Abstract
BACKGROUND:
Tracking surgical complications and unplanned healthcare utilization is essential to inform quality initiatives in aesthetic surgery. This study utilized the Tracking Operations and Outcomes for Plastic Surgeons (TOPS) database to characterize rates and predictors of surgical complications and unplanned healthcare utilization across common aesthetic surgery procedures.
METHODS:
The TOPS database was queried for all patients undergoing breast augmentation, liposuction, blepharoplasty, rhinoplasty, and abdominoplasty from 2008–2019. Incidence and risk factors for complications and unplanned readmission, reoperation, and emergency room visits were determined.
RESULTS:
A total of 214,504 patients were identified. Overall, 94,618 breast augmentations, 56,756 liposuction procedures, 29,797 blepharoplasties, 24,946 abdominoplasties, and 8,387 rhinoplasties were included. A low incidence of peri-operative complications was found, including seroma (1.1%), hematoma (0.7%), superficial wound complication (0.9%), deep surgical site infection (0.2%), need for need for blood transfusion (0.05%), and DVT/PE (0.1%). Incidence of unplanned readmission, emergency room visits, and reoperation were 0.34%, 0.25%, and 0.80%, respectively. Patients who underwent an abdominoplasty more commonly presented to the emergency room and had unplanned readmissions or reoperations compared to other studied procedures. Furthermore, an increased age, diabetes, higher BMI, ASA class, longer operative times, and pursuit of combined aesthetic procedures were associated with increased risk for unplanned healthcare utilization.
CONCLUSIONS:
There is a low incidence of perioperative complications and unplanned healthcare utilization following common aesthetic surgery procedures. Continued entry into large national databases in aesthetic surgery is essential for internal benchmarking and quality improvement.
INTRODUCTION
Tracking surgical outcomes, including post-operative complications and unplanned hospital readmissions, is essential to promote informed decision-making and quality improvement efforts across surgical subspecialties.1,2 Tracking outcomes is particularly relevant in aesthetic plastic surgery, where the elective nature of procedures and reliance on patient satisfaction make transparency of surgical outcomes an important benchmarking tool.3,4 According to the American Society for Plastic Surgeons (ASPS), over eighteen million aesthetic procedures were performed in 2019, a statistic that has continued to grow over the past decade.5
Despite a need for granular complications and readmissions data in aesthetic surgery, published studies are limited in their retrospective, single-center designs. To date, the incorporation of aesthetic surgery data into national databases has been limited. The Tracking Operations and Outcomes for Plastic Surgeons (TOPS) database was established to provide a source of national data on aesthetic surgery outcomes with participation from surgeons across the United States.6–12 While limited by reliance on surgeon entry and variable participation, the TOPS database represents one of the largest sources of aesthetic surgery outcomes with unique representation of the private practice aesthetic surgery population. In addition, TOPS has been shown to have comparable reporting of surgical complications compared to the National Surgical Quality Improvement Program (NSQIP)9 and CosmetAssure.13,14
Given the relative paucity of large national data on surgical complications and unplanned healthcare utilization in aesthetic surgery, the aim of this study was to utilize the TOPS database to characterize rates and predictors of surgical complications and unplanned healthcare utilization including readmissions, emergency room visits, and returns to the operating room across common aesthetic plastic surgery procedures.
METHODS
After Institutional Review Board approval, the TOPS database was queried for all adult patients undergoing aesthetic plastic surgery procedures from 2008–2019. De-identified data was collected for patients undergoing the top five most common aesthetic surgery procedures as defined by 2019 ASPS statistics,5 including [1] breast augmentation, [2] liposuction, [3] rhinoplasty, [4] blepharoplasty, and [5] abdominoplasty.
Demographics collected included age, race/ethnicity, gender, body mass index (BMI), and comorbidities including tobacco use, diabetes mellites (DM), and American Society of Anesthesiologists (ASA) status. Practice characteristics examined included facility type, operative time, anesthetic provider and facility type, and the occurrence of more than one procedure within a single operation. Unplanned healthcare utilization was defined as unplanned hospital readmissions, unplanned emergency room (ER) visits, and unplanned returns to the operating room within 30 days of the index procedure. Perioperative complications examined included hematoma, seroma, wound disruption, surgical site infection (SSI), need for intravenous (IV) or oral (PO) antibiotics, implant loss (for breast augmentation), blood transfusion, and deep vein thrombosis (DVT) or pulmonary embolism (PE) within 30 days. Combined procedures identified as procedures recorded on the same date with the same surgeon ID in TOPS. Given that procedure logs in TOPS are entered for individual procedures and corresponding CPT codes, complications for combined procedures were recorded under the CPT code in which they were initially reported. All duplicates in TOPS were deleted, and variables with a high degree of missingness were excluded from the analysis. Operative times below 30 minutes or above 10 hours were regarded as invalid.
Outcomes of Interest
The primary outcome of interest was the incidence of unplanned healthcare utilization and surgical complications across common aesthetic procedures. Secondary outcomes included demographic and surgical factors associated with risk of unplanned emergency room visits, unplanned returns to the operating room, and unplanned readmissions across procedures. Finally, relative per-year reporting of selected procedures within the TOPS database was calculated.
Statistical Analysis
Patient characteristics were summarized using mean and standard deviation (SD) or frequency and percentage for continuous and categorical measures, respectively. Multivariate logistic regression was used to identify predictors of unplanned emergency room visits, hospital readmissions, and unplanned returns to the operating room. Selection of independent variables was based on their importance and relevance to the outcomes. P-values less than 0.05 were considered statistically significant. Analyses were conducted using R (R Foundation for Statistical Computing, Vienna, Austria), Microsoft Excel and Microsoft Access.
RESULTS
A total of 214,504 procedures were identified in the TOPS database from 2008–2019, including 94,618 breast augmentations, 56,756 liposuction procedures, 29,797 blepharoplasties, 8,387 rhinoplasties, and 24,946 abdominoplasties. Patient characteristics by procedure type are shown in Table 1. Briefly, the majority (93.8%) of patients were female with a mean age of 41.3 years and mean BMI of 24.5 kg/m2. Comparing demographic characteristics across procedures, the highest proportion of a male patient population was seen in rhinoplasties (21.4%) and blepharoplasties (14.8%). On average, a younger patient population was found to undergo rhinoplasty (32.3 years) and breast augmentation (36.0 years), and BMI was higher among those undergoing liposuction (27.0 kg/m2) and abdominoplasty (27.0 kg/m2) compared to other studied procedures. The majority of patients were ASA Class 1 (53.7%), with medical comorbidities relatively uncommon across the patient population including current tobacco use (6.0%) and diabetes mellitus type 2 (1.1%), Table 1.
Table 1.
Demographic characteristics across procedures.
| All Procedures (n=214,504) |
Breast Augmentation (n=94,618) |
Liposuction (n=56,756) |
Blepharoplasty (n=29,797) |
Rhinoplasty (n=8,387) |
Abdominoplasty (n=24,946) | |
|---|---|---|---|---|---|---|
| Age (mean, SD) (years) | 41.3 (13.6) | 36.0 (11.4) | 43.1 (12.0) | 55.8 (11.9) | 32.3 (14.6) | 42.9 (11.0) |
| Gender, n (%) | ||||||
| Female | 201,306 (93.8%) | 94,174 (99.5%) | 51,131 (90.1%) | 25,397 (85.2%) | 6,594 (78.6%) | 24,010 (96.2%) |
| Male | 13,195 (6.2%) | 443 (0.5%) | 5,624 (0.9%) | 4,400 (14.8%) | 1,792 (21.4%) | 936 (3.8) |
| Missing | 3 (0.0%) | 1 (0.0%) | 1 (0.0%) | 0 (0.0%) | 1 (0.0%) | 0 (0.0%) |
| Race/Ethnicity, n (%) | ||||||
| White/Caucasian | 161,404 (75.3%) | 74,313 (78.5%) | 40,537 (71.4%) | 22,793 (76.5%) | 5,654 (67.4%) | 18,107 (72.6%) |
| Black/African American | 8,463 (4.0%) | 2,149 (2.3%) | 4,058 (7.2%) | 304 (1.0%) | 190 (2.3%) | 1,762 (7.1%) |
| Asian | 8,319 (3.4%) | 2,751 (2.8%) | 2,572 (2.8%) | 3,074 (10.3%) | 467 (5.6%) | 455 (1.8%) |
| Hispanic/Latino | 17,542 (8.2%) | 7,797 (8.2%) | 5,096 (9.0%) | 1,145 (3.8%) | 834 (9.9%) | 2,670 (10.7%) |
| Other/Unknown | 19,473 (9.1%) | 7,959 (8.4%) | 5,686 (10.0%) | 2,515 (8.4%) | 1,268 (15.1%) | 2,045 (8.2%) |
| BMI (kg/m2, mean) | 24.5 (SD=5.1, n=151,277) | 22.5 (SD=3.9, n=69,964) | 27.0 (SD=5.3, n=38,415) | 24.9 (SD=5.0, n=18,870) | 22.6 (SD=4.3, n=5,256) | 27.0 (SD=5.3, n=18,772) |
| Insurance Status, n (%) | ||||||
| Private insurance | 11,627 (5.4%) | 2,766 (2.9%) | 3,012 (5.3%) | 2,810 (9.4%) | 1,017 (12.1%) | 2,022 (8.1%) |
| Medicaid | 313 (0.2%) | 62 (0.1%) | 37 (0.1%) | 19 (0.1%) | 108 (1.3%) | 87 (0.4%) |
| Medicare | 1,344 (0.6%) | 353 (0.4%) | 89 (0.2%) | 693 (2.3%) | 33 (0.4%) | 176 (0.7%) |
| Self-pay | 155,919 (72.7%) | 70,622 (74.6%) | 40,943 (72.1%) | 20,415 (68.5%) | 5,187 (61.9%) | 18,752 (75.2%) |
| Worker’s comp | 42 (0.0%) | 12 (0.0%) | 9 (0.0%) | 1 (0.0%) | 17 (0.2%) | 3 (0.0%) |
| Other | 2,602 (1.2%) | 1,373 (1.5%) | 668 (1.2%) | 235 (0.8%) | 109 (1.3%) | 217 (0.9%) |
| Missing/Unknown | 47,735 (22.4%) | 20,494 (21.7%) | 13,244 (23.3%) | 6,884 (23.1%) | 2,224 (26.5%) | 4,889 (19.6%) |
| Tobacco use, n (%) | ||||||
| Current Tobacco User | 12,831 (6.0%) | 7,792 (8.2%) | 2,314 (4.0%) | 1,358 (4.6%) | 310 (3.7%) | 1,057 (4.2%) |
| Former Tobacco User | 11,618 (5.4%) | 4,735 (5.0%) | 3,038 (5.4%) | 1,821 (6.1%) | 229 (2.7%) | 1,795 (7.2%) |
| Non-tobacco User | 133,173 (62.1.5%) | 58,843 (62.2%) | 34,477 (60.7%) | 17,682 (59.3%) | 5,184 (61.8%) | 16,987 (68.1%) |
| Missing/Unknown | 56,882 (26.5%) | 23,248 (24.6%) | 16,927 (29.8%) | 8,936 (30.0%) | 2,664 (31.8%) | 5,107 (20.5%) |
| DM2, n (%) | ||||||
| No | 148,601 (69.3%) | 67,855 (71.7%) | 37,693 (66.4%) | 19,176 (64.4%) | 5,391 (64.3%) | 18,486 (74.1%) |
| Yes | 2,363 (1.1%) | 461 (0.5%) | 682 (1.2%) | 658 (2.2%) | 26 (0.3%) | 536 (2.1%) |
| Missing/Unknown | 63,540 (29.6%) | 26,302 (27.8%) | 18,381 (32.4%) | 9,963 (33.4%) | 2,970 (35.4%) | 5,924 (23.7%) |
| ASA status, n (%) | ||||||
| 1 | 115,218 (53.7%) | 56,552 (59.8%) | 27,556 (48.6%) | 13,649 (45.8%) | 4,826 (57.5%) | 12635 (50.6%) |
| 2 | 42,629 (19.9%) | 14,410 (15.2%) | 13,460 (23.7%) | 7,093 (23.8%) | 997 (11.9%) | 6,669 (26.7%) |
| 3 | 1,985 (0.9%) | 412 (0.4%) | 569 (1.0%) | 592 (2.0%) | 36 (0.4%) | 376 (15.1%) |
| Other/Unknown | 54,672 (25.5%) | 23,244 (24.6^) | 15,171 (26.7%) | 8,463 (28.4%) | 2,528 (30.1%) | 5,264 (21.1%) |
Facility, anesthesia, and surgical characteristics across procedure types are shown in Table 2. The majority of procedures were performed in an office or office-based surgery facility (45.9%) or an ambulatory surgery center (33.0%). Among the 18.6% of procedures performed at an acute care hospital, rhinoplasty (25.9%) and abdominoplasty (28.5%) were identified to be most common. Anesthesia was most commonly performed by an anesthesiologist (44.2%) or CRNA (39.4%), with general anesthesia performed in 77.2% of cases. The majority of cases were outpatient procedures (93.2%), with inpatient admissions most common for abdominoplasty (11.4%) and rhinoplasty (6.5%). Mean operative time was longer in abdominoplasty (201 minutes) and liposuction (170 minutes) procedures compared to blepharoplasty (157 minutes), rhinoplasty (145 minutes), and breast augmentation (99 minutes), Table 2.
Table 2.
Facility, anesthesia, and surgical characteristics across procedures.
| All Procedures (n=214,504) |
Breast Augmentation (n=94,618) |
Liposuction (n=56,756) |
Blepharoplasty (n=29,797) |
Rhinoplasty (n=8,387) |
Abdominoplasty (n=24,946) |
|
|---|---|---|---|---|---|---|
| Facility Type, n (%) | ||||||
| Acute care (Hospital) | 39,884 (18.6%) | 15,866 (16.8%) | 9,726 (17.1%) | 5,016 (16.8%) | 2,171 (25.9%) | 7,105 (28.5%) |
| Ambulatory surgery center | 70,821 (33.0%) | 34,207 (36.2%) | 17,325 (30.5%) | 8,675 (29.1%) | 2,546 (30.4%) | 8,068 (32.3%) |
| Office / Office-based surgery facility | 98,468 (45.9%) | 42,177 (44.6%) | 28,261 (49.8%) | 15,328 (51.4%) | 3,516 (41.9%) | 9,186 (36.8%) |
| Missing/Unknown | 5,331 (2.5%) | 2,368 (2.5%) | 1,444 (2.5%) | 778 (2.6%) | 154 (1.8%) | 587 (2.4%) |
| Operative time, mean (SD) (min) | 134.0 (94.0) | 98.7 (71.9) | 170.0 (93.0) | 156.7 (108.3) | 144.6 (80.9) | 200.5 (87.8) |
| Anesthesia provider, n (%) | ||||||
| Anesthesiologist | 94,886 (44.2%) | 43,105 (45.6%) | 23,562 (41.5%) | 11,871 (39.8%) | 4,477 (53.4%) | 11,871 (47.6%) |
| CRNA | 84,485 (39.4%) | 42,325 (44.7%) | 19,834 (34.9%) | 8,563 (28.7%) | 2,573 (30.7%) | 11,190 (44.9%) |
| Procedural surgeon | 16,137 (7.5%) | 3,836 (4.1%) | 6,362 (11.2%) | 5,068 (17.0%) | 444 (5.3%) | 427 (1.7%) |
| RN | 7,299 (3.4%) | 1,380 (1.5%) | 2,923 (5.1%) | 2,311 (7.8%) | 223 (2.7%) | 462 (1.9%) |
| Other/Unknown | 11,697 (5.45%) | 3,972 (4.2%) | 4,075 (7.2%) | 1,984 (6.7%) | 670 (8.0%) | 996 (4.0%) |
| Anesthesia type, n (%) | ||||||
| Conscious sedation | 14,150 (6.6%) | 4,389 (4.6%) | 4,305 (7.6%) | 4,192 (14.1%) | 396 (4.7%) | 868 (3.5%) |
| General | 165,487 (77.2%) | 79,602 (84.1%) | 41,049 (72.3%) | 15,528 (52.1%) | 6,743 (80.4%) | 22,565 (90.5%) |
| MAC | 14,592 (6.8%) | 6,164 (6.5%) | 3,222 (5.7%) | 4,202 (14.1%) | 470 (5.6%) | 534 (2.1%) |
| Anesthetic block | 1,204 (0.6%) | 663 (0.7%) | 171 (0.3%) | 209 (0.7%) | 36 (0.4%) | 125 (0.5%) |
| Tumescent | 21,548 (10.1%) | 2,103 (2.2%) | 15,693 (27.7%) | 874 (2.9%) | 69 (0.8%) | 2,809 (11.3%) |
| Other/Unknown | 16,960 (7.9%) | 5,069 (5.4%) | 4,231 (7.5%) | 5,849 (19.6%) | 800 (9.5%) | 1,011 (4.1%) |
| Admission type, n (%) | ||||||
| Outpatient | 199,833 (93.2%) | 90,029 (95.1%) | 52,733 (92.9%) | 27,981 (93.9%) | 7,663 (91.4%) | 21,427 (86.0%) |
| Inpatient | 8,721 (4.1%) | 2,007 (2.1%) | 2,376 (4.2%) | 943 (3.2%) | 544 (6.5%) | 2,851 (11.4%) |
| Missing/Unknown | 5,950 (2.8%) | 2,582 (2.7%) | 1,647 (2.9%) | 873 (2.9%) | 180 (2.1%) | 668 (2.7%) |
Incidence of 30-day Post-Operative Complications and Unplanned Healthcare Utilization
Incidence of post-operative complications across procedure types is shown in Table 3. Overall, incidence of complications was low across procedure types, with a low overall incidence of seroma (n=2,444, 1.1%), hematoma (n=1,522, 0.7%), superficial wound complication (n=1,960, 0.9%), deep wound complication (n=403, 0.2%), superficial surgical site infection (n=665, 0.3%), deep surgical site infection (n=415, 0.2%), need for IV (n=353, 0.2%) or PO antibiotics (n=2,127, 1.0%), need for blood transfusion (n=103, 0.05%), and occurrence of a DVT/PE (n=258, 0.1%). Among patients undergoing breast augmentation, risk of implant loss was 0.2% (n=211). Comparing procedures, abdominoplasty was associated with the highest incidence of complications, though this incidence was <5% for all complications including seroma (n=1,010, 4.1%), hematoma (n=252, 1.0%), superficial wound complication (n=785, 3.2%), deep wound complication (n=185, 0.7%), superficial surgical site infection (n= 224, 0.9%), deep surgical site infection (n=141, 0.6%), need for IV (n=115, 0.5%) or PO antibiotics (n=690, 2.8%), need for blood transfusion (n=47, 0.2%), and DVT/PE (n=125, 0.5%). Unplanned healthcare utilization is shown in Table 3, with an overall low incidence including unplanned hospital admissions (n=728, 0.34%), unplanned emergency room visits (n=544, 0.25%), and unplanned returns to the operating room (n=1,725, 0.80%). Comparing procedure types, incidence of unplanned hospital admission, ER visit, and return to the operating room was highest after abdominoplasty (incidences 1.2%, 0.8%, and 1.4%, respectively), Table 3.
Table 3.
Complication incidence across procedures.
| All Procedures (n=214,504) |
Breast Augmentation (n=94,618) |
Liposuction (n=56,756) |
Blepharoplasty (n=29,797) |
Rhinoplasty (n=8,387) |
Abdominoplasty (n=24,946) |
|
|---|---|---|---|---|---|---|
| Seroma, n (%) | 2,444 (1.1%) | 317 (0.3%) | 1,030 (1.8%) | 82 (0.3%) | 5 (0.06%) | 1,010 (4.1%) |
| Hematoma, n (%) | 1,522 (0.7%) | 779 (0.8%) | 246 (0.4%) | 232 (0.8%) | 13 (0.2%) | 252 (1.0%) |
| Superficial wound disruption, n (%) | 1,960 (0.9%) | 445 (0.5%) | 607 (1.1%) | 117 (0.4%) | 6 (0.1%) | 785 (3.2%) |
| Deep wound disruption, n (%) | 403 (0.2%) | 83 (0.1%) | 123 (0.2%) | 6 (0.02%) | 6 (0.07%) | 185 (0.7%) |
| Superficial SSI, n (%) | 665 (0.3%) | 134 (0.1%) | 234 (0.4%) | 56 (0.2%) | 17 (0.2%) | 224 (0.9%) |
| Deep SSI, n (%) | 415 (0.2%) | 108 (0.1%) | 146 (0.3%) | 12 (0.04%) | 8 (0.1%) | 141 (0.6%) |
| Need for IV Antibiotics, n (%) | 353 (0.2%) | 105 (0.1%) | 118 (0.2%) | 11 (0.04%) | 4 (0.05%) | 115 (0.5%) |
| Need for PO antibiotics, n (%) | 2,127 (1.0%) | 575 (0.6%) | 696 (1.2%) | 124 (0.4%) | 42 (0.5%) | 690 (2.8%) |
| Implant loss, n (%) | N/A | 211 (0.2%) | N/A | N/A | N/A | N/A |
| Need for blood transfusion, n (%) | 103 (0.05%) | 11 (0.01%) | 45 (0.08%) | 0 (0.0%) | 0 (0.0%) | 47 (0.2%) |
| DVT or Pulmonary embolism, n (%) | 258 (0.1%) | 26 (0.03%) | 97 (0.2%) | 8 (0.03%) | 2 (0.02%) | 125 (0.5%) |
| Unplanned hospital admission, n (%) | 728 (0.34%) | 147 (0.16%) | 248 (0.44%) | 33 (0.11%) | 9 (0.11%) | 291 (1.2%) |
| Unplanned ER visit, n (%) | 544 (0.25%) | 123 (0.13%) | 191 (0.34%) | 18 (0.06%) | 4 (0.048%) | 208 (0.83%) |
| Unplanned OR return, n (%) | 1,725 (0.80%) | 903 (0.95%) | 275 (0.48%) | 172 (0.58%) | 21 (0.25%) | 354 (1.42%) |
Risk Factors for Unplanned ER Visits
Risk factors for unplanned ER visits are shown in Table 4. After multivariate adjustment, independent risk factors for unplanned ER visits included higher BMI [Odds Ratio (OR) 1.06; 95% confidence interval (CI) 1.06–1.10; p=0.001], Black/African American race (vs. White) (OR 1.52; 95% CI 1.07–2.10; p=0.015), ASA class 2 (OR 1.97; 95% CI 1.58–2.45; p<0.001) or 3 (OR 2.94; 95% CI 1.67–4.90; p<0.001) statuses (vs. ASA class 1), increasing operative time (OR=1.0016; 95% CI 1.0004–1.0026; p=0.006), surgery at an acute care hospital (vs. office-based surgery facility) (OR 1.58; 95% CI 1.23–2.02; p<0.001), pursuit of abdominoplasty (vs. breast augmentation) (OR 2.52; 95% CI 1.86–3.44; p<0.001), and pursuit of a combined aesthetic procedure (OR 1.69; 95% CI 1.34–2.12; p<0.001). Pursuit of blepharoplasty (vs. breast augmentation) (OR 0.20; 95% CI 0.04–0.81; p<0.001) was associated with lower risk. Hosmer-Lemeshow test p-value is 0.520, greater than 0.05, indicating no evidence of poor fit of the regression model.
Table 4.
Multivariate logistic regression model assessing predictors of unplanned ER visits, unplanned hospital admissions, and unplanned returns to the operating room after breast augmentation, liposuction, rhinoplasty, blepharoplasty, and abdominoplasty.
| Unplanned ER Visit | Unplanned Hospital Admission | Unplanned Return to OR | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age | 1.00 (0.99 – 1.01) | 0.923 | 1.02 (1.01 – 1.03) | <0.001 | 1.01 (1.00 – 1.01) | 0.015 |
| BMI | 1.06 (1.04 – 1.08) | <0.001 | 1.08 (1.06 – 1.10) | <0.001 | 1.02 (1.01 – 1.03) | 0.001 |
| Race/ethnicity | ||||||
| White (reference level) | ||||||
| Asian | 0.39 (0.10 – 1.04) | 0.110 | 1.14 (0.54 – 2.10) | 0.695 | 0.68 (0.43 – 1.01) | 0.074 |
| Hispanic/Latino | 0.72 (0.47 – 1.05) | 0.100 | 0.62 (0.41 – 0.91) | 0.019 | 0.76 (0.60 – 0.95) | 0.019 |
| Black/African American | 1.52 (1.07 – 2.10) | 0.015 | 1.20 (0.85 – 1.65) | 0.280 | 0.87 (0.64 – 1.16) | 0.354 |
| Tobacco use | ||||||
| Non-tobacco User (reference level) | ||||||
| Former Tobacco User | 1.11 (0.79 – 1.50) | 0.537 | 1.14 (0.86 – 1.49) | 0.334 | 1.33 (1.10 – 1.59) | 0.002 |
| Current Tobacco User | 0.64 (0.39 – 0.99) | 0.061 | 0.75 (0.48 – 1.12) | 0.182 | 1.21 (0.99 – 1.46) | 0.054 |
| ASA status | ||||||
| 1(reference level) | ||||||
| 2 | 1.97 (1.58 – 2.45) | <0.001 | 1.79 (1.47 – 2.17) | <0.001 | 1.54 (1.35 – 1.75) | <0.001 |
| Greater than or equal to 3 | 2.94 (1.67 – 4.90) | <0.001 | 1.65 (1.00 – 2.63) | 0.042 | 1.20 (0.74 – 1.86) | 0.424 |
| DM2 (Yes) | 1.29 (0.74 – 2.10) | 0.334 | 1.83 (1.24 – 2.64) | 0.002 | 1.33 (0.91 – 1.87) | 0.120 |
| Operative time | 1.002 (1.0004–1.003) | 0.006 | 1.004 (1.003–1.005) | <0.001 | OR 1.003(1.002–1.004) | <0.001 |
| Facility type | ||||||
| Office-Based Surgery Facility (reference level) | ||||||
| Ambulatory Surgery Center | 1.02 (0.80 – 1.29) | 0.884 | 1.13 (0.90 – 1.42) | 0.281 | 0.92 (0.81 – 1.05) | 0.220 |
| Acute Care (Hospital) | 1.58 (1.23 – 2.02) | <0.001 | 2.16 (1.73 – 2.69) | <0.001 | 1.02 (0.88 – 1.19) | 0.765 |
| Procedure type | ||||||
| Breast Augmentation (reference level) | ||||||
| Liposuction | 1.22 (0.90 – 1.67) | 0.201 | 1.13 (0.85 – 1.52) | 0.392 | 0.36 (0.30 – 0.43) | <0.001 |
| Blepharoplasty | 0.20 (0.10 – 0.39) | <0.001 | 0.33 (0.20 – 0.52) | <0.001 | 0.41 (0.32 – 0.51) | <0.001 |
| Rhinoplasty | 0.25 (0.04 – 0.81) | 0.056 | 0.57 (0.20 – 1.26) | 0.220 | 0.21 (0.11 – 0.36) | <0.001 |
| Abdominoplasty | 2.52 (1.86 – 3.44) | <0.001 | 2.45 (1.86 – 3.25) | <0.001 | 0.92 (0.77 – 1.08) | 0.312 |
| More than 1 types of procedure (Yes) | 1.69 (1.34 – 2.12) | <0.001 | 1.28 (1.04 – 1.56) | 0.017 | 0.83 (0.72 – 0.96) | 0.013 |
Risk Factors for Unplanned Readmission
Risk factors for unplanned readmission are also shown in Table 4. After multivariate adjustment, independent risk factors for unplanned readmission after studied procedures included age (OR 1.02; 95% CI 1.01–1.03; p<0.001), BMI (OR 1.08; 95% CI 1.06–1.10), ASA class 2 (OR 1.79; 95% CI 1.47–2.17; p<0.001) status (vs. ASA class 1), ASA class 3 (OR 1.65; 95% CI 1.00–2.63; p=0.042) status (vs. ASA class 1), diabetes mellites (OR 1.83; 95% CI 1.24–2.64; p=0.002), increasing operative time (OR 1.004; 95% CI 1.003–1.005; p<0.001), surgery at an acute care hospital (OR 2.16; 95% CI 1.73–2.69; p<0.001), pursuit of abdominoplasty (vs. breast augmentation) (OR 2.45; 95% CI 1.86–3.25; p<0.001), and pursuit of a combined aesthetic procedure (OR 1.28; 95% CI 1.04–1.56; p=0.017). Hosmer-Lemeshow test p-value is 0.109, greater than 0.05, indicating no evidence of poor fit of the regression model.
Risk Factors for Unplanned Reoperation
Risk factors for unplanned reoperation are also shown in Table 4. After multivariate adjustment, independent risk factors for unplanned reoperation included increasing age (OR 1.01; 95% CI 1.00–1.01; p=0.015), BMI (OR 1.02; 95% CI 1.01–1.03; p=0.001), former tobacco user (OR 1.33, 95% CI 1.10–1.59; p=0.002), ASA class 2 (OR 1.54; 95% CI 1.35–1.75; p<0.001) status (vs. ASA class 1) and increasing operative time (OR 1.0032; 95% CI 1.0025–1.0038; p<0.001). Hosmer-Lemeshow test p-value is 0.194, greater than 0.05, indicating no evidence of poor fit of the regression model.
Per-Year Reporting in TOPS
Finally, we examined trends in per-year reporting of all procedures (breast augmentation, liposuction, blepharoplasty, rhinoplasty, and abdominoplasty) in the TOPS database. While reporting of blepharoplasty, abdominoplasty, and rhinoplasty remained stable in TOPS from 2008–2019, relative per-year reporting of breast augmentation decreased, Figure 1.
Figure 1.
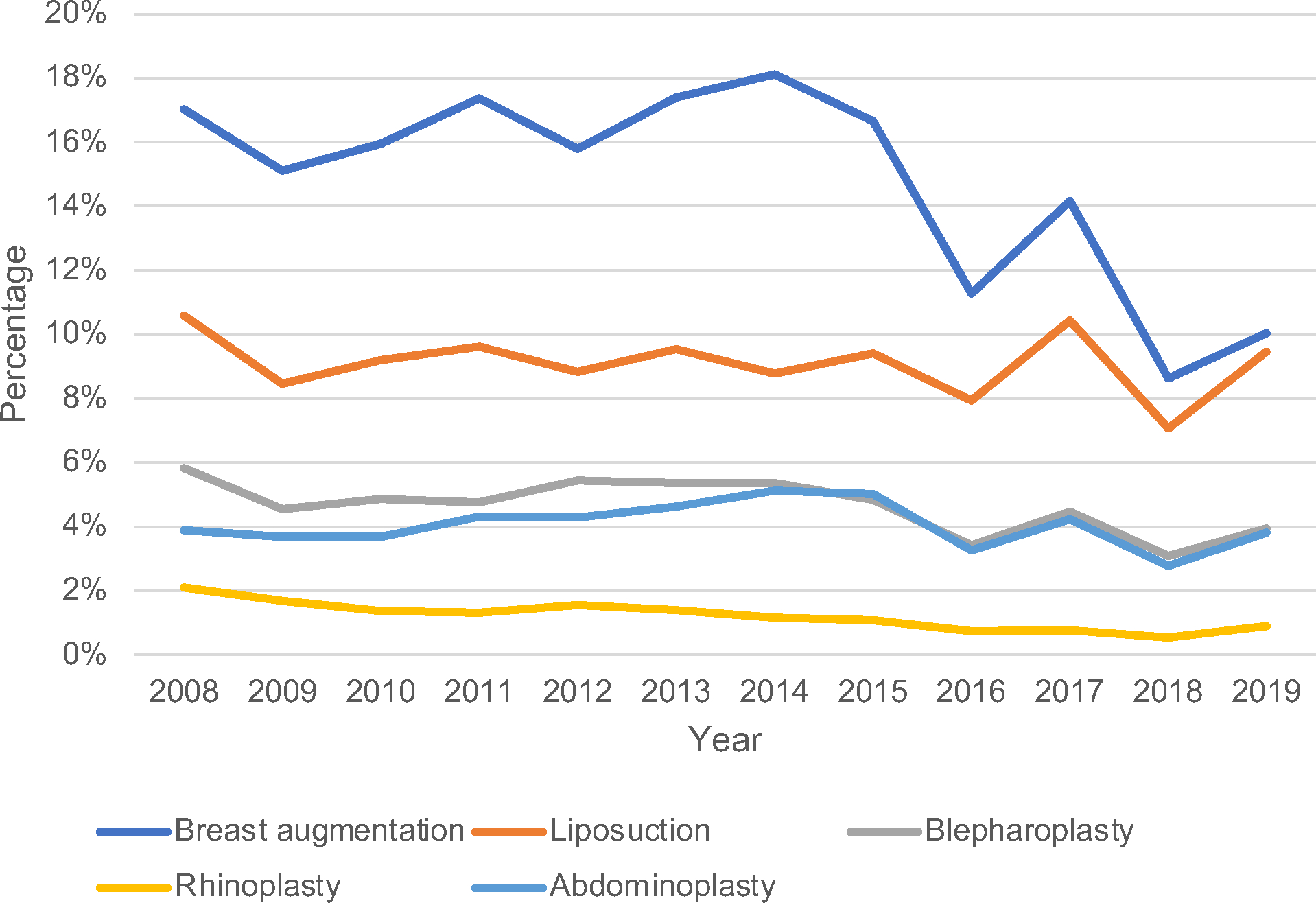
Trends in per-year breast augmentation, liposuction, blepharoplasty, rhinoplasty, and abdominoplasty as reported in TOPS, 2008–2019.
DISCUSSION
In this large contemporary analysis of surgical outcomes in the TOPS database for 214,504 patients undergoing common aesthetic surgery procedures, we report the incidence of surgical complications as well as demographic and procedural risk factors for readmission and unplanned reoperation. We identify an overall low complication rate associated with five of the most common aesthetic surgery procedures as reported in TOPS. Furthermore, we identify demographic and procedural predictors of unplanned readmission, emergency room visits, and reoperation across procedure types. We aim for this study to emphasize the overall safety of aesthetic surgery when performed by board-certified plastic surgeons, and also to identify demographic subgroups at risk for unplanned healthcare utilization who may benefit from additional planning, optimization, and counseling in the pre-operative setting.
To date, the incorporation of the aesthetic surgery population into large national databases has been limited. Existing reviews of complications data are limited to retrospective reviews15 as well as the CosmetAssure insurance database.6,14,16–26 To address this gap, the TOPS database was established in 2002 to serve as a benchmarking and advocacy tool for plastic surgeons, and currently contains data from over one million plastic surgery procedures manually entered by plastic surgeons spanning practice types and geographic regions.27 TOPS has been shown to have similar reported complication rates to both CosmetAssure14 and NSQIP.8 Additionally, TOPS contains a larger cosmetic surgery patient population with a higher proportion of procedures performed via office-based surgery (15.9%26 in CosmetAssure vs. 46.6% in TOPS in our study). Thus, the patient population available in TOPS makes the database a unique national internal benchmarking tool for elective aesthetic surgery outcomes.
The low overall complication rate identified in our study highlights the safety of the most common aesthetic plastic surgery procedures when performed by board-certified plastic surgeons. We identify a <2% overall incidence of all complications including hematoma, seroma, wound complications, infection, and thrombotic events across procedures. This data parallels complication rates identified in both CosmetAssure14,16,17,19,21–23,26,28, NSQIP8, and internal state databases29 and emphasizes the overall safety of elective aesthetic surgery. Compared to breast augmentation, liposuction, blepharoplasty, and rhinoplasty, we do identify a higher complication rate with abdominoplasty across studied complications, a trend which has been previously reported in both CosmetAssure and NSQIP when comparing abdominoplasty to other aesthetic procedures.16,30 This highlights a need for appropriate pre-operative patient selection and post-operative monitoring for patients seeking abdominoplasty compared to other aesthetic procedures, especially when performed as a combined procedure.
With recent shifts in healthcare dynamics, unplanned healthcare utilization, including unplanned readmission, emergency room visits, and reoperation, have become proxies of care and quality metrics by which healthcare systems and surgeons are judged. As such, increasing emphasis has been placed on initiatives to improve these metrics across surgical patient populations. Likely attributable to the preponderance of self-pay patients and relative infrequency of unplanned healthcare utilization in aesthetic surgery, few studies have reported risk factors for readmission, emergency room visits, and reoperation after aesthetic surgery.2,31 These events remain costly and important targets for quality improvement within the specialty. Studies in other surgical specialties have estimated cost of unplanned post-operative ER visits to exceed $1900 and readmission costs to exceed $7300 after elective surgery.32 In our study, we identify an overall <1% incidence of unplanned hospital admissions, emergency room visits, and reoperations across the most common aesthetic surgery procedures performed in the United States. This is in line to prior studies estimating plastic surgery readmission rates to range from 0.90% after outpatient aesthetic surgery to 4.5% after inpatient plastic surgery procedures.31,33 Across procedures, readmission rates in the literature have been comparable to ours including 0.23% after breast augmentation in NSQIP2 (compared to 0.15% in our study), 1.13% after liposuction in NSQIP34 (compared to 0.43%), 0.7% after septo-rhinoplasty in the Healthcare Utilization Project (HCUP)35 (compared to 0.11%), and 1.8% after abdominoplasty in NSQIP (1.4% in our study).31
Despite these low overall rates, identifying risk factors for unplanned healthcare utilization remains essential to guide both internal quality improvement and pre-operative counseling. Unsurprisingly, we find that medical comorbidities, including age, diabetes, higher BMI, and higher ASA class are independent risk factors for hospital readmissions, all of which have been reported as risk factors for unplanned healthcare utilization in prior studies across our selected procedures.2,35–37 This data highlights the importance of pre-operative optimization and counseling in this patient population. Furthermore, we report procedural risk factors for overutilization. In line with prior studies,7 higher operative time was associated with risk of hospital admissions and returns to the operating room. In addition, surgery performed at an acute care hospital (compared to office-based surgery) was associated with unplanned readmission, ER visits, and returns to the operating room, a finding which has also been reported and is likely reflective of a more comorbid patient population or surgeon selection bias.16
Additionally, we find that pursuit of abdominoplasty and combination aesthetic procedures were associated with risk of unplanned hospital admissions and ER visits. Abdominoplasty is often performed combined case in conjunction with other aesthetic procedures due to benefits including reduced occurrences of anesthesia, time, and costs. However, prior studies have demonstrated higher overall complication rates associated with combined surgeries involving abdominoplasty. Using CosmetAssure, both Gupta et al.17 and Winocour et al.16 identified a higher overall complication rate associated with combination cases involving abdominoplasty, including hematoma, infection, and venous thromboembolic events.17 Our data further reinforces this increased risk. In concordance with our complications data, pursuit of abdominoplasty was an independent risk factor for unplanned readmission, ER visits, and returns to the operating room when compared to other studied procedures, and pursuit of a combined procedure was an independent risk factor for hospital readmission and ER presentations. This data underscores the necessity of appropriate preoperative risk stratification in patients seeking combined procedures involving abdominoplasty,7,16 especially in those who possess other identified risk factors (obesity, diabetes, or increasing age) for readmission.
There are limitations to this study with implications for its interpretation, many of which are inherent to the design of TOPS database. Notably, TOPS entry is dependent on manual data entry by surgeons, which may result in reporting bias of complications with potential under-reporting of adverse events as opposed to databases such as NSQIP which rely on third party data entry.8 Additionally, TOPS entry is dependent on surgeon participation. While over 700 ASPS members manually enter data in TOPS, this participation may result in variable capture of the aesthetic surgery patient population nationally. Despite this, the TOPS database enables unique capture of private practice aesthetic surgery patients, and our study highlights the safety of aesthetic surgery and identifies risk factors for unplanned healthcare utilization in over 210,000 procedures. Throughout the study period, reporting of all procedures remained relatively stable, and our study also underscores the importance of continued entry into TOPS to enable continued internal review and benchmarking of national outcomes. In addition, by highlighting the TOPS database as a safety reporting tool in aesthetic surgery, we aim to encourage the continued refinement of the database to mitigate problems inherent to self-reporting data entry. Ultimately, we aim for this data to serve as a benchmarking tool to drive quality initiatives to reduce unplanned complications and healthcare utilization across the specialty.
CONCLUSIONS
Post-operative complications and unplanned healthcare utilization are uncommon after breast augmentation, liposuction, blepharoplasty, rhinoplasty, and abdominoplasty. However, medical comorbidities including obesity and diabetes are associated with a higher risk of unplanned healthcare utilization. Additionally, abdominoplasty is associated with a higher risk of unplanned ER visits, readmission, and reoperation compared to other aesthetic procedures, a risk which is compounded when performed as a combined procedure. This data emphasizes the overall safety of aesthetic surgery when performed by board-certified plastic surgeons, but also identifies subgroups of aesthetic surgery patients at risk for unplanned healthcare utilization who may benefit from additional planning, optimization, and counseling in the pre-operative setting. Continued entry of aesthetic surgery patients in large national databases is essential for internal benchmarking within the specialty.
Acknowledgement:
The authors would like to acknowledge the Tracking Operations and Outcomes for Plastic Surgeons (TOPS) American Society of Plastic Surgeons Committee for study support. In addition, the authors would like to acknowledge Shen Yin for prior statistical support.
Footnotes
Financial Disclosure Statement: The authors have no relevant financial disclosures.
REFERENCES
- 1.Sinno H, Dionisopoulos T, Slavin SA, Ibrahim AM, Chung KC, Lin SJ. The utility of outcome studies in plastic surgery. Plast Reconstr Surg Glob Open. 2014;2(7):e189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mioton LM, Buck DW 2nd, Rambachan A, Ver Halen JGA, Kim JY. Predictors of readmission after outpatient plastic surgery. Plast Reconstr Surg. 2014;133(1):173–180. [DOI] [PubMed] [Google Scholar]
- 3.Keyes GR, Singer R, Iverson RE, et al. Analysis of outpatient surgery center safety using an internet-based quality improvement and peer review program. Plast Reconstr Surg. 2004;113(6):1760–1770. [DOI] [PubMed] [Google Scholar]
- 4.Keyes GR, Singer R, Iverson RE, et al. Mortality in outpatient surgery. Plast Reconstr Surg. 2008;122(1):245–250. [DOI] [PubMed] [Google Scholar]
- 5.Surgeons ASoP. 2018 ASPS Procedural Statistics. 2019.
- 6.Alderman AK, Collins ED, Streu R, et al. Benchmarking outcomes in plastic surgery: national complication rates for abdominoplasty and breast augmentation. Plast Reconstr Surg. 2009;124(6):2127–2133. [DOI] [PubMed] [Google Scholar]
- 7.Khavanin N, Jordan SW, Vieira BL, et al. Combining abdominal and cosmetic breast surgery does not increase short-term complication rates: a comparison of each individual procedure and pretreatment risk stratification tool. Aesthet Surg J. 2015;35(8):999–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Veith J, Collier W, Simpson A, et al. A Comparison of Common Plastic Surgery Operations Using the NSQIP and TOPS Databases. Plast Reconstr Surg Glob Open. 2020;8(5):e2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khavanin N, Gutowski KA, Hume KM, et al. The use of patient registries in breast surgery: a comparison of the tracking operations and outcomes for plastic surgeons and national surgical quality improvement program data sets. Ann Plast Surg. 2015;74(2):157–162. [DOI] [PubMed] [Google Scholar]
- 10.Kim JY, Mlodinow AS, Khavanin N, et al. Individualized Risk of Surgical Complications: An Application of the Breast Reconstruction Risk Assessment Score. Plast Reconstr Surg Glob Open. 2015;3(5):e405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chopan M, Samant S, Mast BA. Contemporary Analysis of Rhytidectomy Using the Tracking Operations and Outcomes for Plastic Surgeons Database with 13,346 Patients. Plast Reconstr Surg. 2020;145(6):1402–1408. [DOI] [PubMed] [Google Scholar]
- 12.Matros E, Shamsunder MG, Rubenstein RN, et al. Textured and Smooth Implant Use Reported in the Tracking Operations and Outcomes for Plastic Surgeons Database: Epidemiologic Implications for BIA-ALCL. Plast Reconstr Surg Glob Open. 2021;9(3):e3499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu VZ, Tuggle CT, Au AF. Promise and Limitations of Big Data Research in Plastic Surgery. Ann Plast Surg. 2016;76(4):453–458. [DOI] [PubMed] [Google Scholar]
- 14.Alderman AK, Collins ED, Streu R, et al. Benchmarking outcomes in plastic surgery: national complication rates for abdominoplasty and breast augmentation. Plast Reconstr Surg. 2009;124(6):2127–2133. [DOI] [PubMed] [Google Scholar]
- 15.Rohrich RJ, Mendez BM, Afrooz PN. An Update on the Safety and Efficacy of Outpatient Plastic Surgery: A Review of 26,032 Consecutive Cases. Plast Reconstr Surg. 2018;141(4):902–908. [DOI] [PubMed] [Google Scholar]
- 16.Winocour J, Gupta V, Ramirez JR, Shack RB, Grotting JC, Higdon KK. Abdominoplasty: Risk Factors, Complication Rates, and Safety of Combined Procedures. Plast Reconstr Surg. 2015;136(5):597e–606e. [DOI] [PubMed] [Google Scholar]
- 17.Gupta V, Yeslev M, Winocour J, et al. Aesthetic Breast Surgery and Concomitant Procedures: Incidence and Risk Factors for Major Complications in 73,608 Cases. Aesthet Surg J. 2017;37(5):515–527. [DOI] [PubMed] [Google Scholar]
- 18.Kaoutzanis C, Winocour J, Yeslev M, et al. Aesthetic Surgical Procedures in Men: Major Complications and Associated Risk Factors. Aesthet Surg J. 2018;38(4):429–441. [DOI] [PubMed] [Google Scholar]
- 19.Kaoutzanis C, Winocour J, Gupta V, et al. The Effect of Smoking in the Cosmetic Surgery Population: Analysis of 129,007 Patients. Aesthet Surg J. 2019;39(1):109–119. [DOI] [PubMed] [Google Scholar]
- 20.Hanemann MS Jr., Grotting JC. Evaluation of preoperative risk factors and complication rates in cosmetic breast surgery. Ann Plast Surg. 2010;64(5):537–540. [DOI] [PubMed] [Google Scholar]
- 21.Layliev J, Gupta V, Kaoutzanis C, et al. Incidence and Preoperative Risk Factors for Major Complications in Aesthetic Rhinoplasty: Analysis of 4978 Patients. Aesthet Surg J. 2017;37(7):757–767. [DOI] [PubMed] [Google Scholar]
- 22.Nguyen L, Gupta V, Afshari A, Shack RB, Grotting JC, Higdon KK. Incidence and Risk Factors of Major Complications in Brachioplasty: Analysis of 2,294 Patients. Aesthet Surg J. 2016;36(7):792–803. [DOI] [PubMed] [Google Scholar]
- 23.Gupta V, Winocour J, Rodriguez-Feo C, et al. Safety of Aesthetic Surgery in the Overweight Patient: Analysis of 127,961 Patients. Aesthet Surg J. 2016;36(6):718–729. [DOI] [PubMed] [Google Scholar]
- 24.Yeslev M, Gupta V, Winocour J, Shack RB, Grotting JC, Higdon KK. Safety of Cosmetic Procedures in Elderly and Octogenarian Patients. Aesthet Surg J. 2015;35(7):864–873. [DOI] [PubMed] [Google Scholar]
- 25.Winocour J, Gupta V, Kaoutzanis C, et al. Venous Thromboembolism in the Cosmetic Patient: Analysis of 129,007 Patients. Aesthet Surg J. 2017;37(3):337–349. [DOI] [PubMed] [Google Scholar]
- 26.Gupta V, Parikh R, Nguyen L, et al. Is Office-Based Surgery Safe? Comparing Outcomes of 183,914 Aesthetic Surgical Procedures Across Different Types of Accredited Facilities. Aesthet Surg J. 2017;37(2):226–235. [DOI] [PubMed] [Google Scholar]
- 27.Tracking Operations and Outcomes for Plastic Surgeons (TOPS) American Society for Plastic Surgeons (ASPS); 2019. [Google Scholar]
- 28.Kaoutzanis C, Gupta V, Winocour J, Shack B, Grotting JC, Higdon K. Incidence and Risk Factors for Major Surgical Site Infections in Aesthetic Surgery: Analysis of 129,007 Patients. Aesthet Surg J. 2017;37(1):89–99. [DOI] [PubMed] [Google Scholar]
- 29.Parina R, Chang D, Saad AN, Coe T, Gosman AA. Quality and safety outcomes of ambulatory plastic surgery facilities in California. Plast Reconstr Surg. 2015;135(3):791–797. [DOI] [PubMed] [Google Scholar]
- 30.Vu MM, Ellis MF, Blough JT, Gutowski KA, Kim JYS. Development and Internal Validation of the Abdominoplasty Risk Calculator. Plast Reconstr Surg. 2018;141(1):34e–45e. [DOI] [PubMed] [Google Scholar]
- 31.Mioton LM, Alghoul MS, Kim JY. A comparative analysis of readmission rates after outpatient cosmetic surgery. Aesthet Surg J. 2014;34(2):317–323. [DOI] [PubMed] [Google Scholar]
- 32.Wiley MR, Carreon LY, Djurasovic M, et al. Economic analysis of 90-day return to the emergency room and readmission after elective lumbar spine surgery: a single-center analysis of 5444 patients. J Neurosurg Spine. 2020:1–7. [DOI] [PubMed] [Google Scholar]
- 33.Fischer JP, Wes AM, Nelson JA, Serletti JM, Kovach SJ. Factors associated with readmission following plastic surgery: a review of 10,669 procedures from the 2011 American College of Surgeons National Surgical Quality Improvement Program data set. Plast Reconstr Surg. 2013;132(3):666–674. [DOI] [PubMed] [Google Scholar]
- 34.Mioton LM, Buck DW 2nd, Rambachan A, Ver Halen J, Dumanian GA, Kim JYS. Predictors of readmission after outpatient plastic surgery. Plast Reconstr Surg. 2014;133(1):173–180. [DOI] [PubMed] [Google Scholar]
- 35.Spataro E, Branham GH, Kallogjeri D, Piccirillo JF, Desai SC. Thirty-Day Hospital Revisit Rates and Factors Associated With Revisits in Patients Undergoing Septorhinoplasty. JAMA Facial Plast Surg. 2016;18(6):420–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Massenburg BB, Sanati-Mehrizy P, Jablonka EM, Taub PJ. Risk Factors for Readmission and Adverse Outcomes in Abdominoplasty. Plast Reconstr Surg. 2015;136(5):968–977. [DOI] [PubMed] [Google Scholar]
- 37.Vieira BL, Dorfman R, Turin S, Gutowski KA. Rates and Predictors of Readmission Following Body Contouring Procedures: An Analysis of 5100 Patients From The National Surgical Quality Improvement Program Database. Aesthet Surg J. 2017;37(8):917–926. [DOI] [PubMed] [Google Scholar]


