Scholar]
- 112.Ohuchi M, Inoue S, Ozaki Y, et al. . Single-trocar thoracoscopy under local anesthesia for pleural space infection. Gen Thorac Cardiovasc Surg 2014; 62: 503–510. doi: 10.1007/s11748-014-0405-y [DOI] [PubMed] [Google Scholar]
- 113.Mondoni M, Saderi L, Trogu F, et al. . Medical thoracoscopy treatment for pleural infections: a systematic review and meta-analysis. BMC Pulm Med 2021; 21: 127. doi: 10.1186/s12890-021-01492-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kheir F, Thakore S, Mehta H, et al. . Intrapleural fibrinolytic therapy versus early medical thoracoscopy for treatment of pleural infection. Randomized controlled clinical trial. Ann Am Thorac Soc 2020; 17: 958–964. doi: 10.1513/AnnalsATS.202001-076OC [DOI] [PubMed] [Google Scholar]
- 115.Ng T, Ryder BA, Maziak DE, et al. . Treatment of postpneumonectomy empyema with debridement followed by continuous antibiotic irrigation. J Am Coll Surg 2008; 206: 1178–1183. doi: 10.1016/j.jamcollsurg.2008.01.005 [DOI] [PubMed] [Google Scholar]
- 116.Rana MA, El Rahman BA, Mady AF, et al. . Intra-pleural colistin methanesulfonate therapy for pleural infection caused by carbapenem-resistant Acinetobacter baumannii: a successful case report. Infect Dis Rep 2014; 6: 5413. doi: 10.4081/idr.2014.5413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Saqib IU, Iqbal M, Rana A, et al. . Experience with ambulatory management of pleural pathologies utilizing small-bore indwelling pleural catheters. Cureus 2017; 9: e1636. doi: 10.7759/cureus.1636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Davies HE, Rahman NM, Parker RJ, et al. . Use of indwelling pleural catheters for chronic pleural infection. Chest 2008; 133: 546–549. doi: 10.1378/chest.07-1742 [DOI] [PubMed] [Google Scholar]
- 119.Subotic D, Lardinois D, Hojski A. Minimally invasive thoracic surgery for empyema. Breathe 2018; 14: 302–310. doi: 10.1183/20734735.025718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Fitzgerald DB, Waterer GW, Budgeon C, et al. . Steroid Therapy and Outcome of Parapneumonic Pleural Effusions (STOPPE): a pilot randomized clinical trial. Am J Respir Crit Care Med 2022; 205: 1093–1101. doi: 10.1164/rccm.202107-1600OC [DOI] [PubMed] [Google Scholar]
- 121.Porcel JM. PILOTing towards a RAPID predictor of mortality for infectious pleural effusions. Eur Respir J 2020; 56: 2002425. doi: 10.1183/13993003.02425-2020 [DOI] [PubMed] [Google Scholar]


