Cardiovascular conditions are significant contributors to morbidity and mortality among pregnant and postpartum women.1
We used data from the MarketScan Commercial Claims and Encounters database to identify women 12 to 55 years of age who delivered from 2017 to 2019. Delivery hospitalizations and cardiovascular diagnoses and procedures (ie, conditions) were identified using International Classification of Diseases-10th Revision-Clinical Modification codes. Cardiovascular conditions included acute heart failure or pulmonary edema; acute myocardial infarction; arrhythmia; conduction disorders; cardiac arrest, ventricular fibrillation, or ventricular flutter; cardiomyopathy; congenital heart and great artery defects; conversion of cardiac rhythm; endocarditis, myocarditis, or pericarditis; hypertensive heart disease; ischemic heart disease; nonrheumatic valve disorders; pulmonary heart disease; rheumatic heart disease; and other heart diseases and complications. We calculated the prevalence of hospitalizations with any cardiovascular condition in the year postpartum. Among these patients, we calculated the prevalence of cardiovascular conditions at delivery hospitalization and the frequency of postpartum hospitalizations. For postpartum hospitalizations with cardiovascular conditions, we calculated timing relative to delivery hospitalization and the prevalence (95% CI) of specific cardiovascular conditions by timing since delivery hospitalization (early postpartum [1–42 days] vs late postpartum [43–365 days]), accounting for clustering at the patient level. The data were collected and statistically deidentified. The data are also compliant with the conditions set forth in sections 164.514(a) and 164.51(b)(1)(ii) of the Health Insurance Portability and Accountability Act of 1996 Privacy Rule; therefore, approval from an Institutional Review Board was not sought.
Among 374,635 commercially insured U.S. women with a delivery and at least 1 year of follow-up, 1,127 (0.3%) had any postpartum hospitalizations with cardiovascular conditions. Of these, 89 (7.9%) had cardiovascular conditions documented during delivery hospitalization. Among women with any postpartum hospitalization with cardiovascular conditions, 1,057 (93.8%) had 1 hospitalization, 58 (5.1%) had 2 hospitalizations, and 12 (1.1%) had ≥3 hospitalizations. Among postpartum hospitalizations with cardiovascular conditions (n = 1,216), 40.6% (95% CI: 37.6%–43.6%; n = 494) occurred during late postpartum. The most prevalent cardiovascular conditions were acute heart failure or pulmonary edema (46.0%; 95% CI: 42.3%–49.7%; n = 332) during early postpartum and arrhythmia (37.9%; 95% CI: 33.3%–42.4%; n = 187) during late postpartum (Figure 1).
FIGURE 1. Documented Cardiovascular Diagnoses or Procedure Groups in Hospitalizations With Cardiovascular Conditions in the Postpartum Year.
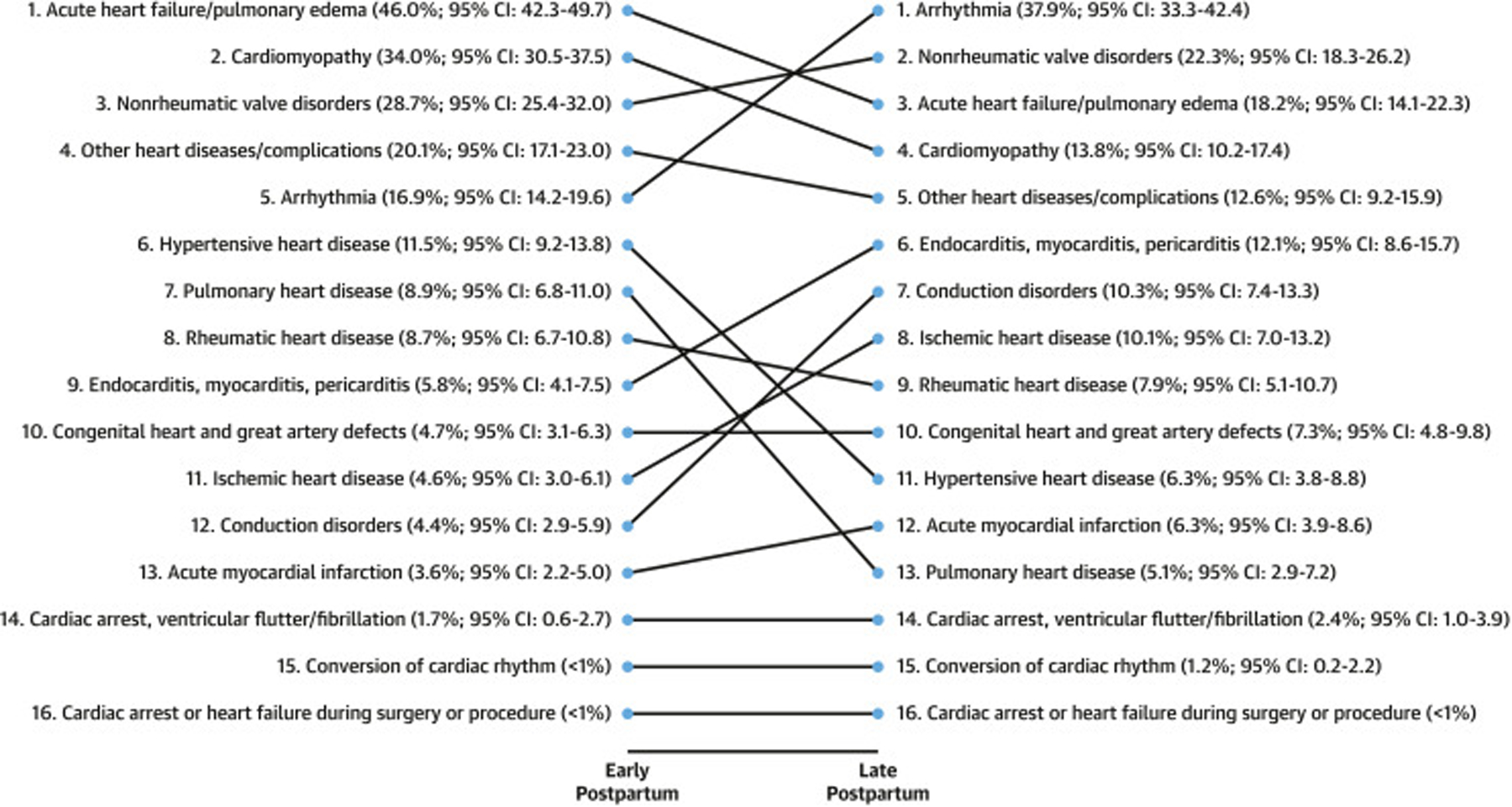
Relative rank and prevalence (%) (95% CI) of documented cardiovascular diagnoses or procedure groups in hospitalizations with cardiovascular conditions in the postpartum year (n = 1,216 postpartum hospitalizations among n = 1,127 women) in early (1–42 days; n = 722) and late (43–365 days; n = 494) postpartum. Data are from the MarketScan Commercial Claims and Encounters database. Arrhythmia includes paroxysmal tachycardia, atrial fibrillation, atrial flutter, and other cardiac arrythmias. Other heart diseases and complications include acquired cardiac septal defect, rupture of chordae tendineae (not elsewhere classified), rupture of papillary muscle (not elsewhere classified), intracardiac thrombosis (not elsewhere classified), myocardial degeneration, cardiomegaly, other ill-defined heart diseases, unspecified heart disease, other heart disorders not classified elsewhere, and nonischemic myocardial injury (nontraumatic).
Postpartum hospitalization with cardiovascular conditions is rare but reflects the potential threat to women’s lives in the year postpartum. Our findings underscore the importance of routine postpartum care for all, not only those with known higher risk for postpartum cardiovascular complications.2 A comprehensive postpartum visit within 12 weeks of delivery can identify and manage risk factors not present or documented at delivery (eg, high blood pressure), as well as urgent symptoms (eg, chest pain) that require evaluation and referral.2
Recognizing signs and symptoms of cardiovascular problems during the perinatal period is challenging, as they may overlap with symptoms of normal pregnancy (eg, shortness of breath). Clinical tools, such as the California Maternal Quality Care Collaborative’s algorithm for symptomatic or high-risk pregnant and postpartum women, which guides stratification and initial work-up, may enhance recognition of cardiovascular complications and improve management.3
In our study, the most prevalent conditions during the early postpartum period were acute heart failure or pulmonary edema and cardiomyopathy. Cardiovascular risk in the early postpartum period is compounded by obstetrical complications such as infection and hemorrhage.1 The most prevalent conditions during the late postpartum period were arrhythmia and nonrheumatic valve disorders. Understanding common diagnoses by postpartum period can inform educational interventions for clinicians and patients.
For women with diagnosed cardiovascular disease or with high cardiovascular risk, it is critical to create care plans for the transitions from intrapartum to postpartum care and from postpartum to well-woman care. The American College of Obstetricians and Gynecologists recommends that women with known cardiovascular disease have an early postpartum visit within 7 to 14 days of delivery to assess symptoms and functional status, followed by a comprehensive visit at 3 months postpartum with a multidisciplinary pregnancy heart team.1,4
Educating clinicians, including those who work in nonobstetrical settings, about the timeline for postpartum risk may improve recognition and management of maternal cardiovascular complications. Furthermore, it is important to educate postpartum individuals that pregnancy complications may arise up to a year after delivery and to make them aware of urgent maternal warning signs to reduce preventable pregnancy-related morbidity and mortality.5
What is the clinical question being addressed?
What is the prevalence of cardiovascular hospitalization in the first year postpartum?
What is the main finding?
Among commercially insured women delivering from 2017 to 2019 in the United States, 0.3% were hospitalized with cardiovascular conditions during the year postpartum, and of these, 41% occurred >42 days postpartum.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
REFERENCES
- 1.American College of Obstetricians and Gynecologists’ Presidential Task Force on Pregnancy and Heart Disease and Committee on Practice Bulletins–Obstetrics. ACOG practice bulletin no. 212: pregnancy and heart disease. Obstet Gynecol. 2019;133:e320–e356. [DOI] [PubMed] [Google Scholar]
- 2.American College of Obstetricians and Gynecologists. ACOG committee opinion no. 736: optimizing postpartum care. Obstet Gynecol. 2018;131:e140–e150. [DOI] [PubMed] [Google Scholar]
- 3.California Maternal Quality Care Collaborative. Improving health care response to cardiovascular disease in pregnancy and postpartum. Accessed November 14, 2023. https://www.cmqcc.org/resources-toolkits/toolkits/improving-health-care-response-cardiovascular-disease-pregnancy-and
- 4.Easter SR, Valente AM, Economy KE. Creating a multidisciplinary pregnancy heart team. Curr Treat Options Cardiovasc Med. 2020;22:3. [DOI] [PubMed] [Google Scholar]
- 5.Division of Reproductive Health. National Center for Chronic Disease Prevention and Health Promotion. Hear her. Accessed November 14, 2023. https://www.cdc.gov/hearher/index.html


