After going through a gloomy period of increased infections, no sign of affordable treatment for the majority of infected patients, no vaccines in human trials, denial that HIV causes AIDS and stigmatization of infected persons, Southern Africa, the epicentre of the AIDS pandemic,1 is in a state of renewed hope. We begin to think in terms of eradicating new infections and substantially reducing the fatality rate in those infected. What has changed? Clearly, the main reason for optimism is a drastic reduction by pharmaceutical companies in the price of antiretroviral drugs and the roll-out of treatment through Government support. A second is the initiation of a phase I trial to test vaccines that incorporate the antigens of Southern African HIV subtype C. A third is the increased empowerment of women, who through unequal and submissive relationships have often been deprived of choices in protecting themselves against the virus. Finally, in a limited number of groups in and around major cities of South Africa, antiretroviral treatment under ideal conditions—skilled clinical staff, appropriate infrastructure, monitoring of compliance and viral load—has achieved success rates very similar to those in Europe and the USA. This indicates that antiretroviral therapy can work in South Africa, though treatment centres especially in the rural areas will need to be greatly upgraded to meet the challenges.
A multi-pronged strategy
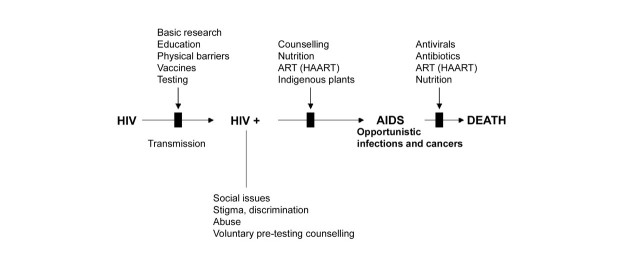
A multi-pronged approach to management is outlined in Figure 1. Only a decade has passed since South Africa freed itself from the shackles of apartheid, and the nation remains beset with inequities in education, life skills and socioeconomic conditions, further complicated by diversities in culture and languages. This legacy has greatly hindered education on HIV prevention, especially on the regular use of condoms, and is a large part of the reason why transmission rates exceed those in the rest of the world.2 South Africa needs to step back from the existing mass media campaigns and develop a more personal programme of education. For an example of how a nation can lower its transmission rates through a consistent and continuing programme, spearheaded by its leaders, we need only to look at Uganda. The programme should be delivered in the language of those concerned and should focus on the routes and consequences of HIV infection, how it can be prevented and where to get oneself tested. But no educational programme can hope to eradicate HIV infection. For this we must look to a vaccine, and the phase I (safety) clinical trial at the Chris Hani-Baragwanath Hospital, Soweto, is an encouraging development. Time will tell whether this candidate vaccine will be effective. Despite the vast body of accumulated knowledge on HIV, we have yet to identify a component of the virus that generates sterilizing immunity. Clearly, development of effective vaccines awaits further information on pathogenesis and how the virus evades host defences; such intensive basic research is too expensive for countries such as South Africa, and progress with vaccines depends heavily on support for this work in developed countries.
Figure 1.
A multi-pronged approach to HIV infection. ART=antiretroviral therapy; HAART=highly active antiretroviral therapy
No disease in history has caused such social turmoil in Southern Africa. Families have been wrecked through the death of parents from AIDS. HIV-infected persons commonly experience not only social stigmatization but also discrimination in the workplace. Fortunately, attitudes do seem to be changing. Women’s activists are educating young women to take control of their lives. The mining companies, major employers in South Africa whose workforce has a high proportion of migrant works infected with HIV, have now made bold decisions to cover antiretroviral therapy for all infected employees. Universities, including my own, have set aside budgets for voluntary testing and pre-testing counselling, as well as for treatment of students and staff. Laws are in place to counter discrimination, and activists who fought for universal treatment have at last persuaded the Government to negotiate pricing with manufacturers and roll out treatment for all. HIV infection is no longer a death sentence with the cruel world looking the other way. Central to the strategy of management of HIV is drug treatment; but it cannot succeed without appropriate nutrition, effective counselling and good adherence. The side-effects of antiretroviral drugs are such that long-term treatment demands compassionate support. Agents with fewer side-effects would help greatly, and a high priority in South Africa should be the exploration of the diverse plant species for potential new antiviral substances. Already there are anecdotal reports of indigenous plant extracts arresting progression of HIV infection to AIDS without side effects. These extracts warrant rigorous scientific analysis and our group has been doing just that; indeed, the very first extract that we examined proved to have potent antiviral activity in minute concentrations. An additional issue is treatment for opportunistic infections, especially tuberculosis, in patients with AIDS. As well as antiretroviral therapy the programme needs to include treatments for these infections, with antivirals and antibiotics.
Potential obstacles to the treatment programmes
Is drug resistance likely to hamper the programme? In the National Institute for Communicable Diseases, Lynn Morris, who leads the HIV/AIDS surveillance programme, has conducted a detailed examination of drug resistance as a consequence of the failure of antiretroviral therapy completely to eliminate HIV replication.3 A key finding from this study is that there are no drug-resistant variants amongst HIV-1 subtype C infected individuals in South Africa. This is reassuring. However, viruses from patients in whom antiretroviral treatment had failed all showed resistance in the reverse transcriptase gene. Morris’s study was confined to patients taking a single drug, neviraprine; presumably resistance will be less troublesome with the highly active antiretroviral therapy delivered under the roll-out programme. Another potential obstacle to the treatment programmes is the current lack of support for the infrastructure and the skilled staff in the public sector, especially in rural areas where the disease has ravaged entire villages.
Relevance of Southern African experience to other countries
The first lesson from experience in Southern Africa is that, in future, no nation should be so slow to react to a public health crisis. Secondly, effective education in health and hygiene can go a long way in preventing the spread of a sexually transmitted disease. Thirdly, antiretroviral therapy under ideal conditions can work well in a developing country. Fourthly, a vaccine that provides sterilizing immunity is the ultimate but still distant goal. And, lastly, we must continue to look for new antiretroviral agents – especially, in our case, by examining the natural products so abundant in our surroundings.
Acknowledgments
This editorial was to have been prepared by Dr Johnny Sachs, a highly respected colleague who passed away earlier this year. GJK is a Senior International Wellcome Trust Fellow for Biomedical Sciences in South Africa. I thank Dr Di Hardie for useful discussion and Mr AbduRehman for assistance with the graphics.
References
- 1.Wilson D, Naidoo S, Bekker L-G, Cotton M, Maartens G, eds. Handbook of HIV Medicine. Oxford: Oxford University Press, 2002
- 2.Regensberg, LD, Hislop MS. A report back on more than four years of HIV/AIDS disease management in Southern Africa. S J HIV Med 2003;10: 7–10 [Google Scholar]
- 3.Morris L. Surveillance of HIV drug resistance: implications for treatment programs and transmission of resistance. Commun Dis Surveillance Bull (NICD) 2003: 5–6