Abstract
National Health Service Hospitals are under pressure to reduce waiting lists within the constraints of a limited infrastructure. We implemented two systems to reduce waiting times for elective non-complex spinal surgery. The first of these was the introduction of managed generic waiting lists for both initial outpatient appointments and subsequent surgery. Thereafter, the MRI booking system was integrated with outpatient review appointments. Times from referral to first outpatient appointment and from scan to outpatient review and time on waiting list for surgery were analysed before and after implementation of these changes.
Despite constant unit capacity there was a global decrease in waiting times. Before introduction of the generic waiting list, 37% of listed patients waited for more than 9 months; this figure fell to zero. Time from scan to outpatient review was 185 days before integration, 30 days after.
Changes of this sort demand a quorum of consultants who will accept each others' recommendations. The generic waiting list will have impact only when there are large disparities in waiting times for different consultants. Targets are met at the expense of continuity of care.
INTRODUCTION
The global trend within the National Health Service over the past decade has been of lengthening waiting times as outdated systems struggle to cope with increased demand and expectation. The Government has adopted a target driven system to address the most obvious shortcomings, often without providing resources to cope with an increased throughput.
According to The NHS Plan1 the maximum waiting time for a routine outpatient appointment will be 3 months, the maximum waiting time for inpatient treatment will be 6 months and the maximum wait for any stage of treatment will be 3 months. These are to be achieved in a staged process, culminating at the end of 2008.
METHODS
All neurosurgical services within Greater Manchester were amalgamated to the Hope Hospital site in Salford in May 2001, and this is the time when our data collection begins. To reduce waiting times, we employed two strategies. First, managed generic waiting lists were introduced for both initial outpatient appointments and dates for surgery. Subsequently the computerized MR booking system was integrated with outpatient review appointments.
The managed generic outpatient waiting list begins with a consultant screening all new GP referred spinal cases to assess their suitability for a pooled waiting list. They are then allocated to the next available appointment irrespective of who the consultant might be. The managed generic surgical waiting list works by a similar process. When consultants list a patient for elective non-complex spinal surgery, they indicate whether the patient should remain under their care or enter a pooled waiting list. The pooled patients are then allocated dates for surgery sequentially. The integration of the MR appointment system with outpatient follow-up entails regular secretarial review of which patients are to be scanned. As soon as these appointments are allocated, ring-fenced outpatient review appointments are provided.
We compared data collected before and after implementation of these two new systems. The outcome measures were time from referral to first outpatient appointment, time from scan to outpatient review and time on waiting list for surgery.
RESULTS
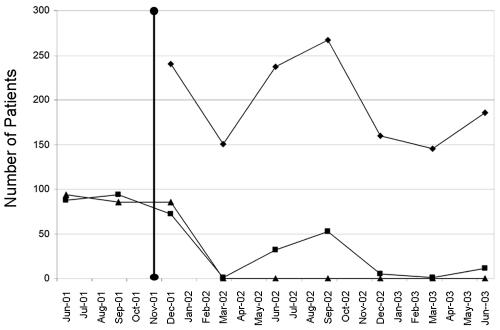
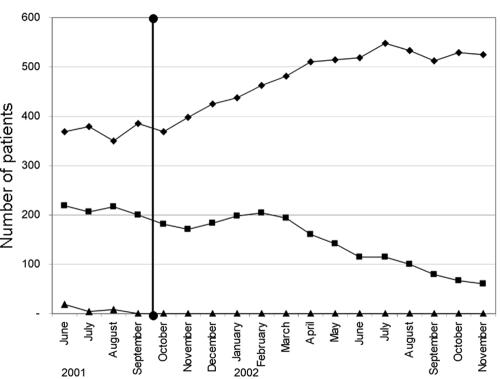
Figure 1 shows times to first neurosurgical outpatient examination. The number of patients waiting more than 26 weeks fell to zero and the number waiting more than 13 weeks declined greatly. After introduction of the integrated MR follow-up system, the mean wait from MR scan to outpatient review fell from 185 days to 31 days. At the time of introduction of the generic waiting list for elective surgery, 37% of listed patients had been waiting for more than 9 months. The number is currently zero (Figure 2).
Figure 1.
Time patients waited from GP referral to consultant outpatient review: number of patients within three waiting time categories before and after introduction of generic waiting list. ⋄ 0–12 weeks; ▪ 13–26 weeks; ▴ 26+ weeks; • introduction of a generic waiting list for elective spinal surgery
Figure 2.
Time patients waited from being placed on a waiting list for surgery until operation: number of patients within three waiting time categories before and after the introduction of generic waiting list. ⋄ Less than 9 months; ▪ 9–18 months; ▴ more than 18 months; • introduction of a generic waiting list for elective spinal surgery
DISCUSSION
The introduction of these systems has dramatically reduced waiting times within our unit for each stage of the referral process. However, the waiting list figures alone paint an incomplete picture. The first potential difficulty we faced with the generic waiting list was in establishing a quorum of consultants within our unit prepared to accept the underlying premise of possible discontinuity in patient care. Of the ten neurosurgical consultants, seven agreed to the principle of operating on the basis of a colleague's recommendation. When such a system was proposed in the Birmingham ophthalmology unit, for cataract surgery, most of the consultants had reservations.
In our experience, as in Birmingham, nearly all patients are happy with the system when it is explained to them that their wait will be shorter and that the operation can be carried out by any appropriately trained neurosurgeon. The general practitioners have not been formally consulted, but many were already referring patients to the department rather than a named specialist. The second hurdle to be surmounted was agreement on which patients were appropriate for the pooled waiting list. The criteria include first-time referrals, clear-cut signs or symptoms of cervical or lumbar neural compromise, and no obvious underlying disease that might require spinal fixation (e.g. rheumatoid arthritis). It was therefore agreed that the generic list should only incorporate patients who needed non-complex spinal surgery of the sort practised by all neurosurgeons. The reason this system has been so successful in our unit is the previous disparity between the waiting times for our various consultants. This allowed reallocation of the longest waiters to the consultants with the shortest lists. A disadvantage of the generic waiting list is the occasional difference of opinion between consultants on the need for treatment. Consultants are operating on patients they have not assessed in an outpatient clinic. We know of only one case, thus far, in which a consultant declined to perform the listed operation. The consultant who originally listed the patient performed the operation on the same admission. The system relies on good communication and flexibility at consultant level.
Disadvantages of these innovations include difficulties in the initial set up, a modest increase in secretarial workload and an occasional lack of continuity of care at consultant level. The great advantage of these schemes is that they are cost neutral but effective in helping to meet government targets. Clearly, waiting times are not a measure of what matters most—namely, clinical outcome. An ideal system would preserve continuity of care, but strategies of this sort are likely to be increasingly applied in the target-driven NHS.
Acknowledgments
We acknowledge the invaluable contributions made by Dawn Wood (Assistant Service Manager for Neurosciences) and Gemma Halliday (Neurosurgical Secretary).
References
- 1.Department of Health. The NHS Plan: A Plan for Investment, a Plan for Reform. Norwich: Stationery Office, 2000
- 2.Ramchandani M, Mirza S, Sharma A, et al. Pooled cataract waiting lists: views of hospital consultants, general practitioners and patients. J R Soc Med 2002;95: 598–600 [DOI] [PMC free article] [PubMed] [Google Scholar]