Abstract
Introduction:
One of the most important complications of stroke after intracranial haemorrhage surgery is impaired quality of life. This study was conducted to determine the impact of spiritual care on the quality of life of stroke patients.
Methods:
This single-blind clinical trial with a pre-test and post-test design was conducted on 100 stroke patients. Participants were recruited and randomly assigned to a control group and an intervention group. The stroke-specific quality of life (SS -QoL) scale was used to assess the quality of life of stroke patients. The intervention group received four sessions of spiritual care.
Results:
The independent t-test showed no significant difference between the two groups in the mean quality of life score (t=−0.120, P=0.281) and its dimensions before the intervention. However, after the intervention, the results showed a significant difference between the two groups in terms of the mean quality of life score (t=1.984, P<0.001) and its dimensions. In addition, the results of the paired t-test showed that in the intervention group, the mean score of quality of life (t=5.161, P<0.001) and its dimensions were significantly different before and after the intervention. Furthermore, the results showed that before and after the intervention in the control group, the mean score of quality of life (t=1.109, P=0.614) and its dimensions were not significantly different.
Conclusions:
Based on this results, the authors strongly recommend the use of spiritual care as a holistic care and complementary method to improve the symptoms and quality of life of stroke patients.
Keywords: clinical trial, quality of life, spiritual care, stroke
Introduction
Highlights
Surgical intervention plays a critical role in the management intracranial haemorrhage.
Impaired quality of life is one of the most important complications of intracranial haemorrhage.
Spiritual care can improve the symptoms and quality of life of stroke patients.
Stroke is a clinical syndrome characterized by localized neurological defects and is often classified as a chronic debilitating disease. It involves a sudden reduction in cerebral blood flow due to haemorrhage and interruption of blood vessels entering the brain1. Moreover, this process of insufficient oxygen supply leads to brain tissue being damaged or even destroyed2. The patient suddenly falls into a state of coma and stupor that lasts for hours or even days and is often accompanied by paralysis of half of the body and face and involuntary urination and defecation1. Stroke is the third leading cause of death worldwide after heart disease and cancer, accounting for ~10% of all deaths3. In Iran, the annual incidence of stroke is 139 persons per hundred thousand for the first time, much higher than in most Western countries4. Of the total population affected by stroke, 30–40% who survive the attack suffer severe disability. The severity and variety of these conditions depend on the location and extent of the lesion and the type of artery involved1.
Surgical intervention plays a critical role in the management of certain cases of intracranial haemorrhage (ICH), particularly when there is evidence of significant mass effect or imminent brain herniation2. The goal of surgical treatment in these patients is to reduce intracranial pressure, control bleeding, and ultimately preserve brain function. Several surgical techniques, including craniotomy, haematoma evacuation, and decompressive hemicraniectomy, have been employed to achieve these objectives4. However, the decision to proceed with surgery in ICH patients requires careful consideration of various factors, including the origin and characteristics of the haemorrhage, patient comorbidities, and neurosurgical expertise3. While surgery can offer life-saving benefits, the selection of appropriate candidates and the timing of intervention remain crucial for optimizing outcomes in intracranial haemorrhage patients5.
Complications of this disease include: Impaired balance and posture, loss of strength, impaired movement, impaired gait, impaired sensation, impaired quality of life, with the most common complication being hemiparesis or hemiplegia1–5. The occurrence of this disease is an unpredictable and devastating event for the patient and his or her family and is considered a family disease, so the life of the patient and his or her family after a stroke becomes a condition that does not return to the pre-stroke situation6. Since stroke leads to physical, functional, and psychological changes in a person’s life, it is now considered as one of the most serious health problems7. In fact, stroke leads to changes in people’s lifestyles that ultimately affect their quality of life and satisfaction. This is because the complications of stroke affect various aspects of quality of life, including psychological, physical, social, economic, family, and sexual aspects8.
Quality of life is a complex and broad concept characterized by a person’s sense of satisfaction and happiness. A person who feels satisfied with his or her life spends more energy taking care of him or herself, which makes him or her healthier and, as a result, has a better quality of life, which perpetuates this cycle9. Quality of life is a multidimensional intrinsic factor that is a combination of cognitive and emotional factors. The issue of quality of life is important because if ignored, it can lead to frustration, lack of motivation for any effort, and limitation of social, economic, cultural, and health activities, and in a deeper dimension, it can affect the socioeconomic development of a country10. Education of these patients by nurses not only informs patients about their disease but also prevents them from misbehaving. Otherwise, they might increase the severity of their disease and decrease their quality of life11.
Supporting the patient in various physical and psychological aspects is one of the crucial and important roles of nurses12. The WHO believes that health includes the four dimensions of physical, mental, social, and spiritual health that nurses should treat and care for13. At the same time, it highlights the role of nurses in creating a safe and appropriate environment, because by considering spiritual contexts for patients and their companions, they can create opportunities for spiritual care14 and contribute significantly to restoring the quality of life of these patients15. Nurses can help patients achieve a full recovery by using a holistic approach to care with an emphasis on the spiritual dimension of care16.
Spiritual care is a holistic approach to addressing the spiritual needs, values, and beliefs of individuals, recognizing and respecting their diverse perspectives. It involves providing support, guidance, and companionship to individuals in their spiritual journey, fostering a sense of meaning, purpose, and connection. Spiritual care can encompass religious practices, existential exploration, inner reflection, and the cultivation of compassion, hope, and resilience17. Spiritual care is care that recognizes and addresses the psychological and spiritual needs of individuals as they cope with trauma, illness, or anxiety18. Spiritual care is an integral component of nursing care, and most nursing models emphasize a holistic approach, but evidence suggests that the spiritual care domain is often overlooked in hospitalized patients17. Meeting the spiritual needs of hospitalized patients is extremely important for recovery time, achieving mental health, and improving quality of life19. Moreover, this issue is of particular importance in the ICU20. Spiritual care provides emotional support and helps patients find meaning and purpose, aiding in coping with distressing experiences. Moreover, spiritual care assists patients in reconnecting with their values, beliefs, and purpose, fostering a positive outlook and motivation for recovery18. In addition, spiritual care connects patients with religious or spiritual communities, offering social support and reducing isolation19. Also, spiritual care promotes acceptance, inner peace, and contentment despite physical limitations or challenges. Spiritual care recognizes the holistic nature of patients, addressing physical, emotional, social, and spiritual dimensions, leading to overall well-being20. By incorporating spiritual care into patient-centred and culturally sensitive approaches, healthcare providers can improve the quality of life for patients with ICH19.
Given numerous inconsistencies in the relationship between spirituality and quality of life in research conducted abroad21,22,23, the interactions of stroke on the spiritual dimension of patients and vice versa, the lack of internal research evidence in the field of spiritual intervention in patients with stroke, and to consider the improvement of patients’ quality of life as a criterion for stroke treatment, this study aimed to determine the effect of spiritual care on the quality of life of patients with stroke.
Methods
Research design
A single-blinded, parallel-group, randomized controlled trial was designed to achieve the research objectives. The work has been reported in line with the CONSORT criteria. CONSORT flow diagram of entering subjects in the study groups has shown in Figure 1. The CONSORT 2010 checklist was used to ensure the quality of reporting in this study24.
Figure 1.
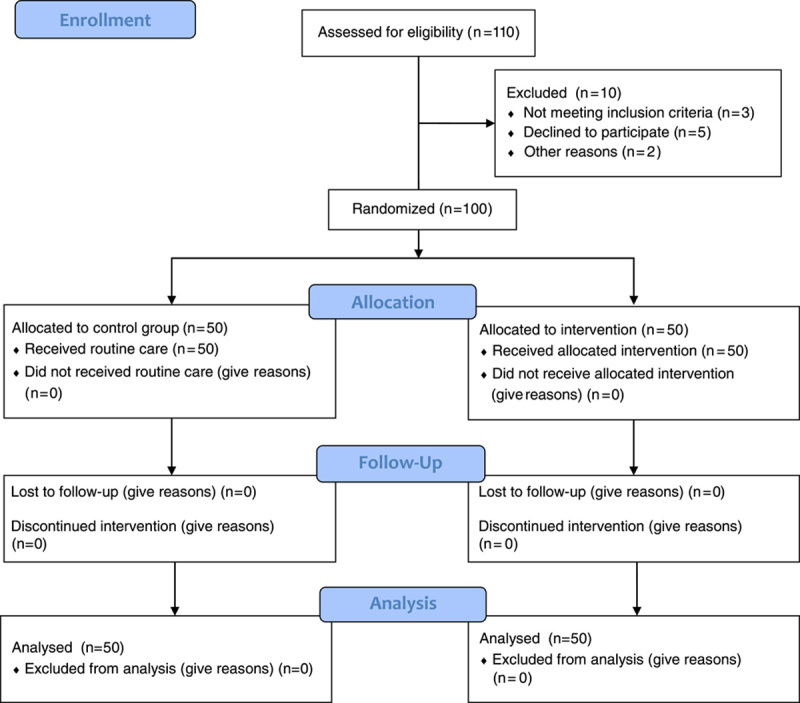
Research flow diagram.
Participants and sample
The study was conducted in REDACTED. After approval of the plan by the Research Council of REDACTED School of Nursing & Midwifery and obtaining a research license from the College Ethics Committee and registration in the REDACTED Clinical Trials Registry, REDACTED was assigned to select the samples. The sample size was calculated using G power statistical software. Following the study by Beinotti et al.25. and based on a confidence interval of 95% and power of 80%, the minimum sample size for each group was set at 45 patients.
The final sample size was 50 patients for each group and 100 patients for both the intervention and control groups to account for an attrition rate of 10%, which were selected based on random sampling. Participants were randomly assigned to two groups, the intervention group and the control group. Inclusion criteria were (a) willingness to participate in the study, (b) undergoing craniotomy at least three months ago, (c) signing of written informed consent, (d) no severe visual or hearing impairment, (e) no mental disorder, (f) ability to care for self and pass more than 48 hours after stroke onset, (g) age between 18 and 60 years. Exclusion criteria were (a) withdrawal from the study for any reason, (b) occurrence of health disorders for any reason during the study, (c) death if any of the selected participants did not want to participate in the study, and the next person was randomly selected and replaced.
In providing spiritual care to patients with ICH, it is crucial to recognize that people’s spiritual needs can indeed vary significantly. To ensure effective and individualized spiritual interventions, a need assessment should ideally be conducted before implementing any specific interventions. This assessment allows healthcare providers to understand the unique spiritual needs, beliefs, and preferences of each patient. A comprehensive spiritual needs assessment involves open and empathetic communication with the patient, allowing them to express their thoughts, fears, hopes, and beliefs regarding their spirituality. It may include exploring religious or spiritual affiliations, discussing personal values and beliefs, evaluating the impact of the illness on their spiritual well-being, and understanding any specific requests or rituals they may desire. By conducting a need assessment, healthcare providers can tailor spiritual interventions to meet the specific requirements of each patient, respecting their individuality and cultural background. This approach acknowledges that spiritual care is highly personal and should be delivered in a manner that aligns with the patient’s beliefs and values. Offering the same intervention to all patients without considering their unique spiritual needs can be inadequate and may not effectively address their concerns. Therefore, healthcare providers should strive to provide patient-centred care, taking into account the diversity of spiritual needs and preferences among individuals.
Data collection
In this study, the data collection instruments consisted of the demographic questionnaire and the stroke-specific quality of life (SS-QoL) scale. The demographic questionnaire included age, sex, education, material status, place of residence, and medical history. The SS-QoL was used to assess the quality of life of patients with stroke. This questionnaire was developed by Post et al. In the study by Post et al. 26 the Cronbach’s alpha coefficient for the scale was reported to be 0.70. This questionnaire consists of 12 items, each representing a major dimension of the 12 dimensions of SS-QOL, which include self-care, mobility, upper limb function, speech (language), vision, work, thinking, family roles, social roles, personality, mood, and energy. These 12 dimensions are divided into two groups, physical and psychosocial. The minimum score was 12 and the maximum score was 60, with higher scores indicating better quality of life26. In Iran, Mahmoodi et al. 27 developed the Persian version of this questionnaire using the cross-cultural adaptation with preserving the original structure. Test and re-test method was used to confirm the reliability of the questionnaire. We asked 60 patients to complete the questionnaire. Then, they took another test in the same condition three days later. The scores obtained from the two tests were used to measure the correlation coefficient (r=0.91) and the alpha (a=0.821).
Intervention
The researcher first introduced himself to the samples who met the inclusion criteria, informed them of the research objectives, and then obtained informed consent at the first session. Participants were randomly divided into two groups: the intervention group and the control group. The intervention group was informed that they were not allowed to share information with the control group and other patients so as not to jeopardize the objectives of the study. In this study, random assignment and concealment were implemented to ensure unbiased and reliable results. In this phase, participants were assigned to the control group (n=50) and the intervention group (n=50) by random sequence generation (Fig. 1). The allocation was done by asking patients to choose one of the two cards (C: control group), (G: intervention group), which were in opaque sealed envelopes. The participant who chose (C) or (G) was placed in the control or intervention group, respectively. This approach prevented researchers and participants from influencing or predicting group assignments, minimizing selection biases. The utilization of random assignment and concealment enhances the internal validity of the study, ensuring comparability between groups and strengthening the causal relationship between the intervention and outcomes. Before the intervention, the demographic questionnaire and the SS-QOL were completed by the control and intervention groups. The questionnaires were anonymous, and patients were assured that the information would remain confidential. Patients participated in the study after discharge from the hospital for spiritual care in the intervention group. Four spiritual care sessions were held in the intervention group (Table 1). Each session lasted one hour. In this study, the training provided to the patients was primarily conducted through face-to-face interactions. This approach involved direct, one-on-one communication between the healthcare providers/researchers and the patients.
Table 1.
Content of spiritual care training sessions.
| First session (present supportive system) | During the first 2 days of hospitalization, the patients were taught about the purpose of the study, the method of implementation and spiritual care. This training was in person and on the patient’s bed and lasted about an hour. Moreover, patients’ questions about spiritual self-care were answered. The following actions were taken in this meeting: 1. Create trust, empathy and honesty between the nurse and the client to establish a proper relationship 2. Listen carefully and attentively to the patient’s words, patients’ worries and anxieties 3. Provide psychological support to patients 4. Strengthen the hope and inner strength of people 5. Use of positive energy sentences accompany by strengthening healthy and constructive thinking 6. Establish verbal and non-verbal communication with the patient 7. Answer the patient’s questions and explaining the treatment process, also giving information and awareness to patients about the disease in order to reduce physical and mental stress. 8. Encourage patients to use recreational and scenic spaces and perform sports activities according to the physician |
| Second session (supporting the patients religious rites) | This session was performed on the patient’s bed for one hour and included the following: 1. Help the client to find the meaning and concept of life and paying attention to the fact that none of the life events is outside of divine destiny 2. Provide the necessary facilities to perform religious acts 3. Encourage the patient to recite the religious beliefs 4. Encourage the patient to express his or her religious beliefs 5. Encourage patients to refer to religious clerics |
| Third session (using supportive systems ) | 1. Encourage patients to refer to people with whom they can feel comfortable 2. Emotional support of patients by companions and medical staff 3. Advise the patient’s companions to help the patient to perform their normal and daily responsibilities such as doing housework 4. Encourage the patient to be present at work |
| Fourth session ( summary) | Patients The training material was summarized during the last three sessions and were asked to express their opinion and question about the spiritual care provided. In case of any ambiguity in the field of education provided. Attempts were made to resolve the ambiguity |
It should be noted that spiritual self-care can include various methods, such as meditation, relaxation, yoga, prayer, spending time in nature, keeping the environment clean, communicating with the community, practicing silence, and learning. However, this study used the methods that were applicable to the patients. Therefore, the main axis of the spiritual self-care program includes the above items. In this study, spiritual care was provided individually and twice a week during morning or afternoon shifts at the patient’s private residence. The patient’s or companion’s landline and cell phone numbers were recorded to follow up and ask any questions about the illness. The control group was not trained, but was provided with the training material after the study. One month after the intervention, the SS-QOL was completed by both the intervention and control groups.
Analysis of the data
The Kolmogorov-Smirnov test was used to determine the normal distribution of the data. The researcher who was blinded to the data performed the analysis (single-blinded). All data were entered into IBM SPSS Statistics 25.0 and analyzed using descriptive (frequency and percentage for qualitative variable analysis, mean and standard deviation for normal quantitative variables) and analytical statistics (χ2 and Fisher’s Exact Test). The t-test for independent samples was used to compare the two groups. Finally, we used the paired samples t-test to compare the mean within groups.
Results
Demographic characteristics
The results showed that the mean age of participants in the control group was 38.32±11.12 years and in the intervention group was 39.14±12.22 years. In addition, most of the participants in the two groups were male and married. Furthermore, the educational level of the majority of the participants was at the college level. It should be noted that the majority of the participants were from the city and more than half of the participants in both groups smoked. The results also showed that there was no statistically significant difference between the two groups in terms of gender, education level, marital status, employment, residence, and smoking (P>0.05). However, there was a statistically significant difference in terms of mean age between the two groups (P=0.01) (Table 2).
Table 2.
Comparison of demographic characteristics of the patients in the study groups.
| Groups | |||
|---|---|---|---|
| Variables | Control, n (%) | Intervention, n (%) | Results |
| Sex | |||
| Male | 27 (54) | 26 (52) | X=0.148 df=1 a P=0.701 |
| Female | 23 (46) | 2 4 (48) | |
| Education level | |||
| Elementary | 4 (8) | 4 (8) | X=4.055 df=3 a P=0.256 |
| Secondary | 10 (20) | 12 (24) | |
| High school | 12 (24) | 17 (34) | |
| University | 24 (48) | 17 (34) | |
| Marital status | |||
| Single | 16 (32) | 13 (26) | b P=0.397 |
| Married | 34 (68) | 37 (74) | |
| Occupation | |||
| Employed | 33 (66) | 3 2 (64) | X=0.784 df=2 a P=0.676 |
| Unemployed | 15 (30) | 14 (28) | |
| Inactive | 2 (4) | 4 (4) | |
| Residual status | |||
| Rural | 11 (22) | 15 (30) | X=1.123 df=1 a P=0.289 |
| Urban | 39 (78) | 35 (70) | |
| Smoking | |||
| Yes | 30 (60) | 33 (66) | b P=0.278 |
| No | 20 (40) | 17 (34) | |
| Age | Control | Intervention | t=2.610 df=98 c P=0.080 |
| Mean±SD1 | Mean±SD | ||
| 38.32±11.12 | 39.14±12.22 | ||
χ2 test.
Fisher’s exact test.
Independent sample t-test.
The quality of life
The independent t-test revealed no statistically significant difference between the two different groups before the intervention in the mean quality of life score (t=−0.120, P=0.281). The dimensions included self-care, mobility, upper limb function, speech (language), vision, work, thinking, family roles, social roles, personality, mood, and energy (Table 3). However, after the intervention, the results of the independent t-test showed a statistically significant difference between the two groups in the mean score of quality of life (t=1.984, P<0.001) and its dimensions (Table 4).
Table 3.
Comparison of the mean quality of life scores of the patients in the study groups before the intervention.
| Variable | Groups | |||
|---|---|---|---|---|
| Quality of life indicators | Control Mean±SD | Intervention Mean±SD | Result | Effect size (Cohen’s d) |
| Self-care | 12.03±1.38 | 12.13±0.95 | t=−0.627 df=98 a P=0.832 | 0.11 |
| Vision | 5.33±0.37 | 5.03±0.46 |
t=0.360 df=98 a P=0.719 |
0.23 |
| Language | 15.04±1.18 | 15.99±0.98 |
t=0.127 df=98 a P=0.532 |
0.06 |
| Mobility | 16.43±1.39 | 15.93±1.28 |
t=0.513 df=98 a P=0.659 |
0.08 |
| Work productivity | 5.13±0.44 | 44 5.32±0.38 |
t=−0.548 df=98 a P=0.874 |
0.21 |
| Upper extremity | 11.44±0.88 | 12.03±1.01 |
t=0.420 df=98 a P=0.658 |
0.17 |
| Thinking | 4.11±0.07 | 4.01±0.09 |
t=0.617 df=98 a P=0.992 |
0.02 |
| Personality | 5.22±0.36 | 5.03±0.33 |
t=0.320 df=98 a P=0.819 |
0.10 |
| Mood | 13.93±1.02 | 14.11±1.04 |
t=0.767 df=98 a P=0.850 |
0.14 |
| Family role | 7.13±0.37 | 6.93±0.35 |
t=0.910 df=98 a P=0.702 |
0.24 |
| Social role | 14.66±1.08 | 15.83±0.99 |
t=−0.677 df=98 a P=0.421 |
0.15 |
| Energy | 6.05±0.32 | 5.93±0.38 |
t=0.669 df=98 a P=0.532 |
0.18 |
| Quality of life | 116.5±7.47 | 118.54±8.24 |
t=−0.120 df=98 a P=0.281 |
0.13 |
Independent sample t-test.
Table 4.
Comparison of the mean quality of life scores of the patients in the study groups after the intervention.
| Groups | ||||
|---|---|---|---|---|
| Variables | Control Mean±SD | Intervention Mean±SD | Result | Effect size (Cohen’s d) |
| Self-care | 12.14±1.22 | 15.33±0.99 |
t=−4.223 df=98 a P<0.001 |
0.56 |
| Vision | 5.11±0.27 | 8.45±0.68 |
t=0.343 df=98 a P<0.001 |
0.86 |
| Language | 14.98±1.10 | 19.01±1.03 |
t=−0.322 df=98 a P<0.001 |
0.75 |
| Mobility | 16.45±1.42 | 18.77±1.32 |
t=−1.433 df=98 a P<0.001 |
0.68 |
| Work productivity | 5.10±0.38 | 7.98±0.44 |
t=−4.567 df=98 a P<0.001 |
0.87 |
| Upper extremity | 11.65±0.98 | 13.87±1.34 |
t=−3.068 df=98 a P<0.001 |
0.77 |
| Thinking | 4.23±0.11 | 6.55±0.48 |
t=−2.543 df=98 a P<0.001 |
0.63 |
| Personality | 5.18±0.39 | 8.04±0.41 |
t=0.873 df=98 a P<0.001 |
0.80 |
| Mood | 14.03±0.99 | 17.11±1.31 |
t=−2.113 df=98 a P<0.001 |
0.82 |
| Family role | 7.18± 0.41 | 9.12±0.76 |
t=2.190 df=98 a P<0.001 |
0.86 |
| Social role | 14.60±1.20 | 18.02±0.20 |
t=−3.003 df=98 a P<0.001 |
0.88 |
| Energy | 5.96±0.12 | 7.89±0.31 |
t=−1.031 df=98 a P<0.001 |
0.69 |
| Quality of life | 116.61±8.59 | 150.14±9.27 |
t=1.984 df=98 a P<0.001 |
0.73 |
Independent sample t-test.
The results of the paired t-test showed that in the intervention group, the mean score of quality of life (t=5.161, P>0.001) and its dimensions were statistically significant before and after the intervention. Additionally, the results of the paired t-test showed that before and after the intervention in the control group, the mean score of quality of life (t=1.109, P=0.614) and its dimensions were not statistically significant (Table 5).
Table 5.
comparison of the mean quality of life scores of the patients within the study groups before and after the intervention.
| Score before the intervention | Score after the intervention | ||||
|---|---|---|---|---|---|
| Variables | Groups | Mean±SD | Mean±SD | Result | Effect size (Cohen’s d) |
| Self-care | Intervention | 12.13±0.95 | 15.33±0.99 |
t=6.672 df=49 a P<0.001 |
1.10 |
| Control | 12.03±1.38 | 12.14±1.22 |
t=−1.360 df=49 a P=0.765 |
0.05 | |
| Vision | Intervention | 5.03±0.46 | 8.45±0.68 |
t=−0.331 df=49 a P<0.001 |
0.95 |
| Control | 5.33±0.37 | 37 5.11±0.27 |
t=1.176 df=49 a P=0.645 |
0.08 | |
| Language | Intervention | 15.99±0.98 | 19.01±1.03 |
t=−0.705 df=49 a P<0.001 |
1.07 |
| Control | 15.04±1.18 | 14.98±1.10 |
t=0.459 df=49 a P=0.648 |
0.04 | |
| Mobility | Intervention | 15.93±1.28 | 18.77±1.32 |
t=5.493 df=49 a P<0.001 |
1.13 |
| Control | 16.43±1.39 | 16.45±1.42 |
t=0.581 df=49 a P=0.564 |
0.12 | |
| Work productivity | Intervention | 5.32±0.38 | 7.98±0.44 |
t=0.230 df=49 a P<0.001 |
1.11 |
| Control | 5.13±0.44 | 5.10±0.38 |
t=0.510 df=49 a P=0.612 |
0.09 | |
| Upper extremity | Intervention | 12.03±1.01 | 13.87±1.34 |
t=−14.99 df=49 a P<0.001 |
0.98 |
| Control | 11.44±0.88 | 11.65±0.98 |
t=0.375 df=49 a P=0.709 |
0.11 | |
| Thinking | Intervention | 4.01±0.09 | 6.55±0.48 |
t=6.651 df=49 a P<0.001 |
0.73 |
| Control | 4.11±0.07 | 4.23±0.11 |
t=1.041 df=49 a P=0.302 |
0.06 | |
| Personality | Intervention | 5.03±0.33 | 8.04±0.41 |
t=6.069 df=49 a P<0.001 |
1.05 |
| Control | 5.22±0.36 | 5.18±0.39 |
t=0.065 df=49 a P=0.948 |
0.12 | |
| Mood | Intervention | 14.11±1.04 | 17.11±1.31 |
t=8.161 df=49 a P<0.001 |
0.63 |
| Control | 13.93±1.02 | 14.03±0.99 |
t=−1.259 df=49 a P=0.543 |
0.15 | |
| Family role | Intervention | 6.93±0.35 | 9.12±0.76 |
t=7.962 df=49 a P<0.001 |
1.13 |
| Control | 7.13±0.37 | 7.18±0.41 |
t=0.487 df=49 a P=0.618 |
0.14 | |
| Social role | Intervention | 15.83±0.99 | 18.02±0.20 |
t=3.121 df=49 a P<0.001 |
0.95 |
| Control | 14.66±1.08 | 14.60±1.20 |
t=−1.259 df=49 a P=0.216 |
0.13 | |
| Energy | Intervention | 5.93±0.38 | 7.89±0.31 |
t=2.902 df=49 a P<0.001 |
1.01 |
| Control | 6.05±0.32 | 5.96±0.12 |
t=0.447 df=49 a P=0.608 |
0.09 | |
| Quality of life | Intervention | 118.54±8.24 | 150.14±9.27 |
t=5.161 df=49 a P<0.001 |
1.10 |
| Control | 116.5±7.47 | 116.61±8.59 |
t=1.109 df=49 a P=0.614 |
0.08 |
Paired sample t-test.
Discussion
The aim of this study was to determine the effects of spiritual care on the quality of life of stroke patients. The results of the present study indicate that there was no statistically significant difference in demographic characteristics between the two groups. Therefore, it can be concluded that the significant difference in mean quality of life and its dimensions of self-care, mobility, upper limb function, speech (language), vision, work, thinking, family roles, social roles, personality, mood, and energy in the intervention group before and after the intervention was due to the positive effect of spiritual care. In fact, the implementation of spiritual care caused this significant difference between the two groups of control and intervention. Consistent with the results of our study, Chen and colleagues showed that spiritual care has a positive effect on the quality of life and spiritual well-being of patients with chronic diseases. They also concluded that health professionals can integrate spiritual care into routine palliative care28.
Another study by Sankhel and colleagues examined the impact of spiritual care on the quality of life of cancer patients in India, and the results showed that spiritual care training improves the quality of life of cancer patients. Finally, they concluded that spiritual care improves not only spiritual well-being but also the overall well-being of patients29, which is consistent with the findings of the present study.
In addition, Balboni et al. 30 showed that patients whose spiritual needs were fully supported by the medical team had a higher quality of life than patients who were not supported. Furthermore, Babamohammadi et al. 31 demonstrated that spiritual care based on a healthy heart pattern was effective on the quality of life of patients with myocardial infarction. In another study by Tajbakhsh et al. 32, results showed that in the intervention group, the patients’ stress decreased after spiritual and religious care, while in the control group, the mean stress score increased significantly.
This result is consistent with the present study. In addition, Mahdavi and colleagues (2015) showed that spiritual care can improve the quality of life of home caregivers of elderly people with Alzheimer’s disease. Therefore, its use is recommended for caregivers of Alzheimer’s disease patients33. In contrast to the results of the present study, the findings of Aviles et al. 34 showed that spiritually oriented interventions did not affect the quality of life and status of patients after admission to the intensive care unit Aviles et al. 34.
Moreover, Blumenthal et al. 35 showed that spiritually oriented interventions have no significant impact on health-related indicators after acute myocardial infarction such as mortality, readmission, and quality of life. The reasons for this difference can be considered in the significant impact of cultural factors, ethnicity, spiritual beliefs, and nationality, which can affect the results of the study. The results of the present study showed that the quality of life in the control group had a lower mean score than the intervention group after one month. Since no special intervention was performed in the control group and they received only routine nursing care, therefore, such a reduction in the quality-of-life score in the control group is expected. Numerous stressors in the life of patients with stroke, long-term physical problems, and widespread changes can increase the possibility of reduced quality of life, which should be considered by healthcare managers.
The differences in conclusions between this paper and other literature may stem from variations in study design, patient populations, intervention protocols, and contextual factors. Understanding the reasons behind these differences is important for interpreting the study’s findings. The reference value lies in contributing to the existing evidence base and highlighting the need for further research to consolidate knowledge in this area.
The innovation in spiritual care in this study lies in its application to stroke psychiatric care, addressing a gap in the literature. The contribution to clinical care is the introduction of a holistic approach that recognizes the importance of spirituality and evaluates its impact on psychiatric well-being. By expanding the understanding and practice of stroke care, this study offers insights that can enhance the quality of care provided to stroke patients and foster a more comprehensive and patient-centred approach.
One of the limitations of the present study was the participants’ differences and psychological conditions, which can affect the results of the study. The second limitation was the differences in the cultural, religious and spiritual beliefs of each patient, which could affect their quality of life. In addition, the present study was performed only in one hospital and on a limited number of patients with stroke, so similar researches in other centres with higher sample size should be conducted over a longer period of time. Moreover, another limitation of the study is the short follow-up period, which may restrict the ability to fully capture and evaluate the long-term effects of the spiritual care intervention on the quality of life of ICH patients. Thus, future research is recommended to investigate the long-term effects of the spiritual care intervention on the quality of life of ICH patients.
Conclusions
Nurses have a fundamental and important role in promoting the patients’ mental and physical health. In general, the findings of the present study confirm the effect of spiritual care on the quality of life in patients with stroke. Therefore, its use as a holistic care approach in improving the symptoms and quality of life of patients with stroke is recommended. It is also suggested that by conducting more studies, its use as a complementary approach in nursing care of patients with stroke should be investigated.
Ethics approval and consent to participate
The ethics committee of Urmia University of Medical Sciences approved the study (Ethical code: IR.UMSU.REC.1400.388). This study was registered in the Iranian Registry of Clinical Trials (Registration code: IRCT20161116030926N9). The participants were fully informed about the purpose of the study. Each participant provided written consent prior to participation. They were explained regarding their voluntary nature of participation and that they can stop cooperation at any given time. They also assured about their privacy and confidentiality of their information.
Consent for publication
Not applicable.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
R.G., A.H., N.F., H.M.: conceptualization, methodology, software. R.G., A.H., N.F., H.M.: data curation, writing—original draft preparation. R.G., A.H., N.F.: visualization, investigation. N.P., R.G.: supervision. R.G., H.M.: software, validation: R.G., N.F.: writing—reviewing and editing. All authors read and approved the final manuscript before submission.
Conflicts of interest disclosure
The authors declare that they have no conflict of interest.
Research registration unique identifying number (UIN)
Name of the registry: Iranian Registry of Clinical Trials
Unique identifying number or registration ID: IRCT20161116030926N9.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.irct.ir/.
Guarantor
Rasoul Goli.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Provenance and peer review
Not commissioned, externally peer-reviewed
Acknowledgements
The researchers express their gratitude to the Vice-Chancellor for Research of Urmia University of Medical Sciences and all patients who helped us conduct this study.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 5 October 2023
Contributor Information
Rasoul Goli, Email: rasoulgoli94@gmail.com.
Navid Faraji, Email: Navidfaraji1993@gmail.com.
Himan Maroofi, Email: h.maroofi@yahoo.com.
Amireh Hassanpour, Email: Amirehhassanpour@gmail.com.
References
- 1. Grotta JC, Albers GW, Broderick JP, Kasner SE, Lo EH, Sacco RL, Wong LK, Day AL. Stroke e-book: Pathophysiology, diagnosis, and management Elsevier Health Sciences; 2021. [Google Scholar]
- 2. Ha SH, Chang JY, Lee SH, et al. Mechanism of stroke according to the severity and location of atherosclerotic middle cerebral artery disease. J Stroke Cerebrovasc Dis 2021;30:105503. [DOI] [PubMed] [Google Scholar]
- 3. Zeng H, Chen J, Guo Y, et al. Prevalence and risk factors for spasticity after stroke: a systematic review and meta-analysis. Front Neurol 2021;11:616097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ranjbar M, Badihian N, Yazdi M, et al. Incidence, characteristics and prognosis of cervical artery dissection-induced ischemic stroke in central Iran. BMC Neurol 2022;22:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McGlinchey MP, James J, McKevitt C, et al. The effect of rehabilitation interventions on physical function and immobility-related complications in severe stroke—protocol for a systematic review. Syst Rev 2018;7:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lin H, Tao J, Du Y, et al. Differentiating the effects of characteristics of PM pollution on mortality from ischemic and hemorrhagic strokes. Int J Hygiene Environ Health 2016;219:204–211. [DOI] [PubMed] [Google Scholar]
- 7. Chen J, Lin Y, Yan J, et al. The effects of spiritual care on quality of life and spiritual well-being among patients with terminal illness: a systematic review. Palliat Med 2018;32:1167–79t. [DOI] [PubMed] [Google Scholar]
- 8. Kim DY, Park HS, Park SW, et al. The impact of dysphagia on quality of life in stroke patients. Medicine 2020;99:e21795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Haraldstad K, Wahl A, Andenæs R, et al. A systematic review of quality of life research in medicine and health sciences. Quality life Res 2019;28:2641–2650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Boudokhane S, Migaou H, Kalai A, et al. Predictors of quality of life in stroke survivors: a 1-year follow-up study of a Tunisian Sample. J Stroke Cerebrovasc Dis 2021;30:105600. [DOI] [PubMed] [Google Scholar]
- 11. Urcan Z, Kolcu M. Effect of a nurse-led education program for stroke patients on sleep quality and quality of life: a randomized controlled study. Clin Nursing Res 2022;31:340–347. [DOI] [PubMed] [Google Scholar]
- 12. Parizad N, Goli R, Faraji N, et al. Effect of guided imagery on anxiety, muscle pain, and vital signs in patients with COVID-19: A randomized controlled trial. Complement Ther Clin Pract 2021;43:101335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jikamo B, Adefris M, Azale T, et al. Cultural adaptation and validation of the Sidamic version of the World Health Organization Quality-of-Life-Bref Scale measuring the quality of life of women with severe preeclampsia in southern Ethiopia, 2020. Health Quality Life Outcomes 2021;19:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rezapour-Mirsaleh Y, Aghabagheri M. The relationship between personality dimensions, spirituality, coping strategies and clinical clerkship satisfaction among intern nursing students: a cross-sectional study. BMC Nursing 2020;19:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Abu HO, Ulbricht C, Ding E, et al. Association of religiosity and spirituality with quality of life in patients with cardiovascular disease: a systematic review. Quality Life Res 2018;27:2777–2797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Taghinezhad F, Mohammadi E, Khademi M, et al. Humanistic care in nursing: Concept analysis using rodgers’ evolutionary approach. Iranian J Nursing Midwifery Res 2022;27:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Giovagnoli AR, Paterlini C, Meneses RF, et al. Spirituality and quality of life in epilepsy and other chronic neurological disorders. Epilepsy Behav 2019;93:94–101. [DOI] [PubMed] [Google Scholar]
- 18. Akbari M, Hossaini SM. The relationship of spiritual health with quality of life, mental health, and burnout: The mediating role of emotional regulation. Iran J Psychiatry 2018;13:22–31. [PMC free article] [PubMed] [Google Scholar]
- 19. Duarte AA, Lucchetti G, Teixeira PJ, et al. Spirituality and religiosity are associated with quality of life in patients with lung disease. J Religion Health 2020;59:1843–1854. [DOI] [PubMed] [Google Scholar]
- 20. Willemse S, Smeets W, Van Leeuwen E, et al. Spiritual care in the intensive care unit: An integrative literature research. J Crit Care 2020;57:55–78. [DOI] [PubMed] [Google Scholar]
- 21. Arad M, Alilu L, Habibzadeh H, et al. Effect of spiritual intelligence training on nurses’ skills for communicating with patients–an experimental study. J Educ Health Promot 2022;11:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Clark CC, Hunter J. Spirituality, spiritual well-being, and spiritual coping in advanced heart failure: Review of the literature. J Holist Nursing 2019;37:56–73. [DOI] [PubMed] [Google Scholar]
- 23. Karimollahi M, Abedi HA, Yousefy A. Spiritual needs as experienced by Muslim patients in Iran: a qualitative study. Ann Gen Psychiatry 2008;7(S1):S147. [Google Scholar]
- 24. Schulz KF, Altman DG, Moher D, Consort Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg 2011;9:672–677. [DOI] [PubMed] [Google Scholar]
- 25. Beinotti F, Christofoletti G, Correia N, et al. Effects of horseback riding therapy on quality of life in patients post stroke. Top Stroke Rehabil 2013;20:226–32t. [DOI] [PubMed] [Google Scholar]
- 26. Post MW, Boosman H, Van Zandvoort MM, et al. Development and validation of a short version of the Stroke Specific Quality of Life Scale. J Neurol, Neurosurg Psychiatry 2011;82:283–286. [DOI] [PubMed] [Google Scholar]
- 27. Mahmoodi M, Safari A, Vossoughi M, et al. Stroke specific quality of life questionnaire: Test of reliability and validity of the Persian version. Iranian J Neurol 2015;14:94. [PMC free article] [PubMed] [Google Scholar]
- 28. Chen L, Xiao LD, Chamberlain D, et al. Enablers and barriers in hospital‐ to‐ home transitional care for stroke survivors and caregivers: a systematic review. J Clin Nursing 2021;30:2786–2807. [DOI] [PubMed] [Google Scholar]
- 29. Sankhe A, Dalal K, Agarwal V, et al. Spiritual care therapy on quality of life in cancer patients and their caregivers: A prospective non- randomized single-cohort study. J Religion Health 2017;56:725–31t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Balboni TA, Paulk ME, Balboni MJ, et al. Provision of spiritual care to patients with advanced cancer: associations with medical care and quality of life near death. J Clin Oncol 2010;28:445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Babamohamadi H, Kadkhodaei-Elyaderani H, Ebrahimian AA, et al. Effects of spiritual care based on GHALBE SALIM model on quality of life of patients with acute myocardial infarction. Koomesh 2019;21:262–270. [DOI] [PubMed] [Google Scholar]
- 32. Tajbakhsh F, Hosseini MA, Rahgozar M. The effect of religious- spiritual care on stress post surgery coronary artery bypass graft patients. IJRN 2016;2:57–65. [Google Scholar]
- 33. Mahdavi B, Fallahi Khoshknab M, Mohammadi F, et al. The effect of group spiritual care on quality of life in family caregivers of elders with Alzheimer’s disease. JHPM 2015;4:34–42. [Google Scholar]
- 34. Aviles JM, Whelan SE, Hernke DA, et al. Intercessory prayer and cardiovascular disease progression in a coronary care unit population: a randomized controlled trial. In Mayo Clin Proc 2001;76:1192–1198. [DOI] [PubMed] [Google Scholar]
- 35. Blumenthal JA, Babyak MA, Ironson G, et al. Spirituality, religion, and clinical outcomes in patients recovering from an acute myocardial infarction. Psychosom Med 2007;69:501–508. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


