Abstract
We have previously shown that intradermal injection of high molecular weight hyaluronan (500–1200 kDa) produces localized anti-hyperalgesia in preclinical models of inflammatory and neuropathic pain. In the present experiments we studied the therapeutic effect of topical hyaluronan, when combined with each of 3 transdermal drug delivery enhancers (dimethyl sulfoxide [DMSO], protamine or terpene), in preclinical models of inflammatory and neuropathic pain. Topical application of 500–1200 kDa hyaluronan (the molecular weight range used in our previous studies employing intradermal administration), dissolved in 75% DMSO in saline, markedly reduced prostaglandin E2 (PGE2) hyperalgesia, in male and female rats. While topical 500–1200 kDa hyaluronan in DMSO vehicle dose-dependently also markedly attenuated oxaliplatin and paclitaxel chemotherapy-induced painful peripheral neuropathy (CIPN) in male rats, it lacked efficacy in females. However, following ovariectomy or intrathecal administration of an oligodeoxynucleotide (ODN) antisense to G-protein coupled estrogen receptor (GPR30) mRNA, CIPN in female rats was now attenuated by topical hyaluronan. While topical co-administration of 150–300, 300–500 or 1500–1750 kDa hyaluronan with DMSO, also attenuated CIPN, a slightly lower molecular weight hyaluronan (70–120 kDa) did not. The topical administration of a combination of hyaluronan with two other transdermal drug delivery enhancers, protamine and terpene, also attenuated CIPN hyperalgesia, an effect that was more prolonged than with DMSO vehicle. Repeated administration of topical hyaluronan prolonged the duration of anti-hyperalgesia. Our results support the use of topical hyaluronan, combined with chemically diverse non-toxic skin penetration enhancers, to induce marked anti-hyperalgesia in preclinical models of inflammatory and neuropathic pain.
Keywords: Hyperalgesia, Hyaluronan (HA), High molecular weight hyaluronan (HMWH), Anti-hyperalgesia, Chemotherapy-induced peripheral neuropathy (CIPN), Inflammation, Topical administration, Pain, Transdermal drug delivery enhancer
SUMMARY
When combined with transdermal drug delivery enhancers, topical hyaluronan can induce marked anti-hyperalgesia for inflammatory and neuropathic pain.
INTRODUCTION
Intra-articular injection of high molecular weight hyaluronan is widely used to treat knee osteoarthritis pain [3; 23; 28; 44; 74]. While it is generally thought to attenuate osteoarthritis pain by its viscoelastic/cushioning properties [25], high molecular weight hyaluronan has been shown to have anti-inflammatory and immunosuppressant effects [26; 39; 46; 52; 78]. For these effects high molecular weight hyaluronan signals via plasma membrane receptors, best characterized for cluster of differentiation 44 (CD44), considered the cognate hyaluronan receptor [72; 75; 76], which is present in nociceptors [13; 34; 36]. We previously demonstrated that both attenuation of nociceptor CD44, by intrathecal (i.t.) administration of an oligodeoxynucleotide (ODN) antisense to CD44 mRNA, or the intradermal administration of a CD44 receptor antagonist, decrease anti-hyperalgesia induced by intradermal injection of 500–1200 kDa hyaluronan [13; 34], providing support that anti-hyperalgesia induced by high molecular weight hyaluronan is mediated by its action at CD44 on nociceptors.
Neuropathic pain, a major side effect of several classes of cancer chemotherapy drugs [80], commonly referred to as chemotherapy-induced painful peripheral neuropathy (CIPN), is a debilitating condition for which there is currently no US Food and Drug Administration (FDA) approved treatment. CIPN is estimated to occur in ~40% [50; 60] of the ~17 million cancer survivors in the United States [51], emphasizing the magnitude of this problem, and bringing an urgency to understanding its underlying mechanisms, in order to develop effective treatment. CIPN prevalence is chemotherapy agent-dependent, being highest (70%–100%) for platinum-based chemotherapy drugs [10; 48; 80]. Oxaliplatin, a third-generation platinum, and paclitaxel, a first-line taxane, both produce neuropathic pain [17] [33] that can persist for months after completion of chemotherapy [47; 57]. Patients receiving bortezomib, a proteasome inhibitor used for the treatment of multiple myeloma and certain types of lymphoma [80], also frequently develop neuropathic pain (CIPN), which may last for months or even years after completion of treatment [32].
Since high molecular weight hyaluronan is poorly skin penetrant [73], in the present experiments we evaluated the anti-hyperalgesic effect of topical hyaluronan combined with three chemically diverse transdermal drug delivery enhancers, dimethyl sulfoxide (DMSO) [77], protamine [73] and terpene [21]. We report that the addition of transdermal drug delivery enhancers allows topical hyaluronan to attenuate inflammatory and neuropathic pain. We also establish the molecular weight range of hyaluronan and concentration range of a transdermal drug delivery enhancer required.
METHODS
Experimental animals
Experiments were performed on 220–400 g male and female Sprague-Dawley rats, purchased from Charles River Laboratories (Hollister, CA, USA). Rats were housed three per cage, under a 12-hour light/dark cycle, in a temperature- and humidity-controlled animal care facility at the University of California, San Francisco. Food and water were available to rats, ad libitum. Experimental protocols were approved by the University of California, San Francisco, Institutional Animal Care and Use Committee, and adhered to the National Institutes of Health Guidelines for the care and use of laboratory animals.
Measurement of nociceptive threshold
Mechanical nociceptive threshold was quantified with an Ugo Basile Analgesymeter (Stoelting, Wood Dale, IL, USA), used to perform the Randall-Selitto paw-withdrawal test [62; 69; 70]. To perform this test, rats were placed in cylindrical acrylic restrainers that had lateral ports, which allow access to the hind paw for nociceptive threshold testing, as described previously [7]. Rats were acclimatized to the testing procedure by placing them in restrainers for 1 h per day for 3 consecutive days, and for 30–40 min prior to experiments [7].
Mechanical nociceptive threshold is defined as the force, in grams, applied by the plinth, to the dorsum of the hindpaw, at which a rat withdraws its paw. Baseline paw-withdrawal threshold is defined as the mean of three readings taken before administration of test agents. To minimize experimenter bias, individuals conducting experiments were blinded to experimental treatments. Each experiment was performed on a different group of rats. Data are presented as mechanical nociceptive threshold, in grams (g), or percentage change from preintervention baseline.
Drugs
The following drugs were used in this study: 500–1200 kDa hyaluronan purchased from Tocris (Minneapolis, MN, USA); 70–120 kDa, 150–300 kDa, 300–500 kDa, and 1500–1750 kDa hyaluronan, paclitaxel, oxaliplatin, prostaglandin (PGE2), Cremophor EL, dimethyl sulfoxide (DMSO) and Ginkgo terpene lactones (here referred to as terpene) purchased from Sigma-Aldrich (St. Louis, MO, USA); bortezomib, purchased from LC Laboratories (Woburn, MA, USA); and, protamine sulfate from Thermo Fisher Scientific (Waltham, MA, USA).
Hyaluronans were initially dissolved in distilled water (dH2O) at a concentration of 10 μg/μL, stock solution, and further diluted by adding DMSO with three final concentrations of hyaluronan (1, 2 and 4 μg/μL), protamine or terpene; unless otherwise stated, the final concentration of DMSO used in experiments was 75%. The DMSO vehicle used to treat control groups was 75% DMSO in 0.9% saline. In one experiment, 500–1200 kDa hyaluronan was administered topically in 0.9% saline vehicle. PGE2 was dissolved in 0.9% saline at the same final concentration that we previously injected intradermally (100 ng/5 μL) [35]. In the experiments in which hyaluronan was dissolved in protamine vehicle, protamine was first dissolved in distilled water (dH2O), to a concentration of 5 μg/μL, and stock solution of hyaluronan was combined with protamine at the final concentration of 2 μg/μL, in a volume of 30 μL, for topical administration. Terpene was first dissolved in dH2O, 2 μg/μL; then hyaluronan was dissolved in stock solution of terpene to its final concentration of 2 μg/μL, in a volume of 30 μL, for topical administration.
Oxaliplatin CIPN:
Oxaliplatin was freshly dissolved in 0.9% saline to a concentration of 2 mg/mL just prior to its intravenous (i.v.) tail vein administration (1 mL/kg) to rats that were briefly anesthetized with isoflurane (2.5% in O2).
Paclitaxel CIPN:
Paclitaxel was dissolved in Cremophor EL and ethanol (1:1) [1; 6; 20; 22] and diluted in 0.9% saline to a concentration of 1 mg/mL, just prior to its intraperitoneal (i.p.) administration (1 mg/kg, i.p.) [19; 42] every other day for a total of 4 doses to rats briefly anesthetized with isoflurane (2.5% in O2).
Bortezomib CIPN:
Bortezomib was dissolved in 3% DMSO and 97% saline, and then diluted in 0.9% saline, to a concentration of 1 mg/mL, just prior to intravenous (0.2 mg/kg, i.v.) administration (1 mL/kg), to rats briefly anesthetized with isoflurane (2.5% in O2), every other day for a total of 4 doses.
Hyaluronans (30 μL) were administered topically on the dorsum of the hind paw, dispensed from a P200 pipette (Gilson, Middleton, WI, USA) with a plastic pipette tip, and then spread manually.
Antisense oligodeoxynucleotides (ODNs)
The roles of nociceptor CD44 and GPR30 in high molecular weight hyaluronan-induced anti-hyperalgesia were assessed by intrathecal (i.t.) administration of ODN antisense against unique regions of the rat mRNA sequences for CD44 and GPR30, respectively.
Antisense ODN sequences used in these experiments were:
CD44 ODN antisense: 5’-GAA AAG GGT CGC GGG GG-3’ (GenBank accession number NM_012924.2)
GPR30 ODN antisense: 5′-ATG TTC AGA GAG GTC CCC AG-3′ (GenBank accession number NM_133573)
Mismatch ODN, corresponding to the antisense sequence with mismatched bases (denoted by bold letters), have no sequence homologies in the rat gene database.
Mismatch ODN sequences were:
CD44 ODN mismatch: 5’-CCC CCG CGA CCC TTT TC-3’
GPR30 ODN mismatch: 5′-AGG TCC AGA AAG ATG CCA AG-3′
We have previously shown that these two antisense ODN sequences, when compared to rats treated with mismatch ODN, synthesized by Life Technologies (Carlsbad, CA, USA), decrease CD44 [13] and GPR30 [4] protein in rat dorsal root ganglia.
Before use, ODNs were reconstituted in nuclease-free 0.9% saline and then administered by the intrathecal (i.t.) route. As described previously [2], rats were transiently anesthetized with isoflurane (2.5% in O2) and 120 μg of ODN, in a volume of 20 μL, injected i.t., using a syringe (300 units/μL) attached to a 29-gauge hypodermic needle that was inserted into the subarachnoid space, between the L4 and L5 vertebrae. The i.t. site of the injectate was confirmed by a sudden flick of the rat’s tail, a reflex evoked by subarachnoid space access and bolus i.t. injection [49]. Animals regained consciousness approximately 2 minutes after i.t. injection of antisense or mismatch ODN. The use of antisense ODN, administered i.t., to attenuate the expression of proteins essential for their role in nociceptor sensitization, is well supported by previous studies, by others [55; 61; 65; 67; 68], as well as our group [5; 7; 8; 11; 34–36; 59].
Ovariectomy
Ovariectomy was performed on 23–26 day old (i.e., prepubertal) female rats that were used for behavioral experiments 3 weeks later (i.e., as adults) [41]. Animals were anesthetized with isoflurane (3% in oxygen) and received preoperative meloxicam (~5 mg/kg, s.c.) and bupivacaine (~0.1 mg/kg s.c. at the incision site) for perioperative pain control. Briefly, ovaries were accessed through bilateral cutaneous followed by peritoneal incisions. Ovaries were located and their vascular bundles ligatured with 5–0 silk suture (Perma-Hand Silk® Ethicon, Johnson & Johnson, Somerville, NJ). Ovaries were then excised, and the peritoneal and cutaneous incisions closed with 5–0 silk suture.
Statistical analysis
Data from behavioral experiments are presented as mechanical nociceptive threshold in grams or percentage change from pre intervention baseline threshold. Experiments were performed with experimenters blinded to experimental groups. Repeated-measures one-way and two-way ANOVAs or Student’s t-test was used for data analysis. Prism 9.3 (GraphPad Software) was used to generate graphics and to perform statistical analyses; P<0.05 is considered statistically significant. Data are presented as mean ± SEM.
RESULTS
Hyaluronan combined with DMSO applied topically produces anti-hyperalgesia for inflammatory pain
When PGE2 (100 ng) was injected intradermally at the site of nociceptive threshold testing on the dorsum of the hind paw, in male and female rats, it produced robust mechanical hyperalgesia; and, when 500–1200 kDa hyaluronan (2 μg/μL, 30 μL) dissolved in DMSO was administered topically, PGE2 hyperalgesia was reversed, in both male (FIG. 1A) and female (FIG. 1B) rats. Of note, topical administration of 500–1200 kDa hyaluronan combined with DMSO, produced anti-hyperalgesia of similar magnitude to that produced by intradermal injection of hyaluronan dissolved in saline vehicle [13].
Figure 1. Topical co-administration of 500–1200 kDa hyaluronan (HA) with DMSO inhibits prostaglandin E2 (PGE2) hyperalgesia in male and female rats.
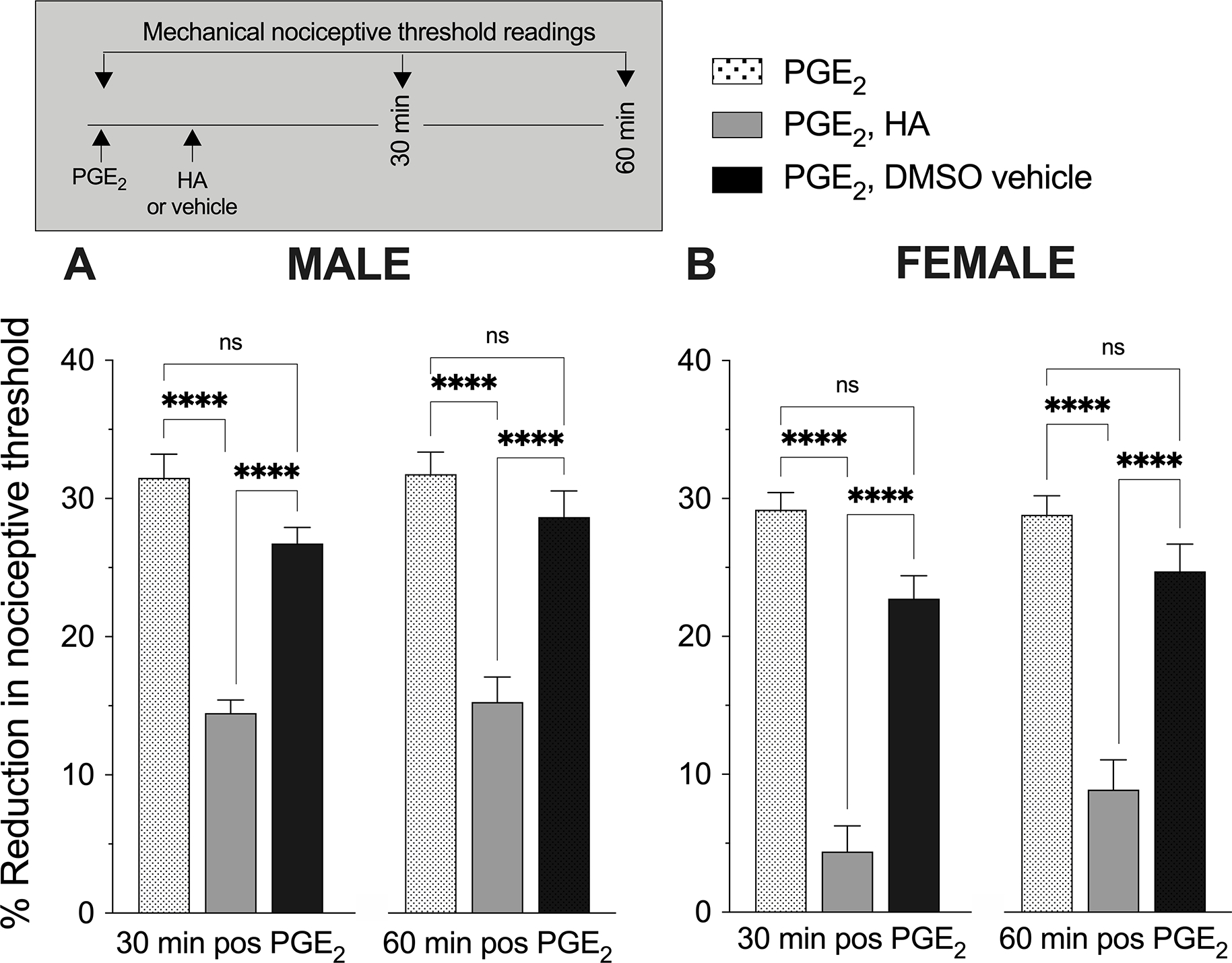
PGE2 was injected intradermally (100 ng/5 μL, i.d.) at the site of nociceptive threshold testing on the dorsum of one hind paw of male and female rats followed, 5min later, by 500–1200 kDa hyaluronan (2 μg/μL in a volume of 30 μL), or its DMSO vehicle (30 μL), was applied topically at the same site. Mechanical nociceptive threshold was measured before and again 30 and 60 min after PGE2 administration. A. Topical administration of high molecular weight hyaluronan 500–1200 kDa hyaluronan in DMSO vehicle attenuated PGE2-induced hyperalgesia in male rats (repeated measures one-way ANOVA, 30 min: Treatment F(1.35,6.75)=40.11, P=0.0003, Tukey’s multiple comparison test PGE2 alone vs. PGE2 + hyaluronan P=0.0003, PGE2 + hyaluronan vs PGE2 + DMSO vehicle P=0.0014; 60 min: Treatment F(1.84,9.2)=40.15, P<0.0001, Tukey’s multiple comparison test PGE2 alone vs. PGE2 + hyaluronan P=0.0009, PGE2 + hyaluronan vs PGE2 + DMSO vehicle P=0.0039). B. Topical administration of 500–1200 kDa hyaluronan in DMSO vehicle also attenuated PGE2-induced hyperalgesia in female rats (repeated measures one-way ANOVA, 30 min: Treatment F(1.85,9.26)=60.23, P<0.0001, Tukey’s multiple comparison test PGE2 alone vs. PGE2 + hyaluronan P=0.0005, PGE2 + hyaluronan vs PGE2 + vehicle P=0.0011; 60 min: Treatment F(1.39,6.93)=29.87, P=0.0006, Tukey’s multiple comparison test PGE2 alone vs. PGE2 + hyaluronan P=0.004, PGE2 + hyaluronan vs PGE2 + DMSO vehicle P=0.0004). n=6 per group.
Topical hyaluronan produces dose-dependent anti-hyperalgesia for neuropathic pain
We next evaluated the anti-hyperalgesia induced by topical 500–1200 kDa hyaluronan, in DMSO vehicle, in preclinical models of neuropathic pain, and its dose dependence, in male rats with oxaliplatin CIPN. Rats that received oxaliplatin (1 mL/kg, i.v.) developed long-lasting hyperalgesia (FIG. 2A). Seven days after oxaliplatin administration rats received 500–1200 kDa hyaluronan in DMSO, at one of three concentrations (1, 2 or 4 μg/μL), each in a volume of 30 μL, applied topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Topical administration of 2 and 4 μg/μL of 500–1200 kDa hyaluronan attenuates CIPN hyperalgesia 30 and 60 min after application. The anti-hyperalgesic effect of 2 and 4 μg/μL 500–1200 kDa hyaluronan dissipated by 120 min after application (FIG. 2A). When 500–1200 kDa hyaluronan (2 μg/μL) was dissolved in saline vehicle, (i.e., 0.9% saline, without DMSO) and applied topically, it did not attenuate oxaliplatin CIPN hyperalgesia (FIG. 2B).
Figure 2. Dose-response relationship for topical hyaluronan-induced anti-hyperalgesia in rats with chemotherapy-induced peripheral neuropathy (CIPN).
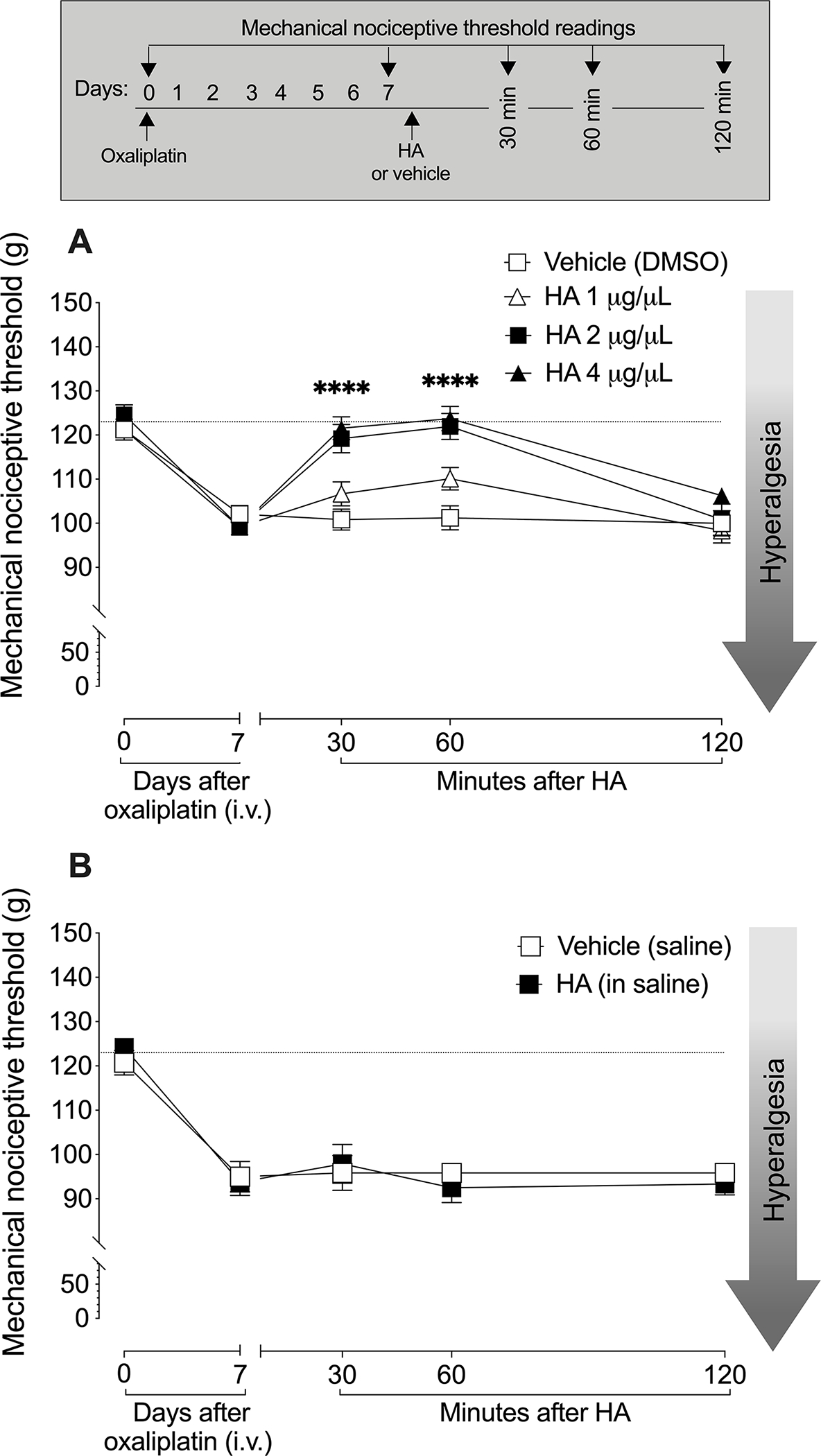
A. Male rats received oxaliplatin (2 mg/kg, i.v.) on day 0. On day 7, at which time oxaliplatin-induced hyperalgesia was established, three different doses of 500–1200 kDa hyaluronan, at (1, 2 or 4 μg/μL) or DMSO vehicle, each in a volume of 30 μL, was administered topically on the dorsum of one hind paw, at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before and 7 days after oxaliplatin administration, and then again 10, 30, 60 and 120 min after 500–1200 kDa topical hyaluronan (in DMSO vehicle). Oxaliplatin decreased mechanical nociceptive threshold (i.e., produced hyperalgesia) (paired Student’s t-test, t(23)=15.62, P<0.0001), and topical administration of 500–1200 kDa hyaluronan in DMSO vehicle dose-dependently attenuated oxaliplatin-induced hyperalgesia (Two-way repeated measures ANOVA, dose F(3,20=10.08), P=0.0003). n=6 per group.
B. Male rats received oxaliplatin (2 mg/kg, i.v.) on day 0. On day 7 after oxaliplatin administration, 500–1200 kDa hyaluronan (2 μg/μL in a volume of 30 μL) dissolved in 0.9% saline (without DMSO), or vehicle (0.9% saline, 30 μL) alone, was administered topically on the dorsum of one hind paw, at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before oxaliplatin and 7 days after oxaliplatin administration, and then again 30, 60 and 120 min after topical administration of hyaluronan. Oxaliplatin decreased mechanical nociceptive threshold (i.e., produced hyperalgesia) (paired Student’s t-test, t(11)=14.65, P<0.0001). Topical administration of 500–1200 kDa hyaluronan dissolved in saline, without DMSO, did not attenuate oxaliplatin-induced hyperalgesia (Two-way repeated measures ANOVA, dose F(1,10)=0.11, P=0.75). n=6 per group.
We next compared the anti-hyperalgesia induced by 500–1200 kDa hyaluronan in male and female rats with CIPN induced by paclitaxel, oxaliplatin or bortezomib. To generate oxaliplatin CIPN, male (FIG. 3A) rats received oxaliplatin (2 mg/kg, i.v.). Seven days later, at which time rats demonstrated robust mechanical hyperalgesia, they were treated with 500–1200 kDa hyaluronan (2 μg/μL, 30 μL) or DMSO vehicle, administered topically on the dorsum of the hind paw. In male rats with oxaliplatin CIPN, 500–1200 kDa hyaluronan induced anti-hyperalgesia (FIG. 3A). A separate group of male rats (FIG. 3B) were treated with paclitaxel, every other day for 4 days. Seven days after the first dose of paclitaxel, they received 500–1200 kDa hyaluronan (2 μg/μL, 30 μL) or DMSO vehicle, administered topically on the dorsum of the hind paw. An additional group of male rats (FIG. 3C) received bortezomib (0.2 mg/kg, i.v., every other day for a total of 4 doses). Approximately 24 h after the last dose of bortezomib, 500–1200 kDa hyaluronan (2 μg/μL, 30 μL) or DMSO vehicle was applied at the site of nociceptive threshold testing. Anti-hyperalgesia induced by topical administration of 500–1200 kDa hyaluronan was observed in male rats with CIPN. However, in female rats topical administration of 500–1200 kDa hyaluronan, in DMSO vehicle, did not attenuate hyperalgesia induced by oxaliplatin (FIG. 3D), paclitaxel (FIG. 3E) or bortezomib (FIG. 3F).
Figure 3. Topical hyaluronan-induced anti-hyperalgesia for CIPN is sexually dimorphic.
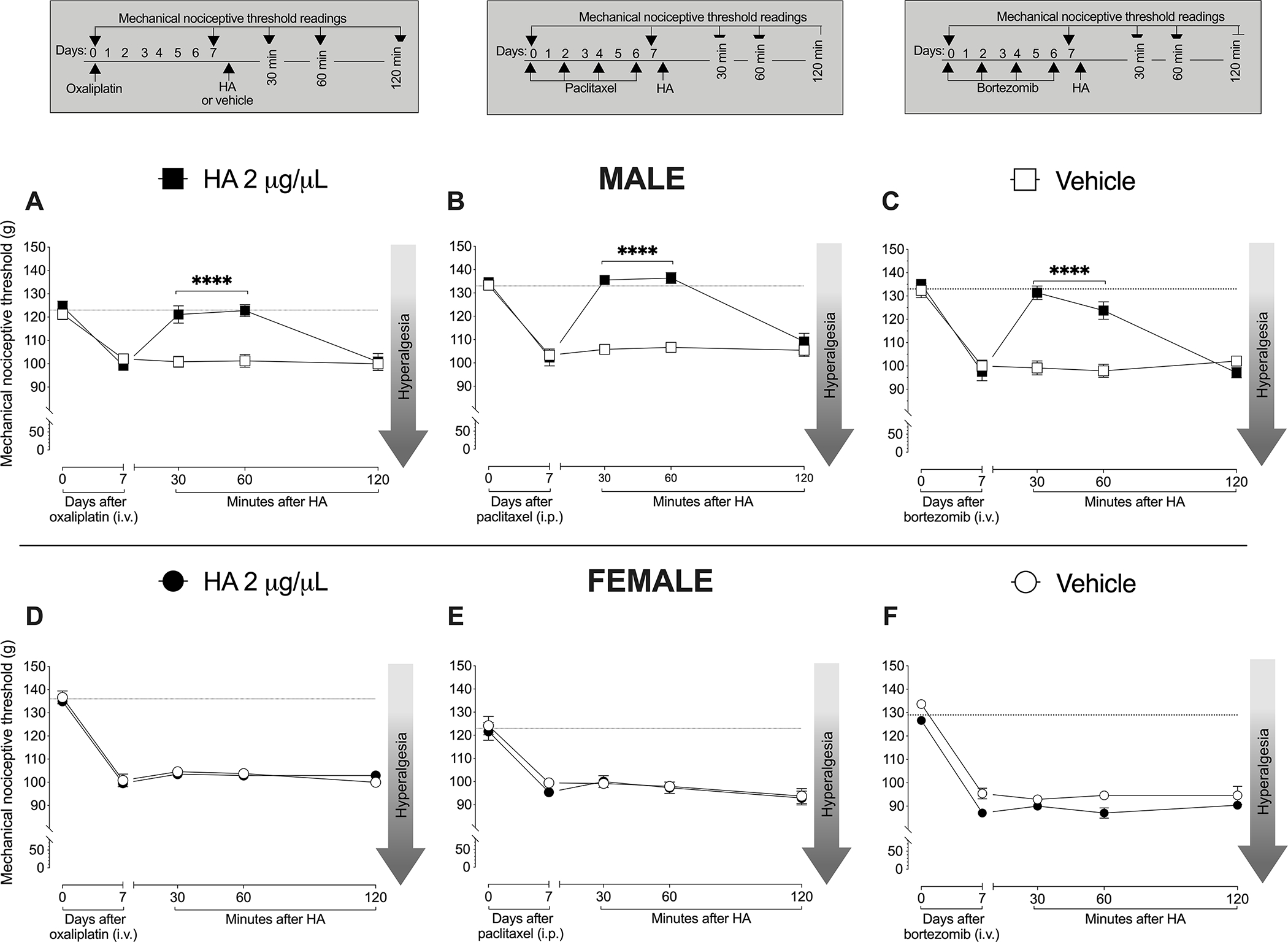
Male and female rats received oxaliplatin (2 mg/kg, i.v.) on day 0. On day 7, 500–1200 kDa hyaluronan (2 μg/μL in a volume of 30 μL) or its DMSO vehicle alone (30 μL) was topically applied to the dorsum of the hind paw, at the site of nociceptive threshold testing. Additional groups of male and female rats received paclitaxel (1 mg/kg, i.p.), every other day for a total of 4 doses (days 0, 2, 4 and 6). On day 7, approximately 24 h after the last dose of paclitaxel, hyaluronan (2 μg/μL in a volume of 30 μL) or its DMSO vehicle (30 μL) was applied topically on the dorsum of one hind paw, at the site of nociceptive threshold testing. Finally, an additional group of rats received bortezomib (0.2 mg/kg, i.v., every other day for a total of 4 doses). On day 7, approximately 24 h after the last dose of bortezomib, 500–1200 kDa hyaluronan (2 μg/μL in a volume of 30 μL) or its DMSO vehicle (30 μL) was applied topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before administration of oxaliplatin, paclitaxel or bortezomib and 7 days after, and then again 30, 60 and 120 min after topical administration of hyaluronan.
A. Oxaliplatin decreased mechanical nociceptive threshold (i.e., produced hyperalgesia) in male rats. Topical administration of 500–1200 kDa hyaluronan attenuated oxaliplatin-induced hyperalgesia (Two-way repeated measures ANOVA, dose F(1,10)=24.98, P=0.0005) (results in this figure are reproduced from FIG. 2A, for comparison).
B. Paclitaxel decreased mechanical nociceptive threshold (i.e., produced hyperalgesia) in male rats. Topical administration of 500–1200 kDa hyaluronan attenuated the hyperalgesia induced by paclitaxel (Two-way repeated measures ANOVA, dose F(1,10)=78.74, P<0.0001).
C. Bortezomib decreased mechanical nociceptive threshold (i.e., produced hyperalgesia) in male rats. Topical administration of hyaluronan attenuated bortezomib-induced hyperalgesia (Two-way repeated measures ANOVA, dose F(1,10)=39.39, P<0.0001).
D. In female rats, oxaliplatin-induced hyperalgesia was not attenuated by topical administration of 500–1200 kDa hyaluronan (Two-way repeated measures ANOVA, dose F(1,10)=0.039, P=0.8464). n=6 per group.
E. In female rats, paclitaxel-induced hyperalgesia was not attenuated by topical administration of 500–1200 kDa hyaluronan (Two-way repeated measures ANOVA, dose F(1,10)=0.004, P=0.9503). n=6 per group.
F. In female rats, bortezomib-induced hyperalgesia was not attenuated by topical administration of 500–1200 kDa hyaluronan (Two-way repeated measures ANOVA, dose F(1,10)=1.41, P=0.2471). n=6 per group.
To determine if there is a sex hormone-dependence to the lack of effect of topical 500–1200 kDa hyaluronan in female rats with CIPN, we performed ovariectomy 3 weeks prior to treating female rats with paclitaxel (FIG. 4A) or oxaliplatin (FIG. 4B). In ovariectomized female rats 500–1200 kDa hyaluronan induced anti-hyperalgesia of similar magnitude to that observed in gonad intact male rats with paclitaxel- and oxaliplatin-induced CIPN. To determine if this effect of sex hormones on hyaluronan-induced anti-hyperalgesia for CIPN was due to their action on sensory neurons, female rats with paclitaxel (FIG. 4C) and oxaliplatin (FIG. 4D) CIPN were treated i.t. with ODN antisense to GPR30 mRNA for 3 consecutive days. As for ovariectomized rats, oxaliplatin and paclitaxel CIPN in female rats that received GPR30 antisense, also demonstrated 500–1200 kDa hyaluronan-induced anti-hyperalgesia (FIG. 4C and 4D).
Figure 4. In female rats hyaluronan-induced anti-hyperalgesia is nociceptor GPER dependent.
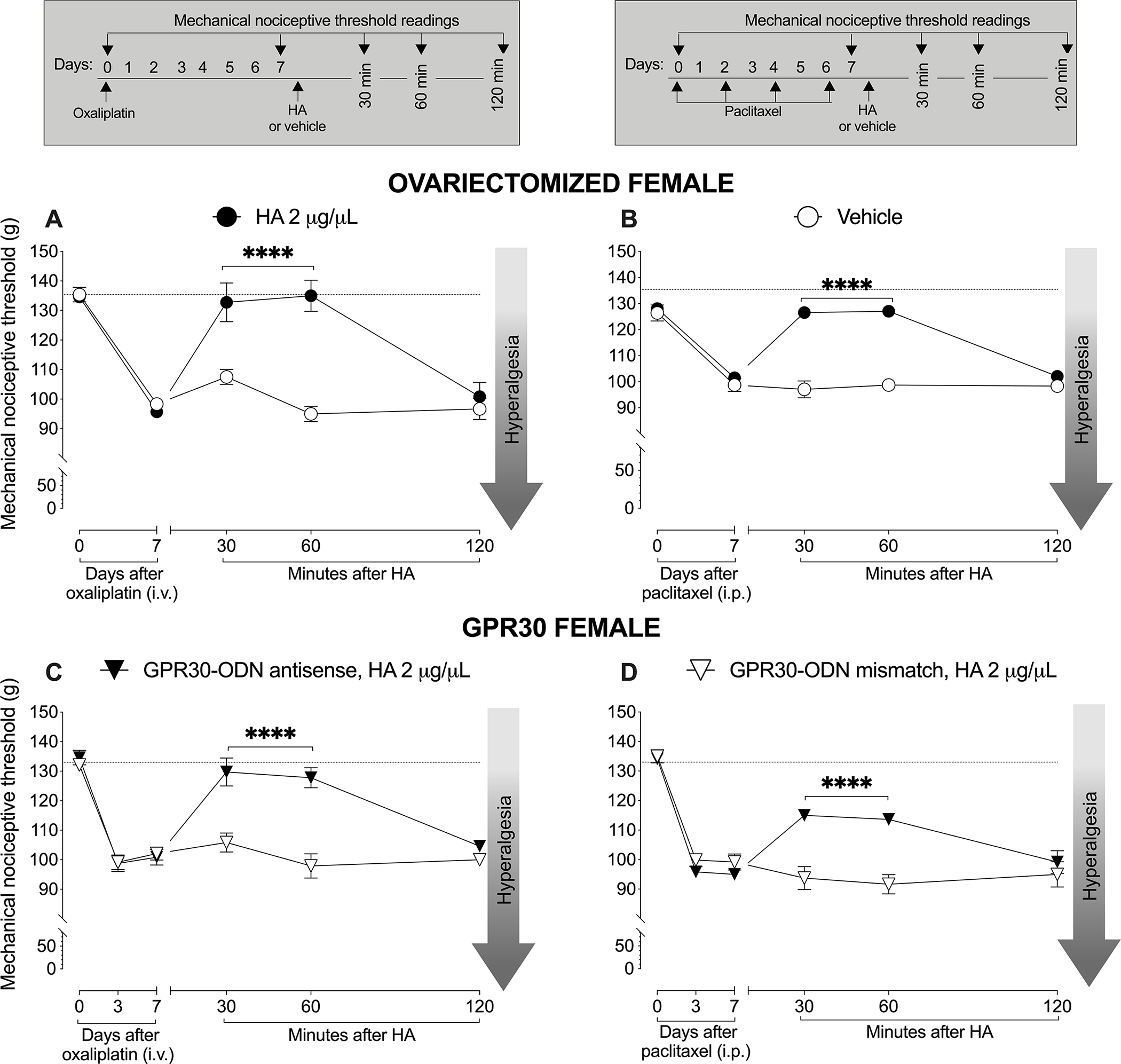
A. A group of female rats underwent surgical ovariectomy 3 weeks prior to receiving oxaliplatin (2 mg/kg, i.v.), administered on day 0. On day 7 they received 500–1200 kDa hyaluronan (2 μg/μL in a volume of 30 μL) or DMSO vehicle (30 μL), administered topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before and 7 days after oxaliplatin, and then again 30, 60 and 120 min after topical hyaluronan. Oxaliplatin decreased mechanical nociceptive threshold, measured 7 days after its administration. On day 7, topical administration of 500–1200 kDa hyaluronan attenuated the hyperalgesia induced by oxaliplatin in ovariectomized (Two-way repeated measures ANOVA, dose F(1,10)=37.75, P=0.0001), but not gonad intact, female rats (Fig. 3C). n= 6 per group.
B. Another group of female rats underwent ovariectomy 3 weeks prior to receiving a first dose of paclitaxel (1 mg/kg, i.p.). Paclitaxel was administered every other day for a total of 4 doses (days 0, 2, 4 and 6). Seven days after the first dose of paclitaxel, rats were treated with 500–1200 kDa hyaluronan (2 μg/μL in a volume of 30 μL) or its DMSO vehicle (30 μL), applied topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before and 7 days after the first dose of paclitaxel, and then again 30, 60 and 120 min after topical hyaluronan. Paclitaxel decreased mechanical nociceptive threshold, measured 7 days after its first dose, in ovariectomized and gonad-intact female rats. Topical 500–1200 kDa hyaluronan attenuated the hyperalgesia induced by paclitaxel in gonadectomized (Two-way repeated measures ANOVA, dose F(1,10)=66.27, P<0.0001) but not gonad intact female rats (Fig. 3D). n= 6 per group.
C. Female rats received oxaliplatin (2 mg/kg, i.v.) on day 0. Four days later, they were treated i.t. with ODN antisense or mismatch (120 μg/20 μL, i.t.) for GPR30 mRNA, daily for 3 consecutive days. On day 7, approximately 24 h after the last dose of ODN, 500–1200 kDa hyaluronan (2 μg/μL in a volume of 30 μL) or its DMSO vehicle (30 μL) was administered topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before oxaliplatin, 3 and 7 days after its administration, and then again 30, 60 and 120 min after topical hyaluronan. Oxaliplatin decreased mechanical nociceptive threshold in both GPR30 antisense- and mismatch-ODN treated rats. However, 500–1200 kDa hyaluronan attenuated the hyperalgesia induced by oxaliplatin only in the GPR30 antisense-treated group (Two-way repeated measures ANOVA, dose F(1,10)=24.83, P=0.0006). n= 6 per group.
D. Another group of female rats received paclitaxel (1 mg/kg, i.p. every other day for a total of 4 doses). Starting four days after the 1st dose of paclitaxel, rats were treated with antisense or mismatch ODN for GPR30 mRNA (120 μg/20 μL, i.t.), daily for 3 consecutive days. On day 7, approximately 24 h after the last dose of ODN and the last dose of paclitaxel, 500–1200 kDa hyaluronan (2 μg/μL in a volume of 30 μL) or its DMSO vehicle (30 μL) was administered topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before paclitaxel, 3 and 7 days after the first administration of paclitaxel, and then again 30, 60 and 120 min after topical 500–1200 kDa hyaluronan. Paclitaxel decreased mechanical nociceptive threshold in both GPR30 antisense- (one-way repeated measures ANOVA F(1.53,7.63) P<0.0001) and mismatch-treated groups (one-way repeated measures ANOVA F(1.13,5.65) P=0.0002). However, 500–1200 kDa hyaluronan only attenuated the paclitaxel-induced hyperalgesia in the GPR30 antisense-treated group (Two-way repeated measures ANOVA, dose F(1,10)=15.51, P=0.0028). n= 6 per group.
DMSO concentration influences hyaluronan-induced anti-hyperalgesia
We next determined the lower end of the concentration range of DMSO necessary for it to facilitate topical hyaluronan induced anti-hyperalgesia in rats with CIPN (FIG. 5). Down to a concentration of 20% DMSO, 500–1200 kDa hyaluronan produced robust anti-hyperalgesia in rats with oxaliplatin CIPN (FIG. 5A). However, when the DMSO concentration was lowered to 15%, 500–1200kDa hyaluronan no longer produced significant anti-hyperalgesia. To better visualize the difference in the DMSO concentration we show an area under curve (AUC) 30 and 60min after topical application (FIG. 5B).
Figure 5. Steep DMSO concentration dependence for hyaluronan-induced anti-hyperalgesia.
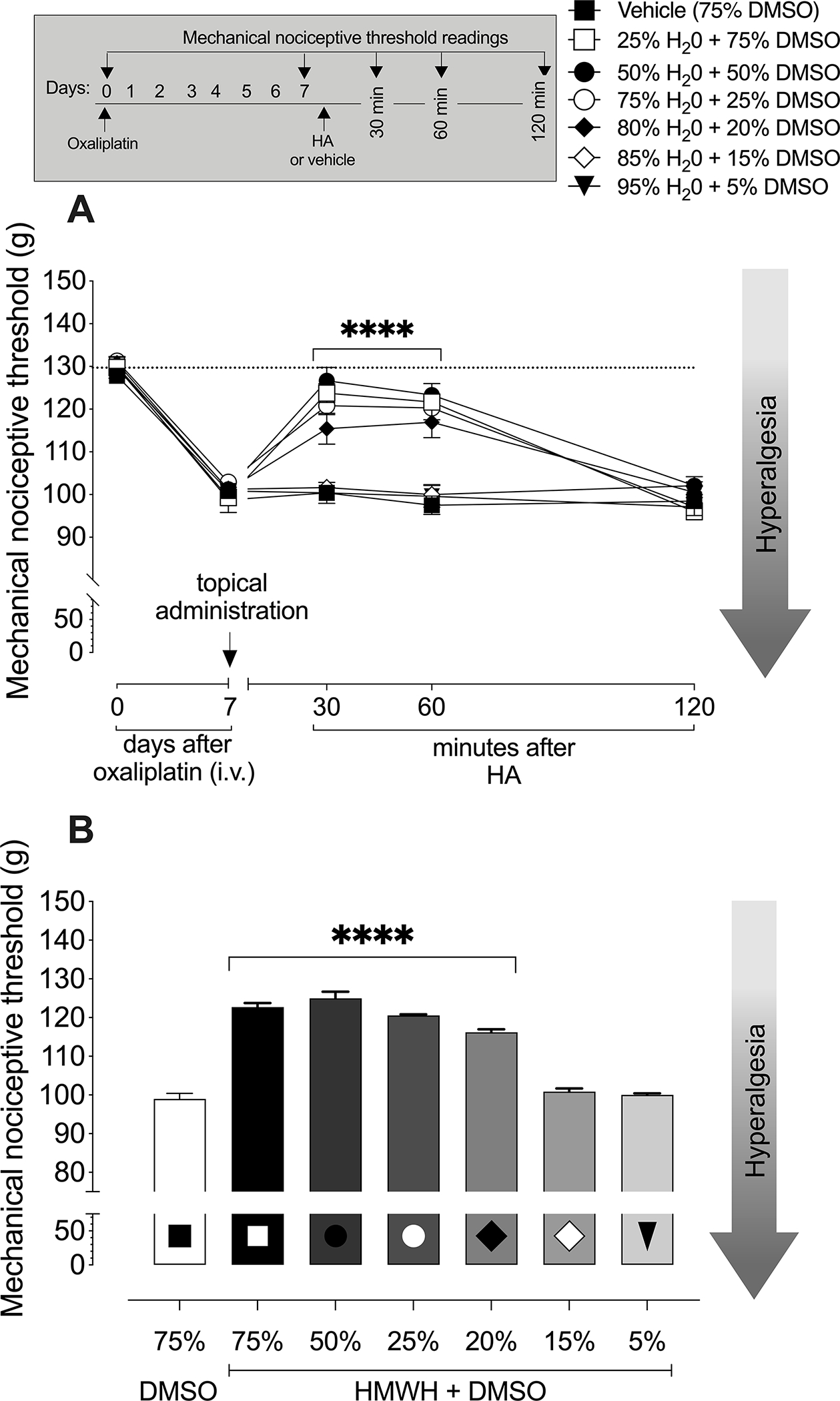
A. Male rats received oxaliplatin (2 mg/kg, i.v.) on day 0. On day 7, 500–1200 kDa hyaluronan (2 μg/μL in a volume of 30 μL) in six different percentages of DMSO (75%, 50%, 25%, 20%, 15% and 5% DMSO) or DMSO vehicle (30 μL) was administered topically on the dorsum of the hind paw at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before oxaliplatin and 7 days after its administration, and then again 30, 60 and 120 min after topical hyaluronan. Results are presented as mechanical nociceptive threshold in grams. Oxaliplatin decreased mechanical nociceptive threshold (i.e., produced hyperalgesia; paired Student’s t-test, baseline versus post-oxaliplatin before hyaluronan, for each group: Vehicle P=0.003956). Topical administration of hyaluronan in 75%, 50%, 25% and 20% produced anti-hyperalgesia (75% of DMSO P<0.0001, 50% of DMSO P<0.0001, 25% of DMSO P<0.0001, 20% of DMSO P<0.0001). However, topical administration of hyaluronan in 15% or 5% of DMSO did not produce significant anti-hyperalgesia (15% of DMSO P>0.99, 5% of DMSO P=0.99). Two-way repeated measures ANOVA, F(24.140)=13.01, P<0.0001. Dunnet’s multiple comparison post-hoc test. n=6 per group.
B. Area Under Curve (AUC) representation of 30 and 60 min data in FIG. 5A.
Repeated administration of hyaluronan prolong the duration of anti-hyperalgesia
The anti-hyperalgesia for oxaliplatin (FIG. 6A) and paclitaxel (FIG. 6B) CIPN, produced by 500–1200 kDa hyaluronan in male rats dissipated by 120 minutes. When reapplied at the same site, however, hyaluronan treatment produced longer lasting anti-hyperalgesia, in rats with oxaliplatin (FIG. 6A) or paclitaxel (FIG. 6B) CIPN, an effect still present 180 minutes after the second administration.
Figure 6. Repeated administration of high molecular weight hyaluronan prolongs anti-hyperalgesia.
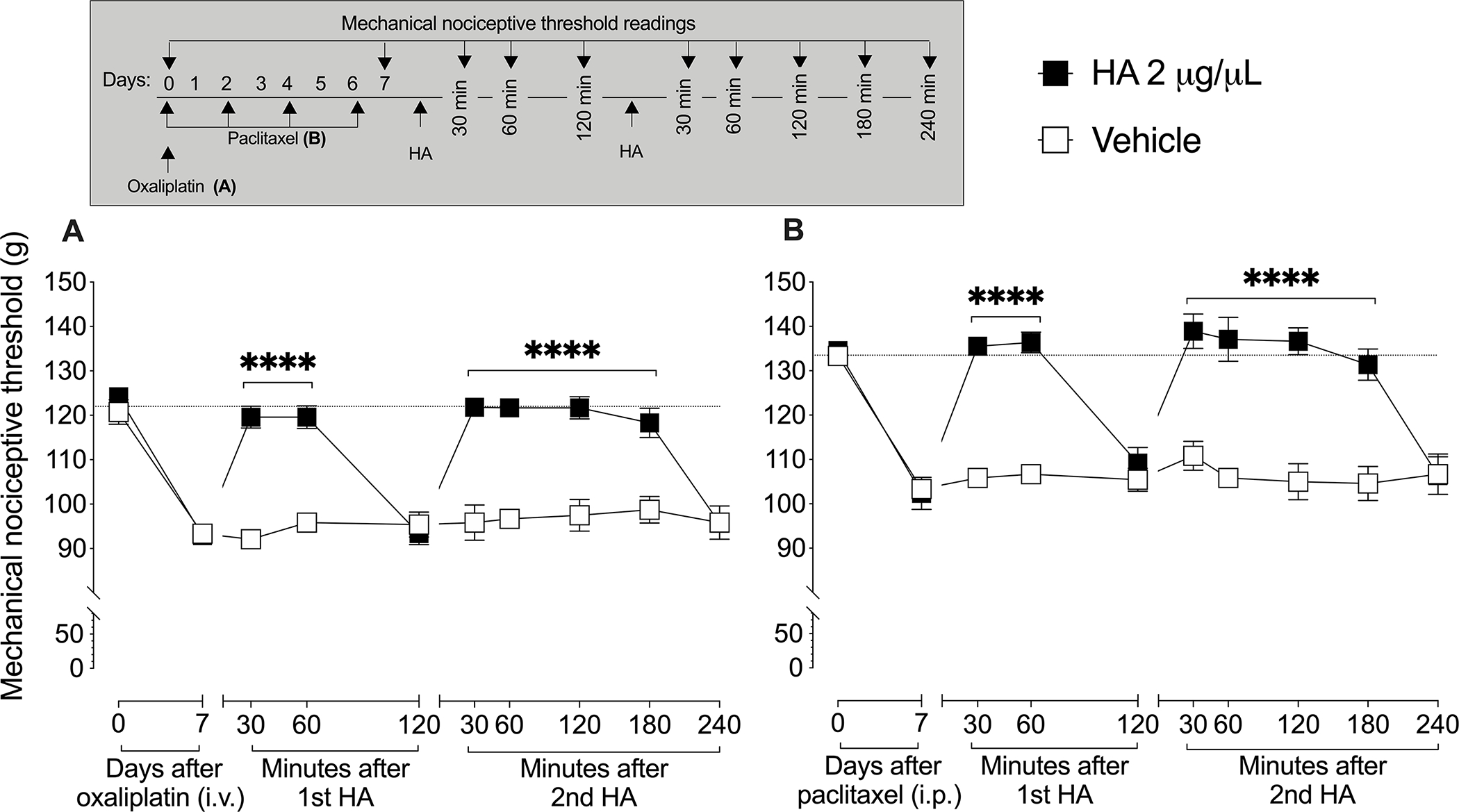
A. Male rats received oxaliplatin (2 mg/kg, i.v.) on day 0. On day 7, 500–1200 kDa hyaluronan (2 μg/μL in a volume of 30 μL) or DMSO vehicle (30 μL) was administered topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Once the anti-hyperalgesic effect of hyaluronan wore off, hyaluronan was again administered, at the same site. Mechanical nociceptive threshold was evaluated before oxaliplatin, 7 days after its administration, 30, 60 and 120 min after the first topical administration of 500–1200 kDa hyaluronan, and then again 30, 60, 120, 180 and 240 min after the second topical administration of hyaluronan. Rats treated with oxaliplatin showed a prolongation of hyaluronan-induced anti-hyperalgesia after a second administration (two-way repeated measures ANOVA, F(1,5)=138.0, P<0.0001). n= 6 per group.
B. Male rats received paclitaxel (1 mg/kg, i.p. every other day for a total of 4 doses). On day 7 hyaluronan (2 μg/μL in a volume of 30 μL) or DMSO vehicle (30 μL) was administered topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Once the anti-hyperalgesic effect of hyaluronan wore off, another dose of hyaluronan was administered at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before paclitaxel, 7 days after its first administration, 30, 60 and 120 min after the first topical administration of hyaluronan, and then again 30, 60, 120, 180 and 240 min after the second topical administration of hyaluronan. Paclitaxel-treated rats showed a prolongation of 500–1200 kDa hyaluronan-induced anti-hyperalgesia after the second administration, (two-way repeated measures ANOVA, F(1,5)=29.0, P=0.003). n= 6 per group.
Hyaluronan anti-hyperalgesia depends on its molecular weight
We have previously shown that while intradermal injection of 500–1200 kDa high molecular weight hyaluronan induces anti-hyperalgesia [12–16; 36], low molecular weight hyaluronan (~1.2 kDa) induces hyperalgesia [13; 14; 34; 36]. Therefore, we next evaluated the range of molecular weights of topical hyaluronan that combined with DMSO produce anti-hyperalgesia. In separate groups of rats experiencing oxaliplatin CIPN, we administered different molecular weight ranges of hyaluronan: 70–120 kDa, 150–300 kDa, 300–500 kDa, 500–1200 kDa, or 1500–1750 kDa. Except for 70–120 kDa hyaluronan, which did not attenuate CIPN hyperalgesia, all the higher molecular weight ranges of hyaluronan tested produced robust anti-hyperalgesia, of similar magnitude and duration (FIG. 7A).
Figure 7. Effect of hyaluronan molecular weight, and use of other transdermal drug delivery enhancers on topical hyaluronan-induced anti-hyperalgesia.
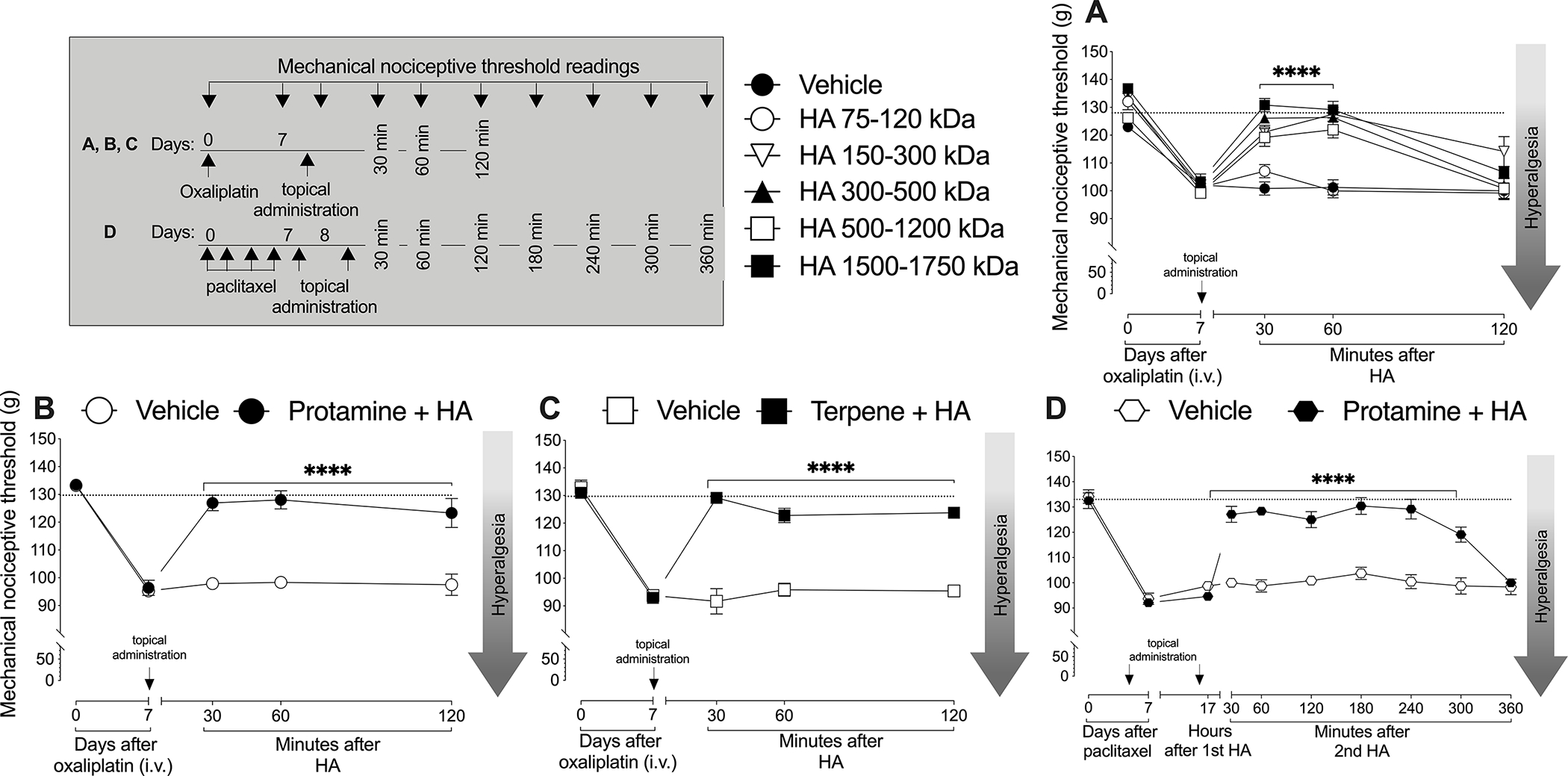
A. Male rats received oxaliplatin (2 mg/kg, i.v.) on day 0. On day 7, hyaluronan of 5 different molecular weight ranges (75–120, 150–300, 300–500, 500–1200, and 1500–1750 kDa), was administered, on the dorsum of the hind paw, at the site of nociceptive threshold testing, in separate groups of rats. Mechanical nociceptive threshold was evaluated before, 7 days after administration of oxaliplatin, and then again 10, 30, 60 and 120 min after topical hyaluronan or DMSO vehicle. Oxaliplatin decreased mechanical nociceptive threshold (i.e., produced hyperalgesia, paired Student’s t-test, baseline versus post-oxaliplatin, before hyaluronan, for each group: Vehicle P=0.003956). Topical administration of all molecular weight ranges of hyaluronan, except 70–120 kDa which did not produce anti-hyperalgesia, produced robust anti-hyperalgesia, of similar magnitude (70–120 kDa P=0.000526, 150–300 kDa P=0.000122, 300–500 kDa P=0.000009, 500–1200 kDa P=0.000169, 1500–1750 kDa P=0.000026). The anti-hyperalgesia induced by all molecular weight ranges of hyaluronan was significant 60 min post-administration (two-way repeated measures ANOVA, F(5,30)=20.60, P<0.0001). n= 6 per group.
B. Male rats received oxaliplatin (2 mg/kg, i.v.) on day 0. On day 7 after oxaliplatin hyaluronan combined with protamine (2 μg/μL in a volume of 30 μL) or protamine alone as a control (30 μL) was administered topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before, 7 days after administration of oxaliplatin, and then again 10, 30, 60 and 120 min after topical application of hyaluronan. Compared with protamine alone, topical administration of hyaluronan combined with protamine produced robust anti-hyperalgesia lasting 120 min post-administration (two-way repeated measures ANOVA, F(4,40)=24.50, P<0.0001). n= 6 per group.
C. Male rats received oxaliplatin (2 mg/kg, i.v.) on day 0. On day 7 after oxaliplatin hyaluronan combined with terpene (2 μg/μL in a volume of 30 μL) or terpene alone as a control (30 μL) was administered topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before, 7 days after administration of oxaliplatin, and then again 10, 30, 60 and 120 min after topical application of hyaluronan. Compared with terpene alone, topical administration of hyaluronan combined with terpene produced anti-hyperalgesia (two-way repeated measures ANOVA, F(4,40)=41.02, P<0.0001). n= 6 per group.
D. Male rats received paclitaxel (1 mg/kg, i.p. every other day for a total of 4 doses). On day 7 hyaluronan combined with protamine (2 μg/μL in a volume of 30 μL) or protamine alone as a control (30 μL) was administered topically on the dorsum of the hind paw, at the site of nociceptive threshold testing in the end of the day. On day 8, another dose of hyaluronan was administered at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before paclitaxel, 7 and 8 days after its administration, and then again 30, 60, 120, 180, 240, 300 and 360 min after the second topical administration of hyaluronan. Paclitaxel-treated rats showed a prolongation of 500–1200 kDa hyaluronan-induced anti-hyperalgesia after the second administration, (two-way repeated measures ANOVA, F(9,90)=21.12, P<0.0001). n= 6 per group.
Efficacy of other transdermal drug delivery enhancers
Since DMSO alone has been reported to have physiological effects [77], to demonstrate the requirement of a transdermal drug delivery enhancer for topical hyaluronan to produce anti-hyperalgesia, male rats with oxaliplatin CIPN received a combination of hyaluronan with protamine (another skin penetration enhancement molecule [73]) administered topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Topical administration of hyaluronan combined with protamine, but not protamine alone, produced robust anti-hyperalgesia (FIG. 7B). As a further test that transdermal drug delivery enhancers, as a class, facilitate anti-hyperalgesia by topical hyaluronan, a combination of hyaluronan and terpene was administered topically on the dorsum of the hind paw, at the same site. Topical administration of hyaluronan combined with terpene, but not terpene alone, also produced anti-hyperalgesia (FIG. 7C). Of note, the duration of hyaluronan anti-hyperalgesia, when it was administered with protamine or terpene vehicle was much longer than when administered in DMSO vehicle.
Since hyaluronan in protamine vehicle produced longer anti-hyperalgesia, and DMSO showed longer lasting anti-hyperalgesia after the second administration, we determined if hyaluronan combined with protamine, when reapplied at the same site, produces longer lasting anti-hyperalgesia. The second topical administration of hyaluronan combined with protamine also produced prolonged anti-hyperalgesia (FIG. 7D), lasting 5 hours.
Anti-hyperalgesia induced by topical hyaluronan is CD44 receptor dependent
We have previously shown that the anti-hyperalgesia induced by intradermal injection of 500–1200 kDa hyaluronan was nociceptor CD44 dependent [12–14; 34; 36]. Here we determined if the anti-hyperalgesia induced by topical 500–1200 kDa hyaluronan in CIPN is also nociceptor CD44 dependent. Male rats received oxaliplatin (2 mg/kg, i.v.) (FIG. 8A) or paclitaxel (1 mg/kg, i.p., 4 doses every other day) (FIG. 8B). Four days after oxaliplatin or the first injection of paclitaxel, rats received i.t. injections of ODN antisense or mismatch to CD44 mRNA, for 3 consecutive days. On the fourth day, approximately 24 h after the last administration of ODN, topical 500–1200 kDa hyaluronan (2 μg/μL, 30 μL) was applied on the dorsum of the hind paw. In male rats with CIPN, induced by oxaliplatin or paclitaxel, the anti-hyperalgesia induced by 500–1200 kDa hyaluronan was markedly attenuated in rats treated intrathecally with ODN antisense to CD44 mRNA (FIG. 8A and 8B).
Figure 8. CD44 dependence of topical hyaluronan-induced anti-hyperalgesia.
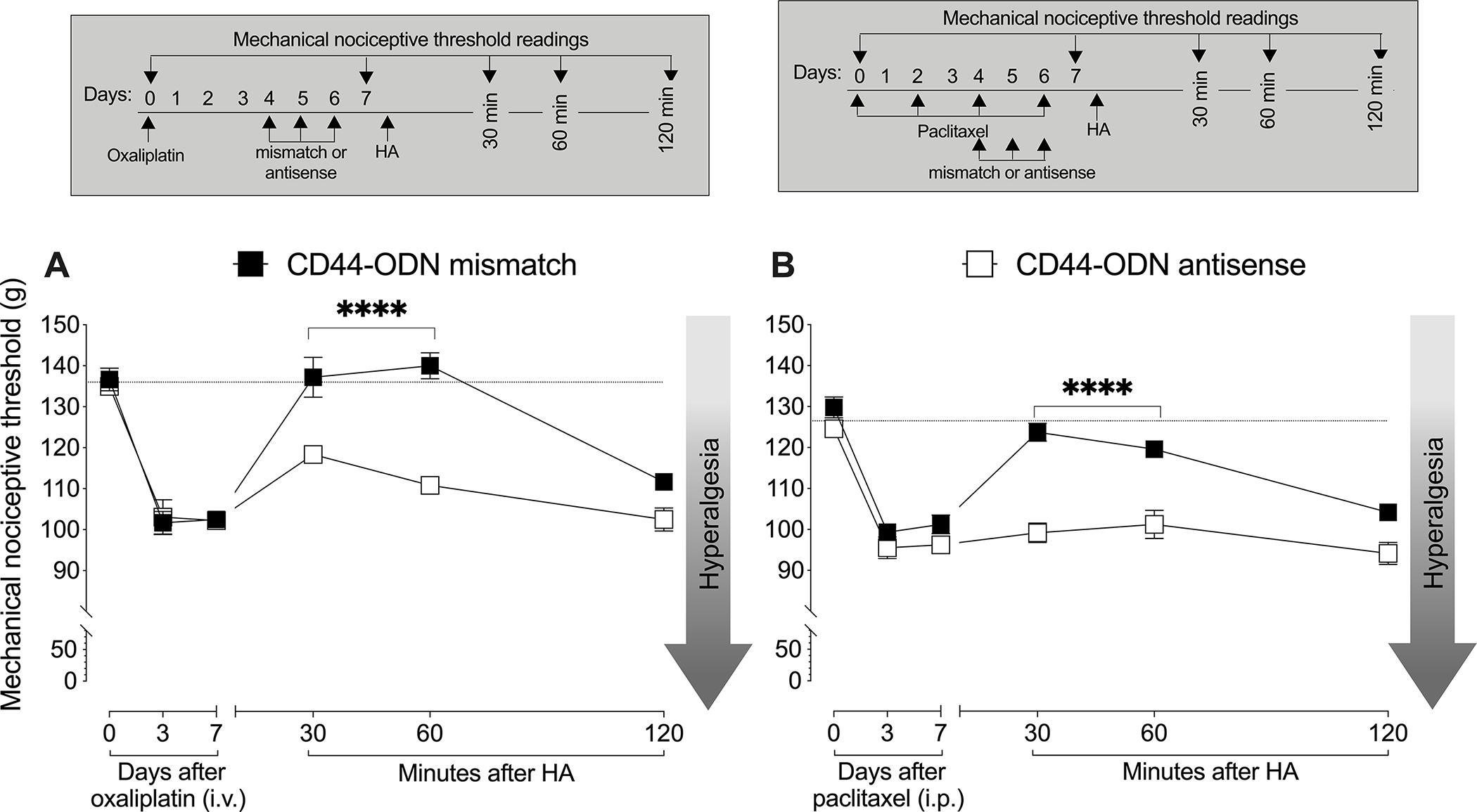
A. Male rats received oxaliplatin (2 mg/kg, i.v.) on day 0. Starting four days later they were treated intrathecally (i.t.) with ODN antisense or mismatch for CD44 mRNA (120 μg/20 μL, i.t.), daily for 3 days. On day 7, approximately 24 h after the last dose of ODN, 500–1200 kDa hyaluronan (2 μg/μL in a volume of 30 μL) or its DMSO vehicle (30 μL) was administered topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before oxaliplatin and 7 days after its administration, and then again 30, 60 and 120 min after topical hyaluronan. Results are presented as mechanical nociceptive threshold in grams. Oxaliplatin decreased mechanical nociceptive threshold, measured 4 days after its administration, in both CD44 antisense- (one-way repeated measures ANOVA F(1.00,5.01)=41.13, P=0.0014) and mismatch- (one-way repeated measures ANOVA F(1.30,6.51)=48.95, P=0.0002) treated groups. However, 500–1200 kDa hyaluronan only attenuated the hyperalgesia induced by oxaliplatin in the CD44 mismatch-treated group (two-way repeated measures ANOVA F(1,10)=40.72, P<0.0001). n= 6 per group.
B. Male rats received paclitaxel (1 mg/kg, i.p., every other day for a total of 4 doses). Four days after the first paclitaxel injection, rats were treated with ODN antisense or mismatch (120 μg/20 μL, i.t.) for CD44 mRNA, daily for 3 consecutive days. On day 7, approximately 24 h after the last ODN dose, and the last administration of paclitaxel, hyaluronan (2 μg/μL in a volume of 30 μL) or DMSO vehicle (30 μL) was applied topically on the dorsum of the hind paw, at the site of nociceptive threshold testing. Mechanical nociceptive threshold was evaluated before paclitaxel, 7 days after its administration, and then again 30, 60 and 120 min after topical 500–1200 kDa hyaluronan. Hyaluronan attenuated the hyperalgesia induced by paclitaxel only in the CD44 mismatch-treated group (two-way repeated measures ANOVA F(1,10)=54.02, P<0.0001). n= 6 per group.
DISCUSSION
A general concern with systemic drug administration is their large number of associated adverse effects on diverse organ systems, some quite serious [56; 63]. These adverse effects can, in some circumstances, be abrogated by using topical/local administration [45]. However, efficacy of topical drug administration may be limited by poor permeation from the site of drug application [73; 79]. In the present experiments we tested the hypothesis that topical drug formulations containing transdermal permeation enhancers may be of potential clinical importance [73].
While the topical route of administration may allow some drugs to access dermal tissues, the skin’s surface contains a lamellar structure, the stratum corneum, which forms a major barrier to deep penetration by many topical drugs [53; 54]. Composed of dead corneocytes, embedded in an intercellular lipid matrix consisting of ceramides, free fatty acids, cholesterol, and cholesteryl esters [54; 58], the stratum corneum is poorly penetrated by large and hydrophilic molecules such as high molecular weight hyaluronan.
Intradermal injection of high molecular weight hyaluronan, which bypasses the stratum corneum barrier to uptake of topically applied drugs, attenuates PGE2-induced hyperalgesia, in female and male rats [13], and hyperalgesia in preclinical models of CIPN, induced by paclitaxel and oxaliplatin, in male and gonadectomized, but not gonad intact, female rats [16]. In the present study we observed that when combined with the classical transdermal permeability enhancer DMSO, topical administration of high molecular weight hyaluronan attenuates PGE2-induced hyperalgesia. To evaluate the potential for the use of topical high molecular weight hyaluronan in the treatment of neuropathic pain, we induced CIPN oxaliplatin, paclitaxel or bortezomib, representatives of three important classes of cancer chemotherapy, which are thought to induce CIPN by different mechanisms [18; 24; 37; 71]. Topical high molecular weight hyaluronan, when co-administered with DMSO, robustly attenuated oxaliplatin, paclitaxel and bortezomib CIPN in male, but not female, rats. This anti-hyperalgesia, in rats with CIPN, is dependent on the action of hyaluronan at CD44, the cognate hyaluronan receptor [9; 34; 66], which is found on nociceptors, as male rats treated intrathecally with ODN antisense against CD44 mRNA, have decreased high molecular weight hyaluronan-induced anti-hyperalgesia [12; 13; 36].
To evaluate the role of sex hormones in the inability of high molecular weight hyaluronan to induce anti-hyperalgesia in female rats with CIPN, we studied ovariectomized female rats and female rats treated intrathecally with ODN antisense against GPR30, a G-protein coupled estrogen receptor [38] found in DRG neurons [29]. In both groups, topical high molecular weight hyaluronan now robustly attenuated paclitaxel and oxaliplatin CIPN, supporting the suggestion that female sex hormones act at GPR30 on nociceptors to suppress the ability of high molecular weight hyaluronan to suppress CIPN, in female rats. However, since many female oncology patients are post-menopausal, and thus have low estrogen levels, topical high molecular weight hyaluronan may be effective for the treatment of CIPN in these patients. Why hyaluronan attenuates inflammatory but not neuropathic pain in gonad intact female rats, is currently being investigated.
Following its initial administration, the anti-hyperalgesic effect of topical high molecular weight hyaluronan in DMSO vehicle lasted approximately 60 minutes. However, its subsequent application, produced substantially longer lasting anti-hyperalgesia, a prolongation that persisted following additional administration (data not shown). This prolongation of anti-hyperalgesia was also observed when protamine or terpene were used as the transdermal drug enhancer. These results support the suggestion that repeated application does not produce tolerance to the therapeutic effect of topical hyaluronan, but rather prolonged anti-hyperalgesia.
Since different weight ranges of high molecular weight hyaluronan are used clinically [43], to identify the molecular weight range effective in producing anti-hyperalgesia with topically administered hyaluronan combined with a transdermal drug delivery enhancer, we studied 4 different molecular weight ranges, in addition to the weight range we previously administered intradermally (500–1,200 kDa, [12–16; 34; 36]). Hyaluronan of higher molecular weight (1,500–1,750 kDa) produced a similar anti-hyperalgesic response. However, a somewhat lower molecular weight range (70–120 kDa) did not induce anti-hyperalgesia. Why this slightly lower molecular weight range fails to produce anti-hyperalgesia remains to be determined. While we have shown previously that even lower molecular weight hyaluronan induces hyperalgesia [14; 34] hyaluronan in the 70–120 kDa range did not produce hyperalgesia.
High molecular weight hyaluronan dissolved in saline does not penetrate the skin [73]; the stratum corneum preventing the transdermal absorption of poorly permeable polar and/or high molecular weight compounds [30; 81]. Here we show that to produce anti-hyperalgesia for inflammatory and neuropathic pain, topical high molecular weight hyaluronan requires the addition of a dermal penetration enhancer. It should be noted that DMSO, a classic transdermal transport enhancer may, alone, have physiological effects; for example, as topically administered DMSO has been used to treat systemic inflammation in veterinary medical practice [27; 64; 77]. However, in our study, DMSO alone has no effect on hyperalgesia in rats with CIPN; nor was high molecular weight hyaluronan dissolved in saline (0.9% of NaCl) able to induce anti-hyperalgesia. Taken together, these observations support our hypothesis that the combination of high molecular weight hyaluronan, of a restricted molecular weight range, and a transdermal drug delivery enhancer, of a minimum concentration is required for topical hyaluronan to produce anti-hyperalgesia.
To better understand the contribution of transdermal drug delivery enhancers to topical hyaluronan-induced anti-hyperalgesia, we tested different percentages of DMSO in combination with high molecular weight hyaluronan. High molecular weight hyaluronan combined with a concentration of DMSO greater than 20% was necessary to produce anti-hyperalgesia that was of similar magnitude to that produced by intradermal injection of hyaluronan, in saline vehicle [12–16; 34; 36].
Finally, we found that two other, chemically dissimilar, transdermal drug delivery enhancers, protamine [73] and terpene [21], when combined with high molecular weight hyaluronan, also produced anti-hyperalgesia. Of note, duration of the anti-hyperalgesia induced by hyaluronan in combination with these other two transdermal drug delivery enhancers was dramatically longer than produced by high molecular hyaluronan with DMSO; and repeat administration produced prolongation of anti-hyperalgesia. While additional experiments will be required to determine the mechanistic basis of the longer anti-hyperalgesia duration produced when hyaluronan is combined with protamine and terpene, as well as the prolongation of anti-hyperalgesia induced by repeated topical administration of hyaluronan, the finding of the present experiments strongly support the suggestion that tolerance to the anti-hyperalgesic effect of topical hyaluronan would not be a limitation to its clinical use.
Since the topical administration of high molecular weight hyaluronan, when combined with a transdermal permeability enhancer, induced anti-hyperalgesia in rats with inflammatory and neuropathic hyperalgesia, we suggest that hyaluronan combined with transdermal drug delivery enhancers may provide a treatment for acute and chronic inflammatory and neuropathic pain. Their combination could potentially also enhance the efficacy of intra-articular injection of hyaluronan, in patients with arthritis, where its use in current therapy is designed to remain in the joint space, to produce its therapeutic effect by acting as a viscoelastic cushion [25; 31; 40], or at other sites in the body where greater spread from the injection site would reach additional sensitized nociceptors. For example, in patients with arthritis, the addition of a transdermal delivery enhancer would allow hyaluronan to act on sensitized nociceptors deeper in the synovium, more remotely from its intra-articular site of administration.
Acknowledgements:
The authors would like to thank Niloufar Mansooralavi for technical assistance. This study was funded by National Institutes of Health (NIH) grants AR075334 and CA250017.
Footnotes
Conflict of Interest: The authors declare no competing financial interests.
The data presented in this study are available from the corresponding author upon reasonable request.
REFERENCES
- [1].Adams JD, Flora KP, Goldspiel BR, Wilson JW, Arbuck SG, Finley R. Taxol: a history of pharmaceutical development and current pharmaceutical concerns. J Natl Cancer Inst Monogr 1993(15):141–147. [PubMed] [Google Scholar]
- [2].Alessandri-Haber N, Yeh JJ, Boyd AE, Parada CA, Chen X, Reichling DB, Levine JD. Hypotonicity induces TRPV4-mediated nociception in rat. Neuron 2003;39(3):497–511. [DOI] [PubMed] [Google Scholar]
- [3].Altman RD, Moskowitz R. Intraarticular sodium hyaluronate (Hyalgan) in the treatment of patients with osteoarthritis of the knee: a randomized clinical trial. Hyalgan Study Group. J Rheumatol 1998;25(11):2203–2212. [PubMed] [Google Scholar]
- [4].Alvarez P, Bogen O, Levine JD. Role of nociceptor estrogen receptor GPR30 in a rat model of endometriosis pain. Pain 2014;155(12):2680–2686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Alvarez P, Green PG, Levine JD. Role for monocyte chemoattractant protein-1 in the induction of chronic muscle pain in the rat. Pain 2014;155(6):1161–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Apfel SC, Lipton RB, Arezzo JC, Kessler JA. Nerve growth factor prevents toxic neuropathy in mice. Ann Neurol 1991;29(1):87–90. [DOI] [PubMed] [Google Scholar]
- [7].Araldi D, Bogen O, Green PG, Levine JD. Role of Nociceptor Toll-like Receptor 4 (TLR4) in Opioid-Induced Hyperalgesia and Hyperalgesic Priming. J Neurosci 2019;39(33):6414–6424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Araldi D, Ferrari LF, Levine JD. Hyperalgesic priming (type II) induced by repeated opioid exposure: maintenance mechanisms. Pain 2017;158(7):1204–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Aya KL, Stern R. Hyaluronan in wound healing: rediscovering a major player. Wound Repair Regen 2014;22(5):579–593. [DOI] [PubMed] [Google Scholar]
- [10].Banach M, Juranek JK, Zygulska AL. Chemotherapy-induced neuropathies-a growing problem for patients and health care providers. Brain Behav 2017;7(1):e00558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Bogen O, Alessandri-Haber N, Chu C, Gear RW, Levine JD. Generation of a pain memory in the primary afferent nociceptor triggered by PKCepsilon activation of CPEB. J Neurosci 2012;32(6):2018–2026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Bonet IJM, Araldi D, Green PG, Levine JD. Sexually Dimorphic Role of Toll-like Receptor 4 (TLR4) in High Molecular Weight Hyaluronan (HMWH)-induced Anti-hyperalgesia. J Pain 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Bonet IJM, Araldi D, Khomula EV, Bogen O, Green PG, Levine JD. Mechanisms Mediating High-Molecular-Weight Hyaluronan-Induced Antihyperalgesia. J Neurosci 2020;40(34):6477–6488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bonet IJM, Green PG, Levine JD. Sexual dimorphism in the nociceptive effects of hyaluronan. Pain 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Bonet IJM, Khomula EV, Araldi D, Green PG, Levine JD. PI3Kgamma/AKT signaling in high molecular weight hyaluronan (HMWH)-induced anti-hyperalgesia and reversal of nociceptor sensitization. J Neurosci 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Bonet IJM, Staurengo-Ferrari L, Araldi D, Green PG, Levine JD. Second messengers mediating high-molecular-weight hyaluronan-induced antihyperalgesia in rats with chemotherapy-induced peripheral neuropathy. Pain 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Branca JJV, Carrino D, Gulisano M, Ghelardini C, Di Cesare Mannelli L, Pacini A. Oxaliplatin-Induced Neuropathy: Genetic and Epigenetic Profile to Better Understand How to Ameliorate This Side Effect. Front Mol Biosci 2021;8:643824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bruno PM, Liu Y, Park GY, Murai J, Koch CE, Eisen TJ, Pritchard JR, Pommier Y, Lippard SJ, Hemann MT. A subset of platinum-containing chemotherapeutic agents kills cells by inducing ribosome biogenesis stress. Nat Med 2017;23(4):461–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Cavaletti G, Bogliun G, Crespi V, Marzorati L, Zincone A, Marzola M, Rota S, Galli A, Tredici P, Tredici G. Neurotoxicity and ototoxicity of cisplatin plus paclitaxel in comparison to cisplatin plus cyclophosphamide in patients with epithelial ovarian cancer. J Clin Oncol 1997;15(1):199–206. [DOI] [PubMed] [Google Scholar]
- [20].Cavaletti G, Tredici G, Braga M, Tazzari S. Experimental peripheral neuropathy induced in adult rats by repeated intraperitoneal administration of taxol. Exp Neurol 1995;133(1):64–72. [DOI] [PubMed] [Google Scholar]
- [21].Chen J, Jiang QD, Chai YP, Zhang H, Peng P, Yang XX. Natural Terpenes as Penetration Enhancers for Transdermal Drug Delivery. Molecules 2016;21(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Cliffer KD, Siuciak JA, Carson SR, Radley HE, Park JS, Lewis DR, Zlotchenko E, Nguyen T, Garcia K, Tonra JR, Stambler N, Cedarbaum JM, Bodine SC, Lindsay RM, DiStefano PS. Physiological characterization of Taxol-induced large-fiber sensory neuropathy in the rat. Ann Neurol 1998;43(1):46–55. [DOI] [PubMed] [Google Scholar]
- [23].Cohen MM, Altman RD, Hollstrom R, Hollstrom C, Sun C, Gipson B. Safety and efficacy of intra-articular sodium hyaluronate (Hyalgan) in a randomized, double-blind study for osteoarthritis of the ankle. Foot Ankle Int 2008;29(7):657–663. [DOI] [PubMed] [Google Scholar]
- [24].Colvin LA. Chemotherapy-induced peripheral neuropathy: where are we now? Pain 2019;160 Suppl 1:S1–S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Cowman MK, Schmidt TA, Raghavan P, Stecco A. Viscoelastic Properties of Hyaluronan in Physiological Conditions. F1000Res 2015;4:622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Cuff CA, Kothapalli D, Azonobi I, Chun S, Zhang Y, Belkin R, Yeh C, Secreto A, Assoian RK, Rader DJ, Pure E. The adhesion receptor CD44 promotes atherosclerosis by mediating inflammatory cell recruitment and vascular cell activation. J Clin Invest 2001;108(7):1031–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Derry S, Conaghan P, Da Silva JA, Wiffen PJ, Moore RA. Topical NSAIDs for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev 2016;4:CD007400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Dougados M, Nguyen M, Listrat V, Amor B. High molecular weight sodium hyaluronate (hyalectin) in osteoarthritis of the knee: a 1 year placebo-controlled trial. Osteoarthritis Cartilage 1993;1(2):97–103. [DOI] [PubMed] [Google Scholar]
- [29].Dun SL, Brailoiu GC, Gao X, Brailoiu E, Arterburn JB, Prossnitz ER, Oprea TI, Dun NJ. Expression of estrogen receptor GPR30 in the rat spinal cord and in autonomic and sensory ganglia. J Neurosci Res 2009;87(7):1610–1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].El Maghraby GM, Williams AC, Barry BW. Can drug-bearing liposomes penetrate intact skin? J Pharm Pharmacol 2006;58(4):415–429. [DOI] [PubMed] [Google Scholar]
- [31].Elmorsy S, Funakoshi T, Sasazawa F, Todoh M, Tadano S, Iwasaki N. Chondroprotective effects of high-molecular-weight cross-linked hyaluronic acid in a rabbit knee osteoarthritis model. Osteoarthritis Cartilage 2014;22(1):121–127. [DOI] [PubMed] [Google Scholar]
- [32].Farquhar-Smith P Chemotherapy-induced neuropathic pain. Curr Opin Support Palliat Care 2011;5(1):1–7. [DOI] [PubMed] [Google Scholar]
- [33].Fernandes R, Mazzarello S, Hutton B, Shorr R, Majeed H, Ibrahim MF, Jacobs C, Ong M, Clemons M. Taxane acute pain syndrome (TAPS) in patients receiving taxane-based chemotherapy for breast cancer-a systematic review. Support Care Cancer 2016;24(8):3633–3650. [DOI] [PubMed] [Google Scholar]
- [34].Ferrari LF, Araldi D, Bogen O, Levine JD. Extracellular matrix hyaluronan signals via its CD44 receptor in the increased responsiveness to mechanical stimulation. Neuroscience 2016;324:390–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Ferrari LF, Khomula EV, Araldi D, Levine JD. Marked Sexual Dimorphism in the Role of the Ryanodine Receptor in a Model of Pain Chronification in the Rat. Sci Rep 2016;6:31221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Ferrari LF, Khomula EV, Araldi D, Levine JD. CD44 Signaling Mediates High Molecular Weight Hyaluronan-Induced Antihyperalgesia. J Neurosci 2018;38(2):308–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Flatters SJL, Bennett GJ. Studies of peripheral sensory nerves in paclitaxel-induced painful peripheral neuropathy: evidence for mitochondrial dysfunction. Pain 2006;122(3):245–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Funakoshi T, Yanai A, Shinoda K, Kawano MM, Mizukami Y. G protein-coupled receptor 30 is an estrogen receptor in the plasma membrane. Biochem Biophys Res Commun 2006;346(3):904–910. [DOI] [PubMed] [Google Scholar]
- [39].Furuta J, Ariyoshi W, Okinaga T, Takeuchi J, Mitsugi S, Tominaga K, Nishihara T. High molecular weight hyaluronic acid regulates MMP13 expression in chondrocytes via DUSP10/MKP5. J Orthop Res 2017;35(2):331–339. [DOI] [PubMed] [Google Scholar]
- [40].Gomis A, Miralles A, Schmidt RF, Belmonte C. Intra-articular injections of hyaluronan solutions of different elastoviscosity reduce nociceptive nerve activity in a model of osteoarthritic knee joint of the guinea pig. Osteoarthritis Cartilage 2009;17(6):798–804. [DOI] [PubMed] [Google Scholar]
- [41].Green PG, Dahlqvist SR, Isenberg WM, Miao FJ, Levine JD. Role of adrenal medulla in development of sexual dimorphism in inflammation. Eur J Neurosci 2001;14(9):1436–1444. [DOI] [PubMed] [Google Scholar]
- [42].Hamers FP, Pette C, Neijt JP, Gispen WH. The ACTH-(4–9) analog, ORG 2766, prevents taxol-induced neuropathy in rats. Eur J Pharmacol 1993;233(1):177–178. [DOI] [PubMed] [Google Scholar]
- [43].Haserodt S, Aytekin M, Dweik RA. A comparison of the sensitivity, specificity, and molecular weight accuracy of three different commercially available Hyaluronan ELISA-like assays. Glycobiology 2011;21(2):175–183. [DOI] [PubMed] [Google Scholar]
- [44].Huang TL, Chang CC, Lee CH, Chen SC, Lai CH, Tsai CL. Intra-articular injections of sodium hyaluronate (Hyalgan(R)) in osteoarthritis of the knee. a randomized, controlled, double-blind, multicenter trial in the Asian population. BMC Musculoskelet Disord 2011;12:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Junqueira LA, Polonini H, Loures S, Raposo NRB, Ferreira AO, Brandao MAF. Permeation Efficacy of a Transdermal Vehicle with Steroidal Hormones and Nonsteroidal Anti-inflammatory Agents as Model Drugs. Curr Drug Deliv 2019;16(2):136–141. [DOI] [PubMed] [Google Scholar]
- [46].Kataoka Y, Ariyoshi W, Okinaga T, Kaneuji T, Mitsugi S, Takahashi T, Nishihara T. Mechanisms involved in suppression of ADAMTS4 expression in synoviocytes by high molecular weight hyaluronic acid. Biochem Biophys Res Commun 2013;432(4):580–585. [DOI] [PubMed] [Google Scholar]
- [47].Kunitoh H, Saijo N, Furuse K, Noda K, Ogawa M. Neuromuscular toxicities of paclitaxel 210 mg m(−2) by 3-hour infusion. Br J Cancer 1998;77(10):1686–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].McWhinney SR, Goldberg RM, McLeod HL. Platinum neurotoxicity pharmacogenetics. Mol Cancer Ther 2009;8(1):10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Mestre C, Pelissier T, Fialip J, Wilcox G, Eschalier A. A method to perform direct transcutaneous intrathecal injection in rats. J Pharmacol Toxicol Methods 1994;32(4):197–200. [DOI] [PubMed] [Google Scholar]
- [50].Miaskowski C, Paul SM, Mastick J, Abrams G, Topp K, Smoot B, Kober KM, Chesney M, Mazor M, Mausisa G, Schumacher M, Conley YP, Sabes JH, Cheung S, Wallhagen M, Levine JD . Associations Between Perceived Stress and Chemotherapy-Induced Peripheral Neuropathy and Otoxicity in Adult Cancer Survivors. J Pain Symptom Manage 2018;56(1):88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, Jemal A, Kramer JL, Siegel RL. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin 2019;69(5):363–385. [DOI] [PubMed] [Google Scholar]
- [52].Mizrahy S, Raz SR, Hasgaard M, Liu H, Soffer-Tsur N, Cohen K, Dvash R, Landsman-Milo D, Bremer MG, Moghimi SM, Peer D. Hyaluronan-coated nanoparticles: the influence of the molecular weight on CD44-hyaluronan interactions and on the immune response. J Control Release 2011;156(2):231–238. [DOI] [PubMed] [Google Scholar]
- [53].Mizutani Y, Mitsutake S, Tsuji K, Kihara A, Igarashi Y. Ceramide biosynthesis in keratinocyte and its role in skin function. Biochimie 2009;91(6):784–790. [DOI] [PubMed] [Google Scholar]
- [54].Mohd F, Todo H, Yoshimoto M, Yusuf E, Sugibayashi K. Contribution of the Hair Follicular Pathway to Total Skin Permeation of Topically Applied and Exposed Chemicals. Pharmaceutics 2016;8(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Oliveira-Fusaro MCG, Zanoni CIS, Dos Santos GG, Manzo LP, Araldi D, Bonet IJM, Tambeli CH, Dias EV, Parada CA. Antihyperalgesic effect of CB1 receptor activation involves the modulation of P2X3 receptor in the primary afferent neuron. Eur J Pharmacol 2017;798:113–121. [DOI] [PubMed] [Google Scholar]
- [56].Ottillinger B, Gomor B, Michel BA, Pavelka K, Beck W, Elsasser U. Efficacy and safety of eltenac gel in the treatment of knee osteoarthritis. Osteoarthritis Cartilage 2001;9(3):273–280. [DOI] [PubMed] [Google Scholar]
- [57].Pachman DR, Qin R, Seisler DK, Smith EM, Beutler AS, Ta LE, Lafky JM, Wagner-Johnston ND, Ruddy KJ, Dakhil S, Staff NP, Grothey A, Loprinzi CL. Clinical Course of Oxaliplatin-Induced Neuropathy: Results From the Randomized Phase III Trial N08CB (Alliance). J Clin Oncol 2015;33(30):3416–3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Pappas A Epidermal surface lipids. Dermatoendocrinol 2009;1(2):72–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Parada CA, Yeh JJ, Reichling DB, Levine JD. Transient attenuation of protein kinase Cepsilon can terminate a chronic hyperalgesic state in the rat. Neuroscience 2003;120(1):219–226. [DOI] [PubMed] [Google Scholar]
- [60].Petrovchich I, Kober KM, Wagner L, Paul SM, Abrams G, Chesney MA, Topp K, Smoot B, Schumacher M, Conley YP, Hammer M, Levine JD, Miaskowski C. Deleterious Effects of Higher Body Mass Index on Subjective and Objective Measures of Chemotherapy-Induced Peripheral Neuropathy in Cancer Survivors. J Pain Symptom Manage 2019;58(2):252–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Quanhong Z, Ying X, Moxi C, Tao X, Jing W, Xin Z, Li W, Derong C, Xiaoli Z, Wei J. Intrathecal PLC(beta3) oligodeoxynucleotides antisense potentiates acute morphine efficacy and attenuates chronic morphine tolerance. Brain Res 2012;1472:38–44. [DOI] [PubMed] [Google Scholar]
- [62].Randall LO, Selitto JJ. A method for measurement of analgesic activity on inflamed tissue. Arch Int Pharmacodyn Ther 1957;111(4):409–419. [PubMed] [Google Scholar]
- [63].Rolf C, Movin T, Engstrom B, Jacobs LD, Beauchard C, Le Liboux A. An open, randomized study of ketoprofen in patients in surgery for Achilles or patellar tendinopathy. J Rheumatol 1997;24(8):1595–1598. [PubMed] [Google Scholar]
- [64].Roth SH. Letter to the editor: The importance of differentiating between topical NSAIDs. Postgrad Med 2011;123(5):251–252; author reply 253–254. [DOI] [PubMed] [Google Scholar]
- [65].Song MJ, Wang YQ, Wu GC. Additive anti-hyperalgesia of electroacupuncture and intrathecal antisense oligodeoxynucleotide to interleukin-1 receptor type I on carrageenan-induced inflammatory pain in rats. Brain Res Bull 2009;78(6):335–341. [DOI] [PubMed] [Google Scholar]
- [66].Stern R, Asari AA, Sugahara KN. Hyaluronan fragments: an information-rich system. Eur J Cell Biol 2006;85(8):699–715. [DOI] [PubMed] [Google Scholar]
- [67].Su L, Wang C, Yu YH, Ren YY, Xie KL, Wang GL. Role of TRPM8 in dorsal root ganglion in nerve injury-induced chronic pain. BMC Neurosci 2011;12:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Sun JL, Xiao C, Lu B, Zhang J, Yuan XZ, Chen W, Yu LN, Zhang FJ, Chen G, Yan M. CX3CL1/CX3CR1 regulates nerve injury-induced pain hypersensitivity through the ERK5 signaling pathway. J Neurosci Res 2013;91(4):545–553. [DOI] [PubMed] [Google Scholar]
- [69].Taiwo YO, Coderre TJ, Levine JD. The contribution of training to sensitivity in the nociceptive paw-withdrawal test. Brain Res 1989;487(1):148–151. [DOI] [PubMed] [Google Scholar]
- [70].Taiwo YO, Levine JD. Prostaglandin effects after elimination of indirect hyperalgesic mechanisms in the skin of the rat. Brain Res 1989;492(1–2):397–399. [DOI] [PubMed] [Google Scholar]
- [71].Tanishima H, Tominaga T, Kimura M, Maeda T, Shirai Y, Horiuchi T. Hyperacute peripheral neuropathy is a predictor of oxaliplatin-induced persistent peripheral neuropathy. Support Care Cancer 2017;25(5):1383–1389. [DOI] [PubMed] [Google Scholar]
- [72].Tavianatou AG, Caon I, Franchi M, Piperigkou Z, Galesso D, Karamanos NK. Hyaluronan: molecular size-dependent signaling and biological functions in inflammation and cancer. FEBS J 2019;286(15):2883–2908. [DOI] [PubMed] [Google Scholar]
- [73].Tokudome Y, Komi T, Omata A, Sekita M. A new strategy for the passive skin delivery of nanoparticulate, high molecular weight hyaluronic acid prepared by a polyion complex method. Sci Rep 2018;8(1):2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Triantaffilidou K, Venetis G, Bika O. Efficacy of hyaluronic acid injections in patients with osteoarthritis of the temporomandibular joint. A comparative study. J Craniofac Surg 2013;24(6):2006–2009. [DOI] [PubMed] [Google Scholar]
- [75].Vigetti D, Karousou E, Viola M, Deleonibus S, De Luca G, Passi A. Hyaluronan: biosynthesis and signaling. Biochim Biophys Acta 2014;1840(8):2452–2459. [DOI] [PubMed] [Google Scholar]
- [76].Vigetti D, Viola M, Karousou E, De Luca G, Passi A. Metabolic control of hyaluronan synthases. Matrix Biol 2014;35:8–13. [DOI] [PubMed] [Google Scholar]
- [77].Williams AC, Barry BW. Penetration enhancers. Adv Drug Deliv Rev 2004;56(5):603–618. [DOI] [PubMed] [Google Scholar]
- [78].Wu PT, Kuo LC, Su FC, Chen SY, Hsu TI, Li CY, Tsai KJ, Jou IM. High-molecular-weight hyaluronic acid attenuated matrix metalloproteinase-1 and −3 expression via CD44 in tendinopathy. Sci Rep 2017;7:40840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Yu YQ, Yang X, Wu XF, Fan YB. Enhancing Permeation of Drug Molecules Across the Skin via Delivery in Nanocarriers: Novel Strategies for Effective Transdermal Applications. Front Bioeng Biotechnol 2021;9:646554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Zajaczkowska R, Kocot-Kepska M, Leppert W, Wrzosek A, Mika J, Wordliczek J. Mechanisms of Chemotherapy-Induced Peripheral Neuropathy. Int J Mol Sci 2019;20(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Zurdo Schroeder I, Franke P, Schaefer UF, Lehr CM. Development and characterization of film forming polymeric solutions for skin drug delivery. Eur J Pharm Biopharm 2007;65(1):111–121. [DOI] [PubMed] [Google Scholar]


