Abstract
Background
Cancer is the leading cause of death for Southeast Asian women in the U.S. Southeast Asian women have significantly high rates of breast and cervical cancers, yet are least likely to obtain regular mammography and Pap testing of all racial/ethnic groups in the U.S.
Objectives
The purpose of this study is to compare a tailored navigation intervention delivered by bilingual and bicultural Community Health Advisors to information and reminder only to increase age-appropriate breast and cervical cancer screening completion among Southeast Asian women.
Methods
The Southeast Asian Women's Health Project study will enroll 232 Cambodian, Filipino, Lao, and Vietnamese women who are not up to date with their breast and cervical cancer screenings. Women randomized to navigation will receive the intervention for 10 weeks. Women in the information group will be mailed information on mammography and Pap testing only. All participants will be contacted post-enrollment to assess screening completion.
Discussion
We will examine intervention efficacy, predictors of each intervention group, and the influence of intergenerational exchange of breast and cervical cancer screening information between mothers and daughters. We will disseminate study results locally to the community, nationally at conferences, and through peer-reviewed journals.
Keywords: Tailored navigation, Southeast Asian, Dyad, Mother and daughter, Cancer screening, Community health advisor
Abbreviations
- APIM
Actor-Partner Interdependence Models
- CCAB
Cultural Community Advisory Board
- CHA
Community Health Advisor
- FQHC
Federally Qualified Health Center
- RCT
Randomized Controlled Trial
- REDCap
Research Electronic Data Capture
- SEAWHP
Southeast Asian Women's Health Project
- SEM
Structural Equation Modeling
- TIMS©
Tailored Intervention Messaging System
- TN
Tailored Navigation
1. Introduction
Cancer is the leading cause of death for Southeast Asian refugee and immigrant women living in the United States [1]. Cambodian, Lao, Vietnamese, and Filipino women, collectively referred to as Southeast Asians, have disproportionately high incidence rates of breast and cervical cancers [2]. Breast cancer incidence increased significantly for all Asian Americans from 1988 to 2013, but the largest increase was among Southeast Asian women (APC = 2.5, 95 % CI 0.8, 4.2) [3]. Cervical cancer incidence continues to be highest among Lao (17.1 per 100,000) and Cambodian (16.7 per 100,000) women compared to all racial/ethnic women in the U.S [5].
Despite evidence that regular screening through mammography and Pap testing reduces breast and cervical cancer mortality [4,5], Southeast Asian women continue to have strikingly low screening rates, and range between 16 % among Cambodians [6] to 85 % among Lao [7]. Similarly, mammography screening is suboptimal with rates ranging between 50.7 % among Cambodian 74 % to Vietnamese women [7,8]. Among Filipino women, mammography rates declined from 81.6 % to 62.1 % from 2008 to 2010 [9].
Low breast and cervical cancer screening rates are exacerbated by limited knowledge of cancer detection, misconceptions about screening, lack of linguistic and culturally appropriate care, lack of having a regular health care provider, and limited English proficiency [10]. Culturally tailored messages in conjunction with ethnically matched navigators have been effective in promoting cancer prevention and early detection and increasing cancer screening in refugee and immigrant populations [[11], [12], [13], [14], [15]]. Cultural tailoring can enhance the relevance of health education materials for racial/ethnic minority populations, such as refugees and immigrants [16,17]. While Southeast Asians are not culturally homogenous, certain key barriers impact cancer screening across different groups [[18], [19], [20]]. They also share common traditional health practices and a unique sociopolitical, such as a history of war and displacement, and migration experience which may influence cancer screening behaviors and increase the risk for breast and cervical cancer in exposed individuals. For this study, we will focus on women from four specific Southeast Asian populations living in the U.S.: Cambodian, Filipino, Lao, and Vietnamese.
2. Methods
2.1. Study design
This study is a randomized controlled experimental design to test the efficacy of a tailored navigation delivered by Community Health Advisors (CHAs) to increase age-appropriate breast and cervical cancer screening completion compared to an information and reminder-only control group (see Fig. 1). Bilingual and bicultural CHAs will use the Tailored Intervention Messaging System (TIMS©) [21] message library to educate and navigate women from Southeast Asian communities into the health clinic to obtain age-appropriate breast (mammogram) and cervical cancer (Pap test) screenings. TIMS© is a library of messaging on benefits, barriers, risk, self-efficacy, and knowledge that has been extensively tested in several racial/ethnic groups in the U.S. [21,22] and was adapted to address the needs of Southeast Asian women in the current study.
Fig. 1.
Participant course of study.
2.2. Primary and secondary aims
The primary aim (AIM 1) of the study is to test the efficacy of tailored navigation intervention delivered by bilingual/bicultural community health advisors (CHA + TN) compared to an information and reminder-only control to increase age-appropriate breast and cervical cancer screening completion among intergenerational Southeast Asian mother-daughter dyads. The secondary aim (AIM 2) is to examine the underlying mechanisms (both mediating and moderating factors) associated with the intervention (CHA + TN) that influence breast and cervical cancer screening completion. Lastly, the third aim is to explore in greater detail the influence of intergenerational exchange of information between mothers and daughters related to breast and cervical cancer screening.
2.3. Inclusion and exclusion criteria
The inclusion and exclusion criteria are detailed in Table 1.
Table 1.
Inclusion and exclusion criteria.
| Inclusion | Exclusion |
|---|---|
| Female | Have been previously diagnosed with breast and/or cervical cancer |
| Live in Ohio | |
| Self-identify as Cambodian, Filipino, Lao, or Vietnamese | |
| Aged 21 years and older | |
| Non-adherent for mammogram, Pap test, or both | |
| Have a mother or daughter aged 21 years or older |
2.4. Cultural Community Advisory Board
The study convenes a Cultural Community Advisory Board (CCAB) comprised of individuals from the target communities who are local leaders, knowledgeable about the culture and language of the communities, and interested in women's health issues. The CCAB has worked with the research team since the conception of the project and helped to ensure that the project is culturally sensitive and responsive to the communities. The role of the CCAB is to help identify resources and organizations to support the project, serve as a liaison between the research team and communities, identify potential bilingual/bicultural CHAs and recruitment locations, provide guidance on culturally appropriate and relevant measures and data collection procedures, and participate in problem-solving with the research team. We will work closely with the CCAB to ensure that our interpretation of the findings is fair and accurate and provide input on how best to disseminate the results back to the community.
2.5. Recruitment
Ethnically matched CHAs will recruit participants in several ways including, but not limited to, recruiting from identified community sites, via word-of-mouth, email, and/or social media. We will use written, electronic, and verbal methods of recruitment. For example, recruitment flyers will be posted at various community locations that Southeast Asians frequent including businesses, temples, and churches. Electronic announcements will be sent to the list serves of various organizations, such as the Cambodian Mutual Assistance Association and the Lao Mutual Assistance Association, and student organizations for distribution or emailed to contacts, and to be shared on social media. Based on our previous experience, recruitment may primarily be through word-of-mouth. We will rely on the CCAB to assist us with accessing the community by making introductions to key community leaders and members and provide recommendations for recruitment locations [23,24]. A respondent-driven sampling method will also be used in which the enrolled participants will have the option to refer their network of peers into the study [25].
2.6. Enrollment
CHAs will use the participant's preferred language, such as their native language, English or both to enroll potential participants in person, over the phone, or via a video conferencing platform. CHAs will introduce themselves to potential participants and explain what the study is about using the guided conversation from a recruitment script to determine the person's interest in the study. Those individuals who meet the inclusion criteria, as summarized in Table 1, and agree to participate will complete the informed consent process. The consent process will be completed with the participant and project staff either in person or using technology, either by phone or a video platform. All participants will be presented with a copy of the consent document in electronic or paper format. Project Staff will also obtain HIPAA permission and medical record release permission from participants using similar procedures described for the consent. After eligible participants have consented, they will complete a baseline questionnaire, which includes basic demographic information, mammogram and Pap test history, self-efficacy, social support, acculturation, etc. All study materials (consent, HIPAA, baseline questionnaire) are translated into Khmer (language spoken by Cambodians), Lao, and Vietnamese. Based on consultation with Filipino community leaders, we did not translate the materials into Tagalog as most Filipinos are fluent in English. Enrolled participants are randomized into the intervention or control groups.
2.7. Sample size and power
Using Optimal Design [26], we estimated the power for multilevel longitudinal models approximating our study design (ICCs between 0.09 and 0.1). A sample size of 232 with 3 data collection points resulting in ∼1392 observations) will have >80 % power to detect a moderate effect (Cohen's d = 0.35) between group differences in breast, cervical, or both screenings testing at α = .05 for all proposed models. These estimates presume a constant effect over time. The statistical power estimate is based on two sources: a) previous TIMS© intervention studies which demonstrated screening Odds Ratios (OR) of 2.2 and 4.221,22 and b) screening interventions with Southeast Asian women, which reported breast screening uptake ORs ranging from a 2.2 [27] to 6.75 [26] and Pap test uptake ORs ranging from a 2.2 [28,29] to 4.5 [12].
2.8. Randomization
We will randomly assign participants from each ethnic group to the intervention or control group. Random assignment ensures that all eligible participants will have an equal chance of being placed in the intervention or control group. Mother-daughter dyads will be randomized into the same groups.
2.9. Intervention
Tailored navigation will be compared to information only. All follow-up contacts will be completed by project staff either by phone, in person, or on a video platform.
2.10. Navigation
Navigation group (CHA + TN) participants will be contacted by CHAs via phone, in person, or social media platform (Facebook messenger) one week after informed consent and completion of the baseline questionnaire. CHAs will contact participants once a week for up to 10 weeks (a maximum of 10 attempts or until a clinic appointment is made, whichever comes first). Contacts will include voicemail messages or live depending on if CHAs can reach participants. Using the TIMS© message library, the CHAs will engage participants in conversations about breast and cervical cancer screening and navigate the participants to overcome any barriers to screening and motivate them to make a clinic appointment. In addition, daughters will be asked to write three messages for their mothers emphasizing the importance of breast and/or cervical cancer screening and encouraging screening uptake. Similarly, mothers will write three messages for their daughters. These messages will be interwoven into the tailored messages from TIMS©, sent with the screening reminder notecards at 12-months, and act as potential conversation starters at home. Participants who do not have a medical home will be referred to one of our partner healthcare clinics. CHAs will navigate participants to mammogram and/or Pap testing completion and, if needed, will provide necessary assistance to complete screening (e.g., transportation, communication with provider, interpreter services, etc.). Screening completion will be measured by self-report and confirmed via medical record check. At 18-months, CHAs will follow-up with navigation group participants who reported completing a mammogram during the navigation process.
2.11. Information only
Control group (information only) participants will be mailed an informational brochure on mammography and Pap testing one week after enrollment into the study. At 3-months post enrollment, CHAs will conduct a follow-up contact with each participant to assess mammogram and/or Pap testing completion. At 12-months post enrollment, CHAs will contact all control group participants to confirm a scheduled appointment or screening completion. For those who completed a mammogram within the 12 months since enrollment, generic screening reminder notecards will be sent by mail. At 18-months, CHAs will follow-up with those control group participants who reported scheduling a mammogram, Pap smear, or both at the 12-month time point.
2.12. Screening reminders
One of our main objectives is to promote routine screenings in this population. It is important that women obtain regular screenings and not just obtain screenings on a one-time basis [30]. As such, CHAs will mail a reminder notecard post-initial screening to each participant who self-reported completing their first screening to remind them to obtain their next screening per screening guidelines. For the intervention group, these reminder notecards will be personalized with tailored messages from the participants’ dyad partner (i.e., mother or daughter). Control group participants will receive a generic screening reminder notecard adapted from public American Cancer Society educational materials.
2.13. Wait-list
Due to Southeast Asian women having limited resources and experiencing significant barriers to accessing breast and cervical cancer screening services, we will offer the tailored navigation as a wait-listed option to women in the control group after the intervention is completed. This offer will not be a part of the intervention. We will assess who accepted the navigation and screening completion.
2.14. Medical record verification
We will verify self-reported screening completion by reviewing medical records post-intervention.
2.15. Data management
We will use REDCap (Research Electronic Data Capture) on tablets for CHAs to collect/store data. All study data are entered via a password-protected REDCap database website. Project Staff will also be able to collect data on paper to enter and upload into REDCap if needed.
2.16. Data analysis
2.16.1. Data analysis by study aims
AIM 1: To test the efficacy of the intervention, we will fit two series of models, cross-sectional and longitudinal. The cross-sectional logistic regression models will estimate the odds of completing screening. The predictors will be the experimental condition and the covariates of socio-demographic characteristics, acculturation, screening history, cancer beliefs, knowledge about cancer and screening, social support, self-efficacy, social influence, and the intergenerational exchange of information between mothers and daughters. We will test for statistical interventions among all covariates and predictor. We will then fit the series of longitudinal multilevel random effects models with time-varying covariates [31] for breast cancer screening (1st and subsequent screening) and for cervical cancer screening (1st and subsequent screening, per provider recommendation) as predicted by the experimental condition and covariates. The most appropriate covariance structure for the residuals εij will be determined after data collection and correlation of responses over time is estimated. Several covariance structures will be examined, and the resulting models compared for fit using the quasi-likelihood independence model information criterion (QIC) fit using SAS 9.4 (Proc NLMIXED). The SAS 9.4 programming for fitting multilevel longitudinal models 1) with continuous outcomes and 2) with dichotomous outcomes are shown in Table 2.
Table 2.
SAS Codes for data analyses.
| Multilevel longitudinal models with continuous outcomes |
|---|
|
PROC MIXED <options>; BYvariables; CLASSvariable <(REF = option)> … <variable <(REF = option)>> </global-options>; CODE<options>; IDvariables; MODELdependent = <fixed-effects> </options>; RANDOMrandom-effects </options>; REPEATED < repeated-effect> </options>; PARMS (value-list) … </options>; PRIOR<distribution> </options>; CONTRAST’label’ <fixed-effect values … > <|random-effect values … >, …</options>; ESTIMATE’label’ <fixed-effect values … > <|random-effect values … > </options>; LSMEANSfixed-effects </options>; LSMESTIMATEmodel-effect lsmestimate-specification </options>; SLICEmodel-effect </options>; STORE<OUT=>item-store-name </LABEL = 'label'>; WEIGHTvariable; |
| Multilevel dichotomous outcomes in SAS |
|
PROC NLMIXED <options>; ARRAYarray-specification; BOUNDSboundary-constraints; BYvariables; CMPTMODELrequired-options conditionally-required-options <options>; CONTRAST'label' expression <, expression> <option>; ESTIMATE'label' expression <options>; IDnames; MODELmodel-specification; PARMSparameters-and-starting-values; PREDICTexpression OUT=SAS-data-set <options>; RANDOMrandom-effects-specification; REPLICATEvariable; Programming statements; |
AIM 2: We will build models that are more complex by testing moderation and mediation in both the cross-sectional and longitudinal models predicting breast and cervical cancer screening. The predictors are the experimental condition, and the covariates are as listed previously above. Rather than detecting mediated effects with the causal steps approach [31], we will use the Joint Significance Test established [32,33], which assesses the statistical significance of the X to M relation, α path, and then the M to Y relation, β path. If both are statistically significant, there is evidence of mediation. Models with more than one mediator are simply extensions of the single-mediator case. In our multilevel models, we will investigate mediation effects both within the different levels of analyses and across levels. The proposed analyses should allow for increased understanding of the mechanisms underlying intervention effects and different responses among participants.
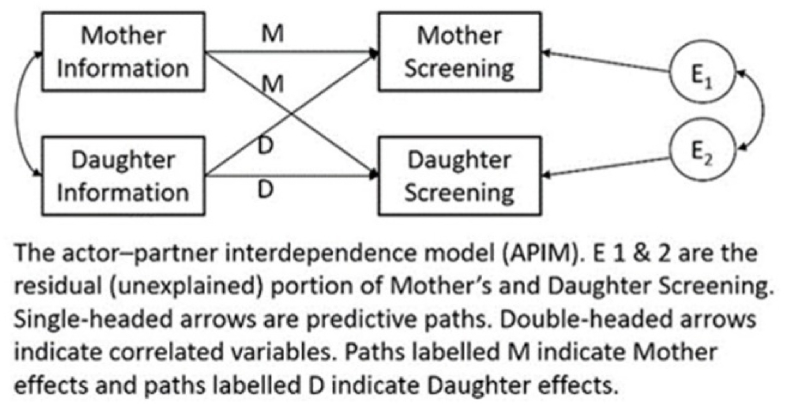
Exploratory AIM 3: To test the influence of intergenerational exchange and solve the statistical problem of non-independence, we will fit a series of actor-partner interdependence models (APIM) in Structural Equation Modeling (SEM) through which we can examine the four potential patterns of this exchange: Mother dominated, Daughter dominated, equal Mother-Daughter effect, and a null effect of (see Fig. 2). The SEM approach has advantages over the ordinary regression analysis approach to testing the APIM: 1) more than one equation can be estimated and tested simultaneously, and 2) the relations between parameters in different equations can be specified [34]. In an APIM, there are three types of predictor variables: between dyads variables, within-dyads variables, and mixed variables [35]. A between-dyads variable is one for which scores are the same for both members of a given dyad, but they differ from dyad to dyad. In this study, the between-dyad variable is the experimental condition; that is, intervention or control group. In contrast, a within-dyads variable is one for which the scores for partners within each dyad are different, but the average score is the same for all dyads. In our model, relationship (mother or daughter) is our within-dyads variable. Finally, a mixed predictor variable is one for which there is variation both within dyads and between dyads.
Fig. 2.
The actor-partner interdependence model.
2.17. Ethics
The study was approved by the academic Institutional Review Board. The five-year project began January 1, 2018, with an anticipated end date of December 31, 2023. The SEAWHP study is registered in clinicaltrials.gov under the identifier NCT04086771.
3. Discussion
The current RCT is designed to test the efficacy of a culturally sensitive, tailored navigation intervention to increase mammography and Pap testing among intergenerational Southeast Asian women, specifically mothers and daughters. Southeast Asian women have significantly high rates of breast and cervical cancers, yet are least likely to obtain regular mammography and Pap testing of all racial/ethnic groups [36]. For women who are from cultures where discussing cancer prevention and early detection is not the norm and perhaps even taboo, timely and sensitive communication about cancer risk and preventive strategies are critical, especially for those who are at high risk for breast and cervical cancer [37,38]. This study's unique focus on intergenerational Southeast Asian women, a highly vulnerable and medically underserved population, has potential to have a lasting impact on women across generations.
3.1. Study design strengths and limitations
The study has several notable strengths. This is a community-engaged RCT with recruitment and implementation by community members (i.e., CHAs) in the community. To our knowledge, this is one of the first studies to engage intergenerational Southeast Asian women, specifically the Lao and Cambodian communities in the U.S., two understudied populations. In addition, our focus on screening behaviors for breast and cervical cancers jointly, rather than centering on only one cancer screening at a time, has potential for decreasing cancer health disparities in Southeast Asians.
This study also has limitations. The communities included in this study are medically underserved and may not be familiar with or involved in research. Engaging and retaining participants from these communities may pose challenges. To mitigate this, the CCAB assisted the investigators with the design of research methods and materials, and we incorporated feedback from community stakeholders to ensure cultural relevance and appropriateness. Lastly, the study is conducted in a single site and specifically targets four Southeast Asians; thus, study findings may not be generalizable to other geographic locations or populations.
3.2. Plans for dissemination
Our approach to dissemination of research findings will include engagement with our CCAB to facilitate stakeholder collaboration in dissemination planning and conduct. The products we expect to develop include, but are not limited to, reports of study methods and findings, tools, and resources to facilitate the use of the tailored message library and implementation methods studied in this study, and presentations in both scientific and community settings.
4. Conclusion
In summary, tailored navigation is an innovative research approach to promoting breast and cervical cancer screening and early detection in underserved populations in the U.S. This multi-faceted intervention combines culturally sensitive tailored messaging and navigation from community into health clinics and has high potential for scalability across community settings for medically underserved, immigrant populations.
Funding
This research is supported by the American Cancer Society Research Scholar Grant [RSG-CPHPS 131811, PI: Kue].
CRediT authorship contribution statement
Jennifer Kue: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. Judith Tate: Investigation, Project administration, Supervision, Writing – original draft, Writing – review & editing. Laura A. Szalacha: Conceptualization, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. Usha Menon: Conceptualization, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We acknowledge the contributions of those who have served on the Community Advisory Board including Bounthanh Phommasathit, Vanh Sivixay, Yan Ke, Somany Pich, Kathy Nguyen, and Sophia Vang. We'd also like to thank our partner health clinics including Heart of Ohio Family Health, Lower Lights Christian Health Center, and The Ohio State University Total Health and Wellness Center.
Data availability
Data will be made available on request.
References
- 1.Centers for Disease C, Prevention Asian American Health 2013. http://www.cdc.gov/minorityhealth/populations/REMP/asian.html
- 2.American Cancer Society Cancer Facts & Figures 2016. http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-047079.pdf 2016.
- 3.Gomez S.L., Von Behren J., McKinley M., et al. Breast cancer in Asian Americans in California, 1988-2013: increasing incidence trends and recent data on breast cancer subtypes. Breast Cancer Res. Treat. 2017 doi: 10.1007/s10549-017-4229-1. epub ahead of printdoi:10.100/s10549-017-4229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Cancer S. Guidelines for the early detection of cancer. Accessed Web Page, http://www.cancer.org/acs/groups/content/@editorial/documents/document/acspc-046343.pdf..
- 5.Centers for Disease C, Prevention. Breast Cancer. 2016. [Google Scholar]
- 6.Kelly A.W., Fores Chacori M., Wollan P.C., et al. A program to increase breast and cervical cancer screening for Cambodian women in a midwestern community. Mayo Clin. Proc. May 1996;71(5):437–444. doi: 10.4065/71.5.437. [DOI] [PubMed] [Google Scholar]
- 7.Dang J., Lee J., Tran J.H. Knowledge, attitudes, and beliefs regarding breast and cervical cancer screening among Cambodian, Laotian, Thai, and Tongan women. J. Cancer Educ. Dec 2010;25(4):595–601. doi: 10.1007/s13187-010-0082-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee H.Y., Ju E., Vang P.D., Lundquist M. Breast and cervical cancer screening disparity among Asian American women: does race/ethnicity matter? J. Wom. Health. 2010;19(10):1877–1884. doi: 10.1089/jwh.2009.1783. [doi] [DOI] [PubMed] [Google Scholar]
- 9.Shoemaker M.L., White M.C. 2010, and 2013. Cancer Causes Control. 2016/06/01. 2008. Breast and cervical cancer screening among Asian subgroups in the USA: estimates from the National Health Interview Survey; pp. 825–829. 2016;27(6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McGarvey E.L., Clavet G.J., Johnson J.B., 2nd, Butler A., Cook K.O., Pennino B. Cancer screening practices and attitudes: comparison of low-income women in three ethnic groups. Ethn. Health. Feb 2003;8(1):71–82. doi: 10.1080/13557850303556. [DOI] [PubMed] [Google Scholar]
- 11.Ngoc Nguyen T.U., Tanjasiri S.P., Kagawa-Singer M., Tran J.H., Foo M.A. Community health navigators for breast- and cervical-cancer screening among Cambodian and Laotian women: intervention strategies and relationship-building processes. Health Promot. Pract. 2008;9(4):356–367. doi: 10.1177/1524839906290251. 1524839906290251 [pii] [DOI] [PubMed] [Google Scholar]
- 12.Bird J.A., McPhee S.J., Ha N.T., Le B., Davis T., Jenkins C.N. Opening pathways to cancer screening for Vietnamese-American women: lay health workers hold a key. Prev. Med. Nov-Dec 1998;27(6):821–829. doi: 10.1006/pmed.1998.0365. [DOI] [PubMed] [Google Scholar]
- 13.Taylor V.M., Nguyen T.T., Jackson J.C., McPhee S.J. Cervical cancer control research in Vietnamese American communities. Cancer Epidemiol. Biomarkers Prev. Nov 2008;17(11):2924–2930. doi: 10.1158/1055-9965.EPI-08-0386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen B.H., Stewart S.L., Nguyen T.T., Bui-Tong N., McPhee S.J. Effectiveness of lay health worker outreach in reducing disparities in colorectal cancer screening in Vietnamese Americans. Am. J. Pub. Health. 2015;(10):2083–2089. doi: 10.2105/AJPH.2015.302713. 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ma G.X., Fang C., Tan Y., Feng Z., Ge S., Nguyen C. Increasing cervical cancer screening among Vietnamese Americans: a community-based intervention trial. J. Health Care Poor Underserved. May 2015;26(2 Suppl):36–52. doi: 10.1353/hpu.2015.0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rimer B.K., Kreuter M.W. Advancing tailored health communication: a persuasion and message effects perspective. J. Commun. 2006;56(s1):S184–S201. doi: 10.1111/j.1460-2466.2006.00289.x. [DOI] [Google Scholar]
- 17.Kreuter M.W., Wray R.J. Tailored and targeted health communication: strategies for enhancing information relevance. Am. J. Health Behav. 2003;3(1):S227–S232. doi: 10.5993/ajhb.27.1.s3.6. 27. [DOI] [PubMed] [Google Scholar]
- 18.Kue J., Zukoski A., Keon K.L., Thorburn S. Breast and cervical cancer screening: exploring perceptions and barriers with Hmong women and men in Oregon. Ethn. Health. 2014;19(3):311–327. doi: 10.1080/13557858.2013.776013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma G.X., Toubbeh J.I., Wang M.Q., Shive S.E., Cooper L., Pham A. Factors associated with cervical cancer screening compliance and noncompliance among Chinese, Korean, Vietnamese, and Cambodian women. J. Natl. Med. Assoc. Jun 2009;101(6):541–551. doi: 10.1016/s0027-9684(15)30939-1. Doi 10.1016/S0027-9684(15)30939-1. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen A.B., Belgrave F.Z. Suc Khoe La Quan Trong Hon Sac Dep! Health is better than beauty! A community-based participatory research intervention to improve cancer screening among Vietnamese women. J. Health Care Poor Underserved. May 2014;25(2):605–623. doi: 10.1353/hpu.2014.0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Menon U., Belue R., Wahab S., et al. A randomized trial comparing the effect of two phone-based interventions on colorectal cancer screening adherence. Ann. Behav. Med. Dec 2011;42(3):294–303. doi: 10.1007/s12160-011-9291-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Menon U., Szalacha L.A., Kue J., et al. Effects of a community-to-clinic navigation intervention on colorectal cancer screening among underserved people. Ann Behav Med. 2020;20(5):308–319. doi: 10.1093/abm/kaz049. 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kue J., Thorburn S., Keon K.L. Research challenges and lessons learned from conducting community-based research with the Hmong community. Health Promot. Pract. May 2015;16(3):411–418. doi: 10.1177/1524839914561515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thorburn S., Kue J., Keon K.L., Lo P. Medical mistrust and discrimination in health care: a qualitative study of Hmong women and men. J. Community Health. Aug 2012;37(4):822–829. doi: 10.1007/s10900-011-9516-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heckathorn D.D. Respondent-driven sampling: a new approach to the study of Hidden populations*. Soc. Probl. 1997;44(2):174–199. doi: 10.2307/3096941. [DOI] [Google Scholar]
- 26.Raudenbush S.W. Version 3.01. 2011. Optimal design software for multi-level and longitudinal research. [Google Scholar]
- 27.Nguyen T.T., Le G., Nguyen T., et al. Breast cancer screening among Vietnamese Americans A randomized controlled trial of lay health worker outreach. Am. J. Prev. Med. Oct 2009;37(4):306–313. doi: 10.1016/j.amepre.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nguyen T.T., McPhee S.J., Bui-Tong N., et al. Community-based participatory research increases cervical cancer screening among Vietnamese-Americans. J. Health Care Poor Underserved. May 2006;17(2):31–54. doi: 10.1353/hpu.2006.0091. DOI 10.1353/hpu.2006.0078. [DOI] [PubMed] [Google Scholar]
- 29.Taylor V.M., Jackson J.C., Yasui Y., et al. Evaluation of an outreach intervention to promote cervical cancer screening among Cambodian American women. Cancer Detect. Prev. 2002;26(4):320–327. doi: 10.1016/s0361-090x(02)00055-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Semaan S., Santibanez S., Garfein R.S., Heckathorn D.D., Des Jarlais D.C. Ethical and regulatory considerations in HIV prevention studies employing respondent-driven sampling. Int. J. Drug Pol. Jan 2009;20(1):14–27. doi: 10.1016/j.drugpo.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 31.Baron R.M., Kenny D.A. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. Dec 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 32.MacKinnon D.P., Lockwood C.M., Hoffman J.M., West S.G., Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol. Methods. Mar 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.MacKinnon D.P. In: Multivariate Applications in Substance Ues Research: New Methods for New Questions. Rose J.S., Chassin L., Presson C.C., Sherman S.J., editors. Erlbaum; 2000. Contrasts in multiple mediator models; pp. 83–104. [Google Scholar]
- 34.Cook W.L., Kenny D.A. The actor-partner interdependence model: a model of bidirectional effects in developmental studies. IJBD (Int. J. Behav. Dev.) Mar 2005;29(2):101–109. doi: 10.1080/01650250444000405. [DOI] [Google Scholar]
- 35.Kenny D.A. Models of interdependence in dyadic research. J. Soc. Pers. Relat. 1996;13:279–294. [Google Scholar]
- 36.Gomez S.L., Tan S., Keegan T.H., Clarke C.A. Disparities in mammographic screening for Asian women in California: a cross-sectional analysis to identify meaningful groups for targeted intervention. BMC Cancer. 2007;7:201. doi: 10.1186/1471-2407-7-201. 1471-2407-7-201 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hay J.L., Meischke H.W., Bowen D.J., et al. Anticipating dissemination of cancer genomics in public health: a theoretical approach to psychosocial and behavioral challenges. Ann. Behav. Med. Nov-Dec 2007;34(3):275–286. doi: 10.1007/BF02874552. [DOI] [PubMed] [Google Scholar]
- 38.Hay J., Shuk E., Brady M.S., Berwick M., Ostroff J., Halpern A. Family communication after melanoma diagnosis. Arch. Dermatol. Apr 2008;144(4):553–554. doi: 10.1001/archderm.144.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.