Abstract
Objective:
We aimed to determine the incidence of major cardiovascular and cerebrovascular events in elderly patients with primary hyperparathyroidism (pHPT) and the impact of parathyroidectomy.
Summary Background Data:
pHPT is under-diagnosed and under-treated in the United States. It is associated with increased cardiovascular disease risk but its association with cerebrovascular disease risk is not well-established. It is also unknown if parathyroidectomy reduces these risks.
Methods:
The incidence of major cerebrovascular and cardiovascular events in 108,869 patients with pHPT diagnosed in the Medicare database between 2008 and 2018 and a matched comparison group of 1,088,690 Medicare subjects was prospectively evaluated. We estimated hazards ratios (HR) for the association of pHPT and parathyroidectomy for the risk of these outcomes from Cox proportional hazards models. Survival curves were calculated to obtain five-year disease-free survival (DFS) estimates.
Results:
For patients with pHPT, five-year DFS was lower and HRs were higher than the comparison group for any outcome (75.9% vs 78.4; HR 1.11, 95% confidence interval [CI] 1.09–1.13), major cerebrovascular events (84.5% vs 86.3%; HR 1.14, 95% CI 1.12–1.17), and major cardiovascular events (87.7% vs 88.8%; HR 1.06, 95% CI 1.03–1.08). However, in patients who had parathyroidectomy, the risks of major cerebrovascular and cardiovascular events did not differ from the comparison cohort. The lower risk in patients who had parathyroidectomy were maintained in subgroup analyses.
Conclusions:
Older patients with pHPT have an increased risk of major cerebrovascular and cardiovascular events compared to patients without the disease. Physicians treating older patients with primary hyperparathyroidism should consider parathyroidectomy.
Mini-Abstract
US Medicare program data showed an increased risk of major cardiovascular and cerebrovascular events in patients with primary hyperparathyroidism compared to a matched comparison group. There was no difference between patients who underwent parathyroidectomy and those who never had primary hyperparathyroidism indicating the procedure is associated with decreased cerebro-cardiovascular risk.
Introduction
Primary hyperparathyroidism is an increasingly common endocrinopathy with an incidence between 13 and 120 per 100,000 person-years and a higher prevalence among older patients and women (approximately three times that of men).1 It is defined by an excess of parathyroid hormone, which leads to hypercalcemia, causing osteoporosis or pathologic fractures and nephrolithiasis, as well as abdominal pain, lethargy, and depression. Primary hyperparathyroidism is caused by hypersecretion of parathyroid hormone in the setting of either sporadic disease or in association with one of several hereditary endocrine syndromes, most notably multiple endocrine neoplasia type 1 and type 2A. Treatment is targeted parathyroidectomy for a solitary adenoma. For multi-gland hyperplasia, patients will either undergo sub-total parathyroidectomy or total parathyroidectomy with autotransplantation. For patients with bone loss, parathyroidectomy has been shown to reverse this sequela, and those with nephrolithiasis experience improvement postoperatively.2
In addition to the classic features of primary hyperparathyroidism, prior work has shown an association with cardiovascular disease.3–10 However, the data assessing parathyroidectomy and its impact on cardiovascular disease in this population is less convincing. Some studies have indicated a benefit in several key outcome measures, including risk reduction for myocardial infarction, left ventricular hypertrophy, and hypertension, but the results are mixed.7,9–11 Additionally, the association between primary hyperparathyroidism and cerebrovascular disease risk is not well established, nor is the potential risk reduction of this sequelae after surgery. In 2020 in the United States, heart disease was the number one cause of death and stroke was fifth,12 indicating that the reduction of this disease burden on the US population, especially among the elderly, is of critical importance.
Analyses have indicated that the incidence of primary hyperparathyroidism is rising and that the disease is underdiagnosed and undertreated in the United States.13–16 Given this data and a potential association with increased cardiovascular and cerebrovascular risk, a greater understanding of the potential benefit from parathyroidectomy in relation to these outcomes is imperative. To evaluate the risks of major cardiovascular and major cerebrovascular events in patients who had parathyroidectomy for primary hyperparathyroidism, we analyzed prospective follow-up data from a large cohort of patients from the United States enrolled in the Medicare program. We compared the estimated risks of cardiovascular and cerebrovascular diseases in patients diagnosed with primary hyperparathyroidism with or without parathyroidectomy to a comparison group matched on age, sex, and multiple comorbidities. We carefully controlled for medical surveillance and other potential confounders. To aid clinical decision making we estimated five-year disease-free survival for major cardiovascular and major cerebrovascular events from cumulative incidence curves.
Methods
Study population
We studied individuals with primary hyperparathyroidism (“cases”) and a matched comparison group without primary hyperparathyroidism who were enrolled in the Medicare claims database between January 1, 2008, and December 31, 2018. Medicare was established in 1965 as a federal health insurance program for disabled adults and elderly persons living in the United States. We focused on patients diagnosed 2008 or later as Medicare Part D supplemental plans that cover prescription drugs became available on January 1, 2006. To be eligible for the present study, the subjects had to have at least 13 months of Medicare plans Part A/B (covering hospital and medical insurance) and supplementary plan Part D insurance.
Selection of primary hyperparathyroidism cases and matched comparison subjects
We identified primary hyperparathyroidism cases using the International Classification of Diseases 9th Revision and 10th Revision Clinical Modification (ICD-10-CM) codes E21.0 and (ICD-9-CM) 252.01. Each patient was required to have at least one hospital claim or two outpatient claims separated by a minimum of 30 days. Cases were restricted to those with a first primary hyperparathyroidism claim between January 1, 2008, and December 31, 2018, and ages 66 through 84. We randomly selected ten comparison subjects per case, frequency-matched based on sex, Black race, calendar year of case selection, and age group at diagnosis/selection (66–69, 70–74, 75–79, 80–84 years), comorbid hypertension, diabetes, ever smoking (yes/no), and lipid disorder (prior to diagnosis or selection age). Individuals in the comparison group were assigned June 30th as the selection date for their selection year. Individuals with claims for end stage renal disease (ICD-9-CM 585.6, ICD-10-CM N18.6) were excluded. We used the Medicare claims data and the Current Procedural Termininology (CPT) code 60500 to identify patients who were diagnosed with pHPT and had parathyroidectomy. Additionally, we excluded individuals if a claim for parathyroidectomy, using CPT code 60500, or cinacalcet administration in Medicare Part D was present greater than one year prior to their first claim for primary hyperparathyroidism. The Supplemental Figure outlines the case selection process.
Outcome measures
We examined the risk of the following outcomes: myocardial infarction (ICD-10-CM: acute I21.0–21.4, I21.9, I21.A; subsequent I22.0–22.2, I22.8–22.9; other I24.0, I24.8–24.9) (ICD-9-CM: acute myocardial infarction 410.0–410.9), chronic ischemic heart disease (ICD-10-CM: I25.1–25.2, I25.5–25.9) (ICD-9-CM: 414.0–414.4, 414.8, 414.9), cerebral infarction (ICD-10-CM: I63.0–63.6, I63.8–63.9), brain stem stroke syndrome (ICD-10-CM: G46.3), cerebellar stroke syndrome (ICD-10-CM: G46.4), occlusion and stenosis of precerebral arteries (ICD-9-CM: 433), occlusion of cerebral arteries (ICD-9-CM: 434), transient cerebral ischemia (ICD-9-CM: 435), angina pectoris (ICD-10-CM: I20.0–20.1, I20.8–20.9) (ICD-9-CM: 413.0, 413.1, 413.9), and cardiac catheterization (CPT codes 93451–93461). Outcomes were investigated individually or grouped into “any outcome”, “major cerebrovascular event” or “major cardiovascular event”.
Covariate definitions and statistical analysis
Race and ethnicities were derived using Medicare claims codes. Conditions and comorbidities were identified using Medicare Part B claims and ICD-9-CM and ICD-10-CM codes and included dyslipidemia (ICD-10-CM: E78) (ICD-9-CM: 272), diabetes (ICD-10-CM: E08, E09, E10, E11, E13) (ICD-9-CM: 250), and hypertension (ICD-10-CM: I10, I11.0, I11.9, I13.0–13.2) (ICD-9-CM: 401–405) from the year 1999 up to the selection date. Comorbidities were ascertained throughout a person’s Medicare enrollment (starting in 1999). To lessen the possibility of making the diagnosis of pHPT incidentally during medical care for other reasons, we accounted for medical surveillance intensity by calculating the average number of physician visits for each six-month interval between 2006 and the selection date, omitting the first and last intervals. We excluded claims from specialists with limited patient contact (radiologists, anesthesiologists, pathologists).
We used a prospective cohort analysis to compare the incidence of cerebrovascular and cardiovascular events in patients with primary hyperparathyroidism and the matched comparison group. Follow-up began at age of diagnosis or age at selection. Follow-up ended at the earliest age of major event, discontinuation of Part B coverage, transfer to an HMO, death, diagnosis of primary hyperparathyroidism (comparison group), attaining age 85 or December 31, 2018. We estimated the hazard ratio (HR) and 95% confidence interval (CI) for the associations of primary hyperparathyroidism case status, parathyroidectomy, and cinacalcet use with the risk of major cerebrovascular and cardiovascular events from Cox proportional hazards models with age as the time scale. We accounted for delayed age at entry using the entrytime statement, proc phreg, SAS Enterprise Guide (version 7.15, SAS Institute Inc., Cary, NC, USA). The models were adjusted for diagnosis/selection year (2008–2011, 2012–2015, 2016–2018), sex, race (White, Black, Hispanic, other/unknown), duration of Medicare Part D coverage (quintiles: 13–71, 72–102, 103–133, 134–153, 154–156 months), the average number of physician visits per six month period (quintiles: ≤ 1.5, ≤ 2.7, ≤ 4.2, ≤ 6.5, > 6.5), Medicaid eligibility (yes/no), limited income subsidy (yes/no), and conditions/comorbidities (dyslipidemia, diabetes, hypertension). Survival curves and five-year disease-free survival estimates were calculated using the lifetable estimates in proc lifetest and groups were compared using the log-rank test.
Results
Of 88,462,175 eligible patients in the Medicare database, 334,377 had a claim code for primary hyperparathyroidism, and 108,869 met inclusion criteria (see Supplemental Figure 1 for exclusion details). From eligible patients, included cases were matched with 1,088,690 comparison subjects without the disease. Cases were predominantly female (78.6%) and white (80.8%). By study design, all subjects were 66 to 84 years old. A higher proportion of patients with primary hyperparathyroidism had kidney diseases compared to comparison subjects (27.4% vs 15.6%). To treat their primary hyperparathyroidism, 37.2% of cases underwent parathyroidectomy, and 8.6% took cinacalcet; no comparison subject had a claim code for either (Table 1).
Table 1.
Clinical characteristics of patients in the study cohort
| Cases with Primary Hyperparathyroidism n=108,869 | Matched Controls n=1,088,690 | |
|---|---|---|
|
| ||
| Sex | ||
| Male | 23283 (21.4%) | 232830 (21.4%) |
| Female | 85586 (78.6%) | 855860 (78.6%) |
|
| ||
| Race | ||
| White | 87948 (80.8%) | 832279 (76.5%) |
| Black | 12286 (11.3%) | 122325 (11.2%) |
| Hispanic | 5167 (4.8%) | 80145 (7.4%) |
| Other/Unknown | 3468 (3.2%) | 53941 (5.0%) |
|
| ||
|
| ||
| Hypertension | 98994 (90.9%) | 989940 (90.9%) |
|
| ||
| Diabetes | 50426 (46.3%) | 504260 (46.3%) |
|
| ||
| Hyperlipidemia | 99227 (91.1%) | 992270 (91.1%) |
|
| ||
| Tobacco Use | 22972 (21.1%) | 229720 (21.1%) |
|
| ||
| Alcohol Use Disorder* | 1460 (1.3%) | 16663 (1.5%) |
|
| ||
| Family History of Stroke* | 1071 (1.0%) | 8312 (0.8%) |
|
| ||
| Family History of Heart Disease * | 5629 (5.2%) | 48131 (4.4%) |
|
| ||
| Hormone Replacement Therapy * | 2141 (2.0%) | 19290 (1.8%) |
|
| ||
| Kidney Disease * | 29842 (27.4%) | 169736 (15.6%) |
|
| ||
| Parathyroidectomy ** | 40481 (37.2%) | NA |
|
| ||
| Cinacalcet Use ** | 9362 (8.6%) | NA |
Controls were not matched on these variables
Patients with claims codes for these treatments were excluded from the control group
NA: not applicable
Incidence of major cerebrovascular or major cardiovascular events in patients with primary hyperparathyroidism
Prior to selection, cases had an increased incidence of cerebral infarction, pre-cerebral occlusion, cerebral occlusion, cerebral ischemia, angina pectoris, cardiac catheterization, and cardiac ischemia (Table 2). After selection, there was an increased incidence of these sequelae as well as brain stem stroke, cerebellar stroke, and myocardial infarction among cases compared to comparison subjects, indicating an association between primary hyperparathyroidism and increased risk of major cerebrovascular and major cardiovascular events. The presence of any of the diseases listed in Table 2 was treated as an independent risk factor in the Cox models.
Table 2.
Major cardiovascular and major cerebrovascular events in the study cohort before and after the diagnosis of primary hyperparathyroidism.
| Events Prior to Diagnosis/Selection | Outcomes After Diagnosis/Selection | |||
|---|---|---|---|---|
| Cases with Primary Hyperparathyroidism n=108,869 | Matched Controls n=1,088,690 | Cases with Primary Hyperparathyroidism n=108,869 | Matched Controls n=1,088,690 | |
| Cerebral Infarction * | 2209 (2.0%) | 16849 (1.6%) | 4751 (4.4%) | 43283 (4.0) |
| Brain Stem Stroke * | 14 (<0.1%) | 108 (<0.1%) | 21 (<0.1%) | 153 (<0.1%) |
| Cerebellar Stroke * | 36 (<0.1%) | 309 (<0.1%) | 49 (0.1%) | 432 (<0.1%) |
| Precerebral Occlusion * | 25786 (23.7%) | 246713 (22.7%) | 1946 (1.8%) | 16869 (1.6%) |
| Cerebral Occlusion * | 11091 (10.2%) | 107022 (9.8%) | 2005 (1.8%) | 19553 (1.8%) |
| Cerebral Ischemia * | 15796 (14.5%) | 149342 (13.7%) | 2644 (2.4%) | 22504 (2.1%) |
| Myocardial Infarction ** | 8751 (8.0%) | 88091 (8.1%) | 2034 (1.9%) | 19996 (1.8%) |
| Angina Pectoris ** | 19729 (18.1) | 192968 (17.8) | 2020 (1.9%) | 16592 (1.5%) |
| Cardiac Catheterization ** | 7498 (6.9%) | 69797 (6.4%) | 8954 (8.2%) | 73212 (6.7%) |
| Ischemic Heart Disease ** | 47515 (43.6%) | 450788 (41.4%) | 7964 (7.3%) | 70912 (6.5%) |
Included in the composite outcome measure Major Cerebrovascular Event
Included in the composite outcome measure Major Cardiovascular Event
For any outcome, five-year disease-free survival was lower in cases than in the comparison subjects (75.9% vs 78.4%, p<0.001) (Figure 1A). Similar differences were seen for major cerebrovascular events (84.5 vs 86.3%, p<0.001) and major cardiovascular events (87.7% vs 88.8%, p<0.001) (Figure 1B–1C).
Figure 1:
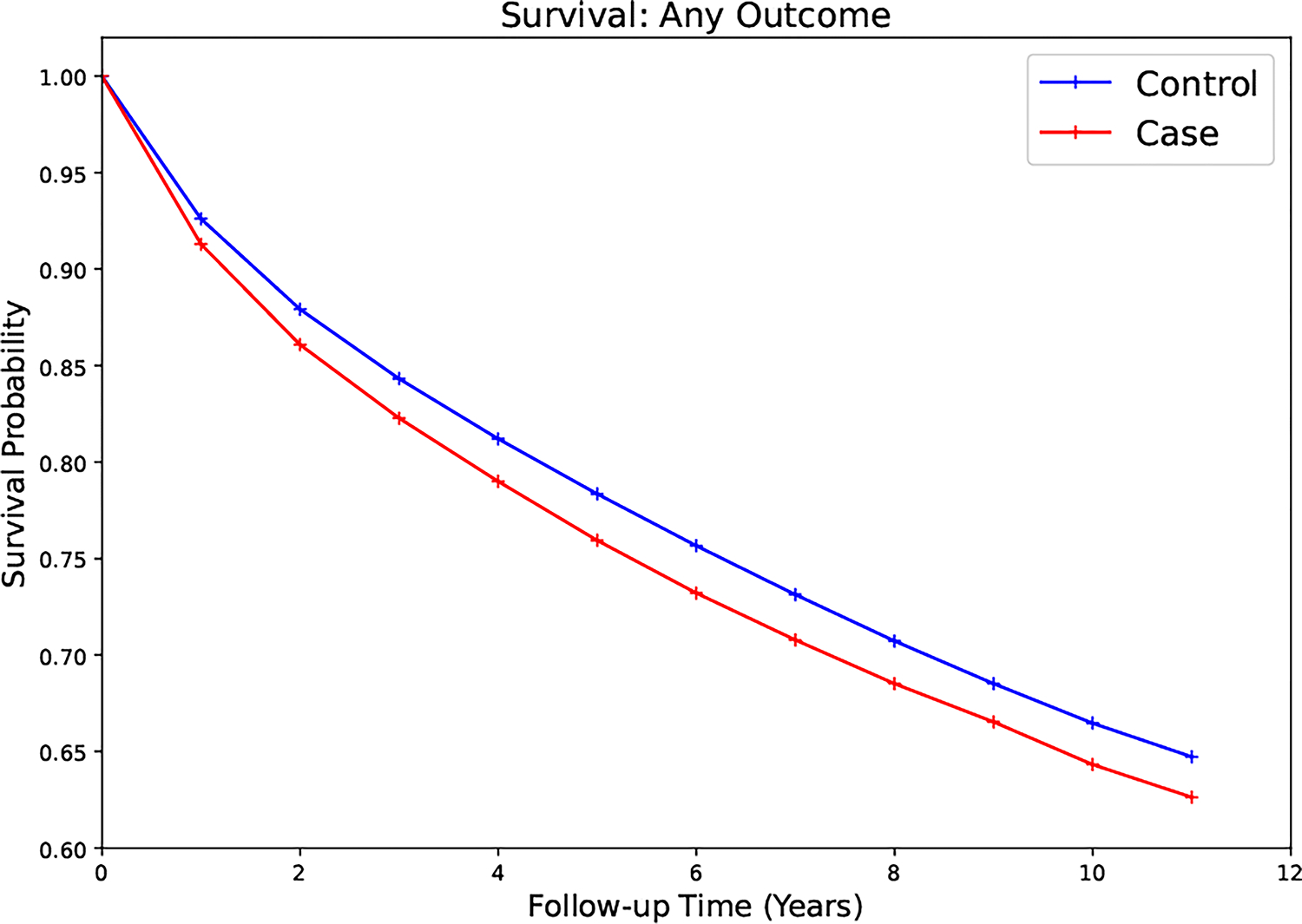
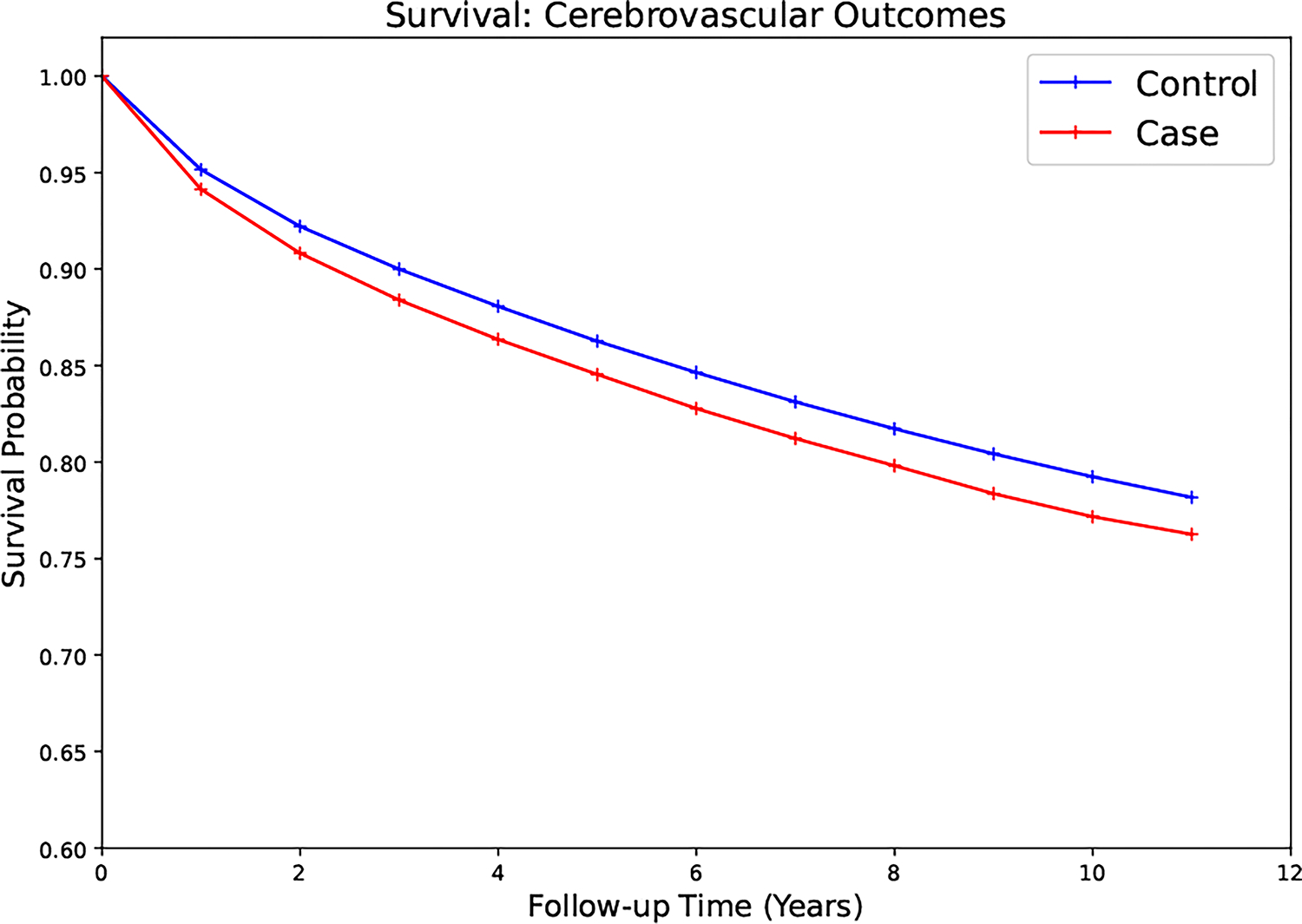
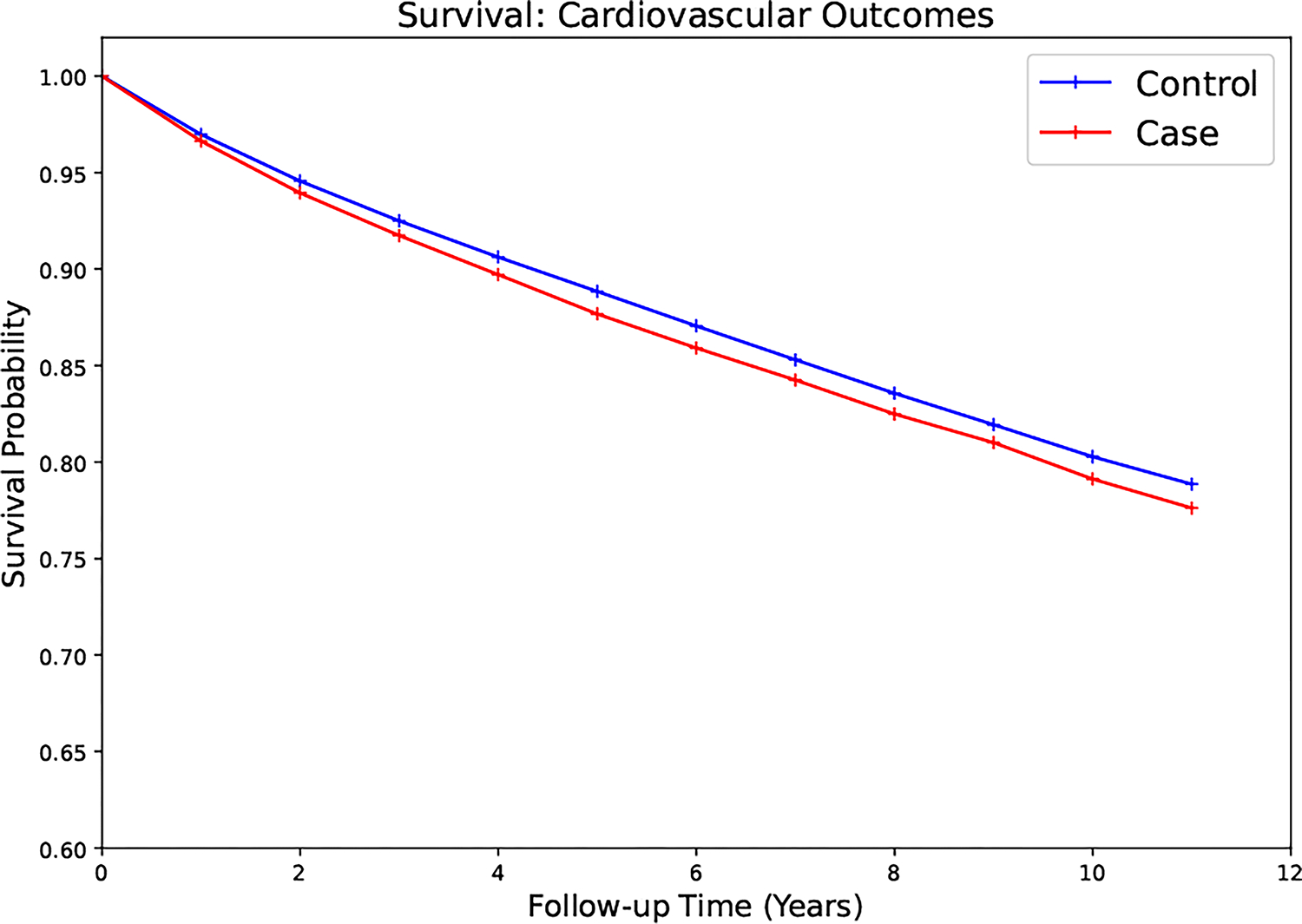
Survival curves for cases and controls (A) for all outcomes (B) major cerebrovascular events (C) major cardiovascular events.
Cases had a statistically significantly increased risk of developing any outcome (11%), major cerebrovascular (14%) or major cardiovascular event (6%) after selection than comparison subjects (Table 3). Men had a higher risk of experiencing any outcome, a major cerebrovascular event, or a major cardiovascular event than women (18% vs 9%, 22% vs 12%, 11% vs 4%, respectively) (Supplemental Table 1A–1B). Among cases treated surgically with parathyroidectomy, the risk of any outcome, major cerebrovascular, or major cardiovascular event was not statistically different from the risk of the comparison subjects, indicating that for patients with primary hyperparathyroidism, underdoing the procedure was associated with lowering the risk of these major outcomes to levels of individuals who never had the disease, a finding which was maintained on subgroup analysis (Table 3, Supplemental Tables 1A–1B and 2A–2C).
Table 3.
Association of selected clinical variables with primary outcomes hazard ratios estimated from multivariable adjusted model
| Association of Select Factors with Primary Outcomes Hazards ratios were estimated from multivariable adjusted model | |||
|---|---|---|---|
| Hazard Ratio (95% Confidence Interval) | |||
| Any Outcome | Major Cerebrovascular Event | Major Cardiovascular Event | |
| Primary Hyperparathyroidism | 1.11 (1.09–1.13) | 1.14 (1.12–1.17) | 1.06 (1.03–1.08) |
| Parathyroidectomy | 0.99 (0.97–1.02) | 0.98 (0.95–1.02) | 0.99 (0.95–1.02) |
| Cinacalcet | 1.31 (1.24–1.85) | 1.25 (1.17–1.33) | 1.37 (1.28–1.47) |
| Pre-Selection Event | 3.09 (3.06–3.12) * | 4.28 (4.24–4.33) ** | 3.23 (3.19–3.28) *** |
| Black Race | 0.97 (0.96–0.98) | 1.03 (1.02–1.05) | 0.90 (0.88–0.92) |
| Hypertension | 1.88 (1.84–1.93) | 1.83 (1.77–1.89) | 2.17 (2.09–2.25) |
| Diabetes | 1.25 (1.24–1.26) | 1.16 (1.15–1.18) | 1.41 (1.40–1.43) |
| Hyperlipidemia | 1.27 (1.24–1.30) | 1.30 (1.27–1.34) | 1.30 (1.26–1.34) |
Includes major cerebrovascular or major cardiovascular event which occurred prior to selection
Includes major cerebrovascular event which occurred prior to selection
Includes major cardiovascular event which occurred prior to selection
Among the total population, subjects who had an event prior to selection (e.g., myocardial infarction or stroke) were at the greatest risk for any future outcome or future major outcome individually (Table 3). Additionally, a diagnosis of hypertension, hyperlipidemia, or diabetes was each associated with a greater risk of any outcome (or major outcome individually) among all subjects compared to a diagnosis of primary hyperparathyroidism. Subjects who were prescribed cinacalcet and did not have surgery had a higher risk of developing any outcome than comparison subjects.
Effect of parathyroidectomy on subjects with pre-existing comorbidities
We fit separate Cox models for each outcome to evaluate the effect of surgery on patients with hypertension, hyperlipidemia, and diabetes (Supplemental Table 3A–3C). Among cases with diabetes or hyperlipidemia, the risk of any outcome, major cerebrovascular event, or major cardiovascular event was similar to the risk seen for the entire case group. The same was true for cases with hypertension with respect to all outcomes or major cardiovascular events. However, in a Cox model evaluating cases with hypertension who had parathyroidectomy, there was a suggestion of decreased risk of major cerebrovascular events compared to the comparison subjects (HR: 0.87, 95% CI: 0.75–1.01), indicating patients with primary hyperparathyroidism and comorbid hypertension may experience the most benefit.
Discussion
This is the largest nationally representative study to evaluate risk of major cerebrovascular and major cardiovascular events in elderly patients with primary hyperparathyroidism and the effect of parathyroidectomy on those outcomes. These data suggest that patients with primary hyperparathyroidism are at greater risk of major cerebrovascular events, which has not been previously shown. This study also confirms prior data that primary hyperparathyroidism is associated with increased cardiovascular risk, although this appears to be minimal. Men had a greater risk of both major cardiovascular and cerebrovascular events compared to women. Further, these data reveal that among patients with primary hyperparathyroidism, parathyroidectomy lowered the risk of these major outcomes back to the average risk of age, sex, and comorbidity-matched individuals within the Medicare beneficiary population without it. When analyzing the independent effect of surgery on cases by comorbidities, parathyroidectomy may be associated with the greatest benefit among patients with primary hyperparathyroidism and hypertension.
The primary metabolic abnormality caused by primary hyperparathyroidism is hypercalcemia, and the primary pathophysiology of atherosclerosis is the accumulation of lipid plaques laden with calcium.17 It follows, then, that the continuously elevated circulating calcium levels caused by primary hyperparathyroidism would worsen the existing atherosclerotic disease, the main driver behind cardiac ischemic events and stroke, and increase the risk of these life-threatening events.18,19 This study showed an increase in both types of end-organ vascular events in cases from the Medicare population. These data also identified an increased incidence of kidney disease (but not end-stage renal disease since patients with this diagnosis were excluded) among cases, indicating an association with primary hyperparathyroidism. Although chronic kidney disease is associated with cardiovascular disease, we did not match the comparison group on this variable because chronic kidney disease is one of the complications seen in patients with primary hyperparathyroidism. Nevertheless, it is a potential confounder in our analysis. A correlation between primary hyperparathyroidism and cerebrovascular disease has only been shown in case reports and a single cohort analysis.20,21 No analysis to date has shown improvement in cerebrovascular outcomes after parathyroidectomy. A recent prospective randomized controlled trial from Scandinavia showed no difference in the incidence of cardiac or cerebrovascular events between patients with mild primary hyperparathyroidism who had parathyroidectomy (n=15/95) and those who were observed (n=15/96).22 However, that trial was designed for a primary endpoint of all-cause mortality, the age of the participants was younger than in this analysis (mean 62.8 years for the parathyroidectomy group and 63.4 years for the observational group), and they included only patients with mild primary hyperparathyroidism, whereas this analysis included all degrees of severity. Additionally, earlier studies have shown that a large proportion of older patients experience primary hyperparathyroidism (1.5%) and they present with more biochemically advanced disease than their younger counterparts.23 Prior observational data revealed that patients who undergo parathyroidectomy returned to the same risk of myocardial infarction as an age and sex (but not comorbidity) matched population.10 Importantly, this group showed that risk of myocardial infarction was increased for the ten years prior to surgery among the case group. While the data presented here did not specifically show an increase in pre-diagnosis incidence of myocardial infarction, an increased incidence of angina, cardiac catheterization, and ischemic heart disease leading up to a diagnosis of primary hyperparathyroidism was shown – all of which can be thought of as surrogate markers for acute cardiac ischemia.
Patients who took cinacalcet had a higher risk of developing a major outcome than comparison subjects, possibly due to selection bias if providers more frequently gave cinacalcet to patients who were not surgical candidates because of prohibitive comorbidies that can increase cardiovascular risk. This selection bias may also confound the higher risk of major events in the non-operative group. However, confounding is minimized by the matching strategy and the large population evaluated here.
The Centers for Disease Control and Prevention reports that in 2020 heart disease was the number one cause of death of Americans and stroke was the fifth (down from fourth the prior year due to a new third leading cause of death, COVID-19), accounting for a combined 857,226 deaths that year.12 Recent data have indicated that primary hyperparathyroidism may be severely underdiagnosed among patients with osteoarthritis24 and, more broadly, the general population, as indicated by the results of a large local cohort analysis from the University of Arkansas, which showed that 72.3% of patients with hypercalcemia were never investigated for the disease.13 Additionally, less than one-third of patients diagnosed with primary hyperparathyroidism undergo surgery, and the rate of parathyroidectomy is declining, especially among older patients in the United States14,15, consistent with the rate of parathyroidectomy in this study. All the while, the incidence of primary hyperparathyroidism has been increasing since the 1970s with the advent of regular measurement of serum calcium levels in American medical practice.16 The current consensus guidelines state surgery may be considered to reduce the potential sequela of cardiovascular disease – a weak recommendation noted in the text of the guidelines to be based on low-quality evidence.25 Further, these guidelines recommend parathyroidectomy for all patients under 50 years of age with primary hyperparathyroidism, but there is no recommendation specifically for the older population.
Parathyroidectomy can be done safely with low rates of perioperative morbidity in the elderly – rates that are comparable to younger populations.23,26–28 This operation can even be done safely and effectively under local anesthesia with sedation if a patient’s comorbid conditions preclude general anesthesia.29 The complication most concerning to patients and surgeons is an injury to the recurrent laryngeal nerve resulting in vocal cord paralysis. Even transient injury to the nerve is rare, occurring in less than one percent of cases after parathyroidectomy. A recent observational study reported 13 injuries to the recurrent laryngeal nerve after 197 parathyroidectomies, three of which were permanent.30 When patients and physicians assess the risk of surgery for this disease, they must compare the risk of morbidity with the risk of developing a major life-threatening cardiac or cerebrovascular event. This analysis shows an increased risk for all outcomes, major cerebrovascular events, and major cardiovascular events of 9%, 12%, and 4%, respectively, which is more severe in men at 18%, 22%, and 11%.
This analysis has several limitations, some shared by all studies using electronic medical records that are not collected for research purposes, such as lack of information on potential confounders, information bias, and incomplete or inappropriate data entry. While we attempted to adjust for confounders and healthcare utilization, some residual effects may be present in our estimates. Specifically for our investigation, it is unknown if parathyroidectomy was successful. Although we did not specifically control for vascular interventions for atherosclerotic carotid or cardiac diseases, we did control for major diagnoses and events that are known indications for these procedures. Thus, the confounding effect of these interventions on our results should be minimal. Additionally, although it is possible that some patients in the non-operative group may have other unmatched co-morbidities, a study showed that less than one-third of patients with primary hyperparathyroidism underwent parathyroidectomy despite the fact that most patients had no significant co-morbidity.31 Strengths of our study include the population representativeness, the large sample size, and the long follow-up among all patients over 65 years often until they die, that allowed careful characterization of incidence of major cardiovascular and major cerebrovascular outcomes.
Conclusions
Older patients with primary hyperparathyroidism had increased risk of major cerebrovascular and major cardiovascular events compared to patients with a similar risk profile without the disease, especially men. Parathyroidectomy was associated with decreased risk of these major life-threatening events; patients with hypertension may benefit the most from surgery. Institutions should improve their practice patterns to identify and treat patients with primary hyperparathyroidism more effectively, and elderly patients with the disease should be referred for surgical intervention, especially if they have comorbidities associated with increased cardiovascular risks.
Supplementary Material
Funding Source:
This research was funded by the Intramural Research Program of the National Cancer Institute and the Supplemental Technology Award Review System from the National Institutes of Health Office of Science and Technology Resources, grant ID 944.
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
References
- 1.Yeh MW, Ituarte PH, Zhou HC, et al. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab. 2013;98(3):1122–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silverberg SJ, Shane E, Jacobs TP, Siris E, Bilezikian JP. A 10-year prospective study of primary hyperparathyroidism with or without parathyroid surgery. N Engl J Med. 1999;341(17):1249–1255. [DOI] [PubMed] [Google Scholar]
- 3.Walker MD, Fleischer JB, Di Tullio MR, et al. Cardiac structure and diastolic function in mild primary hyperparathyroidism. J Clin Endocrinol Metab. 2010;95(5):2172–2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pepe J, Cipriani C, Sonato C, Raimo O, Biamonte F, Minisola S. Cardiovascular manifestations of primary hyperparathyroidism: a narrative review. Eur J Endocrinol. 2017;177(6):R297–R308. [DOI] [PubMed] [Google Scholar]
- 5.Walker MD, Silverberg SJ. Cardiovascular aspects of primary hyperparathyroidism. J Endocrinol Invest. 2008;31(10):925–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stefenelli T, Abela C, Frank H, et al. Cardiac abnormalities in patients with primary hyperparathyroidism: implications for follow-up. J Clin Endocrinol Metab. 1997;82(1):106–112. [DOI] [PubMed] [Google Scholar]
- 7.Stefenelli T, Mayr H, Bergler-Klein J, Globits S, Woloszczuk W, Niederle B. Primary hyperparathyroidism: incidence of cardiac abnormalities and partial reversibility after successful parathyroidectomy. Am J Med. 1993;95(2):197–202. [DOI] [PubMed] [Google Scholar]
- 8.Dalberg K, Brodin LA, Juhlin-Dannfelt A, Farnebo LO. Cardiac function in primary hyperparathyroidism before and after operation. An echocardiographic study. Eur J Surg. 1996;162(3):171–176. [PubMed] [Google Scholar]
- 9.Persson A, Bollerslev J, Rosen T, et al. Effect of surgery on cardiac structure and function in mild primary hyperparathyroidism. Clin Endocrinol (Oxf). 2011;74(2):174–180. [DOI] [PubMed] [Google Scholar]
- 10.Vestergaard P, Mollerup CL, Frokjaer VG, Christiansen P, Blichert-Toft M, Mosekilde L. Cardiovascular events before and after surgery for primary hyperparathyroidism. World J Surg. 2003;27(2):216–222. [DOI] [PubMed] [Google Scholar]
- 11.Agarwal G, Nanda G, Kapoor A, et al. Cardiovascular dysfunction in symptomatic primary hyperparathyroidism and its reversal after curative parathyroidectomy: results of a prospective case control study. Surgery. 2013;154(6):1394–1403; discussion 1403–1394. [DOI] [PubMed] [Google Scholar]
- 12.Murphy SL, Kochanek KD, Xu J, Arias E. Mortality in the United States, 2020. NCHS Data Brief. 2021(427):1–8. [PubMed] [Google Scholar]
- 13.Quilao RJ, Greer M, Stack BC, Jr. Investigating the potential underdiagnosis of primary hyperparathyroidism at the University of Arkansas for Medical Sciences. Laryngoscope Investig Otolaryngol. 2020;5(4):773–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu B, Haigh PI, Hwang R, et al. Underutilization of parathyroidectomy in elderly patients with primary hyperparathyroidism. J Clin Endocrinol Metab. 2010;95(9):4324–4330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim SM, Shu AD, Long J, et al. Declining Rates of Inpatient Parathyroidectomy for Primary Hyperparathyroidism in the US. PLoS One. 2016;11(8):e0161192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heath H, 3rd, Hodgson SF, Kennedy MA. Primary hyperparathyroidism. Incidence, morbidity, and potential economic impact in a community. N Engl J Med. 1980;302(4):189–193. [DOI] [PubMed] [Google Scholar]
- 17.Jinnouchi H, Sato Y, Sakamoto A, et al. Calcium deposition within coronary atherosclerotic lesion: Implications for plaque stability. Atherosclerosis. 2020;306:85–95. [DOI] [PubMed] [Google Scholar]
- 18.Rubin MR, Rundek T, McMahon DJ, Lee HS, Sacco RL, Silverberg SJ. Carotid artery plaque thickness is associated with increased serum calcium levels: the Northern Manhattan study. Atherosclerosis. 2007;194(2):426–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schillaci G, Pucci G, Pirro M, et al. Large-artery stiffness: a reversible marker of cardiovascular risk in primary hyperparathyroidism. Atherosclerosis. 2011;218(1):96–101. [DOI] [PubMed] [Google Scholar]
- 20.Vestergaard P, Mosekilde L. Cohort study on effects of parathyroid surgery on multiple outcomes in primary hyperparathyroidism. BMJ. 2003;327(7414):530–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koufakis T, Antonopoulou V, Grammatiki M, et al. The Relationship between Primary Hyperparathyroidism and Thrombotic Events: Report of Three Cases and a Review of Potential Mechanisms. Int J Hematol Oncol Stem Cell Res. 2018;12(3):175–180. [PMC free article] [PubMed] [Google Scholar]
- 22.Pretorius M, Lundstam K, Heck A, et al. Mortality and Morbidity in Mild Primary Hyperparathyroidism: Results From a 10-Year Prospective Randomized Controlled Trial of Parathyroidectomy Versus Observation. Ann Intern Med. 2022;175(6):812–819. [DOI] [PubMed] [Google Scholar]
- 23.Chen H, Parkerson S, Udelsman R. Parathyroidectomy in the elderly: do the benefits outweigh the risks? World J Surg. 1998;22(6):531–535; discussion 535–536. [DOI] [PubMed] [Google Scholar]
- 24.Park SY, Scotting O, Yen TWF, Evans DB, Wang TS, Dream S. Underdiagnosis of primary hyperparathyroidism in patients with osteoarthritis undergoing arthroplasty. Surgery. 2021. [DOI] [PubMed] [Google Scholar]
- 25.Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg. 2016;151(10):959–968. [DOI] [PubMed] [Google Scholar]
- 26.Kebebew E, Duh QY, Clark OH. Parathyroidectomy for primary hyperparathyroidism in octogenarians and nonagenarians: a plea for early surgical referral. Arch Surg. 2003;138(8):867–871. [DOI] [PubMed] [Google Scholar]
- 27.Stechman MJ, Weisters M, Gleeson FV, Sadler GP, Mihai R. Parathyroidectomy is safe and improves symptoms in elderly patients with primary hyperparathyroidism (PHPT). Clin Endocrinol (Oxf). 2009;71(6):787–791. [DOI] [PubMed] [Google Scholar]
- 28.Bachar G, Gilat H, Mizrachi A, et al. Comparison of perioperative management and outcome of parathyroidectomy between older and younger patients. Head Neck. 2008;30(11):1415–1421. [DOI] [PubMed] [Google Scholar]
- 29.Biertho L, Chu C, Inabnet WB. Image-directed parathyroidectomy under local anaesthesia in the elderly. Br J Surg. 2003;90(6):738–742. [DOI] [PubMed] [Google Scholar]
- 30.Joliat GR, Guarnero V, Demartines N, Schweizer V, Matter M. Recurrent laryngeal nerve injury after thyroid and parathyroid surgery: Incidence and postoperative evolution assessment. Medicine (Baltimore). 2017;96(17):e6674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yeh MW, Wiseman JE, Ituarte PH, et al. Surgery for primary hyperparathyroidism: are the consensus guidelines being followed? Ann Surg. 2012;255(6):1179–1183. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


