ABSTRACT.
Dengue is a global health issue, particularly in the tropical and subtropical regions of the world. Prevention is the most appropriate method to fight the spread of the virus. The objective of this research is to present a model, along with visualizations, that will enable health officials and community leaders to identify when and where potential dengue outbreaks are likely to occur. Armed with this information, local resources can be adequately deployed in an effort to use limited supplies effectively. A mathematical model that uses easily obtainable data, along with visualizations for the 80 barangays of Cebu City, Philippines, is presented. Visualizations are constructed appropriate for a generalist audience to comprehend and use for dengue mitigation. Results of this study include a model that uses readily available data to predict dengue outbreaks one month in advance and visualizations appropriate for decision-makers in public health. Additional items are identified that could enhance the explanatory power of the model, and future directions are discussed.
INTRODUCTION
Dengue, a mosquito-transmitted disease (primarily by the Aedes aegypti mosquito), impacts humans in tropical and subtropical climates around the world. The latest estimates from the WHO indicate that 3.9 billion people are at risk of dengue and there could be between 284 million and 528 million cases per year.1 Roughly 80% of the cases are mild and/or asymptomatic, 19% manifest a more severe form of the illness, and less than 1% manifest severe dengue.1 Recently, the director of the WHO discussed the global burden of dengue, its negative impact on children (who are more susceptible to dengue), and the economic impact of dengue epidemics on local economies. Further, the director mentioned that climate change “is fueling outbreaks of cholera and dengue,”2,3 indicating renewed interest in the prevention of dengue worldwide. There is no specific treatment for dengue, and preventative measures seem to be the first line of defense against dengue, which necessitates the need for a model to predict when and where dengue is likely to occur so that mitigation activities can attempt to slow or stop the spread of dengue. Not only is a model desired, but a model with readily obtainable variables and easily understood outputs could be useful for local politicians, health department officials, and other decision makers responsible for public health.
The objectives of this research are to produce mathematical models for predicting when and where dengue is likely to appear and to produce visualizations to aid public health decision makers in communicating, assessing, and reacting to the threat of dengue to the community.
MATERIALS AND METHODS
Models.
Many models for dengue prediction, surveillance, and spread have been presented in the literature and tested against data, with mixed results. The frequency of dengue cases has been found to be closely related to a variety of climatic factors, including temperature, rainfall, and humidity.4,5 These factors can influence mosquito survival, reproduction, and biting rates, as well as human susceptibility to infection.6
Regression models have been explored for their predictive power for dengue numbers. These models include linear models,7,8 multiple linear regression models,8–10,11 autoregressive models,9,12 and autoregressive with moving average models (ARIMA).13–15 These types of models seem to yield the most useful and actionable results for a (predicted) response to a dengue threat, in that their variables are locally sourced (some with time lags), and predictions are based on a qualitative threat level for dengue (low, medium, high) that can be readily interpreted by a generalist audience.
Many of these models involve complex mathematical structures and parameter estimation techniques that require the use of specialized knowledge and software. Aguiar et al. state “Very complicated models are often developed to understand the dynamics of transmission of infectious diseases. However, due to the high degree of correlation between parameters, the evaluation of the results becomes difficult” and “modelers are often lost with the amount of ‘realistic assumptions’ required to be included in the modeling framework.”16
What is called for is an actionable model with locally available variables that can predict when and where the dengue burden will increase so that mitigation strategies can be applied effectively by local governmental agencies when and where the need is indicated.
Variables.
Variables for models predicting dengue generally concern the environment (precipitation, temperature, humidity), the population (number of dengue cases, human population, population density, urban/rural classification), and the location in both time and space (month and year, latitude and longitude). Table 1 summarizes the interest researchers have shown in each of the variables mentioned, along with other variables from the literature review.
Table 1.
Variables in dengue models
| Variables | References | Comments/data source |
|---|---|---|
| Variables included in models | ||
| Dengue cases* | 15 , 18 , 50 | The variable that models are trying to predict/describe; number of cases per barangay; retrieved from Center for Health Development for Central Visayas Region VII via written request |
| Precipitation* (mm) | 5 , 7 , 8 , 10 , 11 , 18 , 21 , 22 , 34 , 35 , 40 , 41 , 43 , 47 , 48 , 50 – 53 | All authors agree that precipitation has an effect on dengue, as mosquitoes need water to breed, and precipitation is significant in many models; https://www.pagasa.dost.gov.ph/climate/climate-data |
| Median or mean temperature* (°C) | 5 , 7 , 8 , 11 , 18 , 20 – 22 , 34 , 35 , 40 , 41 , 47 , 52 , 54 | Low, average, and high temperatures also used. As temperature increases, virus incubation speeds up; https://www.pagasa.dost.gov.ph/climate/climate-data |
| Relative humidity* | 8 , 10 , 22 , 34 , 41 , 47 , 52 , 54 | Spurious results for humidity; some authors find significance, others do not; https://www.pagasa.dost.gov.ph/climate/climate-data |
| Population* (2010, 2015) | 34 , 43 , 44 | More people can imply more dengue, as humans are the reservoir for dengue; https://www.philatlas.com/visayas/r07/cebu-city.html |
| Elevation (m) | 14 , 22 , 43 | Has not shown to be a good indicator of dengue or of Aedes mosquito populations; https://www.philatlas.com/visayas/r07/cebu-city.html |
| Area of Barangay (km2) | Used for computing population density; https://www.citypopulation.de/en/philippines/cebu/ | |
| Barangay names | Used for labeling (N = 80); https://psa.gov.ph/classification/psgc/?q=psgc/barangays/072217000 | |
| Urban/rural (1/0) | 29 , 30 , 44 | A global definition of urbanization is lacking29; could there be more than two levels of an urban variable?30 900 people/km2 is used to define “urban” in this research. https://psa.gov.ph/classification/psgc/?q=psgc/barangays/072217000 |
| Threat level (H, M, L) | 8 , 23 , 40 , 41 , 55 | Calculated field; a qualitative variable used to indicate when and/or where dengue could be problematic |
| Variables calculated or used for mapping | ||
| Population density (people/km2) | 33 , 43 , 44 | Calculated field; > 1,000 people/km2 can indicate increased levels of arboviral diseases29 |
| Number of dengue cases/1,000 population | Calculated field | |
| Location (latitude and longitude of barangay) | Where dengue cases are recorded; Google API used for coordinates | |
| Time index (month, year) | When dengue cases, precipitation, and temperature are recorded | |
| Variables identified by other authors not available for this study | ||
| Wind speed | 8 , 34 | Spurious results |
| Hours of sunshine | 10 , 41 | Surveillance results indicate that female Aedes mosquitoes are more present during the daylight hours (Microsoft Corp.) |
| El Niño/La Niña (ENSO) index | 17 , 20 , 24 | El Niño/La Niña years correspond to extreme weather events;46 a precipitation variable might describe this effect |
| Socioeconomic factors | 29 , 40 | Poverty index, garbage collection, electricity access, drinking water access, and educational attainment, etc. |
| Surveillance data | 7 , 18 , 34 , 44 | Number of positive containers for Aedes larvae, count of adult mosquitoes in traps, mosquito density |
| Education factors | 56 – 58 | Activities to increase public awareness of the transmission and prevention of dengue |
| Preventative factors | 34 , 44 , 54 , 59 | Mosquito coil, netting, window screen, spraying, garbage disposal |
H = high; L = low; M = medium.
Variables used by the WHO in their Early Warning and Response System for Dengue (EWARS)20; the EWARS needs a minimum of 2 years of data.
Other manipulations of the variables include time-lagged variables, where the lag ranged between 1 week9 and 5 months.17 The lagged variables included temperature,13,14,18–20 precipitation,13,14,18–20 humidity,13,19 and number of dengue cases.13,18,21 Interaction terms have also been used by authors22 to explore interactions between environmental variables. Hittiarachchige et al. found that many terms of interaction between elevation, humidity, temperature, and precipitation variables were significant predictors of mosquito presence in Taiwan in a logistic model.22
Visualizations.
Geospatial models have been used to show where dengue, historically, is higher than usual.12,14,23,24 Most of these geospatial models are at a state (province) or city level of granularity, too large of an area for effective mitigation techniques to be applied.
Three other factors (dengue affects younger people, dengue is underreported, and dengue has large cost consequences) direct researchers to the importance of developing an accurate, actionable, and easily accessible model, along with visualizations, for the prediction of when and where dengue is expected to occur.
Cost of dengue.
The costs of dengue and the burden on society can be measured in diverse ways. The most common is in monetary units, whereas another measure is in disability adjusted life years (DALY).25 These two, along with number of deaths, yield the societal costs of dengue, as well as the potential benefits of a predictive model that would allow the mitigation of dengue and the reduction of these costs. For example,26 it is reported that Mexico had costs of $87 million with 65 DALYs due to dengue in 2010–2011, whereas Taborda et al.27 reported, in 2013, 58.4 million cases of dengue with 14,000 deaths and 1.14 million DALYs in Colombia. Edillo et al.28 estimate 842,867 clinically diagnosed dengue cases costing the Philippines $345 million per year in 2012.
Methods.
The data for the model were collected from the locations listed in Table 1, and the model training data set contained monthly measurements from 2010 through 2019. The 80 barangays of Cebu City were selected to evaluate the availability of the data in this pilot study. Cebu Province has 1,204 barangays spanning the entire island, and plans to collect this larger data set are under way.
The main data cleansing activity was concerned with the names of the 80 barangays (the lowest level of governmental organization in the Philippines) of Cebu City, as some have multiple spellings (Sambag 2 versus Sambag II, Suba versus Suba Poblation, Basak versus Basak Pardo, Central versus Santa Niño, and Camputhaw versus Kamputhaw) depending on the data source. Additionally, linear estimates of barangay populations were made for noncensus years, and the “urban” variable (generally a binary variable) needed adjusting. There is no global definition of urban,29 and one author group30 even poses three levels, namely, urban, semiurban, and rural, as a delineation of population density. The Philippines Statistics Authority31 (PSA) defines urban as a barangay with a population of over 5,000 (main definition).
Upon assignment of a barangay’s rural/urban status based on the PSA table, one error was found with barangay Pulangbato, population 5,539. Pulangbato was assigned the status of rural but should be urban. However, since this paper uses relative metrics for the response variable, number of cases/1,000 population, an alternative method of assigning urban status is sought, namely, population density. A cutoff of 900 people/km2 was selected to minimize the number of discrepancies with the PSA, which is in line with most density definitions of urban29 and will accommodate changes in population over the time interval 2010 to 2019. This cutoff yields a 3.5% difference in classifications, which were then adjusted to adhere to the 900 people/km2 definition.
After obtaining, cleansing, and structuring the data, multiple correlations were run using the data analytics tool pack in Excel (Microsoft Corp.), and it was determined that the relative dengue measurement (number of cases/1,000 people) would be used as the response variable, as the absolute number of dengue cases had less correlation and is more susceptible to interpretation error because of the various sizes of barangays in Cebu City.
Running multiple linear regressions with the variables listed in Table 1 yielded significant variables (P < 0.05) but low explanatory power (R2 ≈ 3–4%). Since the dengue reservoir is the human, the previous month’s dengue incidence was added to the list of independent variables, which added a feedback loop into the model. A 1-month-lagged variable makes sense, due to the short life span of mosquitoes, which involves a rain event (to saturate mosquito eggs), 8 to 10 days for the larva to pupa to adult stages,32 and 1 to 2 months for the adult stage, for which the typical range of the adult mosquito is a few blocks (approximately 200 m).32,33 The addition of variables with a 1-month time delay incorporates the mosquito life cycle and aligns with other authors’ research into lagged variables.13,18,21
The remaining variables from Table 1 (year, month, barangay, dengue incidence, latitude, longitude, urban/rural, and threat level) will be used in conjunction with the analytical results to produce geospatial analysis and indicators of dengue outbreaks.
RESULTS
Analytical results.
Many models (multiple linear regression, logistic regression, and delay equations) for predicting dengue cases in Cebu City, Philippines, were tried, and the top-performing models are given as Equations (1)–(4) and are computed on the training data set (N = 9,600) from 2010 through 2019, across the entirety of Cebu City. These are all multiple linear regression models, some with time delay terms and one with an interaction term, E × Ht (elevation × humidity).
| (1) |
| (2) |
| (3) |
| (4) |
where an asterisk indicates the only variable not significant at 0.05, yt = number of dengue cases/1,000 population; T = mean monthly temperature in Celsius; R = monthly rainfall in millimeters, E = barangay elevation in meters, H = mean monthly relative humidity, SE = standard error, and mean absolute error (MAE). The subscript indicates the time interval, with t – 1 representing the lagged variables. All models perform equally well when measured with the R2 value, but model 4 outperforms the other three according to the MAE value, which is computed on the test data covering 2020 to 2021.
Temperature, rainfall, humidity, and elevation × humidity all have a positive effect on the number of predicted dengue cases, in agreement with other authors’ findings.7,8,18,22,24,34,35 However, the previous month’s dengue incidence is, by far, the strongest predictor of the coming month’s number (per 1,000 people) of dengue cases9,18,21 in all models. Also, as found in Koplewitz et al9, a shorter delay tended to have better predictive power, indicating that recent history is a better predictor for future dengue cases, further supporting the selection of a 1-month delay period. It is interesting to note that population, population density, and urban variables were shown not to be significant predictors of dengue incidents, in contrast to what other authors have found.29,30,34 Many explanations for this have been explored, including the presence of more vector control measures (mosquito nets, spraying, and larval eradication) in urban areas.36,37 Other authors have found that the relationship between population density and dengue cases varied depending on the strain of dengue virus, with some strains being more efficiently transmitted in areas with lower population density.38 Overall, the relationship between population density and dengue cases is complex and depends on several factors. It is important to consider these factors when studying the impact of population density, socioeconomic factors, and urbanization on the incidence of dengue fever.
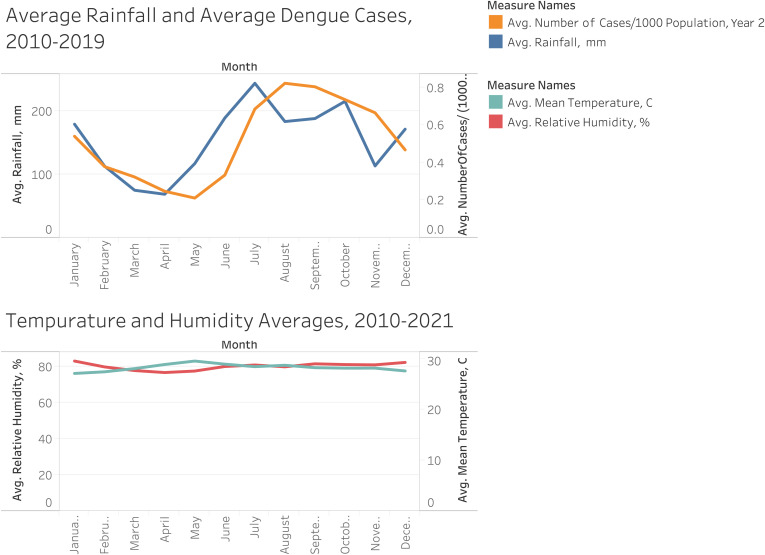
Figure 1 illustrates that dengue incidence closely follows seasonal rains and helps to rationalize the 1-month time lag for the variables in this study. Colón-González et al.39 also observed that the highest predictive ability of their model had a lead time of 1 month, with predictive ability declining for higher lead times.
Figure 1.
Dengue and rainfall. Average median temperature and humidity, monthly 2010–2021. Figure created with Tableau (Salesforce, San Francisco, CA).
Figure 1 also illustrates the lack of noticeable effect that mean temperature and mean humidity have on the average number of dengue cases, being relatively constant over the time period of the study, especially during the peak months for dengue, June to December. Su11 also concludes that temperature is not significantly related to dengue incidence, whereas rainfall does have an influence in his study area, Metro Manila. These indicators lend credence to model 4, which does not include temperature or humidity.
Equation (4) is an easily deployable, readily understood model applicable to a generalist audience that can predict when the dengue threat is high, medium, or low in a given barangay.
When applied to the test data set (2020–2021), model 4 performed 22% better, on average, than the other models. More importantly, from an application standpoint, model 4 predicted the threat level with an overall accuracy level of 61.7%, comparing favorably with the R2 values of Equation (4), as shown in Table 2.
Table 2.
Classification matrix for model 4 with test data, 2020–2021
| Threat level | Predicted | Total | |||
|---|---|---|---|---|---|
| Low | Medium | High | |||
| Actual | Low | 976 | 577 | 16 | 1,569 |
| Medium | 93 | 182 | 16 | 291 | |
| High | 7 | 26 | 27 | 60 | |
| Total | 1,076 | 785 | 59 | 1,920 | |
Table 2 introduces a classification scheme that was generated to illustrate, using visualizations, to interested parties if the barangay has a low (L), medium (M), or high (H) threat level for dengue, based on annual historical averages. Different author groups define L, M, and H slightly differently, but all are reasonably close and follow standard statistical protocols. For example, in a study by Buzcak et al.,40 the cutoff between L and H occurs at (where s is the standard deviation) whereas Descloux et al.8 uses terciles to determine outbreaks and Hau et al.41 computes one s above the mean. Another study, conducted in the Barbados,17 uses the 75th percentile to define the outbreak threshold, whereas the WHO42 discusses many types of “outbreak alert” conditions to include 2 s above the mean for various moving averages, 1.25 s of the moving mean for 2 weeks, and an “endemic channel” that uses a time series and quartiles to produce an “alarm zone” throughout the year. Colón-González et al.39 add a level to have low, moderate, high, and very high if dengue levels are below the mean or 1 or 2 SD above the mean. This paper uses the following definition to establish H, M, or L threat levels, per barangay, per month, and for each year, as the variables change throughout the time period of observation:
| (5) |
where is the annual average of dengue cases (density) per barangay and s is the annual standard deviation (SD) of dengue cases (density) per barangay. Equation (5) relies on the annual dengue density of the barangay (number of cases/1,000 population) and therefore uses 10 years of data observations, localized in both time and space, to better assess the local risk and can thus inform the local response to these “dengue alerts.” Specificity and sensitivity for each of the threat levels are given in Table 3.
Table 3.
Specificity and sensitivity for model 4 with test data, 2020–2021
| Barangay threat level | Specificity, % | Sensitivity, % |
|---|---|---|
| Low | 67.6 | 62.2 |
| Medium | 62.5 | 62.5 |
| High | 97.3 | 45.0 |
Two other classifications of interest are barangays that are classified as high threat but are not (N = 32, 54.2% false-positive error) and barangays that are high threat but are classified lower (N = 33, 55.0% false-negative error) over the course of the 2-year test data set. For the first, resources are deployed where they might not be necessary, and for the second, resources are not deployed when actual need is present.
Arguably, the test years for the models (2020–2021) were skewed because of the COVID restrictions that constrained the movement of the population (the major reservoir for dengue) and could have affected the reporting of dengue as well. The COVID restrictions led to a decrease in population interactions and thus lowered the dengue case load, as shown in Figure 2.
Figure 2.
Average dengue load, 2010–2021. Figure created with Tableau (Salesforce, San Francisco, CA).
The downward trend in the dengue load is evident, as dengue cases dropped to their lowest levels in 2021 (both in absolute and relative measures). As data become available for 2022, the model will be tested further for its predictive power.
Geospatial results.
Creating a visual display for analytical results is critical for communicating these findings to a generalist audience. Variables collected for the visualizations include latitude and longitude coordinates of the barangays, month and year for data collected, number of dengue cases per month, barangay population (linearly extrapolated between census years), and an urban/rural variable to be used as an exploratory filter variable. Also used are the threat level definitions from Equation (5) to determine which barangays have the highest dengue threat, and which thus would be the first to start mitigation measures in a public health effort to slow the spread of dengue. An example of a threat map is given in Figure 3.
Figure 3.
Example of dengue threat map, per barangay, for June 2012. Figure created with Tableau (Salesforce, San Francisco, CA).
Evaluation of Figure 3 tells barangay captains (the elected political leader of the barangay), Department of Health officials, and other decision makers when and where to deploy limited resources to stem the spread of dengue. Hovering over the barangay location gives the text box seen in Figure 3. These maps form a geospatial time series, one map per month from January 2010 through December 2021 (120 maps with 80 barangays each), enabling researchers to view the spatial evolution of dengue throughout Cebu City over time. Visual identification of when, on average, each barangay experiences peak dengue can also be observed in Figure 4.
Figure 4.
Dengue load and rainfall averages, by month, 2010–2019. Figure created with Tableau (Salesforce, San Francisco, CA).
Figures 3 and 4 can be used to advise barangay captains and health officials of the probable location and timing of dengue in their communities. These visualizations are dynamic, showing the time evolution of the dengue load in the Cebu City area by month and barangay. Utilization of these visualizations acquired from readily obtainable data can inform decision makers in the Cebu City area in their deployment of resources in an attempt to mitigate the spread of dengue.
DISCUSSION
Dengue is a global health threat that demands community action to mitigate its spread. Dengue is a leading cause of hospitalization and death in children in southeast Asia,14 which accounts for 70% of the global dengue burden.1 In the Philippines, the disease is predominantly reported among children.43,44 Dengue is getting worse, with cases in the Central Visayas growing from 256 in 2021 to over 11,000 in 2022.45,46 Many studies indicate a concern that as climate change progresses, endemic areas are likely to increase, exposing greater numbers of people to the risk of dengue.47,48
This research accomplishes what many authors have called for, a simple yet effective model for decision makers. As Hau et al.41 describe, “The implementation of an early-warning system for dengue fever requires it to be based on data that is widely accessible throughout Vietnam at short notice, with low costs involved.” Based on the current dengue load in a barangay along with the rainfall totals, this model can compute the next time period’s dengue burden and assign a threat level indicating if mitigating strategies should be immediately started, held in reserve, or deemed not a current concern. The visualizations produced from the data set will assist in communicating the threat level and location of the threat to policymakers and the public. This pilot study of the barangays of Cebu City holds potential for assisting and directing resources in the fight against dengue.
Limitations of study.
This study has several limitations that, if overcome, could increase the predictive power of the model. Some of these limitations include a more localized data gathering activity, as temperature, humidity, and rainfall are recorded for Cebu City, not for each barangay.
Data collection needs to be addressed, as there are anomalies in the data that could be attributed to data entry errors or the lack of reporting. For example, there are 3,757 reports of no dengue cases out of 9,600 reporting intervals in the study. This might not be unusual, but in addition, there are 44 barangays (some repeated) reporting zero cases for the entire year (12 reporting periods). Figure 5 illustrates one of these cases.
Figure 5.
Case count, per year, in Zapetera, Cebu City, 2010–2021. Figure created with Tableau (Salesforce, San Francisco, CA).
Figure 5 shows Zapetera, a barangay in Cebu City, as reporting zero cases for 2011, 2012, 2013, 2016, 2017, and 2018. However, 2012 and 2016 were high years for dengue in the Cebu City area, leading to suspicions of the underreporting of data. Data underreporting has been and continues to be a problem with dengue monitoring.6,48,49
Related to population movement, a nearest neighbor or other proximity variable might aid in the predictive power of the model. Other variables that could contribute to the strength of the model concern the barangay itself. These could include electricity access (percentage of barangay), drinking water access, a sanitation index, the frequency of trash pickup, or other social variables identified by many authors.
Visualizations could be made more effective if the latitude and longitude along with the date of detection of the dengue case could be collected. This would enable greater granularity of the visualization and potentially lead to more effective tracking of the movement of the dengue infections.
Future directions.
Overall, the goal is to enhance the model, through variable acquisition and model improvements, to minimize the number of false negatives and increase the overall accuracy of the model to better inform the decision maker of when and where to take action to prevent the spread of dengue. A larger data set, representing the 1,204 barangays of Cebu province, could shed light on the effect of many variables (urban/rural, elevation) not seen in this urban pilot study area.
REFERENCES
- 1. World Health Organization , 2022. Dengue and Severe Dengue. Available at: https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue. Accessed June 2, 2023.
- 2. World Health Organization , 2022. WHO Director-General’s Opening Remarks at Media Briefing – 2 November 2022. Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-media-briefing–2-november-2022. Accessed June 2, 2023.
- 3. World Health Organization , 2022. WHA55.17 Dengue Fever and Dengue Haemorrhagic Fever Prevention and Control. Available at: https://www.who.int/publications/i/item/wha55.17. Accessed June 2, 2023.
- 4. Kesetyaningsih TW, Andarini S, Sudarto S, Pramoedyo H, 2018. Determination of environmental factors affecting dengue incidence in Sleman District, Yogyakarta, Indonesia. Afr J Infect Dis 12: 13–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gutierrez JA, Laneri K, Aparicio JP, Sibona GJ, 2022. Meteorological indicators of dengue epidemics in non-endemic Northwest Argentina. Infect Dis Model 7: 823–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rungd-Ranzinger S, Horstick O, Marx M, Kroeger A, 2008. What does dengue disease surveillance contribute to predicting and detecting outbreaks and describing trends? Trop Med Int Health 13: 1022–1041. [DOI] [PubMed] [Google Scholar]
- 7. Murphy AK. et al. , 2022. Climate variability and Aedes vector indices in the southern Philippines: an empirical analysis. PLoS Negl Trop Dis 16: e0010478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Descloux E. et al. , 2012. Climate-based models for understanding and forecasting dengue epidemics. PLoS Negl Trop Dis 6: e1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Koplewitz G, Lu F, Clemente L, Buckee C, Santillana M, 2022. Predicting dengue incidence leveraging internet-based data sources. A case study in 20 cities in Brazil. PLoS Negl Trop Dis 16: e0010071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vu HH, Okumura J, Hashizume M, Tran DN, Yamamoto T, 2014. Regional differences in the growing incidence of dengue fever in Vietnam explained by weather variability. Trop Med Health 42: 25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sia Su GL, 2008. Correlation of climatic factors and dengue incidence in Metro Manila, Philippines. Ambio 37: 292–294. [DOI] [PubMed] [Google Scholar]
- 12. Desjardins MR, Eastin MD, Paul R, Casas I, Delmelle EM, 2020. Space-time conditional autoregressive modeling to estimate neighborhood-level risks for dengue fever in Cali, Colombia. Am J Trop Med Hyg 103: 2040–2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Baquero OS, Santana LMR, Chiaravalloti-Neto F, 2018. Dengue forecasting in São Paulo city with generalized additive models, artificial neural networks, and seasonal autoregressive integrated moving average models. PLoS One 13: e0195065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bett B. et al. , 2019. Spatiotemporal analysis of historical records (2001–2012) on dengue fever in Vietnam and development of a statistical model for forecasting risk. PLoS One 14: e0224353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wongkoon S, Jaroensutasinee M, Jaroensutasinee K, 2012. Development of temporal modeling for prediction of dengue infection in Northeastern Thailand. Asian Pac J Trop Med 5: 249–252. [DOI] [PubMed] [Google Scholar]
- 16. Aguiar M, Anam V, Blyuss KB, Estadilla CDS, Guerrero BV, Knopoff D, Kooi BW, Srivastav AK, Steindorf V, Stollenwerk N, 2022. Mathematical models for dengue fever epidemiology: a 10-year systematic review. Phys Life Rev 40: 65–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lowe R, Gasparrini A, Van Meerbeeck CJ, Lippi CA, Mahon R, Trotman AR, Rollock L, Hinds AQJ, Ryan SJ, Stewart-Ibarra AM, 2018. Nonlinear and delayed impacts of climate on dengue risk in Barbados: a modelling study. PLoS Med 15: e1002613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Xu L. et al. , 2017. Climate variation drives dengue dynamics. Proc Natl Acad Sci USA 114: 113–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cardenas R, Hussain-Alkhateeb L, Benitez-Valladares D, Sánchez-Tejeda G, Kroeger A, 2022. The Early Warning and Response System (EWARS-TDR) for dengue outbreaks: can it also be applied to chikungunya and Zika outbreak warning? BMC Infect Dis 22: 235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Colón-González FJ, Lake IR, Bentham G, 2011. Climate variability and dengue fever in warm and humid Mexico. Am J Trop Med Hyg 84: 757–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hii YL, Zhu H, Ng N, Ng LC, Rocklöv J, 2012. Forecast of dengue incidence using temperature and rainfall. PLoS Negl Trop Dis 6: e1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hettiarachchige C, von Cavallar S, Lynar T, Hickson RI, Gamvhir M, 2018. Risk prediction system for dengue transmission based on high resolution weather data. PLoS One 12: e0208203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Baak-Baak CM, Cigarroa-Toledo N, Pinto-Castillo JF, Cetina-Trejo RC, Torres-Chable O, Blitvich BJ, Garcia-Rejon JE, 2022. Cluster analysis of dengue morbidity and mortality in Mexico from 2007 to 2020: implications for the probable case definition. Am J Trop Med Hyg 106: 1515–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chuang TW, Chaves LF, Chen PJ, 2017. Effects of local and regional climatic fluctuations on dengue outbreaks in southern Taiwan. PLoS One 12: e0178698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zeng Z, Shan J, Chen L, Chen H, Cheng S, 2021. Global, regional, and national dengue burden from 1990 to 2017: a systematic analysis based on the global burden of disease study 2017. EClinicalMedicine 32: 100712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Undurraga EA. et al. , 2015. Economic and disease burden of dengue in Mexico. PLoS Negl Trop Dis 9: e0003547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Taborda A, Camorro C, Quintero J, Carrasquilla G, Londoño D, 2022. Cost-effectiveness of a dengue vector control intervention in Colombia. Am J Trop Med Hyg 107: 180–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Edillo FE, Halasa FM, Erasmo JN, Amoin NB, Alera MT, Yoon IK, Alcantara AC, Shepard DS, 2015. Economic cost and burden of dengue in the Philippines. Am J Trop Med Hyg 92: 360–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kolimenakis A, Heinz S, Wilson ML, Winkler V, Yakob L, Michaelakis A, Papachristos D, Richardson C, Horstick O, 2021. The role of urbanization in the spread of Aedes mosquitoes and the diseases they transmit – a systematic review. PLoS Negl Trop Dis 15: e0009631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lizarralde-Bejarano DP, Rojas-Diaz D, Arboleda-Sánchez S, Puerta-Yepes ME, 2020. Sensitivity, uncertainty and identifiability analyses to define a dengue transmission model with real data of an endemic municipality of Colombia. PLoS One 15: e0229668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Philippines Statistics Authority , 2023. ISSiP Inventory of Statistical Standards in the Philippines. Available at: https://psa.gov.ph/ISSiP/concepts-and-definitions/161175. Accessed June 2, 2023.
- 32. CDC Mosquito Life Cycle: Aedes aegypti. Available at: www.cdc.gov/dengue. Accessed June 1, 2023.
- 33. Biogents 2018. Life Cycle of Aedes Mosquitoes. Available at: https://sea.biogents.com/life-cycle-aedes-mosquitoes/. Accessed June 1, 2023.
- 34. Edussuriya C, Deegalla S, Gawarammana I, 2021. An accurate mathematical model predicting number of dengue cases in tropics. PLoS Negl Trop Dis 15: e0009756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ebi KL, Nealon J, 2016. Dengue in a changing climate. Environ Res 151: 115–123. [DOI] [PubMed] [Google Scholar]
- 36. de Oliveira HG, Barreto FR, Da Rosa ES, De Melo AS, De Arruda ME, Guimarães AE, 2014. Population density and dengue dispersion in urban areas. J Infect Dis 210: 670–671. [Google Scholar]
- 37. Barrera R, Amador M, Acevedo V, Caban B, 2011. Status of dengue in Puerto Rico after the Zika epidemic. J Infect Dis 214 ( Suppl 5 ): S297–S302. [Google Scholar]
- 38. Cummings DA, Irizarry RA, Huang NE, Endy TP, Nisalak A, Ungchusak K, Burke DS, 2009. Travelling waves in the occurrence of dengue haemorrhagic fever in Thailand. Nature 427: 344–347. [DOI] [PubMed] [Google Scholar]
- 39. Colón-González FJ. et al. , 2021. Probabilistic seasonal dengue forecasting in Vietnam: a modelling study using superensembles. PLoS Med 18: e1003542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Buczak AL. et al. , 2014. Prediction of high incidence of dengue in the Philippines. PLoS Negl Trop Dis 8: e2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hau VH. et al. , 2022. Deep learning models for forecasting dengue fever based on climate data in Vietnam. PLoS Negl Trop Dis 16: e0010509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. World Health Organization , 2016. Technical Handbook for Dengue Surveillance, Dengue Outbreak Prediction/Detection and Outbreak Response (“Model Contingency Plan”). Available at: https://fctc.who.int/publications/i/item/2016-09-30-technical-handbook-for-dengue-surveillance-dengue-outbreak-prediction-detection-and-outbreak-response. Accessed May 22, 2023.
- 43. Agrupis KA, Ylade M, Aldaba J, Lopez AL, Deen J, 2019. Trends in dengue research in the Philippines: a systematic review. PLoS Negl Trop Dis 13: e0007280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bravo L, Roque VG, Brett J, Dizon R, L’Azou M, 2014. Epidemiology of dengue disease in the Philippines (2000–2011): a systematic literature review. PLoS Negl Trop Dis 8: e3027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sitchon J, 2022. Central Visayas Sees ‘Alarming’ Rise in Dengue Cases in First Half of 2022. Available at: https://www.rappler.com/nation/rise-dengue-cases-central-visayas-first-half-2022/. Accessed July 20, 2023.
- 46. Magsumbol CN, 2022. Dengue Claims 71; Cases Soar to Over 11,000 in CV. Available at: https://www.philstar.com/the-freeman/cebu-news/2022/08/13/2202423/dengue-claims-71-cases-soar-over-11000-cv. Accessed July 20, 2023.
- 47. Pineda-Cortel MRB, Clemente BM, Nga PTT, 2019. Modeling and predicting dengue fever cases in key regions of the Philippines using remote sensing data. Asian Pac J Trop Med 12: 60–66. [Google Scholar]
- 48. Hossain S, Islam MM, Hasan MA, Chowdhury PB, Easty IA, Tusar MK, Rashid MB, Bashar K, 2023. Association of climate factors with dengue incidence in Bangladesh, Dhaka City: a count regression approach. Heliyon 9: e16053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Undurraga EA, Edillo FE, Erasmo JN, Alera MT, Yoon IK, Largo FM, Shepard DS, 2017. Disease burden of dengue in the Philippines: adjusting for underreporting by comparing active and passive dengue surveillance in Punta Princesa, Cebu City. Am J Trop Med Hyg 96: 887–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Panja M, Chakraborty T, Nadim SS, Ghosh I, Kumar U, Liu N, 2023. An ensemble neural network approach to forecase dengue outbreak based on climatic condition. Chaos Solutions Fractals 167: 113124. [Google Scholar]
- 51. Mai ST, Phi HT, Abubakar A, Kilpatrick P, Nguyen HQV, Vandierendonck H, 2023. Dengue fever: from extreme climates to outbreak prediction. 2022 IEEE International Conference on Data Mining proceedings, 1083–1088.
- 52. Olmoguez ILG, Catindig MAC, Amongos MFL, Lazan FG, 2019. Developing a dengue forecasting model: a case study in Iligan City. Int J Adv Comput Sci Appl 10: 281–286. [Google Scholar]
- 53. Subido ME, Aniversario IS, 2022. A correlation study between dengue incidence and climatological factors in the Philippines. Asian Res J Math 18: 110–119. [Google Scholar]
- 54. Solidum JN, 2016. Correlation of climate change factors with dengue incidence in Old Balara, Quezon City, Philippines. IAMURE Int J Ecol Conserv 17: 113–122 [Google Scholar]
- 55. World Health Organization , 2020. Operational Guide Using the Web-Based Dashboard: Early Warning and Response System (EWARS) for Dengue Outbreaks, 2nd ed. Available at: https://apps.who.int/iris/handle/10665/332323. Accessed June 1, 2023.
- 56. Ferdousi F, Yoshimatsu S, Ma E, Sohel N, Wagatsuma Y. 2015. Identification of essential containers for Aedes larval breeding to control dengue in Dhaka, Bangladesh. Trop Med Health 43: 253–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hermida MJ, Santangelo AP, Calero CI, Goizueta C, Espinosa M, Sigman M, 2021. Learning-by-teaching approach improves dengue knowledge in children and parents. Am J Trop Med Hyg 105: 1536–1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Solidum JN, Solidum GG, 2015. Storytelling as a health teaching strategy for dengue prevention and control in the Philippines. Philipp J Sci 144: 61–67. [Google Scholar]
- 59. Labrague LJ, 2013. Dengue knowledge and preventive practices among rural residents in Samar Province, Philippines. Am J Public Health Res 1: 47–52. [Google Scholar]