Abstract
Introduction
Primary pleural epithelial angiosarcoma (EAS) is an extremely rare tumor with no specific clinical symptoms. Clinical data on primary pleural EAS are limited, and misdiagnosis often occurs.
Case Presentation
The present study reports the case of a 31-year-old patient diagnosed with primary pleural EAS with lung and bone metastases. The patient presented with persistent right chest pain for 5 months and dyspnea for 2 months. Chest computed tomography (CT) scan revealed right hydropneumothorax, diffuse thickening of the right pleura, passive atelectasis, and scattered nodules in the left lung. A medical thoracoscopic pleural biopsy revealed a vasogenic tumor. To further confirm the diagnosis, positron emission tomography/CT (PET/CT) examination was recommended to determine the biopsy site after multidisciplinary discussion. Increased 18F-FDG uptake in the right pleura and hypermetabolic nodules in the right chest wall, first lumbar vertebrae, second sacral vertebrae, and bilateral iliac crest was detected via PET/CT. CT-guided chest wall and lung biopsies were performed. Immunohistochemistry of specific markers was performed according to remote consultation with a pathologist, and tumor cells with strong positive expression of CD31, CD34, and ETS-related genes led to the final diagnosis of primary pleural EAS.
Conclusion
Primary pleural EAS should be considered for hydropneumothorax of an unknown cause. PET/CT can accurately locate the lesion. The pathological examination is the basis for primary pleural EAS diagnosis. Moreover, multidisciplinary discussion and remote expert consultation can improve the diagnosis rate of primary pleural EAS.
Keywords: Epithelial angiosarcoma, Pleural epithelial angiosarcoma, Positron emission tomography/computed tomography, CD31
Introduction
Angiosarcoma is a rare malignant tumor that accounts for approximately 1–2% of all soft tissue sarcomas. This tumor originates from the endothelial cells of the small blood vessels. It usually occurs in the skin and soft tissue and can invade the lungs, liver, bone, and mammary glands [1]. Primary pleural epithelial angiosarcoma (EAS) has no typical symptomatology or specific physical exam findings, making the diagnosis clinically challenging even with advances in diagnostic imaging. Here, we report a case of primary pleural EAS with lung and bone metastases and review of the relevant literature.
Case Presentation
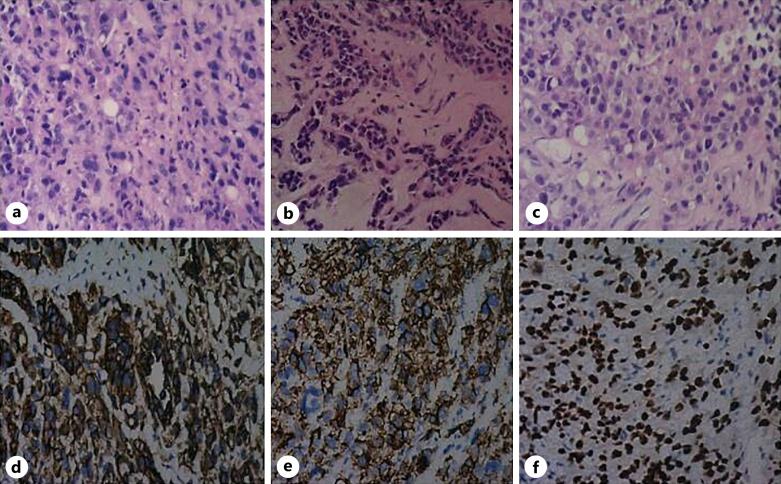
A 31-year-old male without underlying disease was presented to the Respiratory Medicine Department with right chest pain for half a year and an asthma attack 2 months before admission. At baseline, a chest computed tomography (CT) scan was performed which showed thickened pleura and small amount of right pleural effusion. However, 2 months prior, the chest CT scan revealed decreased lung volume, hydropneumothorax (70% compression) (Fig. 1a), scattered nodules in the left lung (Fig. 1b), and thickening of the right pleura (Fig.1c). Serum carcinoembryonic antigen and cytokeratin levels were normal, and thoracic closed drainage was performed. Routine examination of the pleural fluid indicated hemorrhagic effusion with normal carcinoembryonic antigen and cytokeratin levels. No tumor cells were detected in pleural fluid cytology. Positron emission tomography/CT (PET/CT) was performed, which showed two hypermetabolic nodules with mild diffuse thickening of the right pleura, and multiple destructive bone lesions were located at the first lumbar vertebrae, second sacral vertebrae, bilateral ilium, and left ischium (Fig. 2). Thoracoscopic pleural biopsy was performed under local anesthesia. Thoracoscopy revealed hemorrhagic hydrothorax, scattered hemorrhagic sites on the parietal and visceral pleura, and thickened pleura. Immunohistochemistry showed cluster of differentiation (CD) 31 (+) (Fig. 3d), vimentin (+), D2-40 (+), Ki-67 (+10%), tumor protein 53 (P53) (+), and creatine phosphokinase (CK) (−), indicating the possibility of a vasogenic tumor. After multidisciplinary discussion (oncology, pulmonology, pathology, and imaging) and remote expert consultation, it was suggested to perform lung and chest wall biopsies and test for CD34 and ETS-related genes (ERG). The lung and chest walls were biopsied under CT guidance. Pathological hematoxylin-eosin staining showed that pleural tumor cells were more heterogeneous than those of the chest wall and lungs (Fig. 3a–c). Immunohistochemical tests revealed CD34 (+) (Fig. 3e), ERG (+) (Fig. 3f), and F8 (−). Finally, the patient was diagnosed with primary pleural EAS with lung and bone metastases. The patient received 4 cycles of chemotherapy with ifosfamide and adriamycin. Unfortunately, the patient died 4 months after the diagnosis was confirmed.
Fig. 1.
Chest CT and PET/CT. Chest CT showed decreased lung volume and hydropneumothorax (70% compression) on the right (a), scattered nodules in the left lung (b), and thickening of the right pleura (c). PET/CT showed that the right pleura which had two high metabolism nodules was mild diffuse thickened with hypermetabolism (d, e), and multiple bone destruction with hypermetabolism was located at L1 and S2 (f). L1, first lumbar vertebrae; S2, second sacral vertebrae.
Fig. 2.
Medical thoracoscopy. Hemorrhagic hydrothorax (a), scattered hemorrhagic sites on the parietal and visceral pleura (b), and mildly adhesive and thickened pleura (c) were observed through thoracoscopy.
Fig. 3.
HE staining and immunohistochemistry. HE (×200): tumor cells in pleura (a) are more heterogeneous than those in the chest wall (b) and lung tissue (c). Pleural immunohistochemistry (×200): CD31 (+) (d), CD34 (+) (e), and ERG (+) (f).
Discussion
Angiosarcoma is a rare but fatal neoplasm that mainly occurs in the skin and soft tissue and can affect the digestive tract, breast, bone, kidney, spleen, lung, and other internal organs [1]. Primary pleural EAS is uncommon, and no more than 30 cases have been reported [2]. It is characterized by easy recurrence, rapid development, and poor prognosis. However, its etiology and pathogenesis remain unclear. Some Japanese researchers have reported that pleural angiosarcoma is associated with a history of chronic tuberculous pyothorax [3]. Some researchers have reported that pleural angiosarcoma is associated with a history of exposure to radiation and asbestos exposure [4]. However, our patient was not exposed to these risk factors.
Primary pleural EAS is an extremely rare malignancy with atypical clinical symptoms and CT findings, resulting in a high rate of misdiagnosis. Wang et al. [5] summarized 43 cases of primary pleural angiosarcoma with a mean age of 64 years (24–87 years) which indicated a higher incidence in males. The most frequent manifestations were pleural mass (44%) and pleural invasion (70%). The symptoms were not restricted to dyspnea and included chest pain, hemoptysis, cough, fever, weight loss, fatigue, and anorexia. Pleural angiosarcoma is often epithelioid (56%). The patient in our case presented with chest pain, cough, progressive dyspnea, hemothorax, and extensive pleural thickening, which was consistent with previous reports. Concurrent pneumothorax was first reported.
Pathology is the gold standard for diagnosing primary pleural EAS. No tumor cells were found in the pleural fluid, and the diagnosis was not confirmed by thoracoscopic pleural biopsy in our case. PET/CT can be adopted to assist in staging and guide biopsy. In this case, PET/CT was performed to determine the location of the lesion according to multidisciplinary discussions, and bone metastasis was confirmed. Furthermore, chest wall and lung biopsies were performed based on the PET/CT findings. It is difficult to differentiate mesothelioma from metastatic tumors based on morphology, which may be resolved using immunohistochemistry. CD34 is not only expressed in angiosarcoma but also in nonvascular soft tissue tumors, including epithelioid sarcoma, malignant peripheral nerve sheath tumor, leiomyosarcoma, and clear cell sarcoma. CD31 is a highly specific and sensitive endothelial cell marker. CD31 and CD34 are epithelial-specific markers with high sensitivity and specificity [6, 7]. ERG is expressed in both benign and malignant vascular tumors and is located in the cell nucleus [8]. The expression of vimentin and D2-40 suggests mesenchymal and lymphatic endothelial differentiation, respectively, and Ki-67 is positively correlated with the degree of the tumor [9]. Based on the relevant literature, we made a summary as follows [2, 10–12]: (1) angiosarcoma that is presented with more severe symptoms is more prone to distant metastasis; (2) angiosarcoma cells are more atypical; (3) chromosomal shift t(1; 3) (p36. q25) leads to the formation of the WWTRl-CAMTAI fusion gene, which can be used as a molecular diagnostic tool for the diagnosis of angiosarcoma. In our case, CD34, CD31, and ERG were positively expressed in the pleura, chest wall, and lung tissue, whereas D2-40 and vimentin were only positively expressed in the pleura. Combining pathologic findings and clinical manifestations, including rapid disease progression, the patient was diagnosed with primary pleural epithelioid hemangiosarcoma with lung and bone metastases.
Therapies for pleural EAS include surgery, radiotherapy, and/or chemotherapy. Surgery is proved to be the most effective treatment for limited primary pleural EAS [4]. Chemotherapeutic drugs include gemcitabine, docetaxel, paclitaxel, cisplatin, ifosfamide, doxorubicin, and/or albumin-binding paclitaxel, but their efficacy is limited [13]. Some researchers have also used the PD-1 inhibitor pembrolizumab as an effective treatment [14]. Currently, there is no standard therapy. Pleural effusion and hemothorax were significant predictors of decreased survival [5]. The mean survival after the diagnosis was less than 1 year [14, 15]. The patient in our case was administered chemotherapy with ifosfamide and adriamycin. Unfortunately, the patient died 4 months after the diagnosis was confirmed.
In conclusion, epithelioid angiosarcoma in the pleura is extremely rare, and primary pleural EAS should be considered for hydropneumothorax and hemorrhagic pleural effusion of unknown etiology. PET/CT examination is helpful for accurate location of the lesion. Pathology is the most important method for diagnosing pleural EAS. Multidisciplinary discussion and remote expert consultation can improve diagnostic rates. The CARE Checklist has been completed by the authors for this case report, attached as online supplementary material (for all online suppl. material, see https://doi.org/10.1159/000535985).
Statement of Ethics
This case report did not require ethical approval in accordance with local/national guidelines. Written informed consent was obtained from the patient for publication of the details of their medical case and any accompanying images prior to their passing away.
Conflict of Interest Statement
The authors report no conflict of interest.
Funding Sources
This work was partially funded by the Natural Science Foundation of Jiangsu Province (BK20210981).
Author Contributions
Methodology: Chenghua Zhu. Resources: Xingran Du. Writing – original draft: Chenghua Zhu and Ning Yang. Writing – review and editing: Chenghua Zhu and Jing Yao.
Funding Statement
This work was partially funded by the Natural Science Foundation of Jiangsu Province (BK20210981).
Data Availability Statement
All data generated or analyzed during this study are included in this article and its online supplementary material. Further inquiries can be directed to the corresponding author.
Supplementary Material
References
- 1. Patel AM, Ryu JH. Angiosarcoma in the lung. Chest. 1993;103(5):1531–5. [DOI] [PubMed] [Google Scholar]
- 2. Yu L, Sun Y, Wang M, Yuan L, Wang Q, Qian X. Primary pulmonary epithelioid angiosarcoma with thyroid tumor history: a case report and literature review. Exp Ther Med. 2022;24(1):471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kimura M, Ito H, Furuta T, Tsumoto T, Hayashi S. Pyothorax-associated angiosarcoma of the pleura with metastasis to the brain. Pathol Int. 2003;53(8):547–51. [DOI] [PubMed] [Google Scholar]
- 4. Zhang PJ, Livolsi VA, Brooks JJ. Malignant epithelioid vascular tumors of the pleura: report of a series and literature review. Hum Pathol. 2000;31(1):29–34. [DOI] [PubMed] [Google Scholar]
- 5. Wang X, Lu Z, Luo Y, Cai J, Wei J, Liu A, et al. Characteristics and outcomes of primary pleural angiosarcoma: a retrospective study of 43 published cases. Medicine. 2022;101(6):e28785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Woo JJ, Kim Y, An JK, Lee H. Primary pleural epithelioid angiosarcoma manifesting as a loculated hemothorax: a case report and literature review focusing on CT findings. Radiol Case Rep. 2021;16(10):3072–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Roh MS, Seo JY, Hong SH. Epithelioid angiosarcoma of the pleura: a case report. J Korean Med Sci. 2001;16(6):792–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Miettinen M, Wang Z-F, Paetau A, Tan S-H, Dobi A, Srivastava S, et al. ERG transcription factor as an immunohistochemical marker for vascular endothelial tumors and prostatic carcinoma. Am J Surg Pathol. 2011;35(3):432–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hata H, Aoyagi S, Homma E, Muramatsu R, Shimizu H. Lymphangiosarcoma with strong positivity of D2-40 and LYVE-1 presenting different clinical features from angiosarcoma. J Dermatol. 2014;41(7):656–7. [DOI] [PubMed] [Google Scholar]
- 10. Amin RMS, Hiroshima K, Kokubo T, Nishikawa M, Narita M, Kuroki M, et al. Risk factors and independent predictors of survival in patients with pulmonary epithelioid haemangioendothelioma. Review of the literature and a case report. Respirology. 2006;11(6):818–25. [DOI] [PubMed] [Google Scholar]
- 11. Errani C, Zhang L, Sung YS, Hajdu M, Singer S, Maki RG, et al. A novel WWTR1-CAMTA1 gene fusion is a consistent abnormality in epithelioid hemangioendothelioma of different anatomic sites. Genes Chromosomes Cancer. 2011;50(8):644–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lee SJ, Yang WI, Chung W-S, Kim SK. Epithelioid hemangioendotheliomas with TFE3 gene translocations are compossible with CAMTA1 gene rearrangements. Oncotarget. 2016;7:7480–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hara N, Fujimoto N, Miyamoto Y, Yamagishi T, Asano M, Fuchimoto Y, et al. Angiosarcoma of the thoracic wall responded well to nanoparticle albumin-bound paclitaxel: a case report. Drug Discov Ther. 2016;10(2):114–6. [DOI] [PubMed] [Google Scholar]
- 14. Wang X, Wei J, Zeng Z, Cai J, Lu Z, Liu A. Primary pleural epithelioid angiosarcoma treated successfully with anti-PD-1 therapy: a rare case report. Medicine. 2021;100(35):e27132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sedhai YR, Basnyat S, Golamari R, Koirala A, Yuan M. Primary pleural angiosarcoma: case report and literature review. SAGE Open Med Case Rep. 2020;8:2050313X20904595. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this article and its online supplementary material. Further inquiries can be directed to the corresponding author.