Abstract
Automated blood pressure (BP) devices are used by many hypertensive patients in Hong Kong, with or without medical advice. At two community clinics, we invited hypertensive patients aged between 40 and 70 years who used such a device to fill in a questionnaire and to have four sets of BP measurements, automated and mercury, at two visits. Of 290 hypertensive patients 120 fulfilled the criteria, and 73 of these agreed to participate.
53 devices measured arm BP, 21 measured forearm BP. The agreement between the mercury sphygmomanometer and the automated devices was poor, with average differences of 9.5 mmHg for systolic and 9.4 mmHg for diastolic and no clear advantage for either site of measurement. As a means of screening for BP >140/90 mmHg the sensitivity of the automated devices was 81% and the specificity was 80%. There were large variations in how often and under what circumstances the devices had been used. One-fifth of the devices had been acquired on medical advice but only 11% of the participants were aware of the three important conditions for operating such devices.
Discussion of automated devices, their role and proper use, should now be part of routine hypertensive care.
INTRODUCTION
Control of blood pressure (BP) by patients and their doctors is still far from ideal.1,2 One reason is that BP is affected by transient external events and depends on measurement technique.3–5 Therefore, its diagnosis and control can be deceptive if we rely on a single clinic reading.6 Home BP predicts subsequent BP trends and is useful in the management of borderline hypertension.7 Target organ diseases and cardiovascular events relate closely to BP measurements taken outside the clinic, particularly those obtained by ambulatory monitoring.8 The British Hypertension Society recommends ambulatory monitoring in patients with white-coat hypertension or night-time hypertension, in those who have their drug treatment changed and in elderly patients with hypotension.9
The accuracy of home BP monitoring depends firstly on the machine's intrinsic reliability but also on the way the machine is used. For determining adequacy of BP control, readings should be taken at the same time of the day, preferably in the early morning and occasionally between medications.10,11 Correct technique is critical, and the measurement should be repeated after 5 minutes or more.12
In clinical practice we observed that automated BP devices are very popular in Hong Kong and their use is sometimes anomalous. We therefore conducted a small study to assess the use of such devices in Chinese hypertensive patients and how they reacted to abnormal readings.
METHODS
Two clinics were involved. The Family Medicine Integrated Clinic is based at Prince of Wales Hospital, a major hospital serving New Territory East; and Lek Yuen Health Centre is a university-affiliated community health clinic serving local people in Shatin, a satellite city in New Territory East with a population of 630 000 people with a wide spectrum of social background and education levels. Both centres are part of the government-run outpatient scheme open to the general public. About 4000 active patients are registered in each clinic and the clinics are fully computerized with all diagnoses recorded by use of International Classification of Primary Care (ICPC) codes.3
The clinic record systems were used to generate a list of patients aged between 40 and 70 years who had visited the clinic with the diagnoses of raised BP, hypertension with or without end-organ diseases (ICPC-2 codes K85, 86 and 87), between 31 January 2002 and 1 February 2003. A research assistant phoned all these patients, asking if they had an automated home BP device and had been using it for the last three months. Patients who could not be contacted by phone on three separate occasions were classified as lost to contact. To detect a difference of 10% between the two methods at a two-tailed alpha of 0.05 and power of 80% the estimated sample size was 72.
The patients were requested to attend the health centre on two occasions 7–14 days apart and to avoid smoking, alcohol, eating, bladder distension and exercise for at least 30 minutes before the visits. During the first visit, the research assistant explained the study and asked patients to sign a consent form. Then, during a 10-minute interview, they filled in a questionnaire on knowledge and use of the automated BP device. The participants then measured their BP with their own automated device without help; and about 15 minutes afterwards the research assistant repeated the measurement with a mercury sphygmomanometer. Both procedures were repeated 10 minutes later. During the second visit, the same method and sequence were employed. Therefore, a total of eight BP readings were collected for each participant, four from the automated and mercury sphygmomanometers, and four from the first and second visits. Comparisons between the measurements were made by use of Bland-Altman plots.
RESULTS
The computer records identified 374 patients with diagnoses of raised BP or hypertension who had visited the clinics in 2002–2003. We were able to contact 290 patients, of whom 120 (41%) met our criteria. 73 of these (61% of those eligible) agreed to participate. Data on the patients and their devices are shown in Table 1.
Table 1.
Characteristics of participants and automated BP devices
| Characteristic | Frequency (%) |
|---|---|
| Patient age (years) | |
| 41–50 | 14 (19) |
| 51–60 | 37 (51) |
| 61–70 | 22 (30) |
| Gender | |
| Male | 25 (34) |
| Female | 48 (66) |
| Site for device | |
| Arm | 52 (71) |
| Forearm | 21 (29) |
| Brand of device | |
| OMRON | 20 (27) |
| OSIM | 12 (16) |
| National | 9 (12) |
| OTO | 6 (8) |
| Citizen | 4 (6) |
| Others | 22 (31) |
| Purchase price* | |
| < £43 | 27 (47) |
| > £43 | 31 (53) |
When known
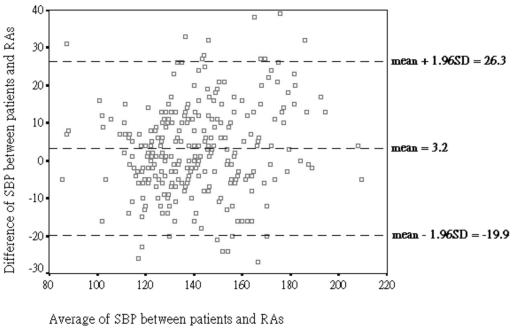
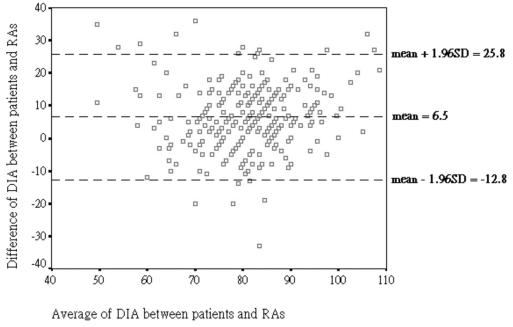
The average absolute difference between measurements with the patient's BP device and the mercury sphygmomanometer for systolic BP (SBP) was 9.5 mmHg (P=0.40) and for diastolic BP (DBP) 9.4 mmHg (P=0.08). For SBP, 39% of readings had an absolute difference below 5 mmHg, 62% of them below 10 mmHg and 81% below 15 mmHg whereas, for DBP, the respective percentages were 36%, 64% and 84%. Figures 1 and 2 illustrate the poor agreement between automated devices and mercury sphygmomanometer–concordance correlation coefficient for SBP 0.84, for DBP 0.52.
Figure 1.
Bland and Altman plot showing difference of systolic BP (SBP) between mercury sphygmomanometer (RA) and automated devices
Figure 2.
Bland and Altman plot showing difference of diastolic BP (DIA) between mercury sphygmomanometer (RA) and automated device
We examined the potential value of the devices for detecting hypertension as defined by the World Health Organization, 4140/90 mmHg. When compared to the mercury standard, the sensitivity of all BP devices used by our sample was 81% (17/21) and the specificity was 80% (218/273). On multivariate logistic regression neither price (5£42.7; P=0.08) nor site of measurement (forearm/arm; P=0.23) was shown to determine whether a machine was 'good' as reflected by the European Society of Hypertension's grade C or above.14
85% of patients said they had had no training on how to operate their machine and only 63% had read the user's manual. About half knew that the position of the cuff should be level with the heart and that they should rest for 5 minutes or more before taking the BP and one-fifth appreciated the importance of appropriate cuff size; although 20% of patients had acquired the device on medical recommendation, only 11% were knowledgeable on all three points.
The frequency with which patients measured their BP varied widely—from more than once a day (4 patients) to less than once a month (16). Two-thirds used the machine when they had symptoms (e.g., headache, dizziness) and one-third for monitoring BP control. Only 11 patients had consulted their doctor after finding a raised BP, and the medication had been changed in 3 of these.
DISCUSSION
The main finding of this study is that automated BP devices, as used by Hong Kong patients with hypertension, are not reliable. A limitation of the work was that most of the patients had well-controlled hypertension, so that the range of reliability measures did not extend far beyond the normal. In this small series we are not able to pass judgment on the individual devices; but part of the inaccuracy clearly stems from the way the devices are used. Patients tend to react cautiously when they obtain an abnormal reading, and seem wise to do so. The agreement between their automated devices and the mercury standard was poor, especially for DBP. Even as a screening instrument for hypertension their sensitivity and specificity was unsatisfactory.
Ownership of automated BP devices is widespread, and we suspect that experience in other developed countries would not differ greatly from ours in Hong Kong. Inaccuracy, through intrinsic properties or incorrect use, can cause harm. False positives can result in unnecessary anxiety; false negatives can provide misleading reassurance and reduce the incentive to change risk behaviours. On the other hand, home measurements do allow patients to take some responsibility for their own care, and BP control is likely to be best in those who are well informed about their condition. We suggest that, whenever hypertension is diagnosed, the advantages and limitations of self-monitoring should come into the discussion. Patients who decide to use home monitors should be trained in the techniques and advised on what to do when their readings are abnormal.
References
- 1.Joffres MR, Hamet P, MacLean DR, L'italien GL, Fodor G. Distribution of blood pressure and hypertension in Canada and the United States. Am J Hypertens 2001; 14: 1009-105 [DOI] [PubMed] [Google Scholar]
- 2.Burt VL, Curtler JA, Higgins M, et al. Trends in the prevalence, awareness, treatment and control of hypertension in the adult population. Data from the health examination surveys, 1960–91. Hypertension 1995; 26: 60-9 [DOI] [PubMed] [Google Scholar]
- 3.Verdecchia P, Clement D, Fagard R, Palatini P, Parati G. Blood Pressure Monitoring. Task force III: target-organ damage, morbidity and mortality. Blood Pres Monitor 1999; 4: 303-17 [DOI] [PubMed] [Google Scholar]
- 4.Chrysohoou C, Pitsavos C, Panagiotakos DB, Kokkinos PF, Stefanadis C, Toutouzas P. The association between physical activity and the development of acute coronary syndromes in treated and untreated hypertensive subjects. J Clin Hypertens 2003; 5: 115-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnett DK, McGovern PG, Jacobs DR, et al. Fifteen-year trends in cardiovascular risk factors (1980–1982 through 1995–1997): the Minnesota Heart Survey. Am J Epidemiol 2002; 156: 929-35 [DOI] [PubMed] [Google Scholar]
- 6.Chung IK, Lip GYH. White coat hypertension: not so benign after all? J Hum Hypertens 2003; 17: 807. [DOI] [PubMed] [Google Scholar]
- 7.Nesbitt SD, Amerena JV, Grant E, et al. Blood pressure as a predictor of future blood pressure stability in borderline hypertension: The Tecumseh Study. Am J Hypertens 1997; 10: 1270-80 [DOI] [PubMed] [Google Scholar]
- 8.Department of Veterans Affairs Web site. Diagnosis and management of hypertension in University Press, 1999 the primary care setting [http://www.oqp.med.va.gov/cpg/HTN/HTN_Base.htm]
- 9.O'Brien E, Coats, A, Owens P, et al. Use and interpretation of ambulatory blood pressure monitoring: recommendations of the British Hypertension Society. BMJ 2000; 320: 1128-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stergiou GS, Skeva II, Baibas NM. Diagnosis of hypertension using home or ambulatory blood pressure monitoring. J Hypertens 2000, 18: 1745-51 [DOI] [PubMed] [Google Scholar]
- 11.Kikuy M, Chonan K, Imai Y. Accuracy and reliability of wrist-cuff devices for self-measurement of blood pressure. J Hypertens 2002; 20: 573-8 [DOI] [PubMed] [Google Scholar]
- 12.American College of Family Physicians. Blood pressure monitoring at home [http://familydoctor.org/x1605.xml?printxml]
- 13.WONCA International Classification Committee. International Classification of Primary Care ICPC-2, 2nd edn. Oxford: Oxford University Press, 1999
- 14.O'Brien E, Waeber B, Parati G, Staessen J, Myers MG. Blood pressure measuring devices: recommendations of the European Society of Hypertension. BMJ 2001; 322: 531-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krecke H-J, Lutkes P, Maiwald M. Patient assessment of self-measurement of blood pressure. J Hypertens 1996,14: 323-6 [DOI] [PubMed] [Google Scholar]
- 16.White WB, Asmar R, Imai Y, Mansoor GA, Padfield P, Thijs L, Waeber B. Task Force VI: self-monitoring of the blood pressure. Blood Pres Monitor 4: 343-51 [DOI] [PubMed]