Abstract
A special unit was set up in an associate teaching hospital to provide a fast-track route for the assessment of acute adult surgical and urological referrals. During an audit period of eight weeks, this surgical assessment unit had 550 referrals, of which 196 (36%) came via the accident and emergency (A&E) department; the other 354 came directly from general practitioners or other hospital departments. Mondays, Tuesdays and Fridays were the busiest days of the week; 57% of all patients arrived between 8 am and 5 pm. 68% were seen by a doctor within 1 hour of their arrival. 68% were either discharged or admitted to the main surgical wards within 4 hours. The study showed that, over the course of a year, the surgical assessment unit might divert some 2301 patients away from the A&E department. To achieve this total it would need to be open and appropriately staffed 24 hours a day. Such a unit offers a strategy for limiting the A&E workload and streamlining the assessment of patients with surgical and urological emergencies.
INTRODUCTION
The initial assessment of most patients referred to hospitals with acute surgical and urological conditions takes place in accident and emergency (A&E) departments.1,2 However, with the numbers of patients presenting as emergencies increasing by up to 5% per year,3-5 these departments experience increasing difficulty in coping with their workload. An additional pressure is the target for patients to spend no more than 4 hours in the A&E department. For non-surgical patients medical assessment units have proved their worth,6 and some hospitals allocate a special area of such units for general surgery emergency patients.7 However, there is only one published report on a surgical assessment unit (SAU).8
When considering the possible merits of an SAU at our hospital we found, in a three-month audit, that the ratio of emergency to elective surgical admissions within general surgery and urology was 1.5 to 1—confirming the impression that emergencies form a major part of the workload in these two specialties. Yet these patients are customarily tagged on to the elective component of the workload and commonly encounter delays. We therefore devised an SAU that would provide a fast-track route for adult (age 16 years and over) emergency surgical and urological referrals, allowing rapid diagnosis and, where appropriate, early access to operating theatres. This paper reports on a prospective eight week audit of activity within the SAU.
PATIENTS AND METHODS
The SAU was created by the allocation of a bay on a general surgical ward. There are six trolleys on which patients can be assessed, with a waiting area for 6 more patients. The unit is staffed 24 hours a day by at least one registered nurse who is trained in the care of surgical patients. The registered nurse is usually assisted by a nursing assistant/auxiliary. Ancillary and clerical support is provided during working hours and the unit has a computer link to the hospital intranet and laboratory service. Unstable patients in need of immediate resuscitation and patients with blunt or penetrating trauma are assessed in the A&E department and are either admitted to the main ward or discharged without going through the SAU. As a matter of policy, assessment is undertaken in the SAU only after the case has been discussed by the referring clinical personnel, usually a doctor, with the middle-grade member of the on-call surgical or urological team. Medical staff timetables were reorganized to ensure that members of the surgical team, including consultants, had no fixed elective commitments while on-call. In addition an operating theatre was made available during working hours exclusively for patients presenting acutely.
This study was undertaken on patients who attended the SAU during the eight weeks between 15 November 2003 and 10 January 2004. In keeping with current targets that limit patients' stay in A&E departments, we set a target for maximum stay on the unit of 4 hours. To achieve this, a second target was created stipulating that all patients were to be seen by a doctor within 1 hour of arrival in the SAU. Once the patients had been assessed and the results of investigations were available, a decision was made by the appropriate middle-grade doctor or consultant to admit to one of the surgical wards or discharge the patient back to primary care. Children under the age of 16 years were admitted directly to a paediatric ward so were not included. Data were collected prospectively on a specially designed proforma and later logged onto a spreadsheet for subsequent analysis. Data collected included the patient's demographic details, source of referral, presenting complaints, date and time of referral, time of arrival in the SAU, time taken for the patient to be seen by a member of the on-call team and total time the patient spent in the SAU.
RESULTS
During the study period 550 patients were referred to the SAU, 281 (51%) male. Their mean age was 51 years (range 16–93). 328 (59%) patients were referred from general practitioners, 196 (36%) came from the A&E department and 26 (5%) were from other sources such as the surgical outpatients department and non-surgical specialties. Mondays, Tuesdays and Fridays were the busiest days, Saturdays and Sundays the least busy (Table 1).
Table 1.
Variation of activity according to day of the week
| No. (%) of patients referred | No. (%) of patients waiting >1 h to be seen by a doctor | No. (%) of patients spending >4 h in the SAU | |
|---|---|---|---|
| Monday | 100 (18) | 36 (23) | 32 (22) |
| Tuesday | 94 (17) | 16 (10) | 26 (18) |
| Wednesday | 74 (13) | 17 (11) | 18 (12) |
| Thursday | 82 (15) | 23 (15) | 20 (14) |
| Friday | 90 (16) | 30 (19) | 31 (21) |
| Saturday | 58 (11) | 20 (13) | 7 (5) |
| Sunday | 52 (9) | 12 (8) | 11 (8) |
| Total | 550 | 154 | 145 |
SAU=surgical assessment unit
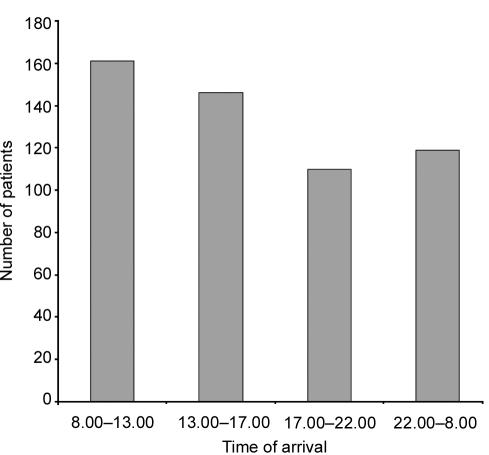
Out of 543 patients for whom data were available, 424 (78%) were referred to the surgical team on-call and the other 119 to the urology team on-call. The distribution of presenting complaints within each specialty is shown in Table 2. The interval between referral and arrival in the unit was recorded in 536 patients; 432 (81%) of these arrived within 2 hours of referral. Whilst most patients arrived between 8 am and 5 pm there was a steady flow throughout the 24 hours (Figure 1).
Table 2.
Distribution of presenting complaints
| Presenting complaint | No. (%) |
|---|---|
| General surgery (n=424) | |
| Abdominal pain (unspecified) | 107 (25) |
| Appendicitis/right iliac fossa pain | 60 (14) |
| Abscess | 54 (13) |
| Upper abdominal pain | 54 (13) |
| Ano-rectal problem (excluding abscess) | 31 (7) |
| Diabetic/ischaemic foot | 26 (6) |
| Painful/obstructed hernia | 20 (5) |
| Bowel obstruction | 19 (4) |
| Diverticulitis/left iliac fossa pain | 10 (2) |
| Head injury | 10 (2) |
| Postoperative problem | 10 (2) |
| Others | 23 (5) |
| Urology (n=119) | |
| Renal pain/colic | 44 (37) |
| Urinary retention | 26 (22) |
| Scrotal/testicular | 18 (15) |
| Haematuria | 15 (13) |
| Penile problem | 6 (5) |
| Catheter problem | 5 (4) |
| Urinary tract infection | 5 (4) |
Figure 1.
Time of arrival of patients (n=536)
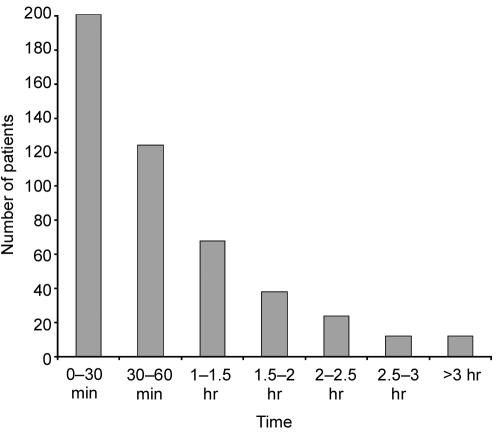
All patients were initially assessed by a registered nurse within 5 minutes of arrival in the SAU. The time that patients waited to see a doctor is shown in Figure 2; in the 479 patients for whom this information was recorded, the median time was 45 minutes (interquartile range 20–80). 325 (68%) patients were seen within 1 hour of arrival. Of the 154 patients who waited for more than 1 hour to see a doctor, 108 (70%) had arrived between 8 am and 5 pm. Mondays and Fridays were the days when patients were most likely to wait more than 1 hour (Table 1).
Figure 2.
Distribution of waiting times to be seen by a doctor (n=479)
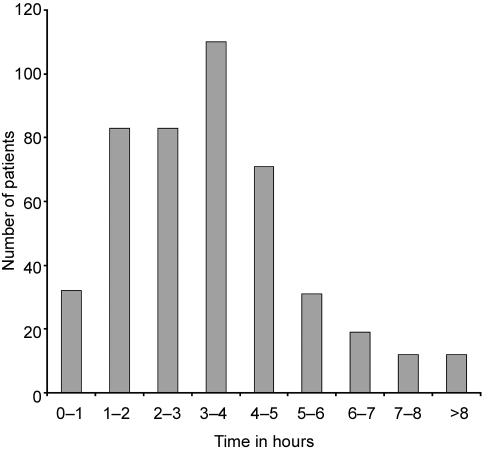
Figure 3 shows the time patients spent in the SAU before admission to a ward or discharge home. Median duration of stay was 3.25 hours (interquartile range 2.0–4.0). Of the 453 patients for whom the data were recorded 308 (68%) left the SAU within 4 hours of their arrival. Of the 145 patients whose stay extended beyond 4 hours, 109 (75%) arrived between 8 am and 5 pm. Mondays and Fridays were the days on which patients were most likely to spend over 4 hours in the unit (Table 1).
Figure 3.
Distribution of time spent in surgical assessment unit (n=453)
DISCUSSION
The most important finding, in terms of alleviating pressures on the A&E department, was that 64% of patients seen in the SAU came from sources other than the A&E department. These patients would have had to be seen in the A&E department if there had been no SAU. Extrapolation of this figure indicates that, over the course of a year, the SAU would divert 2301 patients away from the busy A&E department. The results also indicate that, to cater for the wide range of ages of patients presenting with the full range and severity of acute surgical and urological disease processes, the SAU should ideally be staffed by qualified persons 24 hours a day. We would add that the concentration of acute surgical and urological conditions in the SAU provides excellent educational opportunities for surgical trainees, medical students and nursing staff.
Our data revealed that 68% of patients were seen within 1 hour by a doctor and a similar proportion of patients left the SAU within 4 hours of their arrival. Clearly, we need to improve on this performance; however, there was no conclusive proof that more than an hour's wait to see a doctor was a reason why some patients spent more than 4 hours in the unit. Excessive waits were experienced by surgical and urological patients in equal measure and seemed not to be influenced by source of referral. Mondays and Fridays were the days of longest waits, and part of the reason may be that these are the busiest days for clinical support services such as the pathology laboratories and imaging departments.
In conclusion, the SAU can divert a substantial number of patients from the increasingly busy A&E department and provides a separate facility for rapid assessment and management by senior surgical staff. However, the unit ideally should be staffed 24 hours a day, with reorganization of staff timetables to develop the concept of an 'emergency surgical team' who have no elective commitments when oncall. The SAU then becomes the hub of emergency surgical activity.
Acknowledgments
We thank all the consultant general surgeons and urologists at Medway Maritime Hospital for allowing us to collect data on their patients, and the nursing staff on the SAU for their contributions to data collection.
References
- 1.Perry EP, Crisp JC, Watkin DFL. Changes in emergency surgery between 1973 and 1982: audit of workload of one surgical team. Ann R Coll Surg Engl 1989;71: 341-3 [PMC free article] [PubMed] [Google Scholar]
- 2.Dookeran KA, Bain I, Moshakis V. Audit of general practitioner referrals to a surgical assessment unit: new methods to improve the efficiency of the acute surgical service. Br J Surg 1996;83: 1544-7 [DOI] [PubMed] [Google Scholar]
- 3.Capewell S. The continuing rise in emergency admissions. BMJ 1996;312: 991-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Campbell WB, Lee EJK, Van de Sijpe K, Gooding J, Cooper MJ. A 25 year study of emergency surgical admissions. Ann R Coll Surg Engl 2002;84: 273-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chezian C, Pye J, Jenkinson LR. The mext millennium—are we becoming emergency surgeons? A seven-year audit of surgical and urological admissions in a rural district hospital. Ann R Coll Surg Engl 2001;83: 117-20 [PMC free article] [PubMed] [Google Scholar]
- 6.Wald D, Batty K, Dewhurst G, Holman R. Medical assessments units: a realistic solution? Br J Health Care Management 2001;7: 273-7 [Google Scholar]
- 7.Watkin DLF, Layer GT. A 24-hour snapshot of emergency general surgery in the UK. Ann R Coll Surg Engl 2002;84(suppl): 194-9 [Google Scholar]
- 8.Rowe PH, Lawrence WT, Fellows E. The management of emergency surgical patients in a surgical assessment unit. Ann R Coll Surg Engl 2003;85(suppl): 274-7 [Google Scholar]