Abstract
Background
The early management of polytrauma patients with traumatic spinal cord injury (tSCI) is a major challenge. Sparse data is available to provide optimal care in this scenario and worldwide variability in clinical practice has been documented in recent studies.
Methods
A multidisciplinary consensus panel of physicians selected for their established clinical and scientific expertise in the acute management of tSCI polytrauma patients with different specializations was established. The World Society of Emergency Surgery (WSES) and the European Association of Neurosurgical Societies (EANS) endorsed the consensus, and a modified Delphi approach was adopted.
Results
A total of 17 statements were proposed and discussed. A consensus was reached generating 17 recommendations (16 strong and 1 weak).
Conclusions
This consensus provides practical recommendations to support a clinician’s decision making in the management of tSCI polytrauma patients.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13017-023-00525-4.
Keywords: Traumatic spinal cord injury, Polytrauma, Management
Background
Traumatic spinal cord injury (tSCI) is a devastating condition associated with high mortality and morbidity [1, 2]. Falls from height and road traffic collisions are the most frequent causes of tSCI [1, 2]. In the latter scenario, an association of multisystem trauma was observed in about 80% of accidents [3]. In tSCI, as in traumatic brain injury (TBI), both primary and secondary injuries can occur; the latter, in particular, can be further exacerbated by dangerous secondary insults (such as hypoxia and hypotension) frequently observed in unstable polytrauma patients [3, 4]. Increased organ system injuries are associated with greater intrahospital mortality in polytrauma patients with cervical SCI [5, 6]. Unfortunately, few data are available regarding the acute phase management of tSCI patients with multisystem trauma. A recent survey showed a great worldwide variability in clinical practices in this setting [7]. Moreover, as in TBI, early therapeutic choices can deeply impact the outcome and prognosis of tSCI patients.
Considering the above, the specific aim of this consensus is to provide recommendations on the early management (within 24 h from trauma) of adult tSCI patients with polytrauma.
Methods
An international multidisciplinary consensus panel was composed, including neurosurgeons (n = 44), anesthesiologists/intensivists/neurointensivists (n = 23), acute care surgeons (n = 14), orthopedists (n = 3), neuroradiologists (n = 2), emergency physicians (n = 2) and neurologists (n = 1) having expertise in tSCI polytrauma care (Additional file 1: Appendix 1). The methodology used was similar to previously published consensus conferences [8, 9]. Briefly, following a non-systematic review of the literature, the steering committee (EP, CR and FC) generated a list of questions to be assessed by the panel. Two subsequent online questionnaires were administered between May and September 2023. The list of statements (17) was formulated and distributed to the panelists to allow modifications or additional statements. The analysis of voting results was performed by a non-voting experienced methodologist (CR). Statements were classified as strong recommendation, weak recommendation and no recommendation when > 85%, 75–85% and < 75% of votes were in favor, respectively. This consensus is for tSCI polytrauma patients without severe TBI. Regarding the early management of severe TBI in polytrauma patients, we refer to the 2019 World Society of Emergency Surgery (WSES) consensus conference [8]. The current consensus was endorsed jointly by the WSES and the European Association of Neurosurgical Societies (EANS).
Results
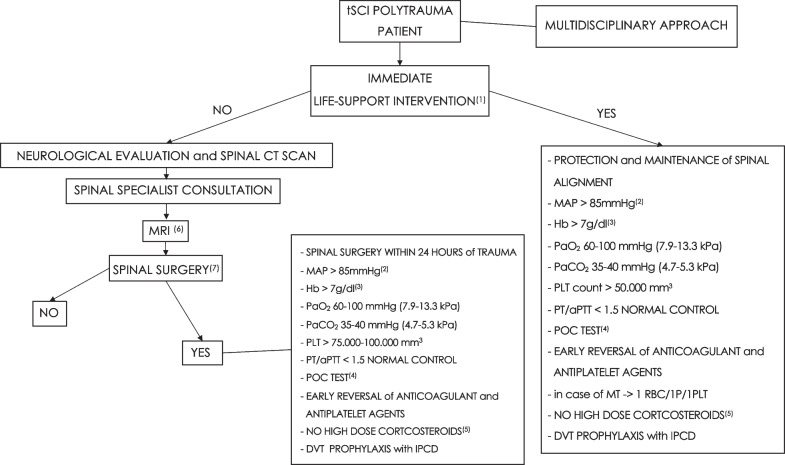
The consensus provided 17 recommendations (Table 1): 16 were strong recommendations, while 1 was a weak recommendation. The consensus algorithm is reported in Fig. 1. The consensus recommendations are listed below with the percentage of agreement.
Table 1.
List of consensus recommendations
| N | Recommendation | Level |
|---|---|---|
| 1 | We recommend that all salvageable tSCI polytrauma patients with life-threatening conditions need immediate life support interventions (e.g., intubation, mechanical ventilation, hemodynamic support, extraspinal surgery/interventional radiology for bleeding control, etc.) | Strong recommendation |
| 2 | We recommend that tSCI polytrauma patients needing extracranial interventions (e.g., surgery, interventional radiology, etc.) for life-threatening conditions require careful positioning (protection and maintenance of spine alignment) to avoid secondary insults to the injured spine | Strong recommendation |
| 3 | We recommend that tSCI polytrauma patients, without life-threatening conditions or after cardiorespiratory stabilization, need urgent neurological evaluation and imaging (i.e., spine reconstruction from a whole-body CT scan) | Strong recommendation |
| 4 | We recommend, in tSCI polytrauma patients (without life-threatening conditions or after cardiorespiratory stabilization), to perform spine MRI after spinal specialist consultation to determine the severity of spinal cord damage and aid in surgical decision making | Strong recommendation |
| 5 | We recommend, in all salvageable tSCI polytrauma patients with surgical spinal lesions, after control of life-threatening conditions, to consider an urgent intervention (decompression/spine stabilization), possibly within 24 h from trauma | Strong recommendation |
| 6 | We recommend the maintenance of a MAP > 85 mmHg during interventions for life-threatening hemorrhage or emergency spinal surgery. In case of difficult intraoperative bleeding control, lower values could be tolerated for the shortest possible time | Strong recommendation |
| 7 | We recommend that the Hb level, during interventions for life-threatening hemorrhage or emergency spinal surgery, be adjusted according to a patient's tolerance to anemia. An Hb < 7 g/dl should promptly trigger RBCTs. A higher threshold for RBCTs could be used in patients "at risk" (e.g., elderly and/or with limited cardiovascular reserve because of pre-existing heart disease, etc.) | Strong recommendation |
| 8 | We recommend the maintenance of a PaO2 between 60 and 100 mmHg (7.9–13.3 kPa) during interventions for life-threatening hemorrhage or emergency spinal surgery | Strong recommendation |
| 9 | We recommend the maintenance of a PaCO2 between 35 and 40 mmHg (4.7–5.3 kPa) during interventions for life-threatening hemorrhage or emergency spinal surgery | Strong recommendation |
| 10 | In case of interventions for life-threatening hemorrhage, we recommend the maintenance of a PLT count > 50.000/mm3. In the case of spinal surgery (decompression/stabilization), a higher value (75.000–100.000/mm3) would be advisable | Strong recommendation |
| 11 | We recommend the maintenance of a PT/aPTT value < 1.5 normal control during interventions for life-threatening hemorrhage or emergency spinal surgery | Strong recommendation |
| 12 | We recommend, if available, the utilization of POC tests (e.g., TEG, ROTEM, etc.) to assess and optimize the coagulation function during interventions for life-threatening hemorrhage or emergency spinal surgery | Weak recommendation |
| 13 | We recommend the early reversal of anticoagulant/antiplatelet agents in all salvageable tSCI polytrauma patients needing interventions for life-threatening hemorrhage or emergency spinal surgery | Strong recommendation |
| 14 | In adult patients with tSCI and polytrauma, we recommend the transfusion of RBCs/Plasma/PLTs at a ratio of 1/1/1 during massive transfusion protocol initiation. Afterward, this ratio can be modified according to laboratory values | Strong recommendation |
| 15 | We recommend against high-dose corticosteroid therapy (e.g., NASCIS I-III) in tSCI patients and polytrauma | Strong recommendation |
| 16 | We recommend DVT prophylaxis with intermittent pneumatic compression devices (if available and feasible) as soon as possible after tSCI and polytrauma | Strong recommendation |
| 17 | We recommend a strict collaboration between the different medical specialties (e.g., critical care medicine, acute care surgery, neurosurgery, neurology, emergency medicine, orthopedics, etc.) involved in the early management of tSCI patients with polytrauma | Strong recommendation |
tSCI Traumatic spinal cord injury, CT Computed tomography, MRI Magnetic resonance imaging, MAP Mean arterial pressure, Hb Hemoglobin, RBC Red blood cell, RBCT RBC transfusion, PLT Platelet, PT Prothrombin time, aPTT Activated partial thromboplastin time, POC Point-of-care, TEG Thromboelastography, ROTEM Rotational thromboelastometry, PaCO2 Arterial partial pressure of carbon dioxide, PaO2 Arterial partial pressure of oxygen, NASCIS National Acute Spinal Cord Injury Study
Fig. 1.
Consensus flowchart. (1) intubation, mechanical ventilation, hemodynamic support, extraspinal surgery/interventional radiology for bleeding control, etc. (2) In case of difficult intraoperative bleeding control, lower values could be tolerated for the shortest possible time. (3) higher values in patients "at risk" (e.g., elderly and/or with limited cardiovascular reserve because of pre-existing heart disease, etc.). (4) if available (e.g., TEG, ROTEM, etc.). (5) as utilized in NABISC I-III studies. (6) in order to determine the severity of spinal cord damage and aid in surgical decision making. (7) decompression and/or stabilization. tSCI = Traumatic spinal cord injury, CT = Computed tomography, MRI = Magnetic resonance imaging, MAP = Mean arterial pressure, Hb = Hemoglobin, PaO2 = Arterial partial pressure of oxygen, PaCO2 = Arterial partial pressure of carbon dioxide, PLT = Platelet, PT = Prothrombin time, aPTT = Activated partial thromboplastin time, POC = Point-of-care, P = Plasma, RBC = Red blood cell, MT = Massive transfusion, DVT = Deep vein thrombosis, IPCD = Intermittent pneumatic compression device
Recommendation 1
We recommend that all salvageable tSCI polytrauma patients with life-threatening conditions need immediate life support interventions (e.g., intubation, mechanical ventilation, hemodynamic support, extraspinal surgery/interventional radiology for bleeding control, etc.) (agreement: 98.9%, strong recommendation).
Recommendation 2
We recommend that tSCI polytrauma patients needing extracranial interventions (e.g., surgery, interventional radiology, etc.) for life-threatening conditions require careful positioning (protection and maintenance of spine alignment) to avoid secondary insults to the injured spine (agreement: 100%, strong recommendation).
Recommendation 3
We recommend that tSCI polytrauma patients, without life-threatening conditions or after cardiorespiratory stabilization, need urgent neurological evaluation and imaging [i.e., spine reconstruction from a whole-body computed tomography (CT) scan] (agreement: 95.5%, strong recommendation).
Recommendation 4
We recommend, in tSCI polytrauma patients (without life-threatening conditions or after cardiorespiratory stabilization), to perform spine magnetic resonance imaging (MRI) after spinal specialist consultation to determine the severity of spinal cord damage and aid in surgical decision making (agreement: 95.5%, strong recommendation).
Recommendation 5
We recommend, in all salvageable tSCI polytrauma patients with surgical spinal lesions, after control of life-threatening conditions, to consider an urgent intervention (decompression/spine stabilization), possibly within 24 h from trauma (agreement: 92%, strong recommendation).
Recommendation 6
We recommend the maintenance of a mean arterial pressure (MAP) > 85 mmHg during interventions for life-threatening hemorrhage or emergency spinal surgery. In case of difficult intraoperative bleeding control, lower values could be tolerated for the shortest possible time (agreement: 88.6%, strong recommendation).
Recommendation 7
We recommend that the hemoglobin (Hb) level, during interventions for life-threatening hemorrhage or emergency spinal surgery, be adjusted according to patient's tolerance to anemia. An Hb < 7 g/dl should promptly trigger red blood cell transfusions (RBCTs). A higher threshold for RBCTs could be used in patients "at risk" (e.g., elderly and/or with limited cardiovascular reserve because of pre-existing heart disease, etc.) (agreement: 92%, strong recommendation).
Recommendation 8
We recommend the maintenance of an arterial partial pressure of oxygen (PaO2) between 60 and 100 mmHg (7.9–13.3 kPa) during interventions for life-threatening hemorrhage or emergency spinal surgery (agreement: 93.2%, strong recommendation).
Recommendation 9
We recommend the maintenance of an arterial partial pressure of carbon dioxide (PaCO2) between 35 and 40 mmHg (4.7–5.3 kPa) during interventions for life-threatening hemorrhage or emergency spinal surgery (agreement: 93.2%, strong recommendation).
Recommendation 10
In case of interventions for life-threatening hemorrhage, we recommend the maintenance of a platelet (PLT) count > 50.000/mm3. In the case of spinal surgery (decompression/stabilization), a higher value (75.000–100.000/mm3) would be advisable (agreement: 93.2%, strong recommendation).
Recommendation 11
We recommend the maintenance of a prothrombin time (PT)/activated partial thromboplastin time (aPTT) value < 1.5 normal control during interventions for life-threatening hemorrhage or emergency spinal surgery (agreement: 92%, strong recommendation).
Recommendation 12
We recommend, if available, the utilization of point-of-care (POC) tests [e.g., thromboelastography (TEG), rotational thromboelastometry (ROTEM), etc.] to assess and optimize the coagulation function during interventions for life-threatening hemorrhage or emergency spinal surgery (agreement: 84.1%, weak recommendation).
Recommendation 13
We recommend the early reversal of anticoagulant/antiplatelet agents in all salvageable tSCI polytrauma patients needing interventions for life-threatening hemorrhage or emergency spinal surgery (agreement: 92%, strong recommendation).
Recommendation 14
In adult patients with tSCI and polytrauma, we recommend the transfusion of RBCs/Plasma/PLTs at a ratio of 1/1/1 during massive transfusion protocol initiation. Afterward, this ratio can be modified according to laboratory values (agreement: 94.3%, strong recommendation).
Recommendation 15
We recommend against high-dose corticosteroid therapy (i.e., National Acute Spinal Cord Injury Study (NASCIS) I-III [10–12]) in tSCI patients and polytrauma (agreement: 89.8%, strong recommendation).
Recommendation 16
We recommend deep vein thrombosis (DVT) prophylaxis with intermittent pneumatic compression devices (if available and feasible) as soon as possible after tSCI and polytrauma (agreement: 94.3%, strong recommendation).
Recommendation 17
We recommend a strict collaboration between the different medical specialties (e.g., critical care medicine, acute care surgery, neurosurgery, neurology, emergency medicine, orthopedics, etc.) involved in the early management of tSCI patients with polytrauma (agreement: 98.9%, strong recommendation).
Discussion
Cardiorespiratory management and bleeding control in tSCI polytrauma patients
Life-threatening hemorrhage is a major preventable cause of early death after trauma [13]. Bleeding control with circulating blood volume restoration is a priority in polytrauma care and the main goal of damage control strategies [14, 15]. Arterial hypotension and hypoxia are frequently observed after isolated tSCI, especially when the injury occurs at high spinal cord levels [1]. These secondary insults, associated with an unfavorable neurological outcome, may occur further in severe polytrauma patients [1, 3]. The most recent guidelines by the Congress of Neurological Surgeons (CNS) for managing tSCI patients recommend maintaining MAP between 85 and 90 mmHg for the first 7 days following an acute cervical SCI (Level III) [16]. These values are difficult to obtain in the acute phase management of bleeding polytrauma patients, also considering the worldwide increase in the utilization of permissive hypotension in the setting of damage control resuscitation [14]. Considering the above, we recommend the maintenance of a MAP > 85 mmHg during interventions for life-threatening hemorrhage or emergency spinal surgery. However, in case of difficult intraoperative bleeding control, we suggest tolerating lower values for the time strictly necessary to achieve bleeding control. Some panelists suggested individualizing an arterial pressure target, considering the spinal cord perfusion pressure (SCPP) [17]. To obtain this, it is necessary to monitor the intraspinal pressure (ISP) by surgically implanting an intradural extramedullary probe at the injury site [17]. Increased SCPP is associated with decreased spinal cord ischemia and favorable neurological outcomes [18–22]. At present, more data are necessary to spread this promising type of monitoring into daily clinical practice. Data about optimal Hb values in tSCI are lacking [16, 23]. We recommend RBCTs in case of Hb < 7 g/dl according to current guidelines [8, 24] and the tolerance to anemia; in this regard, a higher Hb threshold could be used in patients "at risk" (e.g., elderly and/or with limited cardiovascular reserve because of pre-existing heart disease, etc.). As for Hb values, data regarding optimal PaO2 and PaCO2 targets in this setting are lacking. Our recommendations are probably influenced by what is suggested in patients with acute brain damage [25].
Imaging and spinal surgery timing
Whole-body CT scan can be considered a crucial standard diagnostic tool in the acute management of severely injured patients [26, 27]. CT scan is also recommended as the initial imaging modality evaluation of tSCI [28, 29]. Spine reconstruction from a whole-body CT scan can be quickly obtained, limiting the waste of time in the potentially challenging polytrauma setting [30]. Precisely, for the cervical spine, the appropriate standard is a thin slice helical CT scan from the base of the skull to at least the first thoracic vertebra (T1) with both sagittal and coronal reconstructions [30]. This examination should be undertaken as standard practice with the first CT brain scan in all head-injured patients with an altered level of consciousness [30]. The remaining thoracic and lumbar spine may be adequately imaged by sagittal and coronal reformatting of helical CT scans of the chest, abdomen and pelvis as part of a modern CT trauma series [30]. CT provides important information regarding bone pathology (e.g., fractures), disk herniations and epidural/subdural hematomas [28–30]. MRI, allowing a precise evaluation of the spinal cord and related soft tissues, is considered the imaging modality of choice for the evaluation of tSCI patients and for the decision of final neurosurgical/spinal treatment [30, 31]. Recent guidelines suggest MRI examination: (a) before surgical intervention, when feasible, to facilitate improved clinical decision making (Quality of Evidence: Very Low, Strength of Recommendation: Weak) and (b) in the acute period following SCI, before or after surgical intervention, to improve prediction of neurological outcome (Quality of Evidence: Low Strength of Recommendation: Weak) [31]. MRI requires more time from execution with respect to CT scan and can be challenging in cardiorespiratory unstable polytrauma patients. Precise MRI indications and timing in tSCI patients are not clearly defined, and in this regard, more studies are necessary. In the meantime, we recommend performing spine MRI after cardiorespiratory stabilization and spinal specialist consultation to determine the severity of spinal cord damage and aid in surgical decision making. Early decompressive surgery (performed within 24 h from trauma) seems to be associated with better neurological outcomes, highlighting the concept of “time is spine” [32–34]. A more rapid approach (within 12 h or less—“ultra-early”) was also proposed, especially in the case of incomplete spinal lesion [34]. Recent guidelines suggest early surgery (< 24 h after injury) as a treatment option for adult acute SCI patients, regardless of level (Quality of Evidence: Low. Strength of Recommendation: Weak) [35]. Some panelists suggest a wider timing in case of spinal fracture needing surgical stabilization in the absence of neural compression. The optimal timing of spinal surgery in tSCI polytrauma patients must be established and probably individualized according to clinical needs and after intracranial, hemodynamic and respiratory stabilization.
Coagulation management
In bleeding polytrauma patients, an attempt is generally made to maintain PT/aPTT < 1.5 times the normal control and the PLT count > 50,000/mm3 [31]. A PLT count > 100,000/mm3 was recommended for patients with ongoing bleeding and/or TBI and in the case of neurosurgery [24, 36]. POC tests (i.e., TEG, ROTEM, etc.) are increasingly used to evaluate coagulation function in bleeding trauma patients [24]. These tests are useful for a rapid and precise assessment of hemostasis and to provide critical information about specific coagulation deficiencies, especially in patients taking novel oral anticoagulants (NOACs) and in the evaluation of PLTs dysfunction induced by trauma and/or drugs [24]. Several published guidelines about the reversal of anticoagulant/antiplatelets in different settings are available; these, especially regarding antiplatelet drug reversal, provide conflicting indications [24, 37–39]. To our knowledge, no specific guidelines about coagulation management in tSCI patients have been published until now. More studies are needed to provide robust recommendations in this setting. Meanwhile, we recommend the early reversal of anticoagulant/antiplatelet agents in tSCI polytrauma patients needing interventions for life-threatening hemorrhage or emergency spinal surgery. Massive transfusion is frequently utilized in bleeding trauma patients [14, 40]. The pragmatic randomized optimal platelet and plasma ratios (PROPPR) study, involving 680 trauma patients with major bleeding, was performed to determine the safety and the effectiveness of a transfusion strategy involving plasma, PLTs and RBCs in a 1:1:1 ratio compared with a 1:1:2 ratio. None of the studied strategies resulted in significant differences in mortality. However, patients in the 1:1:1 group achieved hemostasis with fewer deaths due to exsanguination within the first 24 hours [41]. Some of our panelists suggest, as an alternative to this strategy, the utilization of whole blood transfusion as indicated in a recently published clinical protocol for damage control resuscitation by the American Association for the Surgery of Trauma (AAST) and the American College of Surgeons Committee on Trauma (ACS-COT) [14]. No data are available regarding trauma coagulopathy and the progression of tSCI. Therefore, we recommend initiating a transfusion protocol of RBCs/plasma/PLTs at a ratio of 1:1:1. This ratio may be modified afterward according to laboratory values. Patients with SCI are at increased risk of developing venous thromboembolism after trauma [42]. Early initiation of mechanical thromboprophylaxis with intermittent pneumatic compression was recommended in immobile trauma patients with elevated bleeding risk [24, 43]. In this regard, we recommend DVT prophylaxis with intermittent pneumatic compression devices (if available and feasible) as soon as possible after tSCI and polytrauma. The initiation of pharmacologic DVT prophylaxis should be considered within 48 h of injury or spine surgery, as suggested by recent published guidelines [43].
Corticosteroid therapy
The utilization of corticosteroid therapy with methylprednisolone sodium succinate (MPSS) after tSCI is a highly debated and controversial topic [2, 7, 10–12]. Specifically, CNS guidelines do not recommend its use [44], whereas AO spine guidelines suggest: (1) “not offering a 24-h infusion of high-dose MPSS to adult patients who present after 8 h with acute SCI”; (2) “a 24-h infusion of high-dose MPSS to adult patients within 8 h of acute SCI as a treatment option” and (3) “not offering a 48-h infusion of high-dose MPSS to adult patients with acute SCI” [45]. We strongly recommend against routine high-dose corticosteroid therapy as proposed in NASCIS I-III studies [10–12]. Some panelists are in favor of the use of corticosteroids at lower doses or in certain patients who may have a favorable risk/benefit ratio. This topic requires further studies, especially in a challenging scenario such as tSCI in polytrauma.
Notes on the use of the current consensus
This consensus aims to support clinicians’ decision making in the early management of tSCI patients with polytrauma in the first 24 h after injury. The included statements are created to assist a physician’s clinical judgment, which is necessary to provide appropriate (personalized) therapy. Considering the lack of high-quality studies in this setting, we adopted a modified Delphi approach involving experts from different countries worldwide; this approach is less rigorous than evidence-based guidelines. However, our methodology can provide useful and practical recommendations for this challenging clinical scenario. The guidelines promulgated in this work do not represent a standard of practice and have no legal implications. They are suggested plans of care based on the best available evidence and the consensus of experts, but they do not exclude other approaches as being within the standard of practice. Ultimately, responsibility for treatment results rests with those directly engaged therein and not with the consensus group. Moreover, as recommended, we think that a strict collaboration between different medical specialties (i.e., a multidisciplinary approach) is of paramount importance for improving the outcome of these patients. This aspect is of great importance not only in the first 24 h after trauma but also in the long-term care (i.e., high-quality neurorehabilitation).
Conclusion
In the future, more studies should be encouraged to improve clinical outcomes for polytrauma patients with tSCI. This international multidisciplinary consensus conference was created to provide practical recommendations to deliver the best early possible care for tSCI polytrauma patients in the first 24 h after injury.
Supplementary Information
Acknowledgements
We would like to thank WSES/EANS for the collaboration and support.
Abbreviations
- SCI
Spinal cord injury
- tSCI
Traumatic spinal cord injury
- WSES
World Society of Emergency Surgery
- EANS
European Association of Neurosurgical Societies
- TBI
Traumatic brain injury
- CT
Computed tomography
- MRI
Magnetic resonance imaging
- MAP
Mean arterial pressure
- Hb
Hemoglobin
- RBCT
Red blood cell transfusion
- PaO2
Arterial partial pressure of oxygen.
- PaCO2
Arterial partial pressure of carbon dioxide.
- PLT
Platelet
- PT
Prothrombin time
- aPTT
Activated partial thromboplastin time.
- POC
Point-of-care
- TEG
Thromboelastography
- ROTEM
Rotational thromboelastometry
- NASCIS
National acute spinal cord injury study
- DVT
Deep vein thrombosis
- CNS
Congress of neurological surgeons
- SCPP
Spinal cord perfusion pressure
- ISP
Intraspinal pressure
- T1
First thoracic vertebra.
- NOAC
Novel oral anticoagulant
- PROPPR
Pragmatic randomized optimal platelet and plasma ratios
- AAST
American Association for the Surgery of Trauma
- ACS-COT
American College of Surgeons Committee on Trauma
- DVT
Deep vein thrombosis
- MPSS
Methylprednisolone sodium succinate
Author contributions
EP, AKD, CR and FC have designed the study. CR has performed acquisition of data. CR has done the analysis and interpretation of data. EP, AKD, CR and FC have drafted the article. All authors have revised it critically for important intellectual content. All authors have given final approval of the version to be submitted.
Funding
None.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
AWK serves as the PI of the COOL trial, which previously was partially supported by the 3M/Acelity Corporation until August 2022. AWK is also a member of the Canadian Forces Medical Services and has consulted for the 3M/Acelity Corporation, Zoll Medical, Innovative Trauma Care and CSL Behring. AWK is the Director of the TeleMentored Ultrasound Supported Medical Interventions (TMUSMI) Research group and serves in the Canadian Forces Medical Services. IH receives funding from the Finnish Medical Foundation, the Päivikki and Sakari Sohlberg Foundation, the Paulo Foundation and the Finnish Cultural Foundation. PJH is supported by the UK NIHR-Senior Investigator Award, Cambridge BRC, Brain Injury Medtech Co-operative, Global Health Research Group on Acquired Brain and Spine Injury and the Royal College of Surgeons of England.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ahuja CS, Wilson JR, Nori S, Kotter MRN, Druschel C, Curt A, Fehlings MG. Traumatic spinal cord injury. Nat Rev Dis Prim. 2017;3:17018. doi: 10.1038/nrdp.2017.18. [DOI] [PubMed] [Google Scholar]
- 2.Eli I, Lerner DP, Ghogawala Z. Acute traumatic spinal cord injury. Neurol Clin. 2021;39(2):471–488. doi: 10.1016/j.ncl.2021.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Yue JK, Winkler EA, Rick JW, Deng H, Partow CP, Upadhyayula PS, Birk HS, Chan AK, Dhall SS. Update on critical care for acute spinal cord injury in the setting of polytrauma. Neurosurg Focus. 2017;43(5):E19. doi: 10.3171/2017.7.FOCUS17396. [DOI] [PubMed] [Google Scholar]
- 4.Hachem LD, Ahuja CS, Fehlings MG. Assessment and management of acute spinal cord injury: from point of injury to rehabilitation. J Spinal Cord Med. 2017;40(6):665–675. doi: 10.1080/10790268.2017.1329076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alvarez Reyes A, Hurlbert RJ, Dumont TM, Ramey WL. The Number of organ system injuries is a predictor of intrahospital mortality in complete cervical spinal cord injury. World Neurosurg. 2022;158:e788–e792. doi: 10.1016/j.wneu.2021.11.063. [DOI] [PubMed] [Google Scholar]
- 6.Marchesini N, Demetriades AK, Peul WC, Tommasi N, Zanatta P, Pinna G, Sala F. Concomitant trauma of brain and upper cervical spine: lessons in injury patterns and outcomes. Eur J Trauma Emerg Surg. 2023 doi: 10.1007/s00068-023-02278-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Picetti E, Iaccarino C, Coimbra R, Abu-Zidan F, Tebala GD, Balogh ZJ, Biffl WL, Coccolini F, Gupta D, Maier RV, Marzi I, Robba C, Sartelli M, Servadei F, Stahel PF, Taccone FS, Unterberg AW, Antonini MV, Galante JM, Ansaloni L, Kirkpatrick AW, Rizoli S, Leppaniemi A, Chiara O, De Simone B, Chirica M, Shelat VG, Fraga GP, Ceresoli M, Cattani L, Minardi F, Tan E, Wani I, Petranca M, Domenichelli F, Cui Y, Malchiodi L, Sani E, Litvin A, Hecker A, Montanaro V, Beka SG, Di Saverio S, Rossi S, Catena F. The acute phase management of spinal cord injury affecting polytrauma patients: the ASAP study. World J Emerg Surg. 2022;17(1):20. doi: 10.1186/s13017-022-00422-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Picetti E, Rossi S, Abu-Zidan FM, Ansaloni L, Armonda R, Baiocchi GL, Bala M, Balogh ZJ, Berardino M, Biffl WL, Bouzat P, Buki A, Ceresoli M, Chesnut RM, Chiara O, Citerio G, Coccolini F, Coimbra R, Di Saverio S, Fraga GP, Gupta D, Helbok R, Hutchinson PJ, Kirkpatrick AW, Kinoshita T, Kluger Y, Leppaniemi A, Maas AIR, Maier RV, Minardi F, Moore EE, Myburgh JA, Okonkwo DO, Otomo Y, Rizoli S, Rubiano AM, Sahuquillo J, Sartelli M, Scalea TM, Servadei F, Stahel PF, Stocchetti N, Taccone FS, Tonetti T, Velmahos G, Weber D, Catena F. WSES consensus conference guidelines: monitoring and management of severe adult traumatic brain injury patients with polytrauma in the first 24 hours. World J Emerg Surg. 2019;29(14):53. doi: 10.1186/s13017-019-0270-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Picetti E, Catena F, Abu-Zidan F, Ansaloni L, Armonda RA, Bala M, Balogh ZJ, Bertuccio A, Biffl WL, Bouzat P, Buki A, Cerasti D, Chesnut RM, Citerio G, Coccolini F, Coimbra R, Coniglio C, Fainardi E, Gupta D, Gurney JM, Hawryluk GWJ, Helbok R, Hutchinson PJA, Iaccarino C, Kolias A, Maier RW, Martin MJ, Meyfroidt G, Okonkwo DO, Rasulo F, Rizoli S, Rubiano A, Sahuquillo J, Sams VG, Servadei F, Sharma D, Shutter L, Stahel PF, Taccone FS, Udy A, Zoerle T, Agnoletti V, Bravi F, De Simone B, Kluger Y, Martino C, Moore EE, Sartelli M, Weber D, Robba C. Early management of isolated severe traumatic brain injury patients in a hospital without neurosurgical capabilities: a consensus and clinical recommendations of the World Society of Emergency Surgery (WSES) World J Emerg Surg. 2023;18(1):5. doi: 10.1186/s13017-022-00468-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bracken MB, Shepard MJ, Hellenbrand KG, Collins WF, Leo LS, Freeman DF, Wagner FC, Flamm ES, Eisenberg HM, Goodman JH, et al. Methylprednisolone and neurological function 1 year after spinal cord injury Results of the National Acute Spinal Cord Injury Study. J Neurosurg. 1985;63(5):704–713. doi: 10.3171/jns.1985.63.5.0704. [DOI] [PubMed] [Google Scholar]
- 11.Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS, Eisenberg HM, Flamm E, Leo-Summers L, Maroon J, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med. 1990;322(20):1405–1411. doi: 10.1056/NEJM199005173222001. [DOI] [PubMed] [Google Scholar]
- 12.Bracken MB, Shepard MJ, Holford TR, Leo-Summers L, Aldrich EF, Fazl M, Fehlings M, Herr DL, Hitchon PW, Marshall LF, Nockels RP, Pascale V, Perot PL, Jr, Piepmeier J, Sonntag VK, Wagner F, Wilberger JE, Winn HR, Young W. Administration of methylprednisolone for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury. Results of the Third National Acute Spinal Cord Injury Randomized Controlled Trial. National Acute Spinal Cord Injury Study. JAMA. 1997;277(20):1597–1604. [PubMed] [Google Scholar]
- 13.Callcut RA, Kornblith LZ, Conroy AS, Robles AJ, Meizoso JP, Namias N, Meyer DE, Haymaker A, Truitt MS, Agrawal V, Haan JM, Lightwine KL, Porter JM, San Roman JL, Biffl WL, Hayashi MS, Sise MJ, Badiee J, Recinos G, Inaba K, Schroeppel TJ, Callaghan E, Dunn JA, Godin S, McIntyre RC Jr, Peltz ED, OʼNeill PJ, Diven CF, Scifres AM, Switzer EE, West MA, Storrs S, Cullinane DC, Cordova JF, Moore EE, Moore HB, Privette AR, Eriksson EA, Cohen MJ; Western Trauma Association Multicenter Study Group The why and how our trauma patients die: a prospective. Multicenter Western Trauma Association study. J Trauma Acute Care Surg. 2019;86(5):864–870. doi: 10.1097/TA.0000000000002205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.LaGrone L, Stein D, Cribari C, Kaups K, Harris C, Miller AN, Smith B, Dutton R, Bulger E, Napolitano LM. American association for the surgery of trauma (AAST)/American College of Surgeons Committee on Trauma (ACS-COT): Clinical Protocol for Damage Control Resuscitation for the Adult Trauma Patient. J Trauma Acute Care Surg. 2023 doi: 10.1097/TA.0000000000004088. [DOI] [PubMed] [Google Scholar]
- 15.Risinger WB, Smith JW. Damage control surgery in emergency general surgery: what you need to know. J Trauma Acute Care Surg. 2023 doi: 10.1097/TA.0000000000004112. [DOI] [PubMed] [Google Scholar]
- 16.Ryken TC, Hurlbert RJ, Hadley MN, Aarabi B, Dhall SS, Gelb DE, Rozzelle CJ, Theodore N, Walters BC. The acute cardiopulmonary management of patients with cervical spinal cord injuries. Neurosurgery. 2013;72(Suppl 2):84–92. doi: 10.1227/NEU.0b013e318276ee16. [DOI] [PubMed] [Google Scholar]
- 17.Saadoun S, Papadopoulos MC. Acute, severe traumatic spinal cord injury: monitoring from the injury site and expansion duraplasty. Neurosurg Clin N Am. 2021;32(3):365–376. doi: 10.1016/j.nec.2021.03.008. [DOI] [PubMed] [Google Scholar]
- 18.Squair JW, Bélanger LM, Tsang A, Ritchie L, Mac-Thiong JM, Parent S, Christie S, Bailey C, Dhall S, Street J, Ailon T, Paquette S, Dea N, Fisher CG, Dvorak MF, West CR, Kwon BK. Spinal cord perfusion pressure predicts neurologic recovery in acute spinal cord injury. Neurology. 2017;89(16):1660–1667. doi: 10.1212/WNL.0000000000004519. [DOI] [PubMed] [Google Scholar]
- 19.Visagan R, Hogg FRA, Gallagher MJ, Kearney S, Zoumprouli A, Papadopoulos MC, Saadoun S. Monitoring spinal cord tissue oxygen in patients with acute, severe traumatic spinal cord injuries. Crit Care Med. 2022;50(5):e477–e486. doi: 10.1097/CCM.0000000000005433. [DOI] [PubMed] [Google Scholar]
- 20.Hogg FRA, Kearney S, Solomon E, Gallagher MJ, Zoumprouli A, Papadopoulos MC, Saadoun S. Acute, severe traumatic spinal cord injury: improving urinary bladder function by optimizing spinal cord perfusion. J Neurosurg Spine. 2021;36(1):145–152. doi: 10.3171/2021.3.SPINE202056. [DOI] [PubMed] [Google Scholar]
- 21.Hogg FRA, Kearney S, Gallagher MJ, Zoumprouli A, Papadopoulos MC, Saadoun S. Spinal cord perfusion pressure correlates with anal sphincter function in a cohort of patients with acute, severe traumatic spinal cord injuries. Neurocrit Care. 2021;35(3):794–805. doi: 10.1007/s12028-021-01232-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Visagan R, Boseta E, Zoumprouli A, Papadopoulos MC, Saadoun S. Spinal cord perfusion pressure correlates with breathing function in patients with acute, cervical traumatic spinal cord injuries: an observational study. Crit Care. 2023;27(1):362. doi: 10.1186/s13054-023-04643-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fehlings MG, Tetreault LA, Wilson JR, Kwon BK, Burns AS, Martin AR, Haw-ryluk G, Harrop JS. A clinical practice guideline for the management of acute spinal cord injury: introduction, rationale, and scope. Global Spine J. 2017;7(3Suppl):84S–94S. doi: 10.1177/2192568217703387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rossaint R, Afshari A, Bouillon B, Cerny V, Cimpoesu D, Curry N, Duranteau J, Filipescu D, Grottke O, Grønlykke L, Harrois A, Hunt BJ, Kaserer A, Komadina R, Madsen MH, Maegele M, Mora L, Riddez L, Romero CS, Samama CM, Vincent JL, Wiberg S, Spahn DR. The European guideline on management of major bleeding and coagulopathy following trauma: sixth edition. Crit Care. 2023;27(1):80. doi: 10.1186/s13054-023-04327-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robba C, Poole D, McNett M, Asehnoune K, Bösel J, Bruder N, Chieregato A, Cinotti R, Duranteau J, Einav S, Ercole A, Ferguson N, Guerin C, Siempos II, Kurtz P, Juffermans NP, Mancebo J, Mascia L, McCredie V, Nin N, Oddo M, Pelosi P, Rabinstein AA, Neto AS, Seder DB, Skrifvars MB, Suarez JI, Taccone FS, van der Jagt M, Citerio G, Stevens RD. Mechanical ventilation in patients with acute brain injury: recommendations of the European Society of Intensive Care Medicine consensus. Intensive Care Med. 2020;46(12):2397–2410. doi: 10.1007/s00134-020-06283-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huber-Wagner S, Kanz KG, Hanschen M, van Griensven M, Biberthaler P, Lefering R. Whole-body computed tomography in severely injured patients. Curr Opin Crit Care. 2018;24(1):55–61. doi: 10.1097/MCC.0000000000000474. [DOI] [PubMed] [Google Scholar]
- 27.Wirth S, Hebebrand J, Basilico R, Berger FH, Blanco A, Calli C, Dumba M, Linsenmaier U, Mück F, Nieboer KH, Scaglione M, Weber MA, Dick E. European society of emergency radiology: guideline on radiological polytrauma imaging and service (short version) Insights Imaging. 2020;11(1):135. doi: 10.1186/s13244-020-00947-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Daffner RH, Hackney DB. ACR appropriateness criteria on suspected spine trauma. J Am Coll Radiol. 2007;4(11):762–775. doi: 10.1016/j.jacr.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 29.Ryken TC, Hadley MN, Walters BC, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Rozzelle CJ, Theodore N. Radiographic assessment. Neurosurgery. 2013;72(Suppl 2):54–72. doi: 10.1227/NEU.0b013e318276edee. [DOI] [PubMed] [Google Scholar]
- 30.Shabani S, Meyer BP, Budde MD, Wang MC. Diagnostic imaging in spinal cord injury. Neurosurg Clin N Am. 2021;32(3):323–331. doi: 10.1016/j.nec.2021.03.004. [DOI] [PubMed] [Google Scholar]
- 31.Fehlings MG, Martin AR, Tetreault LA, Aarabi B, Anderson P, Arnold PM, Brodke D, Burns AS, Chiba K, Dettori JR, Furlan JC, Hawryluk G, Holly LT, Howley S, Jeji T, Kalsi-Ryan S, Kotter M, Kurpad S, Kwon BK, Marino RJ, Massicotte E, Merli G, Middleton JW, Nakashima H, Nagoshi N, Palmieri K, Singh A, Skelly AC, Tsai EC, Vaccaro A, Wilson JR, Yee A, Harrop JS. A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on the role of baseline magnetic resonance imaging in clinical decision making and outcome prediction. Global Spine J. 2017;7(3 Suppl):221S–230S. doi: 10.1177/2192568217703089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Badhiwala JH, Wilson JR, Witiw CD, Harrop JS, Vaccaro AR, Aarabi B, Grossman RG, Geisler FH, Fehlings MG. The influence of timing of surgical decompression for acute spinal cord injury: a pooled analysis of individual patient data. Lancet Neurol. 2021;20(2):117–126. doi: 10.1016/S1474-4422(20)30406-3. [DOI] [PubMed] [Google Scholar]
- 33.Hsieh YL, Tay J, Hsu SH, Chen WT, Fang YD, Liew CQ, Chou EH, Wolfshohl J, d’Etienne J, Wang CH, Tsuang FY. Early versus late surgical decompression for traumatic spinal cord injury on neurological recovery: a systematic review and meta-analysis. J Neurotrauma. 2021;38(21):2927–2936. doi: 10.1089/neu.2021.0102. [DOI] [PubMed] [Google Scholar]
- 34.Quddusi A, Pedro KM, Alvi MA, Hejrati N, Fehlings MG. Early surgical intervention for acute spinal cord injury: time is spine. Acta Neurochir (Wien) 2023;165(9):2665–2674. doi: 10.1007/s00701-023-05698-0. [DOI] [PubMed] [Google Scholar]
- 35.Fehlings MG, Tetreault LA, Wilson JR, Aarabi B, Anderson P, Arnold PM, Brodke DS, Burns AS, Chiba K, Dettori JR, Furlan JC, Hawryluk G, Holly LT, Howley S, Jeji T, Kalsi-Ryan S, Kotter M, Kurpad S, Marino RJ, Martin AR, Massicotte E, Merli G, Middleton JW, Nakashima H, Nagoshi N, Palmieri K, Singh A, Skelly AC, Tsai EC, Vaccaro A, Yee A, Harrop JS. A clinical practice guideline for the management of patients with acute spinal cord injury and central cord syndrome: recommendations on the timing (≤24 hours versus >24 hours) of decompressive surgery. Global Spine J. 2017;7(3 Suppl):195S–202S. doi: 10.1177/2192568217706367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hess AS, Ramamoorthy J, Hess JR. Perioperative platelet transfusions. Anesthesiology. 2021;134(3):471–479. doi: 10.1097/ALN.0000000000003670. [DOI] [PubMed] [Google Scholar]
- 37.Frontera JA, Lewin JJ, 3rd, Rabinstein AA, Aisiku IP, Alexandrov AW, Cook AM, del Zoppo GJ, Kumar MA, Peerschke EI, Stiefel MF, Teitelbaum JS, Wartenberg KE, Zerfoss CL. Guideline for reversal of antithrombotics in intracranial hemorrhage: a statement for healthcare professionals from the neurocritical care society and society of critical care medicine. Neurocrit Care. 2016;24(1):6–46. doi: 10.1007/s12028-015-0222-x. [DOI] [PubMed] [Google Scholar]
- 38.Kietaibl S, Ahmed A, Afshari A, Albaladejo P, Aldecoa C, Barauskas G, De Robertis E, Faraoni D, Filipescu DC, Fries D, Godier A, Haas T, Jacob M, Lancé MD, Llau JV, Meier J, Molnar Z, Mora L, Rahe-Meyer N, Samama CM, Scarlatescu E, Schlimp C, Wikkelsø AJ, Zacharowski K. Management of severe peri-operative bleeding: guidelines from the European Society of Anaesthesiology and Intensive Care: Second update 2022. Eur J Anaesthesiol. 2023;40(4):226–304. doi: 10.1097/EJA.0000000000001803. [DOI] [PubMed] [Google Scholar]
- 39.Iaccarino C, Carretta A, Demetriades AK, Di Minno G, Giussani C, Marcucci R, Marklund N, Mastrojanni G, Pompucci A, Stefini R, Zona G, Cividini A, Petrella G, Coluccio V, Marietta M. Management of antithrombotic drugs in patients with isolated traumatic brain injury: an intersociety consensus document. Neurocrit Care. 2023 doi: 10.1007/s12028-023-01715-3. [DOI] [PubMed] [Google Scholar]
- 40.Lammers DT, Holcomb JB. Damage control resuscitation in adult trauma patients: what you need to know. J Trauma Acute Care Surg. 2023;95(4):464–471. doi: 10.1097/TA.0000000000004103. [DOI] [PubMed] [Google Scholar]
- 41.Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, et al. PROPPR Study Group. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA, 2015;313(5):471–482 [DOI] [PMC free article] [PubMed]
- 42.Shang Z, Wanyan P, Zhang B, Wang M, Wang X. Incidence and risk factors of deep vein thrombosis in patients with spinal cord injury: a systematic review with meta-analysis. Front Cardiovasc Med. 2023;12(10):1153432. doi: 10.3389/fcvm.2023.1153432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yorkgitis BK, Berndtson AE, Cross A, Kennedy R, Kochuba MP, Tignanelli C, Tominaga GT, Jacobs DG, Marx WH, Ashley DW, Ley EJ, Napolitano L, Costantini TW. American Association for the Surgery of Trauma/American College of Surgeons-Committee on Trauma Clinical Protocol for inpatient venous thromboembolism prophylaxis after trauma. J Trauma Acute Care Surg. 2022;92(3):597–604. doi: 10.1097/TA.0000000000003475. [DOI] [PubMed] [Google Scholar]
- 44.Hurlbert RJ, Hadley MN, Walters BC, Aarabi B, Dhall SS, Gelb DE, Rozzelle CJ, Ryken TC, Theodore N. Pharmacological therapy for acute spinal cord injury. Neurosurgery. 2013;72(Suppl 2):93–105. doi: 10.1227/NEU.0b013e31827765c6. [DOI] [PubMed] [Google Scholar]
- 45.Fehlings MG, Wilson JR, Tetreault LA, Aarabi B, Anderson P, Arnold PM, Brodke DS, Burns AS, Chiba K, Dettori JR, Furlan JC, Hawryluk G, Holly LT, Howley S, Jeji T, Kalsi-Ryan S, Kotter M, Kurpad S, Kwon BK, Marino RJ, Martin AR, Massicotte E, Merli G, Middleton JW, Nakashima H, Nagoshi N, Palmieri K, Skelly AC, Singh A, Tsai EC, Vaccaro A, Yee A, Harrop JS. A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on the use of methylprednisolone sodium succinate. Global Spine J. 2017;7(3 Suppl):203S–211S. doi: 10.1177/2192568217703085. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.