Abstract
Purpose
To report a case of bilateral peripheral ulcerative keratitis (PUK) in a patient with underlying Sézary syndrome.
Observations
A 58-year-old male presented with bilateral corneal ulceration with stromal thinning and was diagnosed with PUK. He was actively being treated for Sézary syndrome, a cutaneous T-cell lymphoma. He had no lagophthalmos or other adnexal abnormalities that would lead to ocular surface breakdown. A systemic autoimmune and infectious workup for PUK was unremarkable. His keratitis resolved after treatment with oral prednisone.
Conclusions and importance
We describe a previously undocumented association of PUK with Sézary syndrome in a patient without adnexal disease.
Keywords: Peripheral ulcerative keratitis, Sézary syndrome, Mycosis fungoides
1. Introduction
Peripheral ulcerative keratitis (PUK) is an uncommon, vision-threatening, corneal disease that may be idiopathic (Mooren ulcer) or a manifestation of an underlying systemic process. It is characterized by progressive peripheral corneal thinning in association with an overlying epithelial defect. Most PUK cases are associated with an underlying auto-immune disease.1 Rheumatoid arthritis (RA) is the most common underlying etiology but PUK is also known to be associated with granulomatosis with polyangiitis (GPA), polyarteritis nodosa (PAN), Sjögren's syndrome, relapsing polychondritis, giant cell arteritis, and others.1 Infections cause approximately one fifth of PUK cases and the etiologies of these infections are broad.1 Rarely, PUK has been reported in association with malignancies such as acute myeloid leukemia (AML) and chronic myeloid leukemia (CML).1 We report a novel case of bilateral PUK in a patient with Sézary syndrome, a late-stage cutaneous T-cell lymphoma.
2. Case report
A 58-year-old male was referred for bilateral corneal ulcers in January 2023. He had undergone failed treatment with ciprofloxacin drops (gtt) and Prokera lens bilaterally. His past medical history was notable for Sézary syndrome, first diagnosed in January 2022. At the time of presentation, his Sézary syndrome was late-stage and he was actively undergoing treatment with extracorporeal electrophoresis (ECP). He had no previous history of significant eye disease or surgery.
Upon presentation, his vision was 20/20 in the right eye (OD) and 20/150 in the left eye (OS). Intraocular pressure (IOP) was normal in both eyes (OU). His examination was significant for a 1.5 mm × 1.0 mm epithelial defect in the inferior midperipheral cornea with 50 % stromal thinning OD and a 2.1 mm × 1.2 mm epithelial defect in the inferior midperipheral cornea with 90 % stromal thinning OS. No stromal infiltrate was present in either eye. He had no eyelid or adnexal abnormalities. He had normal vertical palpebral fissures and excellent lid closure in each eye. Eyelids were well positioned against the globe with no ectropion or entropion.
After our initial evaluation, this patient was diagnosed with PUK and was started on daily oral prednisone 80 mg, topical tobramycin, aggressive lubrication, and was placed in bilateral bandage contact lenses (BCL). A broad and comprehensive infectious and autoimmune lab workup including anti-dsDNA, ANCA titers, CRP, anti-CCP antibodies, ESR, uric acid, rheumatoid factor, QuantiFERON TB, lysozyme, ACE, Lyme, ANA, syphilis, Hepatitis panel (A, B, and C) was obtained and was unremarkable.
With treatment, his epithelial defects rapidly improved over several days and eventually healed. His visual acuity remained 20/20 in the right eye and improved to 20/40 in the left eye. The oral prednisone was tapered at a rate of 10 mg weekly until 30 mg daily, at which point the taper was slowed to 5 mg weekly. He was stable on 10 mg daily at his last and most recent visit in May 2023. Slit lamp photos were obtained two weeks after disease onset (Fig. 1A and B) and again after several months (Fig. 2A and B).
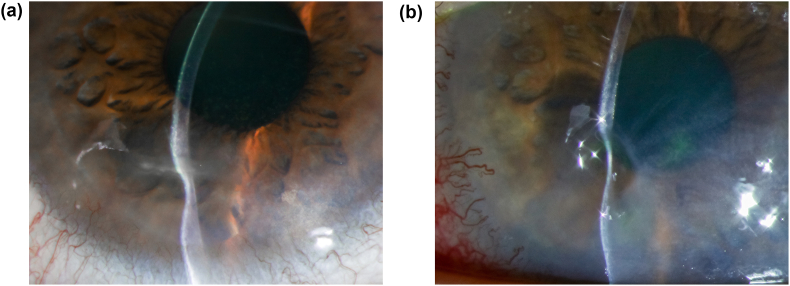
Fig. 1.
External slit lamp photographs at 2 weeks after initial presentation. 1A.) Inferior paracentral stromal thinning with resolved epithelial defect OD. 1B.) Focal severe inferonasal stromal thinning OS.
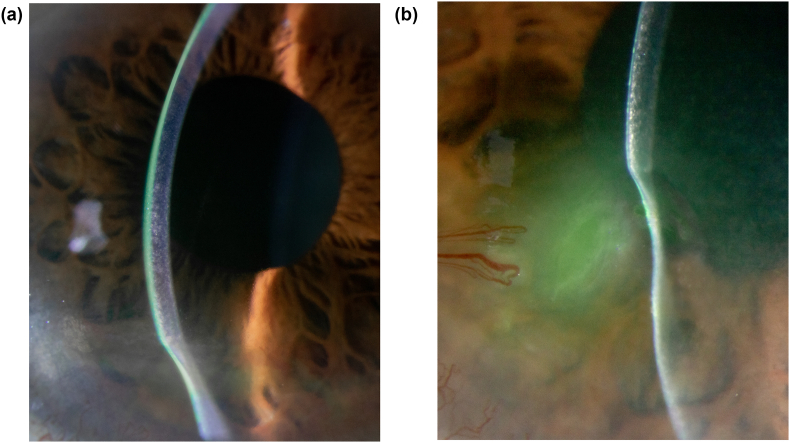
Fig. 2.
External slit lamp photographs at 3 months after initial presentation. 2A.) Stable inferior paracentral stromal thinning OD. 2B.) Stable focal severe inferonasal stromal thinning with fluorescein pooling and adjacent superficial neovascularization OS.
3. Discussion and conclusions
We present a patient with Sézary syndrome who developed bilateral PUK despite ongoing systemic treatment for his malignancy with ECP. PUK has been associated with numerous systemic diseases, including but not limited to rheumatoid arthritis, ANCA vasculitis, lupus, polyarteritis nodosa, Sjögren's syndrome, sarcoidosis, Behçet's disease, relapsing polychondritis, seronegative spondyloarthropathies, giant cell arteritis, eosinophilic granulomatosis with polyangiitis, infection, HIV, and rarely malignancies such as acute myeloid leukemia (AML) and chronic myeloid leukemia (CML).1,2 On review of the literature on PubMed, we also found very few cases of PUK associated with non-leukemic malignancies including gastric adenocarcinoma, invasive ductal carcinoma, metastatic follicular thyroid carcinoma, and sebaceous cell carcinoma.2,3 We could find only two cases of corneal ulceration associated with Sézary syndrome. In these cases, the cause of ulceration was likely due to adnexal disease rather than true PUK.4,5
PUK is typically defined by progressive, painful peripheral corneal ulceration and thinning, not explained by trauma, adnexal disease, ocular surface disease, or infectious process.6 The pathogenesis is incompletely understood; however, the current literature implicates both humoral and cell-mediated immune processes.6 It is thought that circulating immune complexes are deposited in the peripheral cornea and stimulate a complement response that triggers an immunologic cascade.6,7 In the subsequent cascade there is recruitment of proteolytic enzymes that lead to breakdown of extracellular matrix components in the cornea.1,6,7 Auto-antibodies against corneal stromal antigens are also postulated to play a role in the corneal destruction.1 T-cells become involved and can be directly cytotoxic to the cornea or may aid in the dysregulated pro-inflammatory immune response.1
Mycosis fungoides (MF) and Sézary syndrome are the most common forms of cutaneous T-cell lymphoma.8 Sézary syndrome is a late progression of MF and is characterized by generalized erythroderma, lymphadenopathy, and circulating Sézary cells.8 Given the rarity of these diseases, incidence and prevalence are difficult to determine; however, Assaf et el estimated the prevalence of MF in Germany to be approximately 7–8 patients per 100,000 while Sézary syndrome is approximately 0.2–0.5 patients per 100,000.9 Early-stage MF may not limit life expectancy; however, late-stage MF or Sézary syndrome portends a poor prognosis with a median survival of less than 5 years.8 The largest case series examining the ocular manifestations of mycosis fungoides was written by Stenson in 1981 and featured 30 patients with biopsy proven mycosis fungoides.4 11 of the 30 patients had ocular findings; tumor involvement of the eyelids was the most common manifestation with 8 of the 11 patients.4 Only 2 patients had corneal changes but neither case was consistent with PUK; one patient had interstitial keratitis. The other was a patient with a history of extensive eyelid disease, multiple eyelid surgeries, poor follow up, and chronic peripheral keratitis over several years that culminated in the necrosis and perforation of both corneas.4 Histology of the corneal buttons after penetrating keratoplasty demonstrated mycosis fungoides cells in the cornea.4
Finally, Livingstone et al. reported a Sézary syndrome patient with cicatricial eyelid disease, severe exposure keratopathy, and Pseudomonas corneal ulcer with hypopyon that progressed to perforation despite aggressive topical therapy.5 The patient underwent enucleation, and pathology revealed limbal infiltration of atypical lymphoid cells consistent with Sézary cells.5 Rather than PUK, the etiology of the ulceration in this case was likely exposure keratopathy secondary to the patient's cicatricial eyelid disease and bacterial superinfection.5
Our patient offers several important distinctions from these cases. First, our patient had excellent lid closure without evidence of exposure, entropion, or other significant ocular surface disease. Second, our patient's keratitis resolved after treatment with oral prednisone. We excluded other underlying etiologies with a broadly negative infectious and inflammatory workup.
Given the possibility of PUK being idiopathic in nature, it is impossible to say definitively that this patient's disease process is secondary to his Sézary syndrome. The exact mechanism underlying our patient's PUK is not completely understood. It may be related to the deposition of circulating immune complexes in the peripheral cornea or due to his abnormal T-cells causing immune dysregulation or direct cytotoxicity. In conclusion, this is a case of PUK related to Sézary syndrome that responded to high-dose oral prednisone and topical therapy. This case emphasizes the importance of maintaining a wide differential when evaluating a patient with PUK. It also establishes MF and Sézary syndrome as causative diseases to consider when evaluating a patient with undifferentiated PUK.
Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal identifying information.
Acknowledgements and disclosures
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship. No other acknowledgements.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
None.
Contributor Information
Michael J. Maywood, Email: Mikemaywood1@gmail.com.
David G. Heidemann, Email: dgheidemann@gmail.com.
Chirag K. Gupta, Email: chirag.gupta@corewellhealth.org.
References
- 1.Hassanpour K., ElSheikh R.H., Arabi A., et al. Peripheral ulcerative keratitis: a review. J Ophthalmic Vis Res. 2022;17(2):252–275. doi: 10.18502/jovr.v17i2.10797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De la Maza M.S., Foster C.S. Peripheral ulcerative keratitis and malignancies. Cornea. 1994;13(4):364–367. doi: 10.1097/00003226-199407000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Foo V.H.X., Mehta J., Chan A.S.Y., Ong H.S. Case report: peripheral ulcerative keratitis in systemic solid tumour malignancies. Front Med. 2022;9(May):1–6. doi: 10.3389/fmed.2022.907285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stenson S., Ramsay D.L. Ocular findings in mycosis fungoides. JAMA Ophthalmol. 1981;99(February):272–277. doi: 10.1001/archopht.1981.03930010274010. [DOI] [PubMed] [Google Scholar]
- 5.Livingstone I., Ramamurthi S., Drummond S., Kemp E., Roberts F. Corneal perforation due to limbal involvement in Sézary syndrome. Graefes Arch Clin Exp Ophthalmol. 2011;249(7):1091–1094. doi: 10.1007/s00417-010-1611-7. [DOI] [PubMed] [Google Scholar]
- 6.Gomes B.F., Santhiago M.R. Biology of peripheral ulcerative keratitis. Exp Eye Res. 2021;204(January) doi: 10.1016/j.exer.2021.108458. [DOI] [PubMed] [Google Scholar]
- 7.Sura A.A., McCallum R.M. Peripheral ulcerative keratitis due to systemic diseases. Curr Opin Ophthalmol. 2022;33(6):543–550. doi: 10.1097/ICU.0000000000000895. [DOI] [PubMed] [Google Scholar]
- 8.Kamijo H., Miyagaki T. Mycosis fungoides and Sézary syndrome: updates and review of current therapy. Curr Treat Options Oncol. 2021;22(2) doi: 10.1007/s11864-020-00809-w. [DOI] [PubMed] [Google Scholar]
- 9.Assaf C., Dobos G., Zech I.M., Doess A., May M., Jadasz J. Epidemiology of mature T/NK-cell lymphomas in Germany – a representative cross-sectional study based on SHI claims data. JDDG J Ger Soc Dermatology. 2023;(June):1–8. doi: 10.1111/ddg.15187. [DOI] [PubMed] [Google Scholar]