Abstract
Although multiple factors still pose challenges to inpatient/outpatient rehabilitation for survivors of COVID-19, rehabilitation plays a key role for this patient population. This study aimed to improve Physical and Rehabilitation Medicine (PRM) physician’s professional practice for persons with COVID-19-related functioning limitations, to promote functional recovery and reduce activity limitations and/or participation restrictions. A systematic review of the scientific literature was performed from December 2019 to August 2022, followed by production of recommendations through 5 Delphi rounds, by consensus among the delegates of all European countries represented in the Union of European Medical Specialists PRM Section. The systematic literature review is reported together with thirty-two recommendations resulting from the Delphi procedure. The PRM physician’s role for persons with COVID-19-related limitations of functioning is to develop, foster, and monitor the implementation of an individual rehabilitation project tailored to the patient’s age, previous medical and functional status, current comorbidities and complications, activity limitations and participation restrictions and personal and environmental factors. This is done by applying the concept of a multi-specialty integrated service model with multi-professional/interdisciplinary teams, providing care at all stages of COVID-19 illness. This evidence-based position paper represents the official position of the European Union through the UEMS PRM Section.
Key words: COVID-19, Severe acute respiratory syndrome-related coronavirus, Post-Acute COVID-19 syndrome, Physical and rehabilitation medicine, Consensus development conference
SARS-CoV-2 continues to infect several thousands of people daily, leading to preventable morbidity and mortality worldwide. Globally, as of August 16, 2023, there have been 769,774,646 confirmed cases of COVID-19 (275,854,299 confirmed cases in Europe), including 6,955,141 deaths, reported by the World Health Organization (WHO).1 At the outset of the pandemic, the rehabilitation needs for patients recovering from COVID-19 were based on evidence from the critical care population and in the sequelae of COVID-19 in the short- and medium-term.2, 3 In particular, patients suffering from severe COVID-19 and admitted to the intensive care unit (ICU) were at higher risk of developing post-intensive care syndrome (i.e., older persons with underlying diseases such as diabetes, hypertension, increased frailty, and other chronic disorders), which is a range of impairments including physical deconditioning, respiratory, swallow, cognitive, and mental health symptoms.4, 5
So, early rehabilitation became an indispensable part of the multidisciplinary management of critically ill patients.6
However, all hospitalized patients, ICU and non-ICU, reported new illness-related fatigue, breathlessness, post traumatic stress disorder symptoms, pain, voice change, cough, dysphagia, anxiety, depression, and problems with concentration, memory, and continence.7
Moreover, hospitalized patients, particularly those with prolonged stay, are susceptible to pressure injuries given inactivity, use of artificial airways, and prone positioning.8 So, they are at risk of multisystem impairments predisposing them to require acute inpatient rehabilitation, which has been demonstrated to improve functional recovery and safe discharge at home.2, 9, 10
With the progression of the pandemic, the development of vaccines (as of August 15 2023, 13,498,570.620 vaccine doses have been administered),1 new treatments for COVID-19 that have substantially reduced hospitalization, the severity of disease and mortality, and patients’ long-term follow-up, further evidence is emerging about COVID-19 related persistent symptoms. Known by various names, including long COVID or long-haul COVID, and listed in the ICD-10 classification as post COVID-19 condition (PCC) since September 2020,11 its occurrence is variable in terms of expression and impact on daily life.
The WHO defines PCC as the condition occurring in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually three months from the onset, with symptoms that last for at least two months and cannot be explained by an alternative diagnosis. PCC is more common in adults than children, in adult females than adult males, and in those hospitalized than those who were not.12 The empirical findings suggest a PCC global estimated pooled prevalence of approximately 43%.12 Based on a WHO estimate of 770 million worldwide COVID-19 infections, this global pooled PCC estimate indicates that approximately 330 million individuals currently experience or have previously experienced long-term, health-related consequences of COVID-19. Common symptoms include, but are not limited to, fatigue, shortness of breath, and cognitive dysfunction, which generally impact everyday functioning. Symptoms might be new onset following initial recovery from an acute COVID-19 episode or persist from the initial illness. Symptoms might also fluctuate or relapse over time.13 A recent Dutch study acknowledged four subtypes: muscle pain, fatigue, cardiorespiratory, and ageusia/anosmia.14
The pathophysiological mechanisms of post-COVID symptoms are multiple and potentially overlapping, including persisting viral reservoirs, immune dysfunction, microclotting, and end-organ damage.15 Due to the complex nature of this condition, the multi-system impact on functioning, a well-coordinated and organized interdisciplinary/multi-professional team that establishes a rehabilitative multidimensional program is required.16, 17
Physical and Rehabilitation Medicine (PRM) is defined as the medicine of functioning. As such, it represents the primary medical specialty that addresses patients’ health needs by referring to the integrative model of functioning, disability, and health proposed by the WHO and applying rehabilitation as a core health strategy. PRM physicians are adequately trained and qualified to organize and manage the Individual rehabilitation project (IRP) for COVID-19 survivors within a holistic teamwork approach in acute, post-acute, and community settings. The aim of this evidence-based position paper (EBPP) is to improve PRM physician’s professional practice for persons with COVID-19-related limitations of functioning, to promote their functional recovery and reduce activity limitations and/or participation restrictions.
Materials and methods
This paper was developed according to the methodology defined by the Professional Practice Committee of the Union of European Medical Specialists (UEMS) PRM Section and described by Negrini et al.18 It consists of 1) a systematic review of the scientific literature to select papers relevant to the study aim; 2) the development of recommendations grouped in five domains (Table I); c) the progressive selection and refining of recommendations through five Delphi rounds, by consensus among the delegates of all European countries represented in the UEMS PRM Section (Table II).
Table I. —Domains of recommendations listed in the EBPP.
| Domain | Heading and subheadings |
|---|---|
| A | Overall general recommendations |
| B | Recommendations on PRM physician’s role in Medical Diagnosis according to ICD |
| C | Recommendations on PRM physician’s role in PRM diagnosis and assessment according to ICF |
| D | Recommendations on PRM management and process a. Inclusion criteria (e.g., when and why to prescribe PRM interventions) b. Project definition (definition of overall aims and strategies of PRM interventions) c. Teamwork (professionals involved and specific modalities of teamwork) d. PRM interventions e. Outcome criteria f. Length/Duration/Intensity of treatment (overall practical PRM approach) g. Discharge criteria (e.g., when and why to end PRM interventions) h. Follow-up criteria and agenda |
| E | Recommendations on future research of PRM professional practice |
Table II. —Delphi rounds.
| Delphi round | Participants | Timing | Agreement on | Levels |
|---|---|---|---|---|
| 1 | Authors | 14 days | Recommendations | Accept / accept with changes / reject |
| 2 | All delegates | 14 days | Recommendations | Accept / accept with changes / reject |
| 3 | All delegates | 14 days | Recommendations | Accept / reject |
| 4 | Authors | 14 days | Strength of Recommendations | A. It must be normally applied B. It is important but can be applied not in all situations C. Less important, it can be applied on a voluntary basis D. Very low importance |
| 5 | All delegates | 14 days | Final paper with recommendations | Yes / no |
We conducted a comprehensive literature search on September 1st, 2022, covering publication dates between December 1st, 2019, and August 31st, 2022. We searched PubMed, Embase, CINAHL, Scopus, Web of Science, and PEDro for “rehabilitation” and “COVID-19”, adapting search strategies to each database-specific thesaurus and applying the string used by Ceravolo et al.2
Due to the expected poor availability of high-quality research, a comprehensive approach was applied, considering all types of studies in the English language. We selected papers addressing the rehabilitation needs of people 1) with a confirmed diagnosis of COVID-19, in any phase, without age, gender, ethnicity, or care setting restrictions; 2) presenting any limitations of functioning of rehabilitation interest (LFRI); 3) receiving any rehabilitation interventions compared with any other interventions; 4) undergoing any assessment to determine the presence of LFRI and 5) evaluated with any outcome measures.
Eventually, the criterion for including the studies was the professional relevance for PRM physicians as judged by two authors (AF and EA), with the main author (MGC) resolving conflicts.
The grading of the strength of evidence (SoE) and Strength of Recommendations (SoR) was done as described in the original “Methodology paper.”18
Results
Systematic review
The electronic literature search identified 70340 titles. After duplicate removal, 36,327 papers were screened based on titles and abstracts, and those not meeting eligibility criteria were excluded. Of the 615 remaining papers, 514 more were excluded as not relevant to PRM practice based on the full-text content. The remaining 101 articles were considered for the preparation of the recommendations. The selection process is reported in Figure 1. From a former list of 65 recommendations, the consensus procedure ended up with 32 final recommendations, as displayed in Table III. The overall view of the Recommendations, their distribution through the different domains concerning the PRM physician’s role and the grading of evidence, as resulting from the 4th Delphi round, is presented in Table IV.
Figure 1.
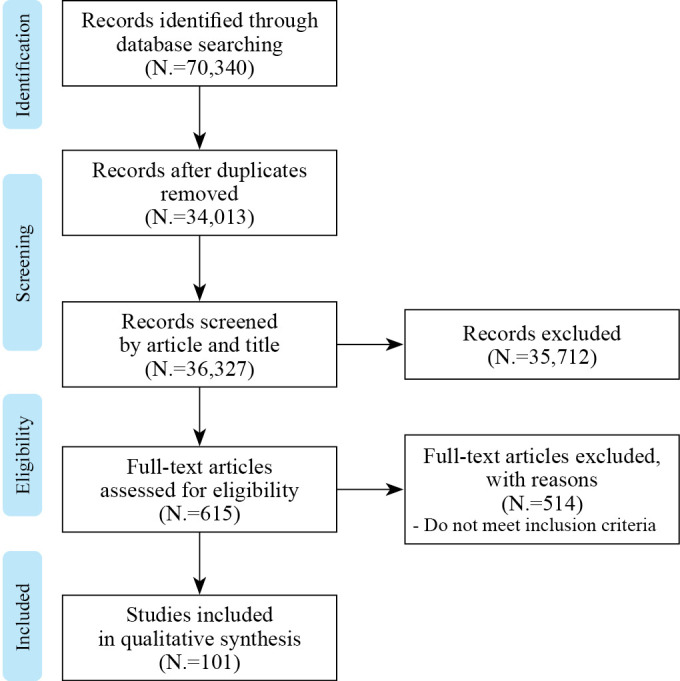
—Flow chart of paper selection.
Table III. —Results of the consensus procedure – recommendation selection.
| Accept | Accept with suggestions | Reject | |||||
|---|---|---|---|---|---|---|---|
| Round | Number of recommendations | Number | % | Number | % | Number | % |
| 1 | 65 | 34 | 52.3 | 29 | 44.6 | 2 | 3.1 |
| 2 | 63 | 8 | 12.7 | 24 | 38.1 | 31 | 49.2 |
| 3 | 32 | 32 | 100.0 | NA | NA | 0 | 0 |
Table IV. —Distribution of recommendations and grading of evidence.
| Domain | N. of recommendations | Strength of recommendations | Strength of evidence | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N. | A | B | C | D | I | II | III | IV | NA | |
| Overall general recommendation | 1 | 100% | 0 | 0 | 0 | 0 | 0 | 0 | 100% | 0 |
| PRM physicians’ role in medical diagnosis according to ICD | 5 | 60% | 40% | 0 | 0 | 0 | 0 | 0 | 80% | 20% |
| PRM physicians’ role in PRM diagnosis and assessment according to ICF | 3 | 100% | 0 | 0 | 0 | 0 | 0 | 0 | 66% | 33% |
| Recommendations on PRM management and process | 22 | 77.2% | 22.7% | 0 | 0 | 4.5% | 13.6% | 0 | 50% | 31.8% |
| Recommendations on future research on PRM professional practice | 1 | 100% | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100% |
| Total | 32 | 68.7% | 31.3% | 0 | 0 | 3.1% | 9.4% | 0 | 53.1% | 34.4% |
The recommendations stated in this EBPP highlight the role of the PRM physician as the leader of the interdisciplinary multi-professional team caring for patients with functional limitations of rehabilitation interest after COVID-19.
Before reporting the recommendations, we describe a few issues emanating from the literature review:
importance of an early provision of tailored rehabilitation care: It is demonstrated that an IRP, starting as early as possible, considering patients’ exercise tolerance, is effective at preventing the vicious cycle of asthenia, respiratory muscle weakness, and progressive respiratory failure of COVID-19 patients admitted to the ICU.19, 20
Relevance of the involvement of the PRM physician in the care pathway dedicated to COVID-19 survivors in any phase of the disease to ensure a thorough assessment of the multiple function impairments following the infection, the prescription of rehabilitation interventions of proper amount and intensity,9 and the evaluation of their effects through the application of disease-related or generic outcome measures.20-24
Need for PRM physicians to schedule regular follow-ups of the patient’s functional status after hospital discharge. The risk for people with COVID-19 to develop a PCC is well-documented, as is the functional relevance of this condition. The PRM physician has specialized competence and skills to provide a comprehensive clinical and functional monitoring of adults with moderate-severe COVID-19 for a minimum of 12 months to tailor rehabilitation interventions for patients with low functional status or post-intensive care syndrome.25-35
Recommendations
Overall general recommendation
1. In managing patients with COVID-19, a PRM physician’s professional responsibilities include developing, facilitating, and supervising an IRP36 customized to the patient’s age, previous medical and functional status, and type and severity of the symptoms. Any IRP should consider the comorbidities that could hinder a patient’s progress or participation, apply the concept of a multi-speciality integrated service model with multiprofessional/interdisciplinary teams and provide individualized care, taking activity limitations and participation restrictions into account at all stages of COVID-19 illness.37, 38 [SoR: A, SoE: IV]
A. Recommendations on PRM physicians’ role in Medical Diagnosis according to ICD
2. It is recommended that the PRM physician acquires knowledge of medical diagnosis and management of individuals with COVID-19 in acute settings. [SoR: B, SoE:NA]
3. It is recommended that the PRM physician working in rehabilitation settings has the skills and knowledge to promptly diagnose COVID-19 in their patients receiving rehabilitation for other conditions through constant surveillance.39 [SoR: A, SoE: IV]
4. It is recommended that the PRM physician has the knowledge and skills to identify and make the preliminary diagnosis of all the medical complications of COVID-19 in an acute hospital and community setting, and provide the proper diagnosis of PCC.40, 41 [SoR: A, SoE: IV]
5. It is recommended that the PRM physician has specific expertise in undertaking prompt baseline investigations and ruling out life-threatening conditions in patients with PCC.37, 39 [SoR: B, SoE: IV]
6. It is recommended that the PRM physician joins the community care programmes for PCC patients and is involved in a closer follow-up for these patients to suspect, diagnose and manage any body function (e.g. either mental, sensory, autonomic or neuromuscular and movement-related) impairment or delayed return to vocational activity arising from PCC.42 [SoR: A, SoE: IV]
B. Recommendations on PRM physicians’ role in PRM diagnosis and assessment according to ICF
7. It is recommended that the PRM physician ensures adequate activities and interventions in the acute setting to prevent complications during the acute phase of COVID-19 by supporting/leading the existing acute interdisciplinary/multi-professional team caring for the patients.43, 44 [SoR: A, SoE: IV]
8. It is recommended that the PRM physician participates in a full functional assessment, which includes activities and participation while paying close attention to whether or not PCC patients have particular impairments. [SoR: A, SoE: NA]
9. It is recommended that the PRM physician uses the International Classification of Functioning, Disability, and Health (ICF) framework developed by the WHO to measure the effects of PCC on patients’ physical, cognitive, emotional, and general well-being.45, 46 [SoR: A, SoE: IV]
C. Recommendations on PRM management and process
a. Inclusion criteria (e.g., when and why to prescribe PRM interventions)
10. It is recommended that the PRM physician develops and implements the IRP and interventions for patients with COVID-19 who are admitted to the acute wards and for patients with debilitating sequelae of COVID-19 who are admitted to the acute rehabilitation settings.43 [SoR: A, SoE: NA]
11. It is recommended that the PRM physician, following a comprehensive assessment, prescribes and implements a tailored inpatient, outpatient or community-based IRP by leading and coordinating the multi-professional team for patients with PCC presenting with activity limitations and/or participation restrictions. [SoR: A, SoE: NA]
12. It is recommended that the PRM physician re-evaluates the symptoms in patients with PCC and modifies the rehabilitation treatment in patients with a progression of symptoms causing functional impairments, activity limitations or participation restrictions. [SoR: A, SoE:NA]
b. Project definition (definition of the overall aims and strategy of PRM interventions)
13. It is recommended that the PRM physician in the acute setting creates capacity to meet the increasing COVID-19 demand, develops pathways and supports early discharge from the acute care units into a rehabilitation setting as well as safe discharge from the inpatient rehabilitation environment to the outpatient and community environment.43 [SoR: B, SoE: NA]
14. It is recommended that the PRM physician establishes a multi-specialty integrated service model for the care of PCC patients (including specialties such as internal medicine, pulmonology, cardiology, neurology, and neuropsychiatry) in inpatient and outpatient settings.37, 47-52 [SoR: A, SoE:IV]
15. It is recommended that the PRM physician, within the multi-specialty integrated service model, specifies the aims and procedures for rehabilitation intervention to provide holistic, long-term care with monitoring of rehabilitation interventions and evaluating outcome measures of PCC patients.37, 52 [SoR: A, SoE: IV]
16. It is recommended that the PRM physician consider using self-management tools such as leaflets, information videos, workshops, lectures and webinars to promote positive physical and mental well-being in patients with PCC.52-57 [SoR: B, SoE: IV]
17. It is recommended that the PRM physician is aware of and adheres to existing recommendations and guidelines while making evidence-based decisions on healthcare interventions for individuals with PCC. [SoR: A, SoE: NA]
c. Teamwork (professionals involved and specific modalities of teamwork)
18. It is recommended that the rehabilitation needs of PCC patients be met by a well-coordinated and organised interdisciplinary/multi-professional team composed of a PRM physician and other pertinent medical professionals (pulmonologists, cardiologists, neurologists, internal medicine physicians, neuropsychiatrists, and primary care physicians). The multi-professional team should include rehabilitation and other relevant health professionals such as physiotherapists, occupational therapists, nurses, clinical (neuro)psychologists, dieticians, speech and language therapists, and social workers to manage patients with PCC. This can be offered at any level of care or setting (including acute care, specialised post-acute care, and community-based services).17, 47-49 [SoR: A, SoE: IV]
d. PRM interventions
19. It is recommended that the PRM physician, together with the multi-professional team, have adequate theoretical knowledge, clinical skills, and therapeutic equipment for clinical and functional assessment to provide a base for planning and early performing a patient-tailored rehabilitation intervention through all stages of COVID-19.58-62 [SoR: A, SoE: IV]
20. It is recommended that the PRM physician provides Individual rehabilitation projects for COVID-19 patients, starting as early as possible, considering exercise tolerance, with the aim of preventing the vicious cycle of asthenia, respiratory muscle weakness and progressive respiratory failure.19 [SoR: A; SoE: II]
21. It is recommended that the PRM physician knows the indications and develops appropriate knowledge and skills to prescribe, when appropriate, rehabilitation interventions relevant to the different phases of COVID-19 and assesses their effects through the application of disease-related (when available) or generic outcome measures. More in detail, the PRM physician should take care that patients admitted to hospital in the acute COVID-19 phase receive, when appropriate:
a. inspiratory muscle training20-23 also in combination with group psychological interventions.24 [SoR: A; SoE: II]
b. Nutritional assessment and malnutrition screening.63-66 [SoR: A; SoE: IV]
c. Swallowing assessment for detecting dysphagia following invasive ventilation and proper swallowing training to promote the recovery of safe oral feeding.67-70 [SoR: A; SoE: IV]
d. Nonpharmacological therapy (such as meditation) and breathing exercises to manage depression, anxiety, and quality of sleep.71 [SoR: B; SoE: II]
e. Self-care breathing exercises to improve respiratory symptoms.72, 73 [SoR:A; SoE:I]
f. Tailored telerehabilitation programs focused on aerobic, resistance, and respiratory muscle training.51, 63, 74-77 [SoR: A; SoE: I]
22. It is recommended that the PRM physician prescribes telerehabilitation programs for persons with COVID-19, not only in the outpatient but also in the inpatient setting, to maximize rehabilitation professionals’ safety while ensuring healthcare delivery.77 [SoR: B; SoE: IV]
23. It is recommended that the PRM physician takes care that patients with PCC receive, when appropriate:
a. respiratory rehabilitation comprehensive of respiratory muscle training, cough exercises, diaphragmatic training, stretching and home exercises to improve respiratory function, quality of life, and anxiety.78 [SoR: A; SoE: II]
b. A combination of pain education, skills training on energy conservation techniques for the management of fatigue, tailored physical exercise training, psychological support for the management of anxiety and depression, olfactory training for the management of olfactory impairment, goal-oriented skills training for the management of swallowing and voice impairment.79-87 [SoR: A; SoE: III]
e. Outcome criteria
24. It is recommended that the PRM physician performs a thorough assessment of pulmonary function, endurance,17, 74, 76, 78, 88-91 functioning and disability,41, 92-94 quality of life, mood, and sleep using standardized assessment tools with adequate psychometric and diagnostic properties for persons with COVID-19.74, 88-91, 95, 96 [SoR: A; SoE: I]
f. Length/duration/intensity of treatment (overall practical PRM approach)
25. It is recommended that the PRM physician adapts treatment/decisions/strategies/schedules to the individual needs of the person with COVID-19 and shares any decision on the length, duration, and intensity of specific treatment with the rehabilitation team members, patient, and family. [SoR: A; SoE: NA]
26. It is recommended that the PRM physician carefully plans the amount and intensity of rehabilitation in the COVID-19 acute phase, keeping in mind that the greater the frequency and duration of intervention, the higher the mobility improvement at hospital discharge and the probability of discharge home.9 [SoR: B; SoE: IV]
More in detail, the PRM physician should take care that patients admitted to hospital in the acute COVID-19 phase receive, when appropriate:
a. Up to 3 speech and language therapy sessions to recover safe swallowing patterns in case of dysphagia following orotracheal intubation.68, 70 [SoR: B; SoE: IV]
b. Moderate-intensity aerobic exercise to decrease the severity and progression of COVID-19-associated disorders and improve quality of life in young and middle-aged persons with mild or moderate ongoing COVID-19.97 [SoR: B; SoE: II]
c. Multimodal inpatient cardiopulmonary rehabilitation intervention (i.e., 25-30 min/session, 5-6 sessions/week for 2-4 weeks) for patients with ongoing severe COVID-19.98 [SoR: B; SoE: IV]
d. Supervised high-intensity interval training (HIIT), with any of the most widely used HIIT protocols (4×4, 6×1, or 10-20-30), for patients recently hospitalized with severe COVID-19 infection and recovering from acute phase.99[ SoR: B; SoE: II]
e. Low-intensity aerobic training exercises (i.e. 30 minutes/sessions, one session/day, four days/week for eight weeks, 40%-60% of maximum heart rate) for older persons with PCC sarcopenia.100 [SoR: B; SoE: II]
f. Rehabilitation treatment, including pulmonary, aerobic and resistance training (3 sessions/week for 6-8 weeks) for persons with PCC.101, 102 [SoR: B; SoE: IV]
27. It is recommended that the PRM physician prescribes exercise protocols comprehensive of a home program to maintain the physical functional performance of patients with COVID-19 throughout the hospital stay and after discharge.103 [SoR: B; SoE: IV]
g. Discharge criteria (e.g., when and why to end PRM interventions)
28. It is recommended that a person with COVID-19 concludes the rehabilitation program after reaching the long-term goals set at the beginning, or during the (program can be modified) rehabilitation program or when there has not been any further progress in his/her functional capacity for the defined time period, or when he or she is not able to participate in the rehabilitation program due to deterioration in his/her health or the onset of a significant co-morbidity. [SoR: A; SoE: NA]
h. Follow-up criteria and agenda
29. It is recommended that the PRM physician tailors the follow-up of persons with COVID-19 based on their individual clinical and functional needs.25, 104 [SoR: A; SoE: IV]
30. It is recommended that the PRM physician provides a comprehensive clinical and functional monitoring of adults with moderate-severe COVID-19 for a minimum of 12 months to develop specific rehabilitation strategies for patients who exhibit a low functional status and pre-admission frailty, comorbidity, female gender, advanced age, active smoking, severe infection at onset, PaO2/FiO2 ratio <324, BMI ≥33 Kg/m2 at admission to the emergency department, or post-intensive care syndrome.25-35 [SoR: A; SoE: IV]
31. It is recommended that the PRM physician provides a comprehensive clinical and functional monitoring of children with moderate-severe COVID-19 for a minimum of three months, in particular for those of older age with a history of muscle pain at onset and admission to the ICU.35, 105, 106 [SoR: A; SoE: IV]
D. Recommendations on future research about best PRM professional practice
32. It is recommended that the PRM physician participates in research on PRM professional practice, which is focused on the effective and comprehensive rehabilitation of limitations of functioning caused by COVID-19, contributing to understanding the functional impact of the new variants of COVID-19 in the long-term, weigh risk factors for persisting LFRI after COVID-19 and ascertain the impact of the PCC on work abilities. [SoR: A; SoE: NA]
Conclusions
The professional role of the PRM physician requires specific expertise in the assessment of the limitations of functioning of patients with COVID-19, at any stage after the infection, to plan, lead and monitor the rehabilitation process in a multi-professional setting through an interdisciplinary approach. PRM physicians should be involved in the care process dedicated to people with COVID-19 as early as possible, addressing the patients’ rehabilitation needs from the acute to the post-acute phase, in any setting, including the screening and assessment of post-COVID conditions, to plan the IRP and supervise its delivery in the continuum of care. Moreover, the PRM physician should work on the implementation and, where existing, improvement of specialized rehabilitation services dedicated to people with limitations of functioning due to COVID-19 or post-COVID conditions.
This EBPP, approved unanimously by the delegates of the UEMS PRM Section at the end of the Consensus procedure (Delphi Round 5), represents the official position of the Section and describes the professional role of PRM physicians in people with COVID-19.
Acknowledgements
The authors wish to acknowledge the members of the UEMS PRM Section Professional Practice Committee and other PRM delegates/experts involved in the Delphi procedure for their valuable comments on this paper: A. Heyns (Belgium), J-F Kaux (Belgium), LV Schnurrer (Croatia), F Boyer (France), I. MacFarlane (Ireland), I Treger (Israel), S. Negrini (Italy), I. Irgens (Norway) E. Vikane (Norway), P Tederko (Poland), V. Golyk (Ukraine).
Footnotes
Conflicts of interest: The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
References
- 1.WHO. World health statistics 2021 [Internet]. Available from https://www.who.int/data/gho/publications/world-health-statistics [cited 2023, Aug 23].
- 2.Ceravolo MG, Arienti C, de Sire A, Andrenelli E, Negrini F, Lazzarini SG, et al. ; International Multiprofessional Steering Committee of Cochrane Rehabilitation REH-COVER action. Rehabilitation and COVID-19: the Cochrane Rehabilitation 2020 rapid living systematic review. Eur J Phys Rehabil Med 2020;56:642–51. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32705860&dopt=Abstract 10.23736/S1973-9087.20.06501-6 [DOI] [PubMed] [Google Scholar]
- 3.de Sire A, Andrenelli E, Negrini F, Patrini M, Lazzarini SG, Ceravolo MG, International Multiprofessional Steering Committee of Cochrane Rehabilitation REH-COVER Action . Rehabilitation and COVID-19: a rapid living systematic review by Cochrane Rehabilitation Field updated as of December 31st, 2020 and synthesis of the scientific literature of 2020. Eur J Phys Rehabil Med 2021;57:181–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33599442&dopt=Abstract 10.23736/S1973-9087.21.06870-2 [DOI] [PubMed] [Google Scholar]
- 4.Biehl M, Sese D. Post-intensive care syndrome and COVID-19 - Implications post pandemic. Cleve Clin J Med 2020. [Epub ahead of print]. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32759175&dopt=Abstract 10.3949/ccjm.87a.ccc055 [DOI] [PubMed]
- 5.Jaffri A, Jaffri UA. Post-Intensive care syndrome and COVID-19: crisis after a crisis? Heart Lung 2020;49:883–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32690219&dopt=Abstract 10.1016/j.hrtlng.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu P, Wei Q, He C. Early Rehabilitation for Critically Ill Patients With COVID-19: More Benefits Than Risks. Am J Phys Med Rehabil 2020;99:468–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32437114&dopt=Abstract 10.1097/PHM.0000000000001445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maltser S, Trovato E, Fusco HN, Sison CP, Ambrose AF, Herrera J, et al. Challenges and lessons learned for acute inpatient rehabilitation of persons with COVID-19: clinical presentation, assessment, needs, and services utilization. Am J Phys Med Rehabil 2021;100:1115–23. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34793372&dopt=Abstract 10.1097/PHM.0000000000001887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malik GR, Wolfe AR, Soriano R, Rydberg L, Wolfe LF, Deshmukh S, et al. Injury-prone: peripheral nerve injuries associated with prone positioning for COVID-19-related acute respiratory distress syndrome. Br J Anaesth 2020;125:e478–80. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32948295&dopt=Abstract 10.1016/j.bja.2020.08.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson JK, Lapin B, Green K, Stilphen M. Frequency of Physical Therapist Intervention Is Associated With Mobility Status and Disposition at Hospital Discharge for Patients With COVID-19. Phys Ther 2021;101:181. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32986836&dopt=Abstract 10.1093/ptj/pzaa181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Puchner B, Sahanic S, Kirchmair R, Pizzini A, Sonnweber B, Wöll E, et al. Beneficial effects of multi-disciplinary rehabilitation in postacute COVID-19: an observational cohort study. Eur J Phys Rehabil Med 2021;57:189–98. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33448756&dopt=Abstract 10.23736/S1973-9087.21.06549-7 [DOI] [PubMed] [Google Scholar]
- 11.Emergency use ICD codes for COVID-19 disease outbreak [Internet]. Available from: https://www.who.int/standards/classifications/classification-of-diseases/emergency-use-icd-codes-for-covid-19-disease-outbreak [cited 2023 August 23].
- 12.Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global Prevalence of Post-Coronavirus Disease 2019 (COVID-19) Condition or Long COVID: A Meta-Analysis and Systematic Review. J Infect Dis 2022;226:1593–607. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35429399&dopt=Abstract 10.1093/infdis/jiac136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV. WHO Clinical Case Definition Working Group on Post-COVID-19 Condition. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis 2022;22:102–7. 10.1016/S1473-3099(21)00703-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Zon SK, Ballering AV, Brouwer S, Rosmalen JG; Lifelines Corona Research Initiative. Symptom profiles and their risk factors in patients with post-COVID-19 condition: a Dutch longitudinal cohort study. Eur J Public Health 2023;ckad152. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=37608757&dopt=Abstract 10.1093/eurpub/ckad152 [DOI] [PMC free article] [PubMed]
- 15.Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol 2023;21:133–46. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=36639608&dopt=Abstract 10.1038/s41579-022-00846-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO. World health statistics [Internet]. Available from https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2023.2 [cited 2023, Nov 15].
- 17.Mayer KP, Parry SM, Kalema AG, Joshi RR, Soper MK, Steele AK, et al. Safety and Feasibility of an Interdisciplinary Treatment Approach to Optimise Recovery From Critical Coronavirus Disease 2019. Critical Care Explor 2021;3:0516. [DOI] [PMC free article] [PubMed]
- 18.Negrini S, Kiekens C, Zampolini M, Wever D, Varela Donoso E, Christodoulou N. Methodology of “Physical and Rehabilitation Medicine practice, Evidence Based Position Papers: the European position” produced by the UEMS-PRM Section. Eur J Phys Rehabil Med 2016;52:134–41. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26681647&dopt=Abstract [PubMed] [Google Scholar]
- 19.Lyadov KV, Koneva ES, Polushkin VG, Sultanov EY, Lukashin MA. Randomised controlled study on pulmonary rehabilitation in COVID-19 patients with pneumonia. Pulmonologiya. 2020;30:569–76. 10.18093/0869-0189-2020-30-5-569-576 [DOI]
- 20.Beom J, Jung J, Hwang IC, Cho YJ, Kim ES, Kim HB, et al. Early rehabilitation in a critically ill inpatient with COVID-19. Eur J Phys Rehabil Med 2020;56:858–61. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33000931&dopt=Abstract 10.23736/S1973-9087.20.06406-0 [DOI] [PubMed] [Google Scholar]
- 21.McWilliams D, Weblin J, Hodson J, Veenith T, Whitehouse T, Snelson C. Rehabilitation Levels in Patients with COVID-19 Admitted to Intensive Care Requiring Invasive Ventilation. An Observational Study. Ann Am Thorac Soc 2021;18:122–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32915072&dopt=Abstract 10.1513/AnnalsATS.202005-560OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abodonya AM, Abdelbasset WK, Awad EA, Elalfy IE, Salem HA, Elsayed SH. Inspiratory muscle training for recovered COVID-19 patients after weaning from mechanical ventilation: A pilot control clinical study. Medicine (Baltimore) 2021;100:e25339. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33787632&dopt=Abstract 10.1097/MD.0000000000025339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jimeno-Almazán A, Buendía-Romero Á, Martínez-Cava A, Franco-López F, Sánchez-Alcaraz BJ, Courel-Ibáñez J, Pallarés JG. Effects of a concurrent training, respiratory muscle exercise, and self-management recommendations on recovery from post-COVID-19 conditions: the RECOVE trial. J Appl Physiol (1985) 2023;134:95–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu Y, Yang YQ, Liu Y, Pei SL, Yang HH, Wu JJ, et al. Effects of group psychological intervention combined with pulmonary rehabilitation exercises on anxiety and sleep disorders in patients with mild coronavirus disease 2019 (COVID-19) infections in a Fangcang hospital. Psychol Health Med 2022;27:333–42. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33877926&dopt=Abstract 10.1080/13548506.2021.1916956 [DOI] [PubMed] [Google Scholar]
- 25.Vilches-Moraga A, Price A, Braude P, Pearce L, Short R, Verduri A, et al. ; COPE Study. Increased care at discharge from COVID-19: the association between pre-admission frailty and increased care needs after hospital discharge; a multicentre European observational cohort study. BMC Med 2020;18:408. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33334341&dopt=Abstract 10.1186/s12916-020-01856-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Lorenzo R, Conte C, Lanzani C, Benedetti F, Roveri L, Mazza MG, et al. Residual clinical damage after COVID-19: A retrospective and prospective observational cohort study. PLoS One 2020;15:e0239570. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33052920&dopt=Abstract 10.1371/journal.pone.0239570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bowles KH, McDonald M, Barrón Y, Kennedy E, O’Connor M, Mikkelsen M. Surviving COVID-19 After Hospital Discharge: Symptom, Functional, and Adverse Outcomes of Home Health Recipients. Ann Intern Med 2021;174:316–25. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33226861&dopt=Abstract 10.7326/M20-5206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roberts P, Wertheimer J, Park E, Nuño M, Riggs R. Identification of Functional Limitations and Discharge Destination in Patients With COVID-19. Arch Phys Med Rehabil 2021;102:351–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33278363&dopt=Abstract 10.1016/j.apmr.2020.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hall J, Myall K, Lam JL, Mason T, Mukherjee B, West A, et al. Identifying patients at risk of post-discharge complications related to COVID-19 infection. Thorax 2021;76:408–11. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33542090&dopt=Abstract 10.1136/thoraxjnl-2020-215861 [DOI] [PubMed] [Google Scholar]
- 30.Hossain MI, Parvin S, Islam MS, Alam MJ, Podder S, Datta R, et al. Demographic profile and outcome of patients admitted to a COVID dedicated hospital in Bangladesh during the second wave. Medicine (Baltimore) 2021;100:e27281. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34664887&dopt=Abstract 10.1097/MD.0000000000027281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao Y, Yang C, An X, Xiong Y, Shang Y, He J, et al. Follow-up study on COVID-19 survivors one year after discharge from hospital. Int J Infect Dis 2021;112:173–82. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34520845&dopt=Abstract 10.1016/j.ijid.2021.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bai F, Tomasoni D, Falcinella C, Barbanotti D, Castoldi R, Mulè G, et al. Female gender is associated with long COVID syndrome: a prospective cohort study. Clin Microbiol Infect 2022;28:611.e9–16. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34763058&dopt=Abstract 10.1016/j.cmi.2021.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rubeshkumar P, John A, Narnaware M, M J, Vidya F, Gurunathan R, et al. Persistent Post COVID-19 Symptoms and Functional Status after 12-14 weeks of recovery, Tamil Nadu, India, 2021. J Infect 2022;84:722–46. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34953913&dopt=Abstract 10.1016/j.jinf.2021.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rapin A, Boyer FC, Mourvillier B, Giordano Orsini G, Launois C, Taiar R, et al. Post-Intensive Care Syndrome Prevalence Six Months after Critical Covid-19: Comparison between First and Second Waves. J Rehabil Med 2022;54:jrm00339. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=36193697&dopt=Abstract 10.2340/jrm.v54.4363 [DOI] [PMC free article] [PubMed]
- 35.Asadi-Pooya AA, Nemati H, Shahisavandi M, Akbari A, Emami A, Lotfi M, et al. Long COVID in children and adolescents. World J Pediatr 2021;17:495–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34478045&dopt=Abstract 10.1007/s12519-021-00457-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zampolini M, Selb M, Boldrini P, Branco CA, Golyk V, Hu X, et al. UEMS-PRM Section and Board . The Individual Rehabilitation Project as the core of person-centered rehabilitation: the Physical and Rehabilitation Medicine Section and Board of the European Union of Medical Specialists Framework for Rehabilitation in Europe. Eur J Phys Rehabil Med 2022;58:503–10. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35148044&dopt=Abstract 10.23736/S1973-9087.22.07402-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barker-Davies RM, O’Sullivan O, Senaratne KP, Baker P, Cranley M, Dharm-Datta S, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Brit J Sport Med 2020;83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kluge HHP, Muscat NA. Call for action: Health services in the European region must adopt integrated care models to manage Post-Covid-19 Conditions. Lancet Regional Heal - Europe 2022;18:100435. [DOI] [PMC free article] [PubMed]
- 39.Pattanakuhar S, Tangvinit C, Kovindha A. A Patient With Acute Cervical Cord Injury and COVID-19: A First Case Report. Am J Phys Med Rehabil 2020;99:674–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32487972&dopt=Abstract 10.1097/PHM.0000000000001485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barker-Davies RM, O’Sullivan O, Senaratne K, Baker P, Cranley M, Dharm-Datta S, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation [Internet]. Available from https://www.bsrm.org.uk/publications/latest-news/post/39-covid-19-bsrm-position-on-rehabilitation [cited 2023, Nov 15]. [DOI] [PMC free article] [PubMed]
- 41.O’Connor RJ, Preston N, Parkin A, Makower S, Ross D, Gee J, et al. The COVID-19 Yorkshire Rehabilitation Scale (C19-YRS): application and psychometric analysis in a post-COVID-19 syndrome cohort. J Med Virol 2022;94:1027–34. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34676578&dopt=Abstract 10.1002/jmv.27415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Demeco A, Marotta N, Barletta M, Pino I, Marinaro C, Petraroli A, et al. Rehabilitation of patients post-COVID-19 infection: a literature review. J Int Med Res 2020;48:300060520948382. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32840156&dopt=Abstract 10.1177/0300060520948382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boldrini P, Bernetti A, Fiore P, SIMFER Executive Committee, SIMFER Committee for International Affairs . Impact of COVID-19 outbreak on rehabilitation services and Physical and Rehabilitation Medicine physicians’ activities in Italy. An official document of the Italian PRM Society (SIMFER). Eur J Phys Rehabil Med 2020;56:316–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32175719&dopt=Abstract 10.23736/S1973-9087.20.06256-5 [DOI] [PubMed] [Google Scholar]
- 44.Ceravolo MG, de Sire A, Andrenelli E, Negrini F, Negrini S. Systematic rapid “living” review on rehabilitation needs due to COVID-19: update to March 31st, 2020. Eur J Phys Rehabil Med 2020;56:347–53. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32316718&dopt=Abstract 10.23736/S1973-9087.20.06329-7 [DOI] [PubMed] [Google Scholar]
- 45.Patel K, Straudi S, Yee Sien N, Fayed N, Melvin JL, Sivan M. Applying the WHO ICF Framework to the Outcome Measures Used in the Evaluation of Long-Term Clinical Outcomes in Coronavirus Outbreaks. Int J Environ Res Public Health 2020;17:6476. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32899534&dopt=Abstract 10.3390/ijerph17186476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Crivelli L, Palmer K, Calandri I, Guekht A, Beghi E, Carroll W, et al. Changes in cognitive functioning after COVID-19: A systematic review and meta-analysis. Alzheimers Dement 2022;18:1047–66. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35297561&dopt=Abstract 10.1002/alz.12644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ahmad M, Kim K, Indorato D, Petrenko I, Diaz K, Rotatori F, et al. Post-COVID Care Center to Address Rehabilitation Needs in COVID-19 Survivors: A Model of Care. Am J Med Qual 2022;37:266–71. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34369895&dopt=Abstract 10.1097/JMQ.0000000000000014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brigham E, O’Toole J, Kim SY, Friedman M, Daly L, Kaplin A, et al. The Johns Hopkins Post-Acute COVID-19 Team (PACT): A Multidisciplinary, Collaborative, Ambulatory Framework Supporting COVID-19 Survivors. Am J Med 2021;134:462–467.e1. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33444589&dopt=Abstract 10.1016/j.amjmed.2020.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Verduzco-Gutierrez M, Estores IM, Graf MJ, Barshikar S, Cabrera JA, Chang LE, et al. Models of Care for Postacute COVID-19 Clinics: Experiences and a Practical Framework for Outpatient Physiatry Settings. Am J Phys Med Rehabil 2021;100:1133–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34793373&dopt=Abstract 10.1097/PHM.0000000000001892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dundumalla S, Barshikar S, Niehaus WN, Ambrose AF, Kim SY, Abramoff BA. A survey of dedicated PASC clinics: Characteristics, barriers and spirit of collaboration. PM R 2022;14:348–56. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35038230&dopt=Abstract 10.1002/pmrj.12766 [DOI] [PubMed] [Google Scholar]
- 51.Gutenbrunner C, Nugraha B, Martin LT. Phase-Adapted Rehabilitation for Acute Coronavirus Disease-19 Patients and Patient With Long-term Sequelae of Coronavirus Disease-19. Am J Phys Med Rehabil 2021;100:533–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33901039&dopt=Abstract 10.1097/PHM.0000000000001762 [DOI] [PubMed] [Google Scholar]
- 52.Sivan M, Halpin S, Hollingworth L, Snook N, Hickman K, Clifton IJ. Development of an integrated rehabilitation pathway for individuals recovering from COVID-19 in the community. J Rehabil Med 2020;52:jrm00089. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32830284&dopt=Abstract 10.2340/16501977-2727 [DOI] [PubMed]
- 53.Ladds E, Rushforth A, Wieringa S, Taylor S, Rayner C, Husain L, et al. Developing services for long COVID: lessons from a study of wounded healers. Clin Med (Lond) 2021;21:59–65. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33479069&dopt=Abstract 10.7861/clinmed.2020-0962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sisó-Almirall A, Brito-Zerón P, Conangla Ferrín L, Kostov B, Moragas Moreno A, Mestres J, et al. On Behalf Of The CAMFiC Long Covid-Study Group . Long Covid-19: Proposed Primary Care Clinical Guidelines for Diagnosis and Disease Management. Int J Environ Res Public Health 2021;18:4350. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33923972&dopt=Abstract 10.3390/ijerph18084350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sivan M, Taylor S. NICE guideline on long covid. BMJ 2020;371:m4938. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33361141&dopt=Abstract 10.1136/bmj.m4938 [DOI] [PubMed] [Google Scholar]
- 56.Heightman M, Prashar J, Hillman TE, Marks M, Livingston R, Ridsdale HA, et al. Post-COVID-19 assessment in a specialist clinical service: a 12-month, single-centre, prospective study in 1325 individuals. BMJ Open Respir Res 2021;8:001041. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34764200&dopt=Abstract 10.1136/bmjresp-2021-001041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Parkin A, Davison J, Tarrant R, Ross D, Halpin S, Simms A, et al. A Multidisciplinary NHS COVID-19 Service to Manage Post-COVID-19 Syndrome in the Community. J Prim Care Community Health 2021;12:21501327211010994. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33880955&dopt=Abstract 10.1177/21501327211010994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Iannaccone S, Alemanno F, Houdayer E, Brugliera L, Castellazzi P, Cianflone D, et al. COVID-19 rehabilitation units are twice as expensive as regular rehabilitation units. J Rehabil Med 2020;52:jrm00073. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32516421&dopt=Abstract 10.2340/16501977-2704 [DOI] [PubMed]
- 59.Simonelli C, Paneroni M, Fokom AG, Saleri M, Speltoni I, Favero I, et al. How the COVID-19 infection tsunami revolutionized the work of respiratory physiotherapists: an experience from Northern Italy. Monaldi Arch Chest Dis 2020;90:90. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32431134&dopt=Abstract 10.4081/monaldi.2020.1085 [DOI] [PubMed] [Google Scholar]
- 60.Brika M, Bossu M, Fautrelle L, Mourey F, Kubicki A. Geriatric Rehabilitation and COVID-19: a Case Report. SN Compr Clin Med 2020;2:2890–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33195995&dopt=Abstract 10.1007/s42399-020-00613-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ferraro F, Calafiore D, Dambruoso F, Guidarini S, de Sire A. COVID-19 related fatigue: which role for rehabilitation in post-COVID-19 patients? A case series. J Med Virol 2021;93:1896–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33295637&dopt=Abstract 10.1002/jmv.26717 [DOI] [PubMed] [Google Scholar]
- 62.Livingston T, Sullivan EK, Wilske G, Gustavson AM. Innovative Care Delivery of Acute Rehabilitation for Patients With COVID-19: A Case Report. Phys Ther 2021;101:204. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33313701&dopt=Abstract 10.1093/ptj/pzaa204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brugliera L, Spina A, Castellazzi P, Cimino P, Arcuri P, Negro A, et al. Nutritional management of COVID-19 patients in a rehabilitation unit. Eur J Clin Nutr 2020;74:860–3. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32433599&dopt=Abstract 10.1038/s41430-020-0664-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hoyois A, Ballarin A, Thomas J, Lheureux O, Preiser JC, Coppens E, et al. Nutrition evaluation and management of critically ill patients with COVID-19 during post-intensive care rehabilitation. JPEN J Parenter Enteral Nutr 2021;45:1153–63. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33666263&dopt=Abstract 10.1002/jpen.2101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pironi L, Sasdelli AS, Ravaioli F, Baracco B, Battaiola C, Bocedi G, et al. Malnutrition and nutritional therapy in patients with SARS-CoV-2 disease. Clin Nutr 2021;40:1330–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32900518&dopt=Abstract 10.1016/j.clnu.2020.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Martin-Martinez A, Ortega O, Viñas P, Arreola V, Nascimento W, Costa A, et al. COVID-19 is associated with oropharyngeal dysphagia and malnutrition in hospitalised patients during the spring 2020 wave of the pandemic. Clin Nutr 2022;41:2996–3006. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34187698&dopt=Abstract 10.1016/j.clnu.2021.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Clayton NA, Walker E, Freeman-Sanderson A. Clinical profile and recovery pattern of dysphagia in the COVID-19 patient: A prospective observational cohort within NSW. Aust Crit Care 2023;36:262–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35177342&dopt=Abstract 10.1016/j.aucc.2022.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lima MS, Sassi FC, Medeiros GC, Ritto AP, Andrade CR. Preliminary results of a clinical study to evaluate the performance and safety of swallowing in critical patients with COVID-19. Clinics (São Paulo) 2020;75:e2021. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32555948&dopt=Abstract 10.6061/clinics/2020/e2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lindh MG, Mattsson G, Koyi H, Johansson MB, Razmi R, Palm A. Swallowing Function in COVID-19 Patients After Invasive Mechanical Ventilation. Arch Rehabil Res Clin Transl 2022;4:100177. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35036903&dopt=Abstract 10.1016/j.arrct.2021.100177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lima MS, Sassi FC, Medeiros GC, Ritto AP, Andrade CR. Functional development of swallowing in ICU patients with COVID-19. CoDAS 2020;32:e20200222. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33053075&dopt=Abstract 10.1590/2317-1782/20192020222 [DOI] [PubMed] [Google Scholar]
- 71.Mahendru K, Pandit A, Singh V, Choudhary N, Mohan A, Bhatnagar S. Effect of Meditation and Breathing Exercises on the Well-being of Patients with SARS-CoV-2 Infection under Institutional Isolation: A Randomized Control Trial. Indian J Palliat Care 2021;27:490–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34898943&dopt=Abstract 10.25259/IJPC_40_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mollerup A, Henriksen M, Larsen SC, Bennetzen AS, Simonsen MK, Kofod LM, et al. Effect of PEP flute self-care versus usual care in early covid-19: non-drug, open label, randomised controlled trial in a Danish community setting. BMJ 2021;375:e066952. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34819329&dopt=Abstract 10.1136/bmj-2021-066952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Öner Cengiz H, Ayhan M, Güner R. Effect of deep breathing exercise with Triflo on dyspnoea, anxiety and quality of life in patients receiving covid-19 treatment: A randomized controlled trial. J Clin Nurs 2022;31:3439–53. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34897869&dopt=Abstract 10.1111/jocn.16171 [DOI] [PubMed] [Google Scholar]
- 74.Gonzalez-Gerez JJ, Saavedra-Hernandez M, Anarte-Lazo E, Bernal-Utrera C, Perez-Ale M, Rodriguez-Blanco C. Short-Term Effects of a Respiratory Telerehabilitation Program in Confined COVID-19 Patients in the Acute Phase: A Pilot Study. Int J Environ Res Public Health 2021;18:7511. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34299962&dopt=Abstract 10.3390/ijerph18147511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Adly AS, Adly MS, Adly AS. Telemanagement of Home-Isolated COVID-19 Patients Using Oxygen Therapy With Noninvasive Positive Pressure Ventilation and Physical Therapy Techniques: Randomized Clinical Trial. J Med Internet Res 2021;23:e23446. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33819166&dopt=Abstract 10.2196/23446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Li J, Xia W, Zhan C, Liu S, Yin Z, Wang J, et al. A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): a randomised controlled trial. Thorax 2022;77:697–706. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34312316&dopt=Abstract 10.1136/thoraxjnl-2021-217382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rosen K, Patel M, Lawrence C, Mooney B. Delivering Telerehabilitation to COVID-19 Inpatients:A Retrospective Chart Review Suggests It Is a Viable Option. HSS J 2020;16(Suppl 1):64–70. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32837409&dopt=Abstract 10.1007/s11420-020-09774-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement Ther Clin Pract 2020;39:101166–101166. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32379637&dopt=Abstract 10.1016/j.ctcp.2020.101166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Castillo-Allendes A, Contreras-Ruston F, Cantor-Cutiva LC, Codino J, Guzman M, Malebran C, et al. Voice therapy in the context of the COVID-19 pandemic: guidelines for clinical practice. J Voice 2021;35:717–27. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32878736&dopt=Abstract 10.1016/j.jvoice.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cantarella G, Aldè M, Consonni D, Zuccotti G, Berardino FD, Barozzi S, et al. Prevalence of Dysphonia in Non hospitalized Patients with COVID-19 in Lombardy, the Italian Epicenter of the Pandemic. J Voice 2023;37:605–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33766419&dopt=Abstract 10.1016/j.jvoice.2021.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Asiaee M, Vahedian-Azimi A, Atashi SS, Keramatfar A, Nourbakhsh M. Voice Quality Evaluation in Patients With COVID-19: An Acoustic Analysis. J Voice 2022;36:879.e13–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33051108&dopt=Abstract 10.1016/j.jvoice.2020.09.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Grilli GM, Giancaspro R, Del Colle A, Quarato CM, Lacedonia D, Foschino Barbaro MP, et al. Dysphagia in non-intubated patients affected by COVID-19 infection. Eur Arch Otorhinolaryngol 2022;279:507–13. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34468824&dopt=Abstract 10.1007/s00405-021-07062-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Archer SK, Iezzi CM, Gilpin L. Swallowing and voice outcomes in patients hospitalized with COVID-19: an observational cohort study. Arch Phys Med Rehabil 2021;102:1084–90. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33529610&dopt=Abstract 10.1016/j.apmr.2021.01.063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dawson C, Capewell R, Ellis S, Matthews S, Adamson S, Wood ME. Dysphagia presentation and management following coronavirus disease 2019: an acute care tertiary centre experience. J Laryngol Otol 2020;134:981–6. 10.1017/S0022215120002443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dani M, Dirksen A, Taraborrelli P, Torocastro M, Panagopoulos D, Sutton R, et al. Autonomic dysfunction in ‘long COVID’: rationale, physiology and management strategies. Clin Med (Lond) 2021;21:e63–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33243837&dopt=Abstract 10.7861/clinmed.2020-0896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Prem B, Liu DT, Besser G, Sharma G, Dultinger LE, Hofer SV, et al. Long-lasting olfactory dysfunction in COVID-19 patients. Eur Arch Otorhinolaryngol 2022;279:3485–92. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34757458&dopt=Abstract 10.1007/s00405-021-07153-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Asvapoositkul V, Samuthpongtorn J, Aeumjaturapat S, Snidvongs K, Chusakul S, Seresirikachorn K, et al. Therapeutic options of post-COVID-19 related olfactory dysfunction: a systematic review and meta-analysis. Rhinology 2023;61:2–11. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=36173148&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 88.Hayden MC, Limbach M, Schuler M, Merkl S, Schwarzl G, Jakab K, et al. Effectiveness of a Three-Week Inpatient Pulmonary Rehabilitation Program for Patients after COVID-19: A Prospective Observational Study. Int J Environ Res Public Health 2021;18:9001. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34501596&dopt=Abstract 10.3390/ijerph18179001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rodriguez-Blanco C, Gonzalez-Gerez JJ, Bernal-Utrera C, Anarte-Lazo E, Perez-Ale M, Saavedra-Hernandez M. Short-Term Effects of a Conditioning Telerehabilitation Program in Confined Patients Affected by COVID-19 in the Acute Phase. A Pilot Randomized Controlled Trial. Medicina (Kaunas) 2021;57:684. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34356965&dopt=Abstract 10.3390/medicina57070684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Stavrou VT, Tourlakopoulos KN, Vavougios GD, Papayianni E, Kiribesi K, Maggoutas S, et al. Eight Weeks Unsupervised Pulmonary Rehabilitation in Previously Hospitalized of SARS-CoV-2 Infection. J Pers Med 2021;11:806. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34442450&dopt=Abstract 10.3390/jpm11080806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pestelli MT, D’Abrosca F, Tognetti P, Grecchi B, Nicolini A, Solidoro P. Do not forget the lungs: preliminary feasibility study on I/E mode physiotherapy for people recovering from COVID-19. Panminerva Med 2022;64:208–14. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34664483&dopt=Abstract 10.23736/S0031-0808.21.04510-9 [DOI] [PubMed] [Google Scholar]
- 92.Baimukhamedov C, Barskova T, Matucci-Cerinic M. Arthritis after SARS-CoV-2 infection. Lancet Rheumatol 2021;3:e324–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33748780&dopt=Abstract 10.1016/S2665-9913(21)00067-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Munblit D, Nicholson T, Akrami A, Apfelbacher C, Chen J, De Groote W, et al. ; PC-COS project steering committee. A core outcome set for post-COVID-19 condition in adults for use in clinical practice and research: an international Delphi consensus study. Lancet Respir Med 2022;10:715–24. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35714658&dopt=Abstract 10.1016/S2213-2600(22)00169-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Post-COVID Condition Core Outcomes [Internet]. Available from: https://www.pc-cos.org/pc-cos_results [cited 2023, Nov 15].
- 95.Hidayati ER, Suharti A, Suratinoyo AT, Zahra SR, Nusdwinuringtyas N. Feasibility of the modified 30-second sit-to-stand test in an isolation ward of moderate COVID-19. Med J Indones 2021;30:306–10. 10.13181/mji.bc.215477 [DOI] [Google Scholar]
- 96.Twomey R, DeMars J, Franklin K, Culos-Reed SN, Weatherald J, Wrightson JG. Chronic Fatigue and Postexertional Malaise in People Living With Long COVID: An Observational Study. Phys Ther 2022;102:pzac005. 10.1093/ptj/pzac005 https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35079817&dopt=Abstract [DOI] [PMC free article] [PubMed]
- 97.Mohamed AA, Alawna M. The effect of aerobic exercise on immune biomarkers and symptoms severity and progression in patients with COVID-19: A randomized control trial. J Bodyw Mov Ther 2021;28:425–32. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34776174&dopt=Abstract 10.1016/j.jbmt.2021.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hermann M, Pekacka-Egli AM, Witassek F, Baumgaertner R, Schoendorf S, Spielmanns M. Feasibility and Efficacy of Cardiopulmonary Rehabilitation following COVID-19. Am J Phys Med Rehab 2020;99:865–9. 10.1097/PHM.0000000000001549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Foged F, Rasmussen IE, Bjørn Budde J, Rasmussen RS, Rasmussen V, Lyngbæk M, et al. Fidelity, tolerability and safety of acute high-intensity interval training after hospitalisation for COVID-19: a randomised cross-over trial. BMJ Open Sport Exerc Med 2021;7:e001156. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34493958&dopt=Abstract 10.1136/bmjsem-2021-001156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nambi G, Abdelbasset WK, Alrawaili SM, Elsayed SH, Verma A, Vellaiyan A, et al. Comparative effectiveness study of low versus high-intensity aerobic training with resistance training in community-dwelling older men with post-COVID 19 sarcopenia: A randomized controlled trial. Clin Rehabil 2022;36:59–68. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34344230&dopt=Abstract 10.1177/02692155211036956 [DOI] [PubMed] [Google Scholar]
- 101.Barbara C, Clavario P, De Marzo V, Lotti R, Guglielmi G, Porcile A, et al. Effects of exercise rehabilitation in patients with long coronavirus disease 2019. Eur J Prev Cardiol 2022;29:e258–60. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35078233&dopt=Abstract 10.1093/eurjpc/zwac019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nopp S, Moik F, Klok FA, Gattinger D, Petrovic M, Vonbank K, et al. Outpatient Pulmonary Rehabilitation in Patients with Long COVID Improves Exercise Capacity, Functional Status, Dyspnea, Fatigue, and Quality of Life. Respiration 2022;101:593–601. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35203084&dopt=Abstract 10.1159/000522118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sinha RK, Sinha S, Effectiveness Of Structured Exercise Protocol On Functional Performance In Subjects With GV. Covid-19. Int J Res Pharm Sci. 2020;11:1244–9. [Google Scholar]
- 104.Ballering AV, van Zon SK, Olde Hartman TC, Rosmalen JG, Lifelines Corona Research Initiative . Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet 2022;400:452–61. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35934007&dopt=Abstract 10.1016/S0140-6736(22)01214-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Roge I, Smane L, Kivite-Urtane A, Pucuka Z, Racko I, Klavina L, et al. Comparison of Persistent Symptoms After COVID-19 and Other Non-SARS-CoV-2 Infections in Children. Front Pediatr 2021;9:752385. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34778143&dopt=Abstract 10.3389/fped.2021.752385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Borch L, Holm M, Knudsen M, Ellermann-Eriksen S, Hagstroem S. Long COVID symptoms and duration in SARS-CoV-2 positive children - a nationwide cohort study. Eur J Pediatr 2022;181:1597–607. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35000003&dopt=Abstract 10.1007/s00431-021-04345-z [DOI] [PMC free article] [PubMed] [Google Scholar]


