Highlights
-
•
Reports of alcohol/cannabis use among youth increases with each additional year.
-
•
Sex and race/ethnicity differences were examined using the 2019 NSDUH data.
-
•
Increased alcohol use across age was much steeper in Whites/Latinos than Blacks.
-
•
Increased cannabis use across age was slightly steeper in Latinos than Whites/Blacks.
-
•
Increased alcohol use across age was slightly steeper in girls than boys.
Keywords: Alcohol, Cannabis, Adolescence, Sex, Race, Ethnicity
Abstract
Background
Early use of alcohol and cannabis is associated with health and social problems. It is unclear how lifetime use changes for each additional year of age during adolescence, and whether this change varies by sex and race/ethnicity. This study characterized lifetime rates of alcohol and cannabis use by age among 12- to 17-year-old American youth and explored differential patterns by sex and race/ethnicity.
Methods
Data were obtained from the 2019 National Survey on Drug Use and Health. Analyses were restricted to 12–17-year-olds who were non-Hispanic White, non-Hispanic Black, or Hispanic/Latino (n = 11,830). We estimated the increase in lifetime use of alcohol and cannabis by age for the full sample and stratified by sex and race/ethnicity. Slopes of the regression lines were compared to assess differential patterns across groups.
Results
In these cross-sectional analyses, reported lifetime use increased substantially from age 12 to 17 for alcohol (6.4 % to 53.2 %) and cannabis (1.3 % to 35.9 %). The increase in lifetime alcohol use was slightly, but not significantly, steeper among girls than boys (F1,8 = 3.40, p = 0.09). White and Latino youth showed similar rates of increase in lifetime alcohol use, which was significantly flatter among Black youth (F2,12=21.26, p<0.0001). Latino youth had a slightly, but not significantly, steeper increase in lifetime cannabis use than White and Black youth (F2,12=3.17, p = 0.07).
Conclusions
Reports of lifetime alcohol and cannabis use substantially increase from age 12 to 17 and the rates are different according to sex and race/ethnicity, highlighting the need for early and tailored substance use prevention in adolescents.
1. Introduction
Alcohol and cannabis are among the most frequently used substances and considerably contribute to global burden of disease (Anthony et al., 2017; GBD 2016 Alcohol and Drug Use Collaborators, 2018; Jayathilaka et al., 2022; Shao et al., 2023). Adolescence is a critical period for experimentation and initiation of alcohol and cannabis use in the United States (U.S.) and around the globe. Most youth begin adolescence never having used alcohol or cannabis and exit adolescence having used one or both substances. Worldwide, 26.5 % of 15–19-year-old youth report current drinking, which is equivalent to almost 155 million youth (WHO, 2018). Prevalence of current and lifetime use of cannabis is highly variable across countries. It is estimated that 3–5 % of the world population have tried cannabis product, but these rates are much higher in North America, Western Europe, and Australia (Anthony et al., 2017; WHO). Specific to the U.S., 53 % of American youth report lifetime alcohol use by the age of 18 and 36 % report lifetime cannabis use (SAMHSA, 2019). According to the Monitoring the Future (MTF), which surveys 8th, 10th, and 12th grade students across the U.S., lifetime prevalence of alcohol and cannabis use are estimated to be around 40 % and 25 %, respectively, in this population (Johnston et al., 2023).
Early use of alcohol and cannabis is a public health concern, as it is associated with poor short- and long-term outcomes (Ahuja et al., 2022; Beverly et al., 2019; Buchmann et al., 2009; Chen et al., 2009; DeWit et al., 2000; Enstad et al., 2019; Hawke et al., 2020; Hingson and Zha, 2009; Millar et al., 2021; Sartor et al., 2016; Trujillo et al., 2019; Volkow et al., 2021; Winters and Lee, 2008). Alcohol and cannabis use may disrupt many of the psychosocial and neurobiological changes taking place during adolescence (Batalla et al., 2013; Meruelo et al., 2017; Squeglia, 2020). Alcohol use greatly increases risk for car crashes and sexual assault, and alcohol and cannabis use are associated with mental and behavioral health problems, including poor school performance and substance use disorders (Buchmann et al., 2010; Hall and Lynskey, 2016; Lees et al., 2021; Miller et al., 2007; Schuler et al., 2019; Senay, 1991; Shapiro and Buckley-Hunter, 2010; Sise et al., 2009; Volkow et al., 2016).
The purpose of this study is to examine lifetime reports of alcohol and cannabis use among a sample of 12–17-year-olds in the U.S., using cross-sectional data and considering how proportions increase with each additional year of age. This investigation will offer insights about the ages at which use of either drug can be considered developmentally “normative” and how “early use” should be conceptualized. An additional aim of this study is to examine potential sex and race/ethnicity differences in the ascending lifetime use of alcohol and cannabis during adolescence. There is strong evidence of group differences in the onset, severity, and progression of substance use (Agrawal and Lynskey, 2007; Becker, 2016; Compton et al., 2004; Evans-Polce et al., 2015; Fairman, 2016; Grant et al., 2006; Harris et al., 2022; Huang and Connell, 2019; Keyes et al., 2017; Kozak et al., 2021; Lee et al., 2021; Martins et al., 2021; Pope et al., 2003; Quigley et al., 2021; Terry-McElrath and Patrick, 2020; Wagner and Anthony, 2007). Although adolescent boys are more likely than girls to use alcohol and cannabis, and to use the substances at younger ages, recent research indicates that sex differences are narrowing both in the U.S. and globally (e.g. Europe) (Cheng and Anthony, 2017; Cheng et al., 2016; Keyes et al., 2022; White, 2020). Furthermore, studies of racial/ethnic differences in substance use suggest that White adolescents report higher prevalence of alcohol use compared to Black and Latino adolescents, and Black adolescents use cannabis at earlier ages compared to White and Latino adolescents (Alcover et al., 2021; SAMHSA, 2021). Our work will shed light on similarities and differences in rates of adolescence alcohol and cannabis use by sex and race/ethnicity, which can inform tailored preventive strategies and larger scale policies.
2. Methods
We used cross-sectional data from the 2019 National Survey on Drug Use and Health (NSDUH). Public-Use Files (PUFs) and the codebook were downloaded from the Substance Abuse and Mental Health Data Archive (SAMHDA). NSDUH is a nationally-representative, annual survey of the U.S. population. The purpose of the survey is to monitor alcohol and drug use, substance use disorders, and other health information. The sample is selected using a multistage area probability sampling method. Participants include civilian, non-institutionalized individuals aged 12 or older from the 50 U.S. States and the District of Columbia. We restricted analyses to 12–17-year-olds who were non-Hispanic White, non-Hispanic Black, or Hispanic/Latino, hereafter referred to as White, Black, and Latino.
2.1. Measures
Study variables included age, sex, race/ethnicity, and lifetime use of alcohol and cannabis. Lifetime use is a dichotomous variable based on respondents’ reports of whether they have ever used the substance.
2.1.1. Age
Participants reported their birthdate (month, day, year) in response to “What is your date of birth?” and had multiple opportunities to correct their age in response to consistency checks throughout the interview.
2.1.2. Sex
This variable was entered by the interviewer, rather than being self-reported, in response to “Record respondent's gender”, and choices included “Male” or “Female”.
2.1.3. Race/ethnicity
Participants were first asked “Are you of Hispanic, Latino, or Spanish origin or descent?”. Subsequently, they were asked several questions and presented with a few showcards, based on which race/ethnicity categories were coded: Non-Hispanic White, Non-Hispanic Black/African American, Non-Hispanic Native American/Alaska Native, Non-Hispanic Native Hawaiian or Other Pacific Islander, Non-Hispanic Asian, Non-Hispanic more than one race, and Hispanic/Latino. Analyses for this study were limited to non-Hispanic White, non-Hispanic Black, and Hispanic/Latino individuals, as the three groups with largest and relatively balanced numbers. Including more groups, especially with low numbers, would require more complex statistical models beyond the scope of this work.
2.1.4. Lifetime (ever) use
Participants reported lifetime alcohol use in response to “Have you ever, even once, had a drink of any type of alcoholic beverage? Please do not include times when you only had a sip or two from a drink”. They also reported lifetime cannabis use in response to “Have you ever, even once, used marijuana or hashish?”.
2.2. Analyses
We used descriptive statistics to characterize the study sample based on age, sex, race/ethnicity, and lifetime alcohol and cannabis use. We created proportions with time held constant, and estimated the percentage who had been affected, i.e., used alcohol or used cannabis, by the age at assessment. The denominator of these proportions is the number at each age (with elapsed time implicit in that denominator) and the numerator is the number affected. Pearson's chi-square tests compared age-specific proportions by sex and race/ethnicity. Regression models assessed differential associations between change in proportions reporting lifetime alcohol and cannabis use by sex and race/ethnicity. Simple linear regressions were applied to find the best fitting line for the two-dimensional datasets of interest in this study. Regression lines were fitted between age and proportion reporting lifetime alcohol or cannabis use and the slopes of the regression lines were compared across groups. IBM SPSS Statistics 25.0 and GraphPad Prism 8.0.1 were used for data analysis and visualization.
3. Results
Fifty-one percent of respondents were male, and the proportion at each year of age ranged from 16 % to 17 % (total weighted n = 11,830). More than one-half of the respondents were White (58 %), 15.1 % were Black, and 26.9 % were Latino. In the full sample, 28.4 % reported lifetime alcohol use and this proportion was somewhat higher among girls than boys (30.3 % % vs. 26.6 %). Lifetime alcohol use was reported by 30.6 %, 20.6 %, and 28.1 % of White, Black, and Latino respondents, respectively. Nearly one-fifth (17.4 %) reported lifetime use of cannabis. Sex difference in the proportions reporting lifetime cannabis use was modest (17.9 % for girls vs. 16.9 % for boys), as were differences by race/ethnicity (16.7 %, 16.6 %, and 19.4 % for White, Black, and Latino respondents, respectively) (Table 1).
Table 1.
Study sample breakdown and reports of lifetime alcohol and cannabis use.
| Total Sample N ( %) | Lifetime Alcohol Use N ( %) | Lifetime Cannabis Use N ( %) | |
|---|---|---|---|
| Variable | 11,830 (100 %) | 3362 (28.4 %) | 2057 (17.4 %) |
| Sex | |||
| Male | 6042 (51.1 %) | 1606 (26.6 %) | 1020 (16.9 %) |
| Female | 5788 (48.9 %) | 1756 (30.3 %) | 1037 (17.9 %) |
| Race/Ethnicity | |||
| Non-Hispanic White | 6863 (58.0 %) | 2101 (30.6 %) | 1145 (16.7 %) |
| Non-Hispanic Black | 1781 (15.1 %) | 366 (20.6 %) | 295 (16.6 %) |
| Hispanic/Latino | 3186 (26.9 %) | 895 (28.1 %) | 617 (19.4 %) |
| Age (years) | |||
| 12 | 1872 (15.8 %) | 120 (6.4 %) | 26 (1.4 %) |
| 13 | 1958 (16.6 %) | 257 (13.1 %) | 119 (6.1 %) |
| 14 | 1959 (16.6 %) | 394 (20.1 %) | 231 (11.8 %) |
| 15 | 2019 (17.1 %) | 654 (32.4 %) | 380 (18.8 %) |
| 16 | 2052 (17.3 %) | 887 (43.2 %) | 593 (28.9 %) |
| 17 | 1970 (16.7 %) | 1050 (53.3 %) | 708 (35.9 %) |
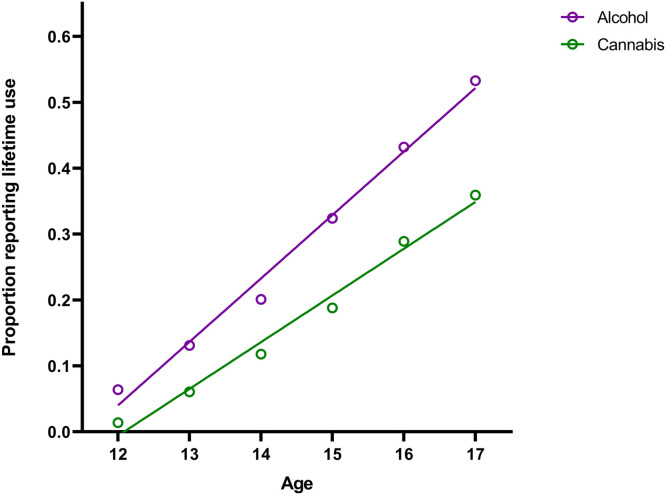
As expected, the proportion reporting lifetime use increased by each additional year of age. At age 12, 6.4 % reported lifetime alcohol use and 1.3 % reported lifetime cannabis use. By age 17, 53.2 % reported lifetime alcohol use and 35.9 % reported lifetime cannabis use (Table 1). Statistical comparison of the regression lines showed that the increase in lifetime alcohol use was steeper than the increase in cannabis use [F (1, 8) = 14.41, p = 0.005] (Fig. 1, Table S1), indicating that, from age 12 to 17, the proportion of youth reporting any alcohol use increases at a more rapid pace than the proportion reporting any cannabis use.
Fig. 1.
Proportions reporting lifetime alcohol and cannabis use across age. The X axes indicate age groups. The Y axes indicate the proportion of respondents reporting lifetime use in each group. Slope of the best fit regression line was steeper for alcohol than cannabis: F (1, 8) = 14.41, p = 0.005.
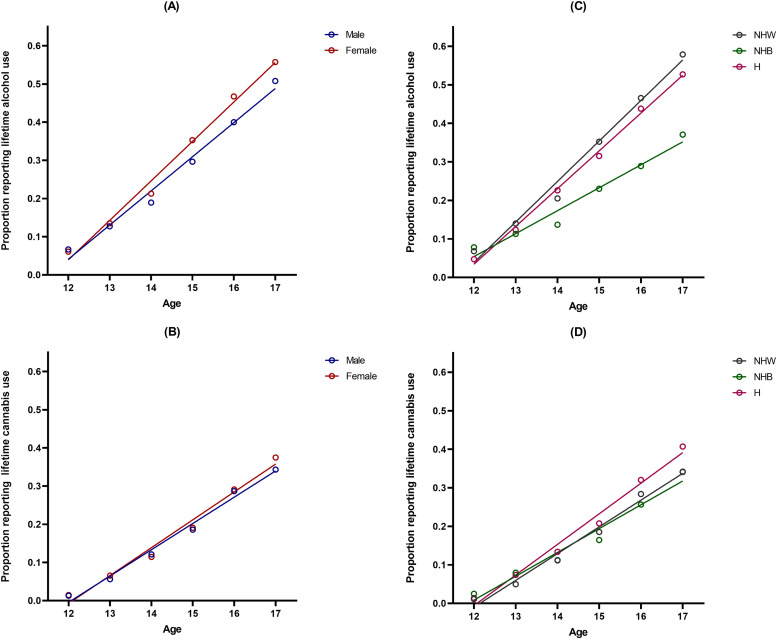
Sex differences in lifetime use of alcohol and cannabis from age 12 to 17 years were modest. There were no statistically significant sex differences in lifetime alcohol use at ages 12, 13, and 14, although lifetime reports of alcohol use were higher among girls than boys at ages 15, 16, and 17 (Table 2), leading to a slightly but not significantly higher slope of the regression line for girls [F (1, 8) = 3.40, p = 0.09] (Fig. 2A, Table S2). Reports of lifetime cannabis use was similar among boys and girls at every age from 12 to 17 years (Table 2) and comparison of the regression lines found no sex difference [F (1, 8) = 0.42, p = 0.53] (Fig. 2B, Table S3).
Table 2.
Percentage reporting lifetime alcohol and cannabis use in each group.
| Lifetime alcohol use | ||||||||
|---|---|---|---|---|---|---|---|---|
| Age | Full sample | Male | Female | Test for difference | Non-Hispanic White | Non-Hispanic Black | Hispanic / Latino | Test for difference |
| 12 | 6.4 % | 6.7 % | 6.1 % | χ2 (1) = 0.26, p = 0.60 | 6.8 % | 7.8 % | 4.7 % | χ2 (2) = 3.59, p = 0.16 |
| 13 | 13.1 % | 12.7 % | 13.5 % | χ2 (1) = 0.26, p = 0.60 | 14.0 % | 11.3 % | 12.3 % | χ2 (2) = 1.90, p = 0.38 |
| 14 | 20.1 % | 18.9 % | 21.3 % | χ2 (1) = 1.68, p = 0.19 | 20.5 % | 13.7 % | 22.6 % | χ2 (2) = 9.58, p = 0.008 |
| 15 | 32.4 % | 29.6 % | 35.3 % | χ2 (1) = 7.38, p = 0.007 | 35.2 % | 23.0 % | 31.5 % | χ2 (2) = 16.71, p < 0.001 |
| 16 | 43.2 % | 40.0 % | 46.7 % | χ2 (1) = 9.48, p = 0.002 | 46.6 % | 28.9 % | 43.8 % | χ2 (2) = 31.44, p < 0.001 |
| 17 | 53.3 % | 50.8 % | 55.7 % | χ2 (1) = 4.86, p = 0.02 | 57.9 % | 37.1 % | 52.7 % | χ2 (2) = 41.55, p < 0.001 |
| Slope | 0.096 | 0.089 | 0.103 | F (1, 8) = 3.40, p = 0.09 | 0.105 | 0.059 | 0.098 | F (2, 12) = 21.26, p < 0.001 |
| Lifetime cannabis use | ||||||||
|---|---|---|---|---|---|---|---|---|
| Age | Full sample | Male | Female | Test for difference | Non-Hispanic White | Non-Hispanic Black | Hispanic / Latino | Test for difference |
| 12 | 1.4 % | 1.3 % | 1.5 % | χ2 (1) = 0.79, p = 0.77 | 1.1 % | 2.5 % | 1.4 % | χ2 (2) = 3.12, p = 0.20 |
| 13 | 6.1 % | 5.6 % | 6.6 % | χ2 (1) = 0.75, p = 0.38 | 5.0 % | 8.0 % | 7.4 % | χ2 (2) = 6.00, p = 0.05 |
| 14 | 11.8 % | 12.1 % | 11.5 % | χ2 (1) = 0.20, p = 0.65 | 11.2 % | 11.2 % | 13.4 % | χ2 (2) = 1.87, p = 0.39 |
| 15 | 18.8 % | 18.6 % | 19.1 % | χ2 (1) = 0.08, p = 0.77 | 18.5 % | 16.4 % | 20.8 % | χ2 (2) = 2.54, p = 0.28 |
| 16 | 28.9 % | 28.7 % | 29.1 % | χ2 (1) = 0.04, p = 0.82 | 28.4 % | 25.6 % | 32.0 % | χ2 (2) = 4.23, p = 0.12 |
| 17 | 35.9 % | 34.3 % | 37.5 % | χ2 (1) = 2.12, p = 0.14 | 34.2 % | 34.1 % | 40.7 % | χ2 (2) = 7.23, p = 0.02 |
| Slope | 0.070 | 0.068 | 0.072 | F (1, 8) = 0.42, p = 0.53 | 0.069 | 0.061 | 0.079 | F (2, 12) = 3.17, p = 0.07 |
Fig. 2.
Proportions reporting lifetime alcohol and cannabis use across age by sex and race/ethnicity. The X axes indicate age groups. The Y axes indicate the proportion of respondents reporting lifetime use in each group. Comparison of the slopes of the best fit regression lines were as follows: (A): F (1, 8) = 3.40, p = 0.09; (B): F (1, 8) = 0.42, p = 0.53; (C): F (2, 12) = 21.26, p = 0.0001; (D): F (2, 12) = 3.17, p = 0.07. H, Hispanic/Latino; NHB, Non-Hispanic Black; NHW, Non-Hispanic White.
There were noteworthy race/ethnicity differences in lifetime use of alcohol and cannabis from age 12 to 17 years. Statistically significant differences were found in proportions reporting lifetime alcohol use for ages 14–17, with lowest rates reported among Black youth (Table 2). Comparing the regression lines showed that White and Latino youth had similar patterns of increased lifetime alcohol use, whereas the rate of increase was significantly flatter among Black respondents [F (2, 12) = 21.26, p = 0.0001] (Fig. 2C, Table S4). For cannabis, there was a significant difference only at age 17, with highest rates reported among Latino youth (Table 2). Latino youth showed a slightly but not significantly steeper increase in lifetime cannabis use, compared to White and Black youth [F (2, 12) = 3.17, p = 0.07] (Fig. 2D, Table S5). Overall, the steepness of regression lines suggest that Black adolescents have the slowest rate of increasing lifetime use of alcohol, while Latino adolescents have the fastest rate of increasing lifetime use cannabis use with each additional year from age 12 to 17.
In a final set of analyses, we explored differential increases in lifetime alcohol and cannabis use by both sex and race/ethnicity. We compared the slopes of the 6 sex-by-race/ethnicity groups and did not observe any significant differences, although for both alcohol and cannabis, Latino boys showed slightly steeper slopes compared to other groups (Figures S1 and S2).
4. Discussion
The purpose of this study was to provide a snapshot of lifetime alcohol and cannabis use among U.S. youth and increased reports of lifetime use from age 12 to 17, with an examination of potential sex and race/ethnicity differences. We observed a marked increase in the percentage of youth reporting lifetime alcohol and cannabis use with each additional year of age, with the largest increases between ages 12 to 13. There was a steeper increase in alcohol use for each additional year than for cannabis use. Reports of lifetime alcohol use was higher than cannabis use at each age, a finding consistent with the exiting literature (Pacula et al., 2016; Sullivan et al., 2022).
Our findings on increased lifetime reports of alcohol and cannabis use with age during adolescence are consistent with other survey studies in the U.S., including the Youth Risk Behavior Surveillance System (YRBSS) and Monitoring The Future (MTF), both of which include students from certain grades (Johnston et al., 2023; Mpofu et al., 2023). One major advantage of using NSDUH is the capacity to look at the full spectrum from early through mid-late adolescence. NSDUH is a nationwide survey, has one of the largest samples sizes, and provides estimates for each and every age, which are key characteristics for the analyses performed here. We used cross-sectional data from the 2019 NSDUH since this was the last version collected prior to the COVID-19 pandemic, therefore not affected by the well-documented changes in mental health and substance use as a result of the pandemic (Hurlocker et al., 2022; Meade, 2021; Temple et al., 2022) and more likely to reflect long-term patterns. Future longitudinal work could explore possible changes over time, for example pre- to post-pandemic, by analyzing data across different years.
Early use of alcohol and cannabis is associated with health and social problems (Ahuja et al., 2022; Beverly et al., 2019; Buchmann et al., 2009; Chen et al., 2009; DeWit et al., 2000; Enstad et al., 2019; Hawke et al., 2020; Hingson and Zha, 2009; Millar et al., 2021; Sartor et al., 2016; Trujillo et al., 2019; Volkow et al., 2021; Winters and Lee, 2008). We found that 20 % of adolescents reported lifetime use of alcohol by age 14, and 19 % reported lifetime cannabis use by age 15. While these results are purely descriptive, they underscore the need for educational programs, behavioral health screening, and prevention in early adolescence. Our study also offers four main insights about sex and race/ethnicity differences in alcohol and cannabis use among U.S. adolescents, as detailed below. It is important to note that, beyond statistical significance, our study aimed to describe patterns across groups and generate hypotheses that need to be tested in more comprehensive work.
First, there were more reports of lifetime alcohol use among girls than boys during mid-adolescence (15, 16, and 17 years old), but the rates were similar across sexes at younger ages. Putting these together, the rate of increase in lifetime alcohol use was slightly higher for girls than boys, although the difference did not reach statistical significance. Historically, rates of alcohol use and associated problems have been higher among men than women, but several reports indicate that this gap is narrowing (Cheng and Anthony, 2017; White et al., 2015). Consistent with our findings, recent epidemiological data suggest that, for example, the probability of starting to drink alcohol in mid-adolescence is higher among females than males and the so-called gender gap in alcohol drinking has disappeared, at least at population level (Cheng et al., 2016). In the last decade, rates of alcohol use increased by 84 % among women, relative to 35 % among men (Grant et al., 2017). Among U.S. adolescents, boys have historically reported higher cannabis use than girls, but analysis of longitudinal epidemiological data shows that the gap is quickly becoming nonexistent (Johnson et al., 2015). Of note, no sex difference in cannabis use was found in this study, meaning that at any given age during adolescence, the proportion of youth reporting lifetime cannabis use did not differ between males and females. While a greater number of adult males meet criteria for a cannabis use disorder diagnosis, some reports suggest that females are more sensitive to the subjective effects of cannabis, possibly contributing to a more rapid progression of cannabis use disorder (Cooper and Haney, 2014; Hasin et al., 2016). Females are also disproportionally affected by negative consequences related to cannabis use compared to males (Gräfe et al., 2023; Grigsby et al., 2023). The diminishing sex differences in use also underscores the need for more access to substance use treatment services for women, given that most of these services have historically been geared toward and utilized by men.
Second, more White youth reported ever drinking alcohol compared to Black or Latino youth, which is consistent with previous literature (Bouchard et al., 2021; Terry-McElrath and Patrick, 2020). Our analyses also revealed that the increase in reports of lifetime alcohol use from age 12 to 17 was similar among White and Latino youth, and that both groups had a steeper increase compared to Black youth. High levels and rapid increases in alcohol use among Whites might be linked to the European cultural significance of alcohol (Engs, 1995; Kilian et al., 2021). The observed similar patterns of increased alcohol use among Latino and White youth may be in part explained by acculturation. Acculturation describes the adoption or adaptation of values, traditions, behaviors, and language by immigrants in new cultures following entry and settlement into a host country (Berry, 2005). Research indicates acculturation among Latino youth is marked by increased drinking, binge drinking, drinking problems, and alcohol use disorder (Almeida et al., 2012; Karriker-Jaffe and Zemore, 2009; Vaeth et al., 2012; Zemore, 2005, 2007). The high level of alcohol use among Latinos may reflect that youth are adopting U.S. patterns of alcohol use.
Third, our study suggests Latino youth are more likely to use cannabis towards the end of adolescence compared to White and Black youth. This is consistent with prior literature suggesting Latino youth have the highest increase in cannabis use among racial/ethnic groups (Johnson et al., 2019; Watson et al., 2021). It is important to highlight that, in our study, significantly higher proportion of lifetime cannabis use among Latino than White and Black youth was only shown at age 17 and not younger ages during adolescence. This could be the beginning of increased use and continue into young adulthood, hence a critical point for education and prevention. Changes in cannabis-related policies and increased access to cannabis highlight the importance youth-oriented interventions and education in this regard (Hammond et al., 2020; Ladegard et al., 2020). Given that Latino youth is a growing segment of the U.S. adolescent population, patterns and disparities in substance use must be closely monitored to guide evidence-based policies.
Fourth, when considering age, sex, and race/ethnicity, Latino boys were identified as a particularly susceptible sub-population, as they showed the most drastic increase in lifetime use of alcohol and cannabis from age 12 to 17. Of note, this interpretation is preliminary and must be examined in more targeted and well-designed studies, as the slopes of the regression lines were not significantly different between the six sex-race/ethnicity groups, but a consistent pattern was observed. Research on adult Latinos suggests that alcohol consumption decreases with age (Ramisetty-Mikler et al., 2010), indicating that existing interventions such as educational campaigns should continue to target Latinos, especially boys, and must be expanded to include cannabis and other drugs as well.
Our study had several limitations that must be considered when interpreting the results. Cross-sectional data from one NSDUH survey were analyzed and, therefore, longitudinal trends across different years or generations could not be assessed. Although NSDUH is one of the largest nationwide surveys, it is limited to the U.S. Youth perception and use of alcohol and cannabis is greatly impacted by factors such as social norms, legal practices, and cultural differences (Anthony et al., 2017; Carpenter and Dobkin, 2015; Rafei et al., 2023; Room and Mäkelä, 2000; Sudhinaraset et al., 2016; Tedor, 2021; Wanke et al., 2022). Therefore, our results may not be generalizable without conducting similar and more sophisticated analyses in other countries/regions or global surveys, (Saewyc, 2021; WHO, Global school-based student health survey). While sex differences in the use of alcohol and other substance have been investigated and reported from different parts of the world, studying race/ethnicity differences, especially those reported here, are more applicable and relevant to the U.S. The categories used are far from perfect and mainly used for sociopolitical purposes of the U.S. Census and government reports. Race and ethnicity are social, not biological, constructs. Health disparities in this regard generally reflect bigger issues such as structural racism, environmental injustice, and access to care (Bauchner, 2015; Flanagin et al., 2021; Ioannidis et al., 2021; Pérez-Stable and Rodriquez, 2020; Pérez-Stable and Webb Hooper, 2021; Williams and Rucker, 2000; Williams and Sternthal, 2010). We only included three racial/ethnic categories with the largest numbers in this work (non-Hispanic White, non-Hispanic Black, and Hispanic/Latino). More comprehensive work needs to be done to include individuals from other racial/ethnic backgrounds, as well as those who self-identify as belonging to more than one group. In addition, although we investigated differences in alcohol and cannabis use by sex and race/ethnicity, we did not explore within-group heterogeneity. Given that these groupings may only be an imperfect proxy of broader disparities, future studies should include more fine-grained information and examine interactions between different demographic and societal factors to better inform public health policy and advocacy efforts around adolescent alcohol and cannabis use. Future research should also investigate the efficacy and implementation of prevention efforts aimed at the primary social and structural drivers of health disparities, including those that influence the development, progression, and outcome of substance use.
Our findings invigorate further research to explore mechanisms and risk factors that might predict subsequent substance use and substance use disorder development into adulthood. Findings from longitudinal studies, such as the ongoing Adolescent Brain Cognitive Development (ABCD) study, will complement this body of knowledge by providing prospective information about the timing of exposures and substance use (Volkow et al., 2018). Longitudinal studies can help identify factors that increase risk for early initiation of alcohol and cannabis use and how early use shapes risk for adverse outcomes in adulthood. Findings can also place contemporary patterns of use into a historical context by comparing estimates with what has been observed for previous generations to indicate whether there is a trend toward earlier or later ages of use (Brown et al., 2008; Twenge and Park, 2019). It is important to note that we applied an age-at-assessment, not age-of-onset, approach by analyzing age-specific proportions who reported lifetime/ever use (Cheng et al., 2018).
Use of alcohol and cannabis in adolescence threatens healthy development and increases risk for a host of adverse outcomes (Karoly et al., 2020; Lees et al., 2021; Meruelo et al., 2017). Prevention of adolescent substance use is a global priority; one of the United Nation's sustainable development goals (SDGs) is to “strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol” (WHO). If we are to achieve SDG health targets on adolescent substance use, descriptive epidemiological studies are needed around the globe to inform regional policies and practices. While findings of this study are unlikely to change current policies or practices in the public health or clinical sector, collective evidence in this regard could have important implications. Findings on subgroup differences, like those presented in this report, can be used to refine strategies for primary prevention of substance use, particularly with regard to timing of interventions and tailoring strategies to specific groups.
CRediT authorship contribution statement
Mehdi Farokhnia: Conceptualization, Methodology, Formal analysis, Writing – original draft, Visualization, Supervision, Project administration. Julia C. Harris: Writing – original draft, Visualization. Shannon N. Speed: Writing – review & editing. Lorenzo Leggio: Writing – review & editing, Funding acquisition. Renee M. Johnson: Conceptualization, Validation, Writing – original draft, Supervision.
Declaration of Competing Interest
The authors have no conflicts of interest to declare.
Acknowledgments
Funding
MF, SNS, and LL are supported by NIH intramural funding (ZIA-DA-000635, joint NIDA and NIAAA).
Acknowledgement
We would like to thank Garrick Sherman, Ph.D., Biostatistician at the Office of the Clinical Director, NIDA Intramural Research Program, for statistical support.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dadr.2023.100214.
Appendix. Supplementary materials
References
- Agrawal A., Lynskey M.T. Does gender contribute to heterogeneity in criteria for cannabis abuse and dependence? Results from the national epidemiological survey on alcohol and related conditions. Drug Alcohol Depend. 2007;88(2–3):300–307. doi: 10.1016/j.drugalcdep.2006.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahuja M., Awasthi M., Gim S., Records K., Cimilluca J., Al-Ksir K., Tremblay J., Doshi R.P., Sathiyasaleen T., Fernandopulle P. Early age of cannabis initiation and its association with suicidal behaviors. Subst. Abuse. 2022;16 doi: 10.1177/11782218221116731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcover K.C., Lyons A.J., Oluwoye O., Muse I.D., Kelly M.E., McDonell M.G. Onset of alcohol use disorder among alcohol initiates by race/ethnicity. Alcohol. 2021;97:13–21. doi: 10.1016/j.alcohol.2021.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida J., Johnson R.M., Matsumoto A., Godette D.C. Substance use, generation and time in the United States: the modifying role of gender for immigrant urban adolescents. Soc. Sci. Med. 2012;75(12):2069–2075. doi: 10.1016/j.socscimed.2012.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anthony J.C., Lopez-Quintero C., Alshaarawy O. Cannabis epidemiology: a selective review. Curr. Pharm. Des. 2017;22(42):6340–6352. doi: 10.2174/1381612822666160813214023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batalla A., Bhattacharyya S., Yücel M., Fusar-Poli P., Crippa J.A., Nogué S., Torrens M., Pujol J., Farré M., Martin-Santos R. Structural and functional imaging studies in chronic cannabis users: a systematic review of adolescent and adult findings. PLoS ONE. 2013;8(2):e55821. doi: 10.1371/journal.pone.0055821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauchner H. Race, poverty, and medicine in the United States. JAMAJAMA. 2015;313(14):1423. doi: 10.1001/jama.2015.2262. [DOI] [PubMed] [Google Scholar]
- Becker J.B. Sex differences in addiction. Dialogues Clin. Neurosci. 2016;18(4):395–402. doi: 10.31887/DCNS.2016.18.4/jbecker. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry J.W. Acculturation: living successfully in two cultures. Int. J. Intercultural Relat. 2005;29:697–712. [Google Scholar]
- Beverly H.K., Castro Y., Opara I. Age of first marijuana use and its impact on education attainment and employment status. J. Drug Issues. 2019;49(2):228–237. doi: 10.1177/0022042618823007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchard L.M., Shin S.H., Chartier K.G. In: The Handbook of Alcohol Use. Frings D., Albery I.P., editors. Academic Press; 2021. Chapter 19 - Alcohol use in adolescence across U.S. race/ethnicity: considering cultural factors in prevention and interventions; pp. 419–451. [Google Scholar]
- Brown S.A., McGue M., Maggs J., Schulenberg J., Hingson R., Swartzwelder S., Martin C., Chung T., Tapert S.F., Sher K., Winters K.C., Lowman C., Murphy S. A developmental perspective on alcohol and youths 16 to 20 years of age. PediatricsPediatrics. 2008;121(Suppl 4):S290–S310. doi: 10.1542/peds.2007-2243D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmann A.F., Schmid B., Blomeyer D., Becker K., Treutlein J., Zimmermann U.S., Jennen-Steinmetz C., Schmidt M.H., Esser G., Banaschewski T., Rietschel M., Schumann G., Laucht M. Impact of age at first drink on vulnerability to alcohol-related problems: testing the marker hypothesis in a prospective study of young adults. J. Psychiatr. Res. 2009;43(15):1205–1212. doi: 10.1016/j.jpsychires.2009.02.006. [DOI] [PubMed] [Google Scholar]
- Buchmann A.F., Schmid B., Blomeyer D., Zimmermann U.S., Jennen-Steinmetz C., Schmidt M.H., Esser G., Banaschewski T., Mann K., Laucht M. Drinking against unpleasant emotions: possible outcome of early onset of alcohol use? Alcohol Clin. Exp. Res. 2010;34(6):1052–1057. doi: 10.1111/j.1530-0277.2010.01180.x. [DOI] [PubMed] [Google Scholar]
- Carpenter C., Dobkin C. The minimum legal drinking age and crime. Rev Econ Stat. 2015;97(2):521–524. doi: 10.1162/REST_a_00489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C.Y., Storr C.L., Anthony J.C. Early-onset drug use and risk for drug dependence problems. Addict. Behav. 2009;34(3):319–322. doi: 10.1016/j.addbeh.2008.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng H.G., Anthony J.C. A new era for drinking? Epidemiological evidence on adolescent male-female differences in drinking incidence in the United States and Europe. Soc. Psychiatry Psychiatr. Epidemiol. 2017;52(1):117–126. doi: 10.1007/s00127-016-1318-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng H.G., Cantave M.D., Anthony J.C. Taking the first full drink: epidemiological evidence on male-female differences in the United States. Alcohol Clin. Exp. Res. 2016;40(4):816–825. doi: 10.1111/acer.13028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng H.G., Lopez-Quintero C., Anthony J.C. Age of onset or age at assessment-that is the question: estimating newly incident alcohol drinking and rapid transition to heavy drinking in the United States, 2002-2014. Int. J. Methods Psychiatr. Res. 2018;27(1) doi: 10.1002/mpr.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton W.M., Grant B.F., Colliver J.D., Glantz M.D., Stinson F.S. Prevalence of marijuana use disorders in the United States: 1991-1992 and 2001-2002. JAMAJAMA. 2004;291(17):2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- Cooper Z.D., Haney M. Investigation of sex-dependent effects of cannabis in daily cannabis smokers. Drug Alcohol Depend. 2014;136:85–91. doi: 10.1016/j.drugalcdep.2013.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWit David J., Ph.D., Adlaf Edward M., Ph.D., Offord David R., M.D., Ogborne Alan C., Ph.D. Age at first alcohol use: a risk factor for the development of alcohol disorders. Am. J. Psychiatry. 2000;157(5):745–750. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- Engs R.C. Do traditional western European drinking practices have origins in antiquity? Addict. Res. 1995;2(3):227–239. [Google Scholar]
- Enstad F., Evans-Whipp T., Kjeldsen A., Toumbourou J.W., von Soest T. Predicting hazardous drinking in late adolescence/young adulthood from early and excessive adolescent drinking - a longitudinal cross-national study of Norwegian and Australian adolescents. BMC Public Health. 2019;19(1):790. doi: 10.1186/s12889-019-7099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Polce R.J., Vasilenko S.A., Lanza S.T. Changes in gender and racial/ethnic disparities in rates of cigarette use, regular heavy episodic drinking, and marijuana use: ages 14 to 32. Addict. Behav. 2015;41:218–222. doi: 10.1016/j.addbeh.2014.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairman B.J. Trends in registered medical marijuana participation across 13 US states and District of Columbia. Drug Alcohol Depend. 2016;159:72–79. doi: 10.1016/j.drugalcdep.2015.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagin A., Frey T., Christiansen S.L., Committee A.M.o.S. Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMAJAMA. 2021;326(7):621–627. doi: 10.1001/jama.2021.13304. [DOI] [PubMed] [Google Scholar]
- GBD 2016 Alcohol and Drug Use Collaborators The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5(12):987–1012. doi: 10.1016/S2215-0366(18)30337-7. https://pubmed.ncbi.nlm.nih.gov/30392731/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gräfe E.L., Reid H.M.O., Shkolnikov I., Conway K., Kit A., Acosta C., Christie B.R. Women are taking the hit: examining the unique consequences of cannabis use across the female lifespan. Front. Neuroendocrinol. 2023 doi: 10.1016/j.yfrne.2023.101076. [DOI] [PubMed] [Google Scholar]
- Grant B.F., Chou S.P., Saha T.D., Pickering R.P., Kerridge B.T., Ruan W.J., Huang B., Jung J., Zhang H., Fan A., Hasin D.S. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry. 2017;74(9):911–923. doi: 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant J.D., Scherrer J.F., Neuman R.J., Todorov A.A., Price R.K., Bucholz K.K. A comparison of the latent class structure of cannabis problems among adult men and women who have used cannabis repeatedly. Addiction. 2006;101(8):1133–1142. doi: 10.1111/j.1360-0443.2006.01463.x. [DOI] [PubMed] [Google Scholar]
- Grigsby T.J., Lopez A., Albers L., Rogers C.J., Forster M. A scoping review of risk and protective factors for negative cannabis use consequences. Subst. Abuse. 2023;17 doi: 10.1177/11782218231166622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W., Lynskey M. Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction. 2016;111(10):1764–1773. doi: 10.1111/add.13428. [DOI] [PubMed] [Google Scholar]
- Hammond C.J., Chaney A., Hendrickson B., Sharma P. Cannabis use among U.S. adolescents in the era of marijuana legalization: a review of changing use patterns, comorbidity, and health correlates. Int. Rev. Psychiatry. 2020;32(3):221–234. doi: 10.1080/09540261.2020.1713056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris J.C., Mereish E.H., Faulkner M.L., Assari S., Choi K., Leggio L., Farokhnia M. Racial differences in the association between alcohol drinking and cigarette smoking: preliminary findings from an alcohol research program. Alcohol. 2022;57(3):330–339. doi: 10.1093/alcalc/agab038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D.S., Kerridge B.T., Saha T.D., Huang B., Pickering R., Smith S.M., Jung J., Zhang H., Grant B.F. Prevalence and correlates of DSM-5 cannabis use disorder, 2012-2013: findings from the national epidemiologic survey on alcohol and related conditions-III. Am. J. Psychiatry. 2016;173(6):588–599. doi: 10.1176/appi.ajp.2015.15070907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawke L.D., Wilkins L., Henderson J. Early cannabis initiation: substance use and mental health profiles of service-seeking youth. J. Adolesc. 2020;83:112–121. doi: 10.1016/j.adolescence.2020.06.004. [DOI] [PubMed] [Google Scholar]
- Hingson R.W., Zha W. Age of drinking onset, alcohol use disorders, frequent heavy drinking, and unintentionally injuring oneself and others after drinking. Pediatrics. 2009;123(6):1477–1484. doi: 10.1542/peds.2008-2176. [DOI] [PubMed] [Google Scholar]
- Huang C.Y., Connell C.M. Racial/ethnic differences in alcohol use trajectories among adolescents involved in child welfare. Am. J. Orthopsychiatry. 2019;89(4):524–533. doi: 10.1037/ort0000375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurlocker M., Madson M.B., Lui P.P., Dvorak R., Ham L.S., Leffingwell T., Looby A., Meier E., Montes K., Napper L.E., Prince M.A., Skewes M., Zamboanga B.L. Mental health risk profiles and related substance use during coronavirus pandemic among college students who use substances. Int. J. Ment. Health Addict. 2022:1–18. doi: 10.1007/s11469-022-00813-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis J.P.A., Powe N.R., Yancy C. Recalibrating the use of race in medical research. JAMAJAMA. 2021;325(7):623–624. doi: 10.1001/jama.2021.0003. [DOI] [PubMed] [Google Scholar]
- Jayathilaka R., Athukorala O., Ishara S., Silva D., Pathirage T. Alcohol brings burdens: a global and continent wise study on alcohol consumption and global burden of diseases. PLoS ONE. 2022;17(7) doi: 10.1371/journal.pone.0270998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R.M., Fairman B., Gilreath T., Xuan Z., Rothman E.F., Parnham T., Furr-Holden C.D.M. Past 15-year trends in adolescent marijuana use: differences by race/ethnicity and sex. Drug Alcohol Depend. 2015;155:8–15. doi: 10.1016/j.drugalcdep.2015.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R.M., Fleming C.B., Cambron C., Dean L.T., Brighthaupt S.C., Guttmannova K. Race/ethnicity differences in trends of marijuana, cigarette, and alcohol use among 8th, 10th, and 12th graders in Washington State, 2004-2016. Prev. Sci. 2019;20(2):194–204. doi: 10.1007/s11121-018-0899-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston, L.D., Miech, R.A., Patrick, M.E., O'Malley, P.M., Schulenberg, J.E., Bachman, J.G., 2023. Monitoring the Future national survey results on drug use 1975-2022: overview, key findings on adolescent drug use. https://monitoringthefuture.org/results/annual-reports/.
- Karoly H.C., Ross J.M., Ellingson J.M., Feldstein Ewing S.W. Exploring cannabis and alcohol co-use in adolescents: a narrative review of the evidence. J. Dual Diagn. 2020;16(1):58–74. doi: 10.1080/15504263.2019.1660020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe K.J., Zemore S.E. Associations between acculturation and alcohol consumption of Latino men in the United States. J. Stud. Alcohol Drugs. 2009;70(1):27–31. doi: 10.15288/jsad.2009.70.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K.M., Kaur N., Kreski N.T., Chen Q., Martins S.S., Hasin D., Olfson M., Mauro P.M. Temporal trends in alcohol, cannabis, and simultaneous use among 12th-grade U.S. adolescents from 2000 to 2020: differences by sex, parental education, and race and ethnicity. Alcohol Clin. Exp. Res. 2022;46(9):1677–1686. doi: 10.1111/acer.14914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K.M., Wall M., Feng T., Cerdá M., Hasin D.S. Race/ethnicity and marijuana use in the United States: diminishing differences in the prevalence of use, 2006-2015. Drug Alcohol Depend. 2017;179:379–386. doi: 10.1016/j.drugalcdep.2017.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilian C., Manthey J., Kraus L., Mäkelä P., Moskalewicz J., Sieroslawski J., Rehm J. A new perspective on European drinking cultures: a model-based approach to determine variations in drinking practices among 19 European countries. Addiction. 2021;116(8):2016–2025. doi: 10.1111/add.15408. [DOI] [PubMed] [Google Scholar]
- Kozak K., P H.S., Lowe D.J.E., Weinberger A.H., Cooper Z.D., Rabin R.A., George T.P. A systematic review and meta-analysis of sex differences in cannabis use disorder amongst people with comorbid mental illness. Am. J. Drug Alcohol Abuse. 2021;47(5):535–547. doi: 10.1080/00952990.2021.1946071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladegard K., Thurstone C., Rylander M. Marijuana Legalization and Youth. Pediatrics. 2020;145(Suppl 2):S165–s174. doi: 10.1542/peds.2019-2056D. [DOI] [PubMed] [Google Scholar]
- Lee M.H., Kim-Godwin Y.S., Hur H. Race/ethnicity differences in risk and protective factors for marijuana use among U.S. adolescents. BMC Public Health. 2021;21(1):1167. doi: 10.1186/s12889-021-11159-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lees B., Debenham J., Squeglia L.M. Alcohol and cannabis use and the developing brain. Alcohol Res. 2021;41(1):11. doi: 10.35946/arcr.v41.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins S.S., Segura L.E., Levy N.S., Mauro P.M., Mauro C.M., Philbin M.M., Hasin D.S. Racial and ethnic differences in cannabis use following legalization in US states with medical cannabis Laws. JAMA Netw. Open. 2021;4(9) doi: 10.1001/jamanetworkopen.2021.27002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade J. Mental health effects of the COVID-19 pandemic on children and adolescents: a review of the current research. Pediatr. Clin. North Am. 2021;68(5):945–959. doi: 10.1016/j.pcl.2021.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meruelo A.D., Castro N., Cota C.I., Tapert S.F. Cannabis and alcohol use, and the developing brain. Behav. Brain Res. 2017;325(Pt A):44–50. doi: 10.1016/j.bbr.2017.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millar S.R., Mongan D., Smyth B.P., Perry I.J., Galvin B. Relationships between age at first substance use and persistence of cannabis use and cannabis use disorder. BMC Public Health. 2021;21(1):997. doi: 10.1186/s12889-021-11023-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller J.W., Naimi T.S., Brewer R.D., Jones S.E. Binge drinking and associated health risk behaviors among high school students. PediatricsPediatrics. 2007;119(1):76–85. doi: 10.1542/peds.2006-1517. [DOI] [PubMed] [Google Scholar]
- Mpofu J.J., Underwood J.M., Thornton J.E., Brener N.D., Rico A., Kilmer G., Harris W.A., Leon-Nguyen M., Chyen D., Lim C., Mbaka C.K., Smith-Grant J., Whittle L., Jones S.E., Krause K.H., Li J., Shanklin S.L., McKinnon I., Arrey L., Queen B.E., Roberts A.M. Overview and methods for the youth risk behavior surveillance system - United States, 2021. MMWR. 2023;72(1):1–12. doi: 10.15585/mmwr.su7201a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NSDUH, National Survey on Drug Use and Health (NSDUH). https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health.
- Pacula R.L., Jacobson M., Maksabedian E.J. In the weeds: a baseline view of cannabis use among legalizing states and their neighbours. Addiction. 2016;111(6):973–980. doi: 10.1111/add.13282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Stable E.J., Rodriquez E.J. Social determinants and differences in mortality by race/ethnicity. JAMA Netw. Open. 2020;3(2) doi: 10.1001/jamanetworkopen.2019.21392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Stable E.J., Webb Hooper M. Acknowledgment of the legacy of racism and discrimination. Ethn. Dis. 2021;31(Suppl 1):289–292. doi: 10.18865/ed.31.S1.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope H.G., Jr., Gruber A.J., Hudson J.I., Cohane G., Huestis M.A., Yurgelun-Todd D. Early-onset cannabis use and cognitive deficits: what is the nature of the association? Drug Alcohol Depend. 2003;69(3):303–310. doi: 10.1016/s0376-8716(02)00334-4. [DOI] [PubMed] [Google Scholar]
- Quigley J.A., Logsdon M.K., Turner C.A., Gonzalez I.L., Leonardo N.B., Becker J.B. Sex differences in vulnerability to addiction. NeuropharmacologyNeuropharmacology. 2021;187 doi: 10.1016/j.neuropharm.2021.108491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafei P., Englund A., Lorenzetti V., Elkholy H., Potenza M.N., Baldacchino A.M. Transcultural aspects of cannabis use: a descriptive overview of cannabis use across cultures. Curr. Addict. Rep. 2023;10(3):458–471. [Google Scholar]
- Ramisetty-Mikler S., Caetano R., Rodriguez L.A. The Hispanic Americans Baseline Alcohol Survey (HABLAS): alcohol consumption and sociodemographic predictors across Hispanic national groups. J. Subst. Use. 2010;15(6):402–416. doi: 10.3109/14659891003706357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Room R., Mäkelä K. Typologies of the cultural position of drinking. J. Stud. Alcohol. 2000;61(3):475–483. doi: 10.15288/jsa.2000.61.475. [DOI] [PubMed] [Google Scholar]
- Saewyc E. The next phase of the global early adolescent study: measuring how gender norms and gender inequality intensify and influence health. J. Adolescent Health. 2021;69(1):S1–S2. doi: 10.1016/j.jadohealth.2021.04.003. [DOI] [PubMed] [Google Scholar]
- SAMHDA, Substance Abuse and Mental Health Data Archive (SAMHDA). https://www.datafiles.samhsa.gov/.
- SAMHSA, 2019. National Survey on Drug Use and Health (2019): detailed Tables. https://www.samhsa.gov/data/report/2019-nsduh-detailed-tables.
- SAMHSA, 2021. National Survey on Drug Use and Health (2021): detailed Tables. https://www.samhsa.gov/data/report/2021-nsduh-detailed-tables.
- Sartor C.E., Jackson K.M., McCutcheon V.V., Duncan A.E., Grant J.D., Werner K.B., Bucholz K.K. Progression from first drink, first intoxication, and regular drinking to alcohol use disorder: a comparison of African American and European American Youth. Alcohol Clin. Exp. Res. 2016;40(7):1515–1523. doi: 10.1111/acer.13113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler M.S., Tucker J.S., Pedersen E.R., D'Amico E.J. Relative influence of perceived peer and family substance use on adolescent alcohol, cigarette, and marijuana use across middle and high school. Addict. Behav. 2019;88:99–105. doi: 10.1016/j.addbeh.2018.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senay E.C. Drug abuse and public health. A global perspective. Drug Saf. 1991;1:1–65. [PubMed] [Google Scholar]
- Shao H., Du H., Gan Q., Ye D., Chen Z., Zhu Y., Zhu S., Qu L., Lu J., Li Y., Duan J., Gu Y., Chen M. Trends of the global burden of disease attributable to cannabis use disorder in 204 countries and territories, 1990-2019: results from the disease burden study 2019. Int. J. Ment. Health Addict. 2023:1–23. doi: 10.1007/s11469-022-00999-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro G.K., Buckley-Hunter L. What every adolescent needs to know: cannabis can cause psychosis. J. Psychosom. Res. 2010;69(6):533–539. doi: 10.1016/j.jpsychores.2010.04.002. [DOI] [PubMed] [Google Scholar]
- Sise C.B., Sack D.I., Sise M.J., Riccoboni S.T., Osler T.M., Swanson S.M., Martinez M.D. Alcohol and high-risk behavior among young first-time offenders. J. Trauma. 2009;67(3):498–502. doi: 10.1097/TA.0b013e3181b19282. [DOI] [PubMed] [Google Scholar]
- Squeglia L.M. Alcohol and the developing adolescent brain. World Psychiatry. 2020;19(3):393–394. doi: 10.1002/wps.20786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudhinaraset M., Wigglesworth C., Takeuchi D.T. Social and cultural contexts of alcohol use: influences in a social-ecological framework. Alcohol Res. 2016;38(1):35–45. [PMC free article] [PubMed] [Google Scholar]
- Sullivan R.M., Wade N.E., Wallace A.L., Tapert S.F., Pelham W.E., Brown S.A., Cloak C.C., Ewing S.W.F., Madden P.A.F., Martz M.E., Ross J.M., Kaiver C.M., Wirtz H.G., Heitzeg M.M., Lisdahl K.M. Substance use patterns in 9 to 13-year-olds: longitudinal findings from the Adolescent Brain Cognitive Development (ABCD) study. Drug Alcohol Dependence Rep. 2022;5 doi: 10.1016/j.dadr.2022.100120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedor M.F. In: The Handbook of Alcohol Use. Frings D., Albery I.P., editors. Academic Press; 2021. Chapter 16 - Alcohol consumption and cultural systems: global similarities and differences; pp. 355–378. [Google Scholar]
- Temple J.R., Baumler E., Wood L., Guillot-Wright S., Torres E., Thiel M. The impact of the COVID-19 pandemic on adolescent mental health and substance use. J. Adolesc. Health. 2022;71(3):277–284. doi: 10.1016/j.jadohealth.2022.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry-McElrath Y.M., Patrick M.E. U.S. adolescent alcohol use by race/ethnicity: consumption and perceived need to reduce/stop use. J. Ethn. Subst. Abuse. 2020;19(1):3–27. doi: 10.1080/15332640.2018.1433094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trujillo C.A., Obando D., Trujillo A. An examination of the association between early initiation of substance use and interrelated multilevel risk and protective factors among adolescents. PLoS ONE. 2019;14(12) doi: 10.1371/journal.pone.0225384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge J.M., Park H. The decline in adult activities among U.S. adolescents, 1976-2016. Child Dev. 2019;90(2):638–654. doi: 10.1111/cdev.12930. [DOI] [PubMed] [Google Scholar]
- Vaeth P.A., Caetano R., Rodriguez L.A. The Hispanic Americans Baseline Alcohol Survey (HABLAS): the association between acculturation, birthplace and alcohol consumption across Hispanic national groups. Addict. Behav. 2012;37(9):1029–1037. doi: 10.1016/j.addbeh.2012.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D., Han B., Einstein E.B., Compton W.M. Prevalence of substance use disorders by time since first substance use among young people in the US. JAMA Pediatr. 2021;175(6):640–643. doi: 10.1001/jamapediatrics.2020.6981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D., Koob G.F., Croyle R.T., Bianchi D.W., Gordon J.A., Koroshetz W.J., Pérez-Stable E.J., Riley W.T., Bloch M.H., Conway K., Deeds B.G., Dowling G.J., Grant S., Howlett K.D., Matochik J.A., Morgan G.D., Murray M.M., Noronha A., Spong C.Y., Wargo E.M., Warren K.R., Weiss S.R.B. The conception of the ABCD study: from substance use to a broad NIH collaboration. Dev. Cogn. Neurosci. 2018;32:4–7. doi: 10.1016/j.dcn.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D., Swanson J.M., Evins A.E., DeLisi L.E., Meier M.H., Gonzalez R., Bloomfield M.A., Curran H.V., Baler R. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: a review. JAMA Psychiatry. 2016;73(3):292–297. doi: 10.1001/jamapsychiatry.2015.3278. [DOI] [PubMed] [Google Scholar]
- Wagner F.A., Anthony J.C. Male-female differences in the risk of progression from first use to dependence upon cannabis, cocaine, and alcohol. Drug Alcohol Depend. 2007;86(2–3):191–198. doi: 10.1016/j.drugalcdep.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Wanke M., Sandberg S., Macit R., Gülerce H. Culture matters! Changes in the global landscape of cannabis. Drugs. 2022;29(4):317–322. [Google Scholar]
- Watson C.V., Puvanesarajah S., Trivers K.F. Racial and ethnic differences in marijuana use in e-cigarettes among US youth in 2017, 2018, and 2020. JAMA Pediatr. 2021;175(7):746–748. doi: 10.1001/jamapediatrics.2021.0305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A., Castle I.J., Chen C.M., Shirley M., Roach D., Hingson R. Converging patterns of alcohol use and related outcomes among females and males in the United States, 2002 to 2012. Alcohol Clin. Exp. Res. 2015;39(9):1712–1726. doi: 10.1111/acer.12815. [DOI] [PubMed] [Google Scholar]
- White A.M. Gender differences in the epidemiology of alcohol use and related harms in the United States. Alcohol Res. 2020;40(2):01. doi: 10.35946/arcr.v40.2.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, Alcohol, Drugs and Addictive Behaviours Unit - Cannabis. https://www.who.int/teams/mental-health-and-substance-use/alcohol-drugs-and-addictive-behaviours/drugs-psychoactive/cannabis.
- WHO, Sustainable Development Goals (SDGs) and alcohol. https://www.who.int/teams/mental-health-and-substance-use/alcohol-drugs-and-addictive-behaviours/alcohol/governance/sdgs.
- WHO, Global School-Based Student Health Survey. https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/global-school-based-student-health-survey.
- WHO . Global Status Report On Alcohol and Health 2018. World Health Organization; Geneva: 2018. https://www.who.int/publications/i/item/9789241565639 [Google Scholar]
- Williams D.R., Rucker T.D. Understanding and addressing racial disparities in health care. Health Care Financ. Rev. 2000;21(4):75–90. [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J. Health Soc. Behav. 2010;51(Suppl):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters K.C., Lee C.Y. Likelihood of developing an alcohol and cannabis use disorder during youth: association with recent use and age. Drug Alcohol Depend. 2008;92(1–3):239–247. doi: 10.1016/j.drugalcdep.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore S.E. Re-examining whether and why acculturation relates to drinking outcomes in a rigorous, national survey of Latinos. Alcohol Clin. Exp. Res. 2005;29(12):2144–2153. doi: 10.1097/01.alc.0000191775.01148.c0. [DOI] [PubMed] [Google Scholar]
- Zemore S.E. Acculturation and alcohol among Latino adults in the United States: a comprehensive review. Alcohol Clin. Exp. Res. 2007;31(12):1968–1990. doi: 10.1111/j.1530-0277.2007.00532.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.