Age-related macular degeneration (ARMD) is the most common cause of irreversible central visual loss in the elderly populations of the industrialized world,1-3 and will place increasing demands on health services as people live longer. For many years, the only treatment proven to be effective in arresting the progression of the wet form of ARMD was laser photocoagulation.4 Even then, only a small proportion of patients within a specific disease subgroup have been shown to benefit from this treatment, and the rate of disease recurrence (paradoxically often under the fovea) is high.5 Lately, researchers have developed novel strategies based on improved understanding of the pathophysiology, and this article summarizes recent advances in treatment.
DISEASE CLASSIFICATION
ARMD is probably a polygenic disease affected by multiple environmental factors. This may account for the wide range of phenotypes. Customarily, it is classified into a dry or atrophic form (Figure 1) and a wet or neovascular form (Figure 2). The dry form of disease is characterized by the slow progressive atrophy of macular retinal pigment epithelium and the underlying choroid, leading to secondary photoreceptor death. The wet form is characterized by new blood vessel growth from the inner choroid, stimulated by a vascular endothelial growth factor, through defects in Bruch's membrane to the potential space underneath the retinal pigment epithelium and retina. These new vessels are associated with massive exudation of fluid and lipid, which severely damages the photoreceptors.6 On fluorescein angiography the neovascularization may be graded as classic, occult or mixed6 (Figure 3)—a classification that is helpful for prognostic purposes and for subgroup analysis in clinical trials, since the natural history seems to differ between subtypes.
Figure 1.
Fundus photograph showing atrophic or dry age-related macular degeneration. Note the well demarcated area of central retinal, retinal pigment epithelium and choroidal atrophy revealing the pale underlying sclera. Colour version available on [www.jrsm.org]
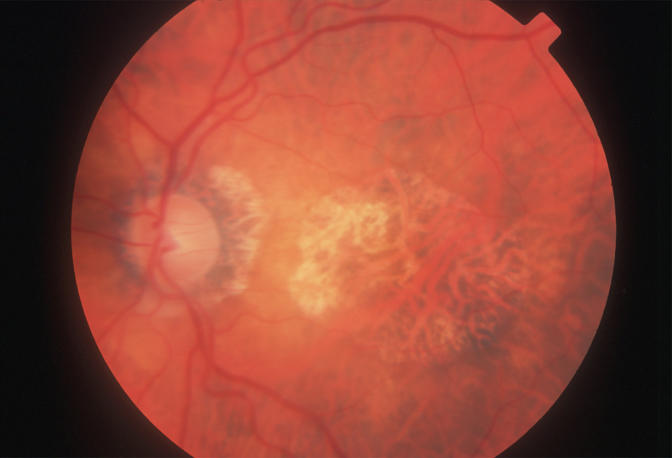
Figure 2.
Fundus photograph showing extensive wet age-related macular degeneration. Note the large central area of retinal elevation surrounded by retinal haemorrhages and lipid exudates. Colour version available on [www.jrsm.org]
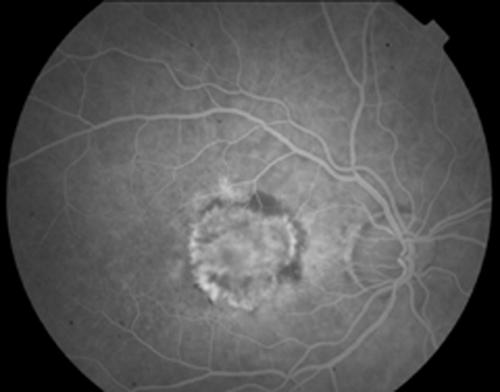
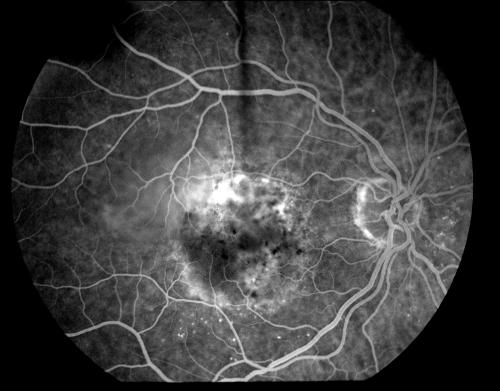
Figure 3.
Fundus fluorescein angiogram showing marked central leakage (bright white area) from a subfoveal lesion classified as classic with occult (a) at presentation and (b) three months after photodynamic therapy. Note that the central area of leakage is much reduced in (b) denoting closure of the choroidal neovascular membrane
ANTIOXIDANT SUPPLEMENTATION
For established dry ARMD, no treatment has been proven effective by randomized trial. However, subgroup analysis of a multicentre randomized placebo-controlled trial (AREDS trial) suggested that progression to advanced disease can be reduced in high-risk patients by daily supplements of vitamins C (500 mg) and E (400 IU), zinc (80 mg) and beta carotene (15 mg).7 This approach was based on the hypothesis that free radicals are involved in pathogenesis and that oxidative damage to the retina might be prevented by antioxidant supplements.8,9 On the basis of these results the AREDS research group recommend that persons older than 55 years should have dilated eye examinations to determine their risk of developing advanced ARMD; then, those with high-risk characteristics (Box 1) or with vision loss due to advanced ARMD in one eye, and without contraindications such as smoking, should consider taking supplements of antioxidants plus zinc.
Box 1.
Established risk factors for age-related macular degeneration
| Relative risk | |
|---|---|
| Age | — |
| Smoking | 3.6 |
| Large drusen | 5.7 |
| Soft drusen | 9.9 |
PHOTODYNAMIC THERAPY
Before 1999, the only treatment proven by randomized controlled trial to provide long-term visual benefit in wet ARMD (subfoveal choroidal neovascularization) was laser photocoagulation.10 Unfortunately, the treatment is associated with an immediate and dramatic drop in Snellen visual acuity of up to 6 lines—a consequence that most patients and their ophthalmologists are not prepared to accept, so uptake has been low. In current photodynamic therapy (PDT), a photosensitizer (verteporfin) is injected intravenously and the neovascular lesion is then irradiated with a diode laser (689 nm) for 83 seconds. The excited photosensitizer generates free radicals which, by damaging vascular endothelium, cause thrombosis within the irradiated vessels.11
In 1999, initial results from the TAP trial indicated that, after twelve months' follow-up, the proportion of patients losing fewer than 15 letters on a standard visual acuity chart (which corresponds to about three lines or less) was 67% with verteporfin PDT and 39% with placebo.12 At twenty-four months this advantage was maintained, the difference being 59% versus 31%.13 Since the occluded vasculature commonly recanalized, patients required an average of 5.6 treatments in the twenty-four months of the study, though most of these were in the first year. An open-label extension of the study indicated that visual acuity was stable during the third year14—but, as the authors point out, this result must be treated with caution since only one-third of the original group could be examined at thirty-six months. In a second large multicentre study (Verteporfin in Photodynamic therapy or VIP), confined to patients with pure ‘occult’ choroidal neovascular lesions, the proportion of patients losing fewer than 15 letters on the visual acuity chart was 45% in the PDT group and 32% in the placebo group.15 Overall, the TAP and VIP investigations have shown significant benefit from PDT in patients with predominantly classic or pure occult subfoveal neovascularization.
On the basis of numbers needed to treat (NNT), PDT is one of the most effective treatments in medicine. Only 3.6 patients have to be treated to prevent one case of moderate visual loss (15 letter loss on the visual acuity chart).16 This can be compared with the use of topical antibiotics for treatment of acute bacterial conjunctivitis (NNT=6) or of warfarin for the prevention of stroke in non-rheumatic atrial fibrillation (NNT=18). However, despite the good clinical results, the expense of PDT makes it poorly cost-effective.17,18 The cost/quality adjusted life year (QALY) for this treatment has been calculated at £60 000 to £122 000 and the cost utility from £151 000 to £182 000.18
The National Institute for Clinical Excellence (NICE) has recently issued guidance for the use of PDT in the treatment of wet ARMD [www.nice.org.uk]. PDT is recommended for patients with ‘classic’ lesions (no occult) in whom the best corrected visual acuity is 6/60 or better. Patients with lesions classified as predominantly classic in nature may also be treated, but only as part of an ongoing or new clinical trial.
MACULAR RELOCATION SURGERY
Macular translocation surgery is a technique currently undergoing evaluation as an alternative to photodynamic therapy or laser photocoagulation for subfoveal choroidal neovascular membranes (CNV). The underlying principle of the surgery is to relocate the neuroretina of the fovea away from the underlying CNV to an area of healthy retinal pigment epithelium and choroid. The techniques are various but all involve a subtotal vitrectomy followed by a partial or total retinal detachment. The neurosensory retina can then be moved relative to the underlying retinal pigment epithelium either by rotation/displacement or by scleral shortening. The retina is reattached in its new position away from the CNV, which is then destroyed by laser photocoagulation. Although the technique is not yet widely practised in the UK, studies in selected patients have yielded promising results. One-year follow-up on 102 eyes treated with limited macular translocation indicated improvement (two or more lines on the Snellen chart) in 39%.19 A second series of 90 patients followed for twelve months showed at least 15 letters' improvement in visual acuity in 24 (27%); 37 were stable and 29 deteriorated.20 No long-term follow-up is yet available, but this technique does seem to offer hope of visual improvement—unlike photodynamic therapy, which at best aims to stabilize. A drawback is that such major surgery carries a risk of complications—including proliferative vitreoretinopathy (19%), retinal detachment (12-23%), macular hole formation (9%)—that can lead to loss of both central and peripheral vision.
Since ARMD is a common disease, there is scant prospect of macular translocation surgery being made available to more than a small fraction of patients who might benefit. Furthermore, the recurrence rate is high. There is a need, therefore, for further randomized controlled studies to identify the subgroups of patients who have most to gain from limited surgical resources.
TRANSPUPILLARY THERMOTHERAPY
Transpupillary thermotherapy employs an infrared diode laser whose emission is taken up predominantly by the melanin granules of the retinal pigment epithelium and choroid. The resultant localized heating effect has been used to treat choroidal melanomas and to close vascular channels in choroidal neovascular membranes while leaving the overlying retina relatively intact. Several small short-term studies have yielded promising results in occult choroidal neovascularization.21 In an uncontrolled pilot study, 59% of eyes with predominantly occult disease had lost fewer than 15 letters at twelve months' follow-up22—an encouraging result since this subgroup of patients gain little from photodynamic therapy. A large randomized prospective clinical trial, the TTT4CNV trial, is now underway.
PHARMACOLOGICAL INHIBITION OF ANGIOGENESIS
It has become clear that, in the pathogenesis of choroidal neovascularization, endothelial growth factor (VEGF) plays a key role. Several pilot studies are now underway to test the effects of selectively inhibiting intraocular VEGF or pharmacologically altering its action. These treatments include intravitreal injection of an anti-VEGF aptamer (Eyetech study) or humanized anti-VEGF monoclonal antibody (RhuFab V2).23 The aptamer is a small stable RNA-like molecule that binds with high affinity to VEGF. Both the aptamer and the humanized antibody effectively bind and inhibit the action of VEGF, thereby reducing the drive for intraocular angiogenesis and increased vascular permeability.24 Another approach is to inject an anti-angiogenic steroid, either periocularly (anecortave acetate) or intravitreally (triamcinolone acetonide). These steroid molecules have potent inhbitory effects on angiogenesis and vascular permeability with the advantage of negligible glucocorticoid and mineralocorticoid actions. They are thought to work by modification of endothelial cell adhesion and cell junction molecules. Clinical results are at present sparse, but in the phase II Eyetech study (21 patients) intravitreal anti-VEGF aptamer was well tolerated and a quarter of the eyes showed three lines or more visual improvement.24 In a study of 128 eyes (predominantly classic choroidal neovascularization), vision was preserved at twelve months in 84% receiving periocular injections of anecortave acetate compared with 50% of those receiving placebo.25 A single intravitreal injection of triamcinolone acetonide had no effect on the risk of severe visual loss during the first year of follow-up, despite a significant reduction in the size of the choroidal neovascular membrane within three months.26
Box 2 Ongoing research
VER Study—photodynamic therapy using verteporfin with six-weekly retreatments. Aim is to improve treatment efficacy by more sustained and early neovascular membrane closure
VIO Study—photodynamic therapy using verteporfin in occult choroidal neovascularization
VIM Study—photodynamic therapy study using verteporfin in minimally classic choroidal neovascularization
TTT4AMD—large multicentre randomized placebo controlled trial evaluating transpupillary thermotherapy
Choroidal Neovascularization Prevention Trial (CNVPT)—multicentre, randomized controlled trial to study the effect of retinal laser photocoagulation on the resolution of drusen
MARAN and SST trials—international multicentre prospective randomized controlled trials of macular relocation compared with natural history.
CONCLUSIONS
Until lately, the outlook for patients with age-related macular degeneration was bleak; few were eligible for treatment with conventional laser photocoagulation. The novel treatments reviewed in this article, though not curative, offer at least the hope of visual stabilization. Many of these treatments are now being assessed in large international multicentre trials (Box 2).
References
- 1.Klein R, Klein BEK, Linton KLP. Prevalence of age related maculopathy, The Beaver Dam Eye Study. Ophthalmology 1992;99: 933-43 [DOI] [PubMed] [Google Scholar]
- 2.Mitchell P, Smith W, Attebo K, Wang JJ. Prevalence of age related maculopathy in Australia. Ophthalmology 1995;102: 145060. [DOI] [PubMed] [Google Scholar]
- 3.Vingerling JR, Dielemans I, Hofman A, et al. The prevalence of age-related maculopathy in the Rotterdam study. Ophthalmology 1995; 102: 205-10 [DOI] [PubMed] [Google Scholar]
- 4.Macular Photocoagulation Study Group. Argon laser photocoagulation for neovascular maculopathy: five-year results from randomised clinical trials. Arch Ophthalmol 1991;109: 1109-14 [PubMed] [Google Scholar]
- 5.Macular Photocoagulation Study Group. Recurrent choroidal neovascularisation after argon laser photocoagulation for neovascular maculopathy. Arch Ophthalmol 1986;104: 503-12 [DOI] [PubMed] [Google Scholar]
- 6.Chopdar A, Chakravarthy U, Verma D. Age related macular degeneration. BMJ 2003;326: 485-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.A randomised, placebo-controlled clinical trial of high dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss. AREDS report No 8. Arch Ophthalmol 2001;119: 1417-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Young RW. Solar radiation and age related macular degeneration. Surv Ophthalmol 1988;32: 252-69 [DOI] [PubMed] [Google Scholar]
- 9.Beatty S, Koh H, Phil M, Henson D, Boulton M. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol 2000;45: 115-34 [DOI] [PubMed] [Google Scholar]
- 10.Macular Photocoagulation Study Group. Laser photocoagulation of subfoveal neovascular lesions of age related macular degeneration: updated findings from two clinical trials. Arch Ophthalmol 1993; 111: 1200-9 [DOI] [PubMed] [Google Scholar]
- 11.Sickenberg M, Schmidt-Erfurth U, Miller JW, et al. A preliminary study of photodynamic therapy using verteporfin for choroidal neovascularisation in pathologic myopia, ocular histoplasmosis syndrome, angioid streaks, and idiopathic causes. Arch Ophthalmol 2000;117: 327-36 [DOI] [PubMed] [Google Scholar]
- 12.Photodynamic therapy of subfoveal choroidal neovascularisation in age related macular degeneration with verteporfin. One year results of 2 randomised clinical trials—TAP report 1. Arch Ophthalmol 1999;117: 1329-45 [PubMed] [Google Scholar]
- 13.Photodynamic therapy of subfoveal choroidal neovascularization in age related macular degeneration with verteporfin. Two year results of 2 randomised clinical trials—TAP report 2. Arch Ophthalmol 2001;119: 198-207 [PubMed] [Google Scholar]
- 14.Photodynamic therapy of subfoveal choroidal neovascularization in age related macular degeneration with verteporfin. Three year results of an open label extension of 2 randomised clinical trials—TAP report No 5. Arch Ophthalmol 2002;120: 1307-14 [DOI] [PubMed] [Google Scholar]
- 15.Verteporfin therapy of subfoveal choroidal neovascularization in age related macular degeneration: two-year results of a randomised clinical trial including lesions with occult with no classic choroidal neovascularisation—verteporfin in photodynamic therapy report 2. Am J Ophthalmol 2001;131: 541-60 [DOI] [PubMed] [Google Scholar]
- 16.Sharma S. Update in retina: photodynamic therapy for the treatment of subfoveal choroidal neovascularisation secondary to age related macular degeneration. Can J Ophthalmol 2001;36: 7-10 [DOI] [PubMed] [Google Scholar]
- 17.Sharma S, Brown GC, Brown MM, Hollands H, Shah GK. The cost-effectiveness of photodynamic therapy for fellow eyes with subfoveal choroidal neovascularisation secondary to age-related macular degeneration. Ophthalmology 2001;108: 2051-9 [DOI] [PubMed] [Google Scholar]
- 18.Meads C, Sales C, Roberts T, Moore D, Fry-Smith A, Hyde C. Clinical Effectiveness and Cost Utility of Photodynamic Therapy for Wet Age-related Macular Degeneration. Birmingham: West Midlands Technology Assessment Group, University of Birmingham, 2002 [DOI] [PubMed]
- 19.Fujii GY, De Juan E, Pieramici DJ, et al. Inferior limited macular translocation for subfoveal choroidal neovascularisation: 1-year visual outcome and recurrence report. Am J Ophthalmol 2002;134: 69-74 [DOI] [PubMed] [Google Scholar]
- 20.Aisenbrey S, Lafaut B, Szurman P, et al. Macular translocation with 3608 retinotomy for exudative age related macular degeneration. Arch Ophthalmol 2002;120: 451-9 [DOI] [PubMed] [Google Scholar]
- 21.Ciulla TA. Recent advances in the treatment of exudative age related macular degeneration, including transpupillary thermotherapy. Acta Ophthalmol Scand 2003;81: 103-4 [DOI] [PubMed] [Google Scholar]
- 22.Algvere PV, Libert C, Lindgarde G, Seregard S. Transpupillary thermotherapy of predominantly occult choroidal neovascularisation in age related macular degeneration with 12 months follow-up. Acta Ophthalmol Scand 2003;81: 110-17 [DOI] [PubMed] [Google Scholar]
- 23.Krzystolik MG, Afshari MA, Adamis AP, et al. Prevention of experimental choroidal neovascularisation with intravitreal anti-vascular endothelial growth factor antibody fragment. Arch Ophthalmol 2002;120: 338-46 [DOI] [PubMed] [Google Scholar]
- 24.The Eyetech Study Group. Anti-vascular endothelial growth factor therapy for subfoveal choroidal neovascularisation secondary to age related macular degeneration, phase II study results. Ophthalmol 2003;110: 979-86 [DOI] [PubMed] [Google Scholar]
- 25.The Anecortave Acetate Clinical Study Group. Anecortave acetate as monotherapy for treatment of subfoveal neovascularisation in age related macular degeneration: twelve-month clinical outcomes. Ophthalmology 2003;110: 2372-85 [DOI] [PubMed] [Google Scholar]
- 26.Gillies MC, Simpson JM, Luo W, et al. A randomised clinical trial of a single dose of intravitreal triamcinolone acetonide for neovascular age related macular degeneration. Arch Ophthalmol 2003;121: 667-73 [DOI] [PubMed] [Google Scholar]