Abstract
Background
One of the most feared complications of hydrocephalus is shunt migration. Although rare, bowel migration is the most commonly encountered type of migration. The relatively high frequency of this occurrence allowed us to gather a substantial number of reports for study.
Objectives
The aim of this study was to better understand this complication and aid in decreasing its incidence.
Methods
The PubMed and Scopus databases were searched for cases of anal shunt migration. In total, 49 records describing 56 clinical cases were included in this review. Additionally, we present and include the clinical case of a patient managed by our team; therefore, 57 cases were included in this study. Relevant parameters were collected, organized, analyzed, and discussed. This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement from 2009.
Results
Extrusion through the anus was observed in 82% of cases, 68% of which were in males. The age range varied from 1 month to 75 years. Congenital hydrocephalus was the etiology in 66% of cases. The time interval between shunt insertion and migration varied from 12 days to 19 years. In 70% of patients, the tube was pulled out through the anus, whereas a laparotomy or laparoscopy was used in 14% of cases. Infectious complications were noted in 35% of patients. The overall outcome was mostly favorable; two patients died as a complication of the migration.
Conclusions
Bowel and anal shunt migration is a relatively rare complication occurring predominantly within the initial weeks after the initial surgery. This condition leads to infectious complications, which can potentially be life-threatening. Urgent management is required, and in most cases, the removal of the shunt through the anus is sufficient. Early intervention generally results in favorable outcomes.
Keywords: Anal migration, Bowel migration, Hydrocephalus, Neurogastroenterology, Shunt complication, Shunt migration
المخلص
أهداف البحث:تعترف الدراسة بأن إدارة موه الرأس نسبيا بسيطة، إلا أنه لا تزال هناك بعض المضاعفات التي يمكن أن تؤثر على التشخيص. واحدة من المضاعفات الأكثر إثارة للخوف هي هجرة التحويلة. على الرغم من ندرتها، إلا أن هجرة الأمعاء هي أكثر أنواع الهجرة شيوعا. تم جمع تقارير كافية للدراسة. الهدف هو فهم هذه المضاعفة بشكل أفضل للحد من حدوثها.
طرق البحث:شملت الدراسة مراجعة حالات هجرة التحويلة الشرجية من قواعد بيانات "ببميد" و "سكوبوس". ما مجموعه ٤٩ سجل تم تضمينها تصف ٥٦ حالة سريرية. تم تضمين حالة سريرية إضافية تم إدارتها بواسطة فريق الدراسة، مما يجعل المجموع ٥٧ حالة. جمعت وحللت الدراسة البيانات الديموغرافية والسريرية، ونهج الإدارة، والنتائج، وغيرها من المعايير ذات الصلة. تم تضمين حالات اختراق الأمعاء، وهي عامل أولي للإخراج الشرجي. التزمت الدراسة ببيان العناصر المفضلة للتقارير في الاستعراضات المنهجية والتحليلات التلوية من عام ٢٠٠٩.
النتائج:تم ملاحظة الإخراج الشرجي في ٨٢٪ من الحالات، وكان 68% منهم من الأطفال الذكور. كانت الفئة العمرية من شهر واحد إلى ٧٥ سنة، مع فقط ١٨٪ تشمل المرضى فوق سن ١٤ عاما. كانت موه الرأس الخلقي هو السبب في ٦٦٪ من الحالات. تفاوت الفاصل الزمني بين إدخال التحويلة والهجرة بشكل كبير من 12 يوم إلى 19 عام. وفي 55% من الحالات، حدثت الهجرة خلال الـ 12 شهرا الأولى، بينما حدثت 7 حالات في السنة الثانية، و8 حالات في السنة الثالثة، و3 حالات في السنة الرابعة، و6 حالات بعد 4 سنوات. في 70% من المرضى، تم سحب الأنبوب من خلال فتحة الشرج، بينما تم استخدام فتح البطن أو منظار البطن في 14% من الحالات. تم ملاحظة مضاعفات معدية، بما في ذلك التهاب السحايا، في ٣٥٪ من المرضى. تم الإبلاغ عن ست حالات فقط من التهابات الجهاز الخارجي العصبي، بما في ذلك حالتين من التهاب الصفاق وأربع حالات من الخراج تحت الجلد والمجموعات المصابة. كانت النتيجة الإجمالية إيجابية في الغالب، على الرغم من وفاة مريضين بسبب مضاعفات الهجرة.
الاستنتاجات: هجرة التحويلة الشرجية والأمعاء، على الرغم من ندرتها، هي مضاعفة مهمة تكون ملاحظتها بشكل رئيسي في الأطفال الذكور. يحدث هذا في الغالب خلال الأسابيع أو الأشهر الأولى بعد الجراحة الأولية. غالبا ما تؤدي هذه الهجرة إلى مضاعفات معدية داخل الجهاز العصبي المركزي، والتي يمكن أن تهدد الحياة. المطلوب إدارة عاجلة، وفي معظم الحالات، تكون إزالة التحويلة من خلال فتحة الشرج كافية، ما لم تكن هناك مؤشرات واضحة لإجراء جراحة في البطن، مثل التهاب الصفاق. يؤدي التدخل المبكر في العادة إلى نتائج إيجابية، مما يبرز أهمية العلاج بالمنظار لموه الرأس.
الكلمات المفتاحية: الهجرة الشرجية, الهجرة المعوية, موه الرأس, علم الأعصاب والجهاز الهضمي, مضاعفات القسطرة, هجرة القسطرة
Introduction
Hydrocephalus, one of the most common pathologies in neurosurgery, remains a healthcare challenge in underdeveloped countries. The management of hydrocephalus is one of the earliest techniques learned by resident neurosurgeons during training. Although this condition is generally considered relatively simple to manage through shunting methods or endoscopic treatment, potential complications can nonetheless affect prognosis. One of the most dreaded complications is shunt migration, which can occur to any part of the body, including the limbs,1 and can affect various organs, such as the heart, liver, stomach, and urogenital organs. Although bowel migration is rare, it is the most frequently encountered type of migration. This relatively high frequency enabled us to gather a substantial number of reports for inclusion in this study aimed at better understanding this complication and ultimately decreasing its incidence.
Materials and Methods
Literature review
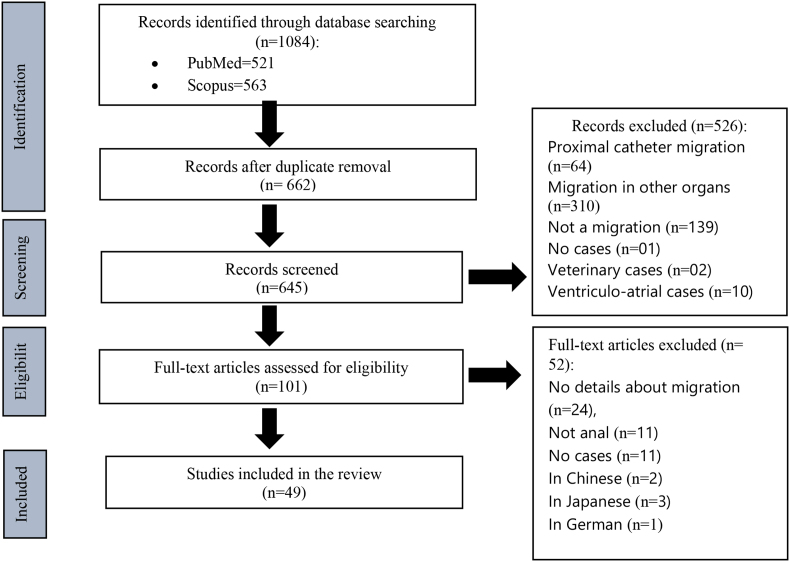
A comprehensive search was conducted in the PubMed and Scopus databases to retrieve journal articles by using the keywords “ventriculoperitoneal,” “shunt,” and “migration.” No date restrictions were applied during the search. In total, 563 records were identified in Scopus, and 521 results were found in PubMed. All records were imported into an online version of Endnote, where duplicates were merged, thus resulting in 662 unique records. After removal of duplicates, 645 records underwent screening on the basis of their abstracts. After the screening, 526 records were excluded for various reasons: 64 were associated with proximal catheter migration, 310 described migration in other organs, 139 did not pertain to migration, 1 had no reported cases, 2 were focused on veterinary cases, and 10 involved ventriculo-atrial cases. For 18 records, the full texts could not be screened. After thorough evaluation of the full texts, 52 records were excluded: 24 lacking details about migration, 11 not associated with anal migration, 11 not involving any cases, 2 in Chinese, 3 in Japanese, and 1 in German. This review included 49 records providing descriptions of 56 clinical cases of anal ventriculoperitoneal shunt (VPS) migration (Figure 1). A case of subdural peritoneal shunt was included in the study. Additionally, the clinical case of a patient managed by our team, which we believe is directly relevant to this review, was presented and included. Consequently, a total of 57 cases were included in this study (as presented in Table 1). Various parameters were collected, organized, analyzed, and discussed, including the year of publication, geographic distribution, demographics, indication for VPS, age at the time of VPS placement, side of VPS, time between insertion and migration, repeat migration, extrusion through the anus, surgical technique, infectious complications, site of intestinal perforation, general examination findings, and shunt model used. Bowel perforation cases were included in this review, because we considered this condition to be a preliminary factor for anal extrusion. Cases that did not focus on migration were deemed non-useful and were excluded from the review. Importantly, this study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses2 statement from 2009. However, the protocol for this systematic review was not registered.
Figure 1.
Flowchart of study selection process.
Table 1.
Summary of reviewed cases.
| Authors | Years | Age | Out |
|---|---|---|---|
| King | 1976 | 2 m | Yes |
| – | – | ||
| Arico et al. | 1985 | 4 y | Yes |
| Gelabert et al. | 1987 | 1 m | Yes |
| 10 y | Yes | ||
| Azzam | 1988 | – | Yes |
| Sharma et al. | 1988 | 23 m | Yes |
| Latcham | 1996 | 4.5 m | Yes |
| Swan | 1996 | 14 y | Yes |
| Jindal et al. | 1999 | 3 y | Yes |
| Nourisamie et al. | 2001 | 10 m | No |
| Yousfi et al. | 2003 | 24 y | Yes |
| Thipphavong et al. | 2004 | 12 y | Yes |
| Akcora et al. | 2006 | 6 y | Yes |
| Nakahara et al. | 2006 | 62 y | No |
| Aquino et al. | 2006 | 18 y | Yes |
| Sengul et al. | 2007 | 4 m | Yes |
| Zhou et al. | 2007 | 18 m | Yes |
| Matsuoka et al. | 2008 | 4 y | Yes |
| Kanojia et al. | 2008 | – | Yes |
| Birbilis et al. | 2009 | 54 y | Yes |
| Chiang et al. | 2010 | 4 y | Yes |
| Kumar et al. | 2010 | 3 y | Yes |
| Oliveira et al. | 2011 | 30 m | Yes |
| Glatstein et al. | 2011 | 11 y | Yes |
| Ozturk et al. | 2012 | 2 y | Yes |
| Sharifian et al. | 2012 | 30 m | Yes |
| Mihajlović et al. | 2012 | 6 m | Yes |
| Elizabeth et al. | 2013 | 1 y | Yes |
| Knuth et al. | 2013 | 42 y | No |
| Chang et al. | 2014 | 75 y | Yes |
| Wang et al. | 2014 | 32 m | Yes |
| Bansal et al. | 2015 | 1 y | Yes |
| Thiong'o et al. | 2015 | 7 m | Yes |
| 18 m | Yes | ||
| Bales et al. | 2016 | 29 y | Yes |
| Udoh et al. | 2016 | 3 y | No |
| Sarkari et al. | 2016 | 2 y | Yes |
| Chugh et al. | 2018 | 7 y | Yes |
| 11 m | Yes | ||
| 8 m | Yes | ||
| Parshuram et al. | 2018 | 6 y | Yes |
| Burhan et al. | 2018 | 3 y | Yes |
| 3 y | Yes | ||
| Marino et al. | 2019 | 2 m | Yes |
| Ghritlaharey | 2019 | 10 y | No |
| Bakshi. | 2020 | 8 m | Yes |
| Cardinale et al. | 2020 | 3 m | Yes |
| İştemen et al. | 2020 | 18 m | Yes |
| 2.5 y | No | ||
| White et al. | 2021 | 51 y | No |
| Alhendawy et al. | 2021 | 13 y | Yes |
| Shiro et al. | 2021 | 20 y | No |
| Bal'afif et al. | 2022 | 2 y | No |
| Şahin et al. | 2022 | 30 m | Yes |
| Lammamr et al. | 2022 | 74 y | No |
| Our case | 2022 | 11 m | Yes |
Case report
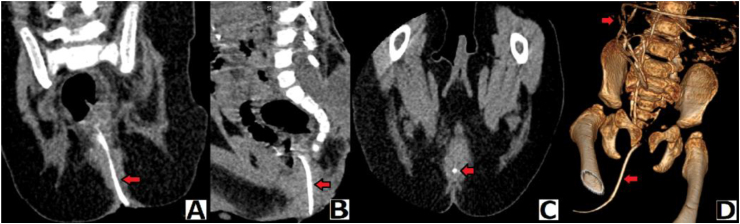
Our patient was an 11-month-old boy born from a non-consanguineous marriage as part of a twin pregnancy. The child had lumbar myelomeningocele and hydrocephalus. When he was 6 months old, our team performed myelomeningocele sac removal and VPS. During the post-operative period, delayed healing of the lumbar wound due to CSF leakage was observed. After discharge, the patient underwent regular follow-up through multidisciplinary consultations involving neurosurgery, pediatric care, and functional rehabilitation. After 4 months, during which the patient showed some improvement in his lower limb motor deficit, the parents observed the presence of a valve tube at the edge of their child's anus. Because they assumed that the presence of the valve tube at the edge of the child's anus was normal, the parents delayed seeking medical consultation until approximately 10 cm of the tube had protruded from the anus. At admission, the patient was conscious but presented with a fever of 38.3 °C and exhibited slight symptoms of meningitis syndrome. Clear CSF was observed dribbling from the distal tip of the catheter and draining into his diaper (Figure 2). A trans-fontanellar ventricular puncture was performed, which revealed CSF with a citrine appearance, containing more than 300 elements per cc, with lymphocytic predominance, elevated protein levels, and diminished glucose levels. No bacterial pathogens were isolated from the CSF. The child was immediately started on dual antibiotic therapy consisting of cefotaxime and gentamicin. An emergency abdominal CT scan was performed to trace the complete catheter trajectory (Figure 3). Because this condition was recognized as a reported, albeit rare, complication of VPS, the patient was promptly admitted to the operating room. The shunt was removed in an aseptic manner: the proximal end of the shunt was extracted from the ventricle, and was followed by the distal tube, which was disconnected from its proximal side and withdrawn from the anus. The surgeons determined that the patient's bowel had self-sealed and did not require additional direct repair. Subsequently, an external ventricular drainage was inserted. Three weeks later, the child showed clinical improvement with no fever, and the CSF appearance had returned to normal. The laboratory analysis revealed no signs of meningitis. Because the child did not exhibit symptoms of peritonitis, the bowel perforation was believed to have healed spontaneously. The patient was readmitted to the operating room, and the external drainage was removed, and reinsertion of a VPS was performed. The postoperative course was uneventful, and the child was discharged 3 days later.
Figure 2.
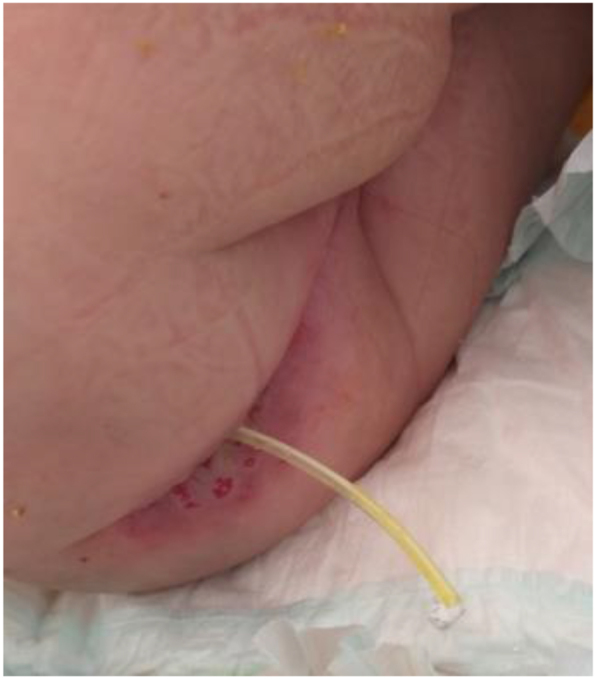
Preoperative photograph showing the VPS tube passing through the anus with CSF leakage.
Figure 3.
Preoperative abdomino-pelivian CT. A: coronal, B: sagittal, C: axial, and D: 3D reconstruction, showing the distal VPS catheter in intra- and extra-abdominal positions (arrow).
Abbreviations
CSF: cerebrospinal fluid; VPS: ventriculoperitoneal shunt.
Results
Externalization through the anus was observed in 82% of cases (46 of 56 cases for which this detail was provided). Among those cases, 80% (46 cases) were reported in the past 20 years (since 2003). A total of 29% of cases (13 cases) were from India, 14% (8 cases) were from Turkey, and 10% (6 cases) were from the United States. The sex of the patients was determined in 53 cases: 68% in males (36 cases) and 32% in females (17 cases), with a sex ratio of 2.12. The age of the patients was specified in 54 cases, and varied across all age groups, ranging from 1 month to 75 years. However, only 18% of cases (ten cases) involved patients older than 14 years. Among the 50 cases in which the etiology of hydrocephalus was specified, 66% (33 cases) were attributed to congenital causes, including 22% (11 cases) with myelomeningocele and 14% (7 cases) with post-meningitis hydrocephalus. Other etiologies included post-traumatic hemorrhage, obstructive hydrocephalus, and normal pressure hydrocephalus. Additionally, 10% of the patients (six cases) had a confirmed history of abdominopelvic surgery or radiation therapy. In 25 patients, the confirmed placement of the shunt was as follows: 64% (16 cases) on the right side, 32% (8 cases) on the left side, and 4% (1 case) with bilateral placement. Among the 46 patients with confirmed information regarding the age at which the shunt was placed, 57% (26 children) underwent the procedure in the first year of life, 30% (14 children) were between 1 and 14 years of age, and 13% (6 patients) were operated on when they were older than 14 years. The delay between shunt insertion and migration was determined in 53 cases, and ranged from 12 days to 19 years. In 55% of the cases (29 cases), migration occurred within the first 12 months, whereas seven cases occurred in the second year, eight cases occurred in the third year, three cases occurred in the fourth year, and six cases occurred after 4 years (Figure 4). No cases of repeat migration through the anus or bowel were observed. In 43 cases, information regarding the technique of tube removal was obtained. In 70% of patients (30 cases), the tube was pulled through the anus, either directly or with endoscopic control. In 14% (six cases), a laparotomy or laparoscopy was performed for tube removal. In 11% (five cases), the surgeons associated laparotomy/laparoscopy with subsequent tube extraction through the anus. In one case, without provision of specific details, the tube was pulled from the cervical region, and in another intriguing case, the shunt migrated to the rectum and passed through the anus spontaneously in preparation for colonoscopy. Details regarding infectious complications in the central nervous system were obtained in 51 patients. In 63% (32 cases), no evidence of infection was found, whereas 35% (18 patients) were diagnosed with meningitis. In one patient, the microbiological study was negative, but air was observed in the brain ventricles. Meningitis was associated with ventriculitis in four patients, brain abscess was observed in three patients, and empyema was found in one patient. In some cases, specific pathogens were isolated, including Escherichia coli in four cases; Staphylococcus aureus in three cases; Klebsiella pneumoniae, Streptococcus faecalis, Enterococcus gallinarum, Serratia marcescens, Proteus vulgaris, Citrobacter freundii, Enterobacter cloacae, group B Streptococcus, Enterobacteria, and Enterococcus in one case; Gram-negative bacteria in one case; and Enterococcus in another case. The sites of bowel perforation were defined in 23 cases: eight cases in the transverse colon, seven cases in the descending colon, four cases in the rectosigmoid colon, one case in the ascending colon, two cases in the small bowel, and one case in the ileum. General examination findings were available for 47 patients, 40% (19 patients) of whom showed positive signs of systemic inflammation. Only six cases of extranervous system infections were reported: two cases of peritonitis and four cases of subcutaneous abscess and infected collections. The outcome was specified in 49 cases, 45 of which achieved good outcomes. One patient presented a duplication of the ileum but had a good outcome after surgery. Another patient experienced a small amount of hematochezia 2 weeks after the procedure. Two patients died as a complication of the migration. The shunt models described in the study included Chhabra in six cases; Hakim in two cases; Pudenz in two cases; and other models, such as Holter, Upadahayaya, Bactiseal, and Silastic, in additional cases.
Figure 4.
Graphical representation of ventriculoperitoneal shunt migration incidence after shunt insertion over time.
Discussion
This review focused on anal migration, because it is the most common manifestation of bowel migration.3 Colonic perforation caused by VPS is a rare mechanical complication accounting for only 0.1% of operated cases.4 Although approximately one-third of the cases in this review were in India, no clear geographic distribution or racial predominance was observed. In recent years, reports and reviews have increasingly addressed VPS bowel perforation, possibly because improvements in healthcare coverage have increased the number of VPS procedures performed and subsequently the reporting of complications. In this review, bowel and anal migration were found to be more frequent in males, in agreement with findings from other studies.3 Although shunt migration can occur in individuals of all ages, anal migration is rarely observed in the adult population, and most cases are reported in pediatric populations, possibly because of the fragility of the bowel in children,3,5 as well as the higher rate of intestinal motility in children than adults. Additionally, the delay in intestinal motility is greater in the adult colon than the child colon,6 thus possibly explaining why the site of perforation in this review was frequently the colon. On the basis of the rationale provided, most patients reviewed in this study were children with congenital hydrocephalus. The presence of myelomeningocele in many patients with VPS migration, as observed in this review and other studies,3 suggests a potential motility disorder. Exploring the field of neurogastroenterology might provide further explanations regarding the pathophysiology underlying this phenomenon. Additionally, the absence of repeat migration cases in this review suggested that migration events are individual and not necessarily associated with any preexisting condition. The review also indicated that migration can occur shortly after shunting, even within the first few days or weeks after surgery. However, the risk of migration decreases significantly within the first 4 years, and the risk persists thereafter but is considerably diminished, as shown in Figure 4. Although only six patients in this review had undergone previous abdominal surgery, three were adults, accounting for nearly one-third of the adult population. Given that most VPS placements are traditionally performed on the right side, the finding that most migration cases in this series were on the right side might not be significant. Regarding tube removal, in two-thirds of the reviewed cases, the tube was aseptically removed distally. Detaching the tube proximally and pulling it from the anus can help prevent the transport of microorganisms proximally. Some authors favored laparotomy or laparoscopy for the treatment of suspected peritonitis,7 repair of the perforation site,8 or exploration laparotomy/laparoscopy.9 Moreover, in most cases, protrusion occurs several weeks or months after surgery, and because few adhesions are usually present in the tube tract, pulling it out appears to be easy and safe. Some authors favor transanal repair of the defect.10 On the basis of the uniformly good outcomes observed in this review with simple tube pulling, we agree with the majority of authors3 that pulling the catheter from the anus and administering antibiotics with clinical observation is generally sufficient unless suspicion of peritonitis is present. As expected, more than one-third of the cases presented with central nervous system sepsis, predominantly meningitis, but also abscesses, empyema, and ventriculitis. This finding emphasizes the serious nature of this complication and the need for urgent management. Gram-negative bacteria, particularly E. coli, were frequently implicated in infectious events, as seen in most reviews.3 Gram-positive bacteria, particularly S. aureus, were also found, albeit less frequently. Although approximately half the patients exhibited systemic inflammatory signs, only six patients had localized infections, mainly subcutaneous infections, along with two cases of peritonitis. Therefore, signs suggestive of retrograde infection should be carefully investigated, starting from the peritoneum, skin, and central nervous system.
In neurosurgical practice, distal catheters that rarely exceed 120 cm in length are typically addressed, and a maximum of 35 cm is introduced into the intra-abdominal cavity. Therefore, a catheter that protrudes through the anus would logically have a perforation point in the colon, particularly if it remains connected or near the proximal catheter. In this review, only three patients were found to have extra-colic perforation points, and the tube did not reach the anus in in any of those cases. Overall, the outcomes in this review were generally good with prompt management. However, two patients died directly as a result of this complication, thus further emphasizing the serious nature of the condition and the need for urgent management. Although the Chhabra shunt was the most frequently cited model implicated in migration in this review, other shunt models were also present. Given that the exact pathophysiology of migration is not yet fully understood, proposing technical solutions for bowel perforation was not discussed in this review. Finally, we agree with the opinion of Volkan Etus that anal protrusion is an opportunity for early diagnosis of bowel perforation and therefore early management.5 Sometimes in routine practice, physicians are faced with the choice of leaving an old catheter that is difficult to retrieve. However, with the increasing number of migration cases, surgeons must importantly make additional efforts to remove these foreign bodies.11,12
Conclusion
Bowel and anal shunt migration is a relatively rare but significant complication, observed particularly frequently in male children, and occurring most commonly within the first weeks or months after the initial surgery. This complication can lead to frequent infectious complications in the central nervous system, which can potentially be fatal. Therefore, urgent management is necessary. In most cases, pulling the shunt from the anus can be sufficient unless a clear indication exists for abdominal surgery, such as suspected peritonitis. Early management of this complication generally leads to favorable outcomes. One important lesson from our case, as well as other cases in this review, is the need to explain the normal position of the shunt to patients and their families, and to make them aware of the possibility of this complication. Additionally, any patient with a VPS who presents with persistent abdominal symptoms should be thoroughly evaluated for potential bowel migration. These complications underscore the importance of considering endoscopic treatment options for hydrocephalus.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
There are no ethical issues.
Consent
The parents consented (both the father and mother) to the use of their child's case in a scientific research paper without revealing his identity.
Authors contributions
KA: guarantor, literature search, data acquisition, statistical analysis. AF: manuscript review. BT: author: concept, design, manuscript preparation. AM: manuscript review, final approval of the version to be published. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgment
The authors would like to express their gratitude to Dr. Bouazid Iskander, a pediatric surgeon, for his valuable assistance in the operating room during the removal of the migrated shunt. His expertise and support were greatly appreciated in the successful management of the patient.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Nourisamie K., Vyas P., Swanson K.F. Two unusual complications of ventriculoperitoneal shunts in the same infant. Pediatr Radiol. 2001 Nov;31(11):814–816. doi: 10.1007/s002470100545. PMID: 11692241. [DOI] [PubMed] [Google Scholar]
- 2.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7) doi: 10.1371/journal.pmed.1000097. Epub 2009 Jul 21. PMID: 19621072; PMCID: PMC2707599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harischandra L.S., Sharma A., Chatterjee S. Shunt migration in ventriculoperitoneal shunting: a comprehensive review of literature. Neurol India. 2019 Jan-Feb;67(1):85–99. doi: 10.4103/0028-3886.253968. PMID: 30860103. [DOI] [PubMed] [Google Scholar]
- 4.Snow R.B., Lavyne M.H., Fraser R.A. Colonic perforation by ventriculoperitoneal shunts. Surg Neurol. 1986 Feb;25(2):173–177. doi: 10.1016/0090-3019(86)90289-2. PMID: 3941987. [DOI] [PubMed] [Google Scholar]
- 5.Etus V. Ventriculoperitoneal shunt catheter protrusion through the anus: case report of an uncommon complication and literature review. Commentary. Childs Nerv Syst. 2011 Nov;27(11):2015. doi: 10.1007/s00381-011-1555-1. Epub 2011 Aug 9. PMID: 21826450. [DOI] [PubMed] [Google Scholar]
- 6.Wasson W.W. Study of the gastro-intestinal tract of children and its relation to the adult. Radiology. 1941;37(3):277–283. [Google Scholar]
- 7.Akcora B., Serarslan Y., Sangun O. Bowel perforation and transanal protrusion of a ventriculoperitoneal shunt catheter. Pediatr Neurosurg. 2006;42(2):129–131. doi: 10.1159/000090470. PMID: 16465086. [DOI] [PubMed] [Google Scholar]
- 8.Burhan B., Serdar K.B., Abdurrahman A., Edip A.M., Ebuzer D. Abdominal complications of ventriculoperitoneal shunt in pediatric patients: experiences of a pediatric surgery clinic. World Neurosurg. 2018 Oct;118:e129–e136. doi: 10.1016/j.wneu.2018.06.140. Epub 2018 Jun 26. PMID: 29959071. [DOI] [PubMed] [Google Scholar]
- 9.Aricó M., Beluffi G., Fiori P., Chiari G., Pezzotta S., Podesta A.F., et al. Rectal extrusion of the catheter and air ventriculography following bowel perforation in ventriculo-peritoneal shunt. Pediatr Radiol. 1985;15(1):53–55. doi: 10.1007/BF02387854. PMID: 3969296. [DOI] [PubMed] [Google Scholar]
- 10.Chiang L.L., Kuo M.F., Fan P.C., Hsu W.M. Transanal repair of colonic perforation due to ventriculoperitoneal shunt – case report and review of the literature. J Formos Med Assoc. 2010 Jun;109(6):472–475. doi: 10.1016/S0929-6646(10)60079-4. Erratum in: J Formos Med Assoc. 2010 Oct;109(10):774. Fan, Bih-Juan [corrected to Fan, Pi-Chuan]. PMID: 20610149. [DOI] [PubMed] [Google Scholar]
- 11.Shiro T., Akai T., Yamamoto S., Kashiwazaki D., Tomita T., Kuroda S. A case of intestinal perforation with a residual shunt tube placed during childhood: should we remove the non-functioning tube? Childs Nerv Syst. 2022 Jul;38(7):1389–1392. doi: 10.1007/s00381-021-05414-2. Epub 2021 Nov 15. PMID: 34779898. [DOI] [PubMed] [Google Scholar]
- 12.Thipphavong S., Kellenberger C.J., Rutka J.T., Manson D.E. Hepatic and colonic perforation by an abandoned ventriculoperitoneal shunt. Pediatr Radiol. 2004 Sep;34(9):750–752. doi: 10.1007/s00247-004-1195-7. Epub 2004 May 26. PMID: 15164137. [DOI] [PubMed] [Google Scholar]