Abstract
Background/Objective
The purpose of this study was to find factors indicating the occurrence of the Segond fracture, a specific type of anterolateral ligament injury.
Methods
From January 2015 to December 2017, we retrospectively reviewed the medical records of patients diagnosed with acute anterior cruciate ligament (ACL) injury who underwent reconstruction within 90 days of injury. Diagnosis of the Segond fracture was determined either by magnetic resonance imaging or plain radiographs. Factors examined were: age at surgery, sex, body mass index (kg/m2), status of menisci, and activities led to ACL injury. After univariate screening, multivariate logistic regression analyses were performed. Patients were divided into four groups based on the presence of lateral meniscal (LM) and/or medial meniscal (MM) injuries and compared with respect to the occurrence of Segond fractures.
Results
A total of 375 patients were included (163 males, 212 females), with mean age 25.8 years old. Among them, 22 of 375 (5.9 %) had a Segond fracture. We identified injured lateral menisci (adjusted odds ratio (aOR), 3.029; 95 % Confidence Interval (CI), 1.206–7.609; P = 0.018), intact medial menisci (aOR, 0.229; 95 % CI, 0.065–0.810; P = 0.022), and higher body mass index (aOR, 1.102; 95 % CI, 1.008–1.205; P = 0.034) as factors indicative of the occurrence of Segond fracture. LM injury without MM injury suggested the existence of a Segond fracture.
Conclusion
LM injury without a MM injury indicated the occurrence of a Segond fracture. Higher body mass index also increased the risk for Segond fracture occurrence.
Keywords: Anterior cruciate ligament injury, Anterolateral ligament, Lateral meniscal injury, Medial meniscal injury, Risk factors, Segond fracture
1. Introduction
The Segond fracture is a well-known radiographic sign that indicates anterior cruciate ligament (ACL) injury. In the past, orthopaedic surgeons used the Segond fracture as a sign to assist in the diagnosis of ACL injury, but the emergence of magnetic resonance imaging (MRI) has made this radiographic sign less important in terms of diagnosis. Circumstances dramatically changed in 2012 and 2013 when the importance of the anterolateral ligament (ALL) started to gain attention among knee surgeons via anatomical studies.1,2 Subsequent biomechanical studies showed the crucial role of the ALL, especially under the ACL-deficient condition, in maintaining antero-posterior and rotatory stability of the knee joint.3, 4, 5, 6 Orthopaedic surgeons specializing in ACL reconstruction (ACLR) had long been aware that a certain subset of patients showed residual rotatory instability following reconstruction. As their understanding of the anatomical and biomechanical properties of the ALL evolved, surgeons strived to reduce this instability by augmenting the antero-lateral structure.6,7
During this period, the Segond fracture was increasing being perceived as a representative type of ALL injury, (i.e., an avulsion fracture of the ALL attachment to the tibia) which resulted in renewed clinical importance. Some knee surgeons thought of the lesion as an indicator for surgical reconstruction of the ALL.8, 9, 10, 11, 12
Although radiographic diagnosis of the Segond fracture is less difficult, not all the lesions could be detected on radiography. Kumahara et al. reported 4 out of 22 cases were detected only using computed tomography (CT).13 Moreover, given the remarkable healing potential of the Segond fracture, its detection becomes increasingly challenging as time elapses. When designing the present study, we anticipated that any secondary findings accompanying the Segond fracture would aid in both the diagnosis and surgical planning of ACLR. Several recent studies have brought to light variations in the frequency of meniscal injuries between knees with or without the Segond fracture. Age, sex, and body mass index (BMI) were also reported to be correlated with the occurrence of Segond fractures.14,15
The purpose of this study, therefore, was to identify possible factors, including meniscal injuries, that could serve as indicators of the Segond fracture. Our hypothesis was that the absence or existence of lateral meniscal (LM) and medial meniscal (MM) injuries, along with other factors, could indicate the occurrence of a Segond fracture.
2. Materials and methods
2.1. Patient selection
This research has been approved by the IRB of the authors’ affiliated institutions. This study was performed in line with the principles of the Declaration of Helsinki, and informed consent was obtained from all patients.
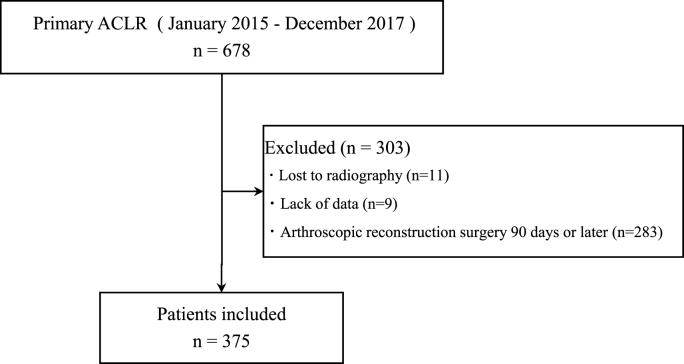
Patients diagnosed with acute ACL injury and who underwent arthroscopic reconstruction at the participating institutions from January 2015 to December 2017 (36 months) were retrospectively considered for the present study. The inclusion criteria were: no more than 90 days from injury to surgery and age more than 18 years old. The exclusion criteria included previous ACL reconstruction in which accompanying meniscal procedures were often carried out and lack of demographic and clinical data or imaging results (Fig. 1).
Fig. 1.
Flow diagram of patients.
The medical records were reviewed to determine patient-specific factors, including age at surgery, sex, BMI (kg/m2), meniscal surgery record, time from injury to surgery, time from injury to MRI, time from injury to plain radiography, and cause of injury classified into: contact sports, non-contact sports, or accident.
2.2. Image analysis
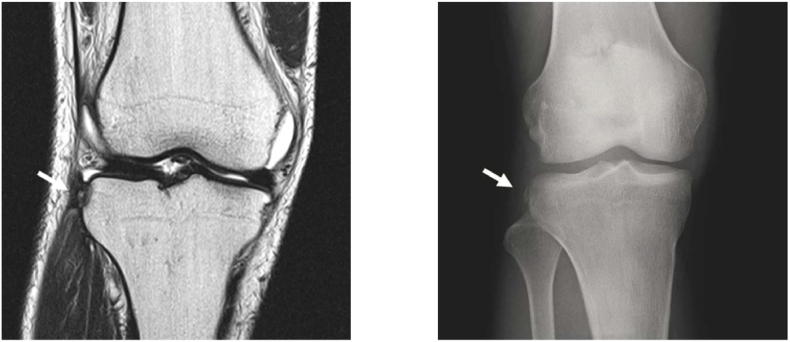
MRI and plain radiographs of the patient's knee were retrospectively reviewed. All imaging analyses were performed by two orthopaedic surgeons with over 10 years of experience in musculoskeletal imaging analysis. The examiners were blinded to the patient demographics and clinical outcomes. To assess the intra- and inter-rater reliability, all imaging analyses were performed twice by the same observer at more than 6-week intervals. The Segond fracture was judged as present when both readers reached consensus based on either MRI or plain radiographs (Fig. 2).
Fig. 2.
The Segond fracture
The Segond fracture, i.e., avulsion fracture of the lateral condyle of the tibia (white arrow), was detected on MRI (left, T2-weighed coronal image) or on the radiograph (right).
2.3. Arthroscopic findings during ACL reconstruction
All patients underwent ACLR under arthroscopy. The anatomical double-bundle ACLR technique using hamstring tendon was performed as described by Muneta et al. and Yasuda et al.16,17 Meniscal injuries, if present, were classified according to the International Knee Documentation Committee (IKDC).18 The location of the meniscus injuries was classified as anterior, middle, or posterior. The morphology of injuries was classified as either longitudinal, horizontal, complex, root, flap, radial, or ramp. Meniscal suturing was performed when the lesion was located within the red-white boundary, except for stable small lesion. The pull-out technique was used for root tears, while tie grip suturing was employed for radial tears. For horizontal tears, a fibrin clot was introduced.19, 20, 21 Unstable lesions in the avascular area were excised. Surgeries were performed by one of two senior knee surgeons.
2.4. Statistical analysis
Data are presented as mean and standard deviation (SD) of continuous data and number and percentage for categorical variables. The unpaired t-test or Mann–Whitney U test were used to compare differences in patient demographics based on the distribution of the data determined by the Shapiro–Wilk test. All patients were classified according to the presence or absence of the Segond fracture, and meniscal lesions were tabulated based on laterality, location, type of tear, and surgical intervention. Evaluation of the relationship between categorical variables was performed using the Chi-squared test or Fisher's exact test, as appropriate.
We performed univariate screening to identify potential predictive factors, selecting candidates for further analysis. These candidate-predictive factors, namely age, sex, BMI, LM injuries, and MM injuries, were selected a priori based on previous literature. Subsequently, a multivariate logistic regression analysis was utilized to assess the risk factors associated with the presence of Segond fractures.
Participants were divided into four groups based on the presence or absence of LM and/or MM injuries and were compared with regard to the occurrence of Segond fractures using the Chi-squared test or Fisher's exact test.
Cohen's kappa coefficient was calculated to assess the intra- and inter-rater reliability for determining the presence or absence of Segond fractures on MRI.22
Statistical analyses were performed using the SAS statistical software package, version 9.4 (SAS Institute, Cary, NC, USA), and P < 0.05 indicated statistical significance. Since this study was an exploratory study, the sample size was not calculated. A post hoc power analysis showed a power of 91.7 % for detecting differences that are suggestive of the existence of a Segond fracture.
3. Results
3.1. Demography and incidence of the Segond fracture
In total, 678 patients diagnosed with acute ACL injury during the study period were considered; patients were excluded due to absence of radiographs (n = 11), lack of data (n = 9), and surgery performed 90 days post-injury (n = 283). Thus, a total of 375 patients were included in the analysis. One hundred and sixty-three patients were male and 212 were female, with ages ranging from 13 to 61 years (mean age = 25.8 years old). The mean time from injury to radiographic imaging and MRI were 5.6 days (0–45 days) and 12.2 days (0–65 days), respectively. The mean time from injury to the reconstruction surgery was 57.3 days (6–90 days).
Among them, 22 of 375 (5.9 %) had a Segond fracture, with 20 cases diagnosed on both MRI and plain radiographs, while the remaining two cases were diagnosed by radiography only. Of the 22 patients, 14 were male and eight were female, which indicated that the Segond fracture occurred at a significantly higher rate in males (P = 0.041).
Thereafter, patients with Segond fractures were classified as group S (n = 22), and patients without the Segond fracture were classified as group N (n = 353) (Table 1).
Table 1.
Demographic data of the patients.
| Variables | Group S (n = 22) | Group N (n = 353) | P Value |
|---|---|---|---|
| Age, y, mean ± SD | 23.5 ± 10.5 | 25.9 ± 11.0 | 0.330 |
| Sex, male:female | 14:8 | 149:204 | 0.041 |
| BMI, kg/m2, mean ± SD | 25.1 ± 5.8 | 23.1 ± 3.5 | 0.123 |
| Time from injury, d, mean ± SD | 62.1 ± 18.5 | 57.0 ± 17.6 | 0.188 |
| Injury mechanism, n (%) | 0.537 | ||
| Contact | 9 (41.0 %) | 64 (18.1 %) | |
| Non-contact | 12 (54.5 %) | 247 (70.0 %) | |
| Accident/fall | 1 (4.5 %) | 12 (3.4 %) | |
| Lateral meniscus injuries, n (%) | 14 (63.6 %) | 149 (42.2 %) | 0.049 |
| Medial meniscus injuries, n (%) | 3 (13.6 %) | 126 (35.7 %) | 0.034 |
Data are presented as mean ± standard deviation (SD) or number of patients (percentage).
Group S: Knees with Segond fracture; Group N: Knees without Segond fracture.
3.2. Injury mechanism
In group S, nine injuries were contact sports injuries, and twelve were non-contact sports injuries. In group N, sixty-four injuries were contact sports injuries, and two hundred forty-seven injuries were non-contact sports injuries. As for the injury mechanism (either Group S or Group N), there was no statistically significant difference between the two groups.
Detailed information on the types of injury was not available for 30 cases (Table 1).
3.3. Consistency of imaging analysis
There was sufficient agreement in the intra-rater reliability for both readers (kappa coefficient = 0.929 and 0.954), and in the inter-rater reliability for determining the presence of Segond fractures (κ = 0.911).
3.4. Factors for the Segond fractures
Factors associated with the presence of Segond fractures were BMI (adjusted odds ratio [aOR], 1.102; 95%CI 1.008–1.205; P = 0.034), LM injuries (aOR, 3.029; 95%CI 1.206–7.609; P = 0.018), and MM injuries (aOR, 0.229; 95%CI 0.065–0.810; P = 0.022) (Table 2).
Table 2.
Multivariate logistic regression analysis: the association between the presence of Segond fracture and clinical factors.
| Risk Factor | Adjusted OR | 95 % CI | P Value |
|---|---|---|---|
| BMI | 1.102 | 1.008–1.205 | 0.034 |
| Lateral meniscus injuries | |||
| Intact | Reference | ||
| Torn | 3.029 | 1.206–7.609 | 0.018 |
| Medial meniscus injuries | |||
| Intact | Reference | ||
| Torn | 0.229 | 0.065–0.810 | 0.022 |
BMI, body mass index; CI, confidence interval; OR, odds ratio.
3.5. Meniscus injuries
In group S, 12 of 22 (54.5 %) participants had LM injuries, whereas 75 of 353 (21.2 %) in group N (P = 0.001). In group S, one of 22 (4.5 %) was a MM injury and 52 of 353 (14.7 %) in group N (P = 0.153). In group S, two of 22 (9.1 %) injuries were bilateral meniscus injuries and 74 of 353 (21.0 %) in group N (P = 0.140). By dividing participants into four groups according to the existence of LM injuries and/or MM injuries, LM injury without MM injury (LM injury alone group) indicated the occurrence of Segond fractures with statistical significance (Table 3).
Table 3.
Meniscus injury rate in ACL injuries.
| Variables | Group S (n = 22) | Group N (n = 353) | P Value |
|---|---|---|---|
| No meniscus injury | 7 (31.8 %) | 152 (43.1 %) | 0.210 |
| Lateral meniscus injury alone | 12 (54.5 %) | 75 (21.2 %) | 0.001 |
| Medial meniscus injury alone | 1 (4.5 %) | 52 (14.7 %) | 0.153 |
| Bilateral meniscus injuries | 2 (9.1 %) | 74 (21.0 %) | 0.140 |
Data are presented as number of patients (percentage).
Group S: Knees with the Segond fracture; Group N: Knees without the Segond fracture ACL: anterior cruciate ligament.
3.6. Location, morphology, and intervention for meniscus injuries
As for the location of meniscus injuries, there was no statistically significant difference between group S and group N (Table 4). In addition, there was no statistically significant difference between the two groups in the morphology of meniscus injury.
Table 4.
Meniscus injuries and intervention.
| Variables | Lateral Meniscus |
Medial Meniscus |
||||
|---|---|---|---|---|---|---|
| Group S | Group N | P Value | Group S | Group N | P Value | |
| Location of meniscal injury | P = 1.000 | P = 0.416 | ||||
| Anterior | 0/14 (0.0 %) | 5/149 (3.4 %) | 0/3 (0.0 %) | 1/126 (0.8 %) | ||
| Middle | 2/14 (14.3 %) | 27/149 (18.1 %) | 1/3 (33.3 %) | 19/126 (15.1 %) | ||
| Posterior | 12/14 (85.7 %) | 117/149 (78.5 %) | 2/3 (66.7 %) | 106/126 (84.1 %) | ||
| Morphology of meniscal injury | P = 0.366 | P = 1.000 | ||||
| Longitudinal | 11/14 (78.6 %) | 74/149 (49.7 %) | 3/3 (100 %) | 103/126 (81.7 %) | ||
| Horizontal | 0/14 (0.0 %) | 5/149 (3.4 %) | 0/3 (0.0 %) | 8/126 (6.3 %) | ||
| Complex | 1/14 (7.1 %) | 11/149 (7.4 %) | 0/3 (0.0 %) | 9/126 (7.1 %) | ||
| Root | 0/14 (0.0 %) | 7/149 (4.7 %) | 0/3 (0.0 %) | 1/126 (0.8 %) | ||
| Flap | 2/14 (14.3 %) | 24/149 (16.1 %) | 0/3 (0.0 %) | 2/126 (1.6 %) | ||
| Radial | 0/14 (0.0 %) | 28/149 (18.8 %) | 0/3 (0.0 %) | 1/126 (0.8 %) | ||
| Ramp | N.A. | N.A. | 0/3 (0.0 %) | 2/126 (1.6 %) | ||
| Treatment options for meniscal injury | P = 0.842 | P = 0.747 | ||||
| Suture | 7/12 (58.3 %) | 70/129 (54.3 %) | 3/3 (100 %) | 64/118 (54.2 %) | ||
| Rasping | 4/12 (33.3 %) | 37/129 (28.7 %) | 0/3 (0.0 %) | 21/118 (17.8 %) | ||
| Meniscectomy | 1/12 (8.3 %) | 22/129 (17.1 %) | 0/3 (0.0 %) | 33/118 (28.0 %) | ||
Data are presented as number of patients (percentage).
Group S: Knees with Segond fracture; Group N: Knees without Segond fracture.
N.A.: Not applicable.
With respect to treatment options, there was no statistically significant difference between the two groups.
4. Discussion
In the present study, we found out that ACL deficient knees with an LM injury but an intact MM injury were suggestive of the existence of a Segond fracture through a comprehensive multivariate analysis that identified LM injury, intact MM, and higher BMI as factors indicative of Segond fracture occurrence. Although radiographic diagnosis of the Segond fracture is not particularly challenging, its significance becomes evident in chronic situations when radiographic examination is scheduled three months or more after ACL injury. This is due to the fracture's remarkable self-healing potential, with Kumahara et al. reporting an average healing rate of within 90 days.13 The Segond fracture was considered as an indicator for ALL reconstruction for surgeons, including the ALL expert group.8, 9, 10, 11, 12,23 The findings of the present research offer valuable information, even in cases when the lesion has healed.
4.1. Meniscal injuries and the Segond fracture
To our knowledge, no studies have been reported using meniscal injuries as factors indicative of the occurrence of a Segond fracture, but several studies have reported the incidence of meniscal injuries in knees with a Segond fracture. Sulaiman et al. described a higher incidence of LM injuries.14 The biomechanical function of the LM might account for this. In a cadaveric knee study, Musahl et al. reported that the LM appeared to be a more important restraint to anterior tibial translation during combined valgus and rotatory loads applied during a pivoting manoeuvre.24 The frequent existence of a connection band between the ALL and LM might be another reason accounting for the higher incidence of LM injuries.25 On the other hand, Kumahara et al. reported that the incidence of LM injuries did not differ regardless of the existence of a Segond fracture even in which the patients had the same ethnic background as ours.13 Kim et al. reported a higher incidence of specific types of tears, e.g., LM root tears, accompanied by a Segond fracture, and that lateral tibial slope affected the occurrence of LM injuries,15 indicating that inherent bone morphology affected LM injuries. This might partially account for the inconsistent results among previous studies.
As for the incidence of MM injuries, contrary to the present study, Kumahara et al. and Sulaiman et al. reported no difference regardless of the presence of a Segond fracture.13,14 Again, other factors that affect the incidence of MM injuries might be present; however, we could not identify probable factors. Much larger cohort studies would elucidate the incidence more accurately.
4.2. Factors related to the Segond fracture other than meniscal injuries
We identified higher BMI as another factor. In previous studies, factors other than meniscal injuries related to the incidence of the Segond fracture have been reported, but no definite and consistent factors have been identified. Sulaiman et al. reported that sex, age, BMI, time from injury, and mechanism of injury were not associated with the incidence of the Segond fracture.14 On the other hand, Kumahara et al. reported that a higher BMI was observed in the Segond group, but sex, age, mechanism of injury, and knee recurvatum did not affect the incidence.13 Slagstad et al. reported older age and downhill skiing was observed more often in the Segond fracture group compared to a non-Segond fracture group.26
These inconsistent results are likely due to the variety of background characteristics in each patient cohort at each institute. The relatively lower incidence of the Segond fracture among ACL-injured knees might further hinder the inception of comprehensive studies to elucidate the cause of these inconsistencies.
4.3. Adaption for ALL injury
The present study only dealt with the Segond fracture, one of the types of ALL injury. It might be more valuable if we could adapt the derived results for the diagnosis of ALL injury because imaging diagnosis of ALL injury is still controversial. MRI is considered a standard modality for diagnosing abnormalities of the ALL, but Young et al. reported that physicians should not rely on MRI to diagnose an ALL injury in the presence of an ACL injury.27,28 Thus, seeking possible secondary imaging findings would be worth further consideration.
A high frequency of LM injuries in ALL-injured knees, reported by Van Dyck et al., supports the idea that a higher rate of LM injury is not restricted to Segond fractures but can also be generally observed in ALL injury.29
However, it would be unfounded to conclude that LM injury without MM injury could be a factor indicative of ALL injury at present. A new study using a reliable modality to assess the state of the ALL is necessary.
4.4. Clinical relevance
The ALL expert group has reported the Segond fracture as a decisive factor for considering combined ACLR and ALL reconstruction.23 However, regarding ACLR alone, the Segond fracture does not appear to carry substantial clinical importance. Nagai et al. reported in a systematic review that unrepaired Segond fracture during ACLR did not negatively impact the clinical outcomes.30 Interestingly, studies that compared the presence of Segond fracture with its absence inevitably had participants with ALL injured-knees in the non-Segond group. Thus, the question of whether intervention in ALL injuries, including Segond fractures, is necessary remains unanswered.
The current debate in the field of ACLR revolves around whether to add ALL reconstruction or antero-lateral augmentation (ALA) when performing ACLR irrespective of ALL injury. Lai S. et al. reported in a systematic review that ACLR with ALA had better stability and lesser likelihood of failure than those without ALA; however, the IKDC scores, Tegner scores, KOOS subscores, and return to sports did not differ between the two groups.31 Ibrahim SA et al. reported in a randomized clinical trial that ACLR with ALL reconstruction resulted in similar physical examination findings and clinical scores as isolated ACLR, except in the case of instrumented knee laxity measured with KT-1000; the authors advocated that ALL reconstruction should not be performed routinely.10 Some surgeons have emphasized the need for patient selection in combined ACLR and ALL reconstruction. Barahona M et al. reported the effectiveness of a formal consensus method among experts to create appropriate indications of ALA. The method selected variables as follows: age less than 25 years, high grade physical examination findings, radiological risk factors (including Segond fracture), pivoting sport, acute injury, recurvatum, and meniscal status.32
In theory, to advance this discussion, the status of ALL or anterolateral complex (ALC) should be considered. Herbst E et al. reported the clinical results of isolated ACLR with or without MRI-detected ALC injury and found no difference between the two groups in terms of clinical scores and physical examination data.33 While accumulating such studies is crucial to determine a standardised treatment for ALL injury, establishing a secure method to evaluate ALL status is a prerequisite for planning future research. MRI has been considered as the gold standard modality for ALL evaluation, but poor interobserver reliability and difficulty in diagnosing chronic situations have been reported.28,34 Thus, in the present study, we focused on the Segond fracture, which can confidently be diagnosed using radiography or MRI. Although we acknowledge the need for future studies, we believe that LM injury with MM intact might be adaptable to indicate ALL injury, as demonstrated by our findings. Given that avulsion fractures of the ACL or PCL are thought to be caused by the same underlying mechanism as significant ACL or PCL injury, this concept warrants further discussion.
4.5. Limitations
The present study had several limitations. First, we did not cover all the possible factors such as bone marrow oedema, tibial slope, and location of cartilage lesion. Second, there may have been recall bias owing to the length of the study and its retrospective nature. Despite the multivariate logistic regression analysis, the results could have been influenced by other uncontrolled factors. Third, the number of Segond fractures was small. We did not perform a power analysis prior to the study but the post hoc power calculated after the study exceeded 90 %; hence, the number of cases for the analysis was sufficient. Fourth, ethnicity of the subjects was limited to Japanese people. Fifth, radiographic examinations might not have been performed early enough. We selected subjects that received reconstructive surgery within 90 days from the injury. As a result, radiography and MRI were performed at an average of 5.6 days (0–45 days) and 12.2 days (0–65 days) from the injury. Sulaiman et al. reported that radiographic examination within a month was ideal.14 In the present study, 98 % of radiographic examinations and 88 % of MRIs were performed within a month; thus, chances of overlooked cases were low enough to not affect the results.
In conclusion, a LM injury without a MM injury indicated the existence of the Segond fracture. Higher BMI also increased the risk for the occurrence of the Segond fracture.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributions
Nobutada Suzuki contributed to the design, acquisition of the data, analysis and interpretation, drafting and revising of the manuscript. Atsuya Watanabe, Taishi Ninomiya, Hirofumi Nakajima, Manato Horii, Shotaro Watanabe and Takahisa Sasho performed data acquisition. Yuki Shiko performed the analysis and interpretation of the data. Nobutada Suzuki, and Takahisa Sasho contributed to the critical revision and final approval of the manuscript. All authors read and approved the final manuscript.
Ethics approval
This study was approved by the Institutional Review Board of Eastern Chiba Medical Center (September 2, 2022 ID 187).
Consent to participate
Informed consent was obtained from all patients and parents.
Consent for publication
Not Applicable.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
The authors appreciate all the assistance and cooperation from the Chiba University.
References
- 1.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vincent J.P., Magnussen R.A., Gezmez F., et al. The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20:147–152. doi: 10.1007/s00167-011-1580-3. [DOI] [PubMed] [Google Scholar]
- 3.Rasmussen M.T., Nitri M., Williams B.T., et al. An in vitro robotic assessment of the anterolateral ligament, part 1: secondary role of the anterolateral ligament in the setting of an anterior cruciate ligament injury. Am J Sports Med. 2016;44:585–592. doi: 10.1177/0363546515618387. [DOI] [PubMed] [Google Scholar]
- 4.Ruiz N., Filippi G.J., Gagnière B., Bowen M., Robert H.E. The comparative role of the anterior cruciate ligament and anterolateral structures in controlling passive internal rotation of the knee: a biomechanical study. Arthroscopy. 2016;32:1053–1062. doi: 10.1016/j.arthro.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 5.Sonnery-Cottet B., Lutz C., Daggett M., et al. The involvement of the anterolateral ligament in rotational control of the knee. Am J Sports Med. 2016;44:1209–1214. doi: 10.1177/0363546515625282. [DOI] [PubMed] [Google Scholar]
- 6.Tavlo M., Eljaja S., Jensen J.T., Siersma V.D., Krogsgaard M.R. The role of the anterolateral ligament in ACL insufficient and reconstructed knees on rotatory stability: a biomechanical study on human cadavers. Scand J Med Sci Sports. 2016;26:960–966. doi: 10.1111/sms.12524. [DOI] [PubMed] [Google Scholar]
- 7.Smith J.O., Yasen S.K., Lord B., Wilson A.J. Combined anterolateral ligament and anatomic anterior cruciate ligament reconstruction of the knee. Knee Surg Sports Traumatol Arthrosc. 2015;23:3151–3156. doi: 10.1007/s00167-015-3783-5. [DOI] [PubMed] [Google Scholar]
- 8.Hardy A., Casabianca L., Hardy E., Grimaud O., Meyer A. Combined reconstruction of the anterior cruciate ligament associated with anterolateral tenodesis effectively controls the acceleration of the tibia during the pivot shift. Knee Surg Sports Traumatol Arthrosc. 2017;25:1117–1124. doi: 10.1007/s00167-017-4515-9. [DOI] [PubMed] [Google Scholar]
- 9.Hopper G.P., Aithie J.M.S., Jenkins J.M., Wilson W.T., Mackay G.M. Combined anterior cruciate ligament repair and anterolateral ligament internal brace augmentation: minimum 2-year patient-reported outcome measures. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120968557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ibrahim S.A., Shohdy E.M., Marwan Y., et al. Anatomic reconstruction of the anterior cruciate ligament of the knee with or without reconstruction of the anterolateral ligament: a randomized clinical trial. Am J Sports Med. 2017;45:1558–1566. doi: 10.1177/0363546517691517. [DOI] [PubMed] [Google Scholar]
- 11.Sonnery-Cottet B., Thaunat M., Freychet B., Pupim B.H.B., Murphy C.G., Claes S. Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med. 2015;43:1598–1605. doi: 10.1177/0363546515571571. [DOI] [PubMed] [Google Scholar]
- 12.Trinchese G.F., Oliva F., Maffulli N. Minimally invasive anatomic reconstruction of the anterolateral ligament with ipsilateral gracilis tendon. Muscles Ligaments Tendons J. 2017;7:240–246. doi: 10.11138/mltj/2017.7.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumahara R., Kimura Y., Sasaki S., et al. Prevalence of Segond fractures associated with anterior cruciate ligament injuries and their influence on knee joint stability; A case-control study. BMC Muscoskel Disord. 2022;23:180. doi: 10.1186/s12891-022-05127-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sulaiman Y., Li J., Chen G., Abudouaini H., Li Q., Tang X. The relationship between a Segond fracture and meniscus injury in patients with anterior cruciate ligament tears. Knee. 2021;33:193–199. doi: 10.1016/j.knee.2021.09.008. [DOI] [PubMed] [Google Scholar]
- 15.Kim S.H., Seo J.-H., Kim D.-A., Lee J.-W., Kim K.I., Lee S.H. Steep posterior lateral tibial slope, bone contusion on lateral compartments and combined medial collateral ligament injury are associated with the increased risk of lateral meniscal tear. Knee Surg Sports Traumatol Arthrosc. 2022;30:298–308. doi: 10.1007/s00167-021-06504-z. [DOI] [PubMed] [Google Scholar]
- 16.Muneta T., Sekiya I., Yagishita K., Ogiuchi T., Yamamoto H., Shinomiya K. Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy. 1999;15:618–624. doi: 10.1053/ar.1999.v15.0150611. [DOI] [PubMed] [Google Scholar]
- 17.Yasuda K., Kondo E., Ichiyama H., Tanabe Y., Tohyama H. Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy. 2006;22:240–251. doi: 10.1016/j.arthro.2005.12.017. [DOI] [PubMed] [Google Scholar]
- 18.Brittberg M., Winalski C.S. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003 doi: 10.2106/00004623-200300002-00008. 85-A;Suppl 2:58–69. [DOI] [PubMed] [Google Scholar]
- 19.Kamimura T., Kimura M. Repair of horizontal meniscal cleavage tears with exogenous fibrin clots. Knee Surg Sports Traumatol Arthrosc. 2011;19:1154–1157. doi: 10.1007/s00167-011-1404-5. [DOI] [PubMed] [Google Scholar]
- 20.Kim J.H., Ryu D.-J., Park J.S., Shin T.S., Wang J.H. Arthroscopic transtibial pull-out repair of medial meniscus posterior root tear with a whip running suture technique. Arthrosc Tech. 2021;10:e1017–e1024. doi: 10.1016/j.eats.2020.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsujii A., Amano H., Tanaka Y., et al. Second look arthroscopic evaluation of repaired radial/oblique tears of the midbody of the lateral meniscus in stable knees. J Orthop Sci. 2018;23:122–126. doi: 10.1016/j.jos.2017.09.023. [DOI] [PubMed] [Google Scholar]
- 22.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 23.Sonnery-Cottet B., Daggett M., Fayard J.M., et al. Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament - deficient knee. J Orthop Traumatol. 2017;18:91–106. doi: 10.1007/s10195-017-0449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Musahl V., Citak M., O'Loughlin P.F., Choi D., Bedi A., Pearle A.D. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38:1591–1597. doi: 10.1177/0363546510364402. [DOI] [PubMed] [Google Scholar]
- 25.Watanabe J., Suzuki D., Mizoguchi S., Yoshida S., Fujimiya M. The anterolateral ligament in a Japanese population: study on prevalence and morphology. J Orthop Sci. 2016;21:647–651. doi: 10.1016/j.jos.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 26.Slagstad I., Parkar A.P., Strand T., Inderhaug E. Incidence and prognostic significance of the Segond fracture in patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2020;48:1063–1068. doi: 10.1177/0363546520905557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Andrade R., Rebelo-Marques A., Bastos R., et al. Identification of normal and injured anterolateral ligaments of the knee: a systematic review of magnetic resonance imaging studies. Arthroscopy. 2019;35:1594–1613. doi: 10.1016/j.arthro.2018.10.120. [DOI] [PubMed] [Google Scholar]
- 28.Young B.L., Ruder J.A., Trofa D.P., Fleischli J.E. Visualization of concurrent anterolateral and anterior cruciate ligament injury on magnetic resonance imaging. Arthroscopy. 2020;36:1086–1091. doi: 10.1016/j.arthro.2019.09.039. [DOI] [PubMed] [Google Scholar]
- 29.Van Dyck P., Clockaerts S., Vanhoenacker F.M., et al. Anterolateral ligament abnormalities in patients with acute anterior cruciate ligament rupture are associated with lateral meniscal and osseous injuries. Eur Radiol. 2016;26:3383–3391. doi: 10.1007/s00330-015-4171-8. [DOI] [PubMed] [Google Scholar]
- 30.Nagai K., Kamada K., Kay J., et al. Clinical outcomes after anterior cruciate ligament reconstruction in patients with a concomitant Segond fracture: a systematic review. Am J Sports Med. 2023;51:525–533. doi: 10.1177/03635465211045689. [DOI] [PubMed] [Google Scholar]
- 31.Lai S., Zhang Z., Li J., Fu W.L. Comparison of anterior cruciate ligament reconstruction with versus without anterolateral augmentation: a systematic review and meta-analysis of randomized controlled trials. Orthop J Sports Med. 2023;11 doi: 10.1177/23259671221149403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barahona M., Mosquera M., Padua V., et al. Latin American formal consensus on the appropriate indications of extra-articular lateral procedures in primary anterior cruciate ligament reconstruction. J ISAKOS. 2023;8:177–183. doi: 10.1016/j.jisako.2022.08.007. [DOI] [PubMed] [Google Scholar]
- 33.Herbst E., Costello J., Popchak A.J., et al. Untreated injuries to the anterolateral capsular structures do not affect outcomes and kinematics after anatomic anterior cruciate ligament reconstruction. J Clin Med. 2023;12:4408. doi: 10.3390/jcm12134408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ahn J.H., Koh I.J., McGarry M.H., et al. Elongation patterns of the anterior and posterior borders of the anterolateral ligament of the knee. Arthroscopy. 2019;35:2152–2159. doi: 10.1016/j.arthro.2019.02.042. [DOI] [PubMed] [Google Scholar]