Abstract
Background:
“CoviSainik Program” was implemented in collaboration with the Ambuja Cement Foundation and Community Medicine Department in rural districts of eight states of India from May to December 2021 to create a cadre of volunteers. The aim of the present paper is to describe the program and evaluate it so that the findings can be the guiding tool for policymakers to replicate a similar program.
Material and Method:
A cross-sectional, mixed-method – concurrent study design was adopted to evaluate the program for its short-term outcomes such as gain in the basic knowledge of COVID-19 amongst master trainers and their feedback and program output viz – the proportion of volunteers trained and their profile by census sampling. Motivational factors, experiences of volunteers, and outcomes of COVID-19 work in their villages were explored by purposive with maximum diversity sampling with 62 online in-depth interviews and 8 online focus group discussions (FGDs).
Results:
There was a statistically significant difference in the pre-test (12.8 ± 5.6) and post-test (25.9 ± 9.3) scores of the Master Training Program evaluation test. Out of 6534 trained volunteers, 5901 worked as volunteers, and amongst those, 47.1%, 35.1%, and 17.8% worked for ≤3 months, 3 to 6 months, and ≥6 months, respectively, in their villages. The major themes generated for motivational factors to join the program were altruism, savior nature, generating awareness, and concern for others. The major outcomes generated by trained volunteers COVID-19 vaccination were in raising awareness on COVID-19 appropriate behavior and early identification of COVID-19 cases in their villages.
Conclusion:
The “CoviSainik Program” was successful in creating cadres of trained volunteers.
Keywords: Human resources, public-private partnership, rural community, volunteers
INTRODUCTION
Various strategies had been implemented in India to address manpower shortages during the COVID-19 pandemic such as the utilization of intern doctors and private sector staff, postponement of final-year postgraduate examinations, etc., However, most of these strategies were suitable to tackle COVID-19 cases in urban areas. Given that around 65% of India’s population lives in rural regions, sufficient efforts were needed to prevent health disasters in rural India, as the country was experiencing a rise in cases in rural areas in the second wave.[1]
The central government in the month of May 2021 released the Standard Operating Practices on COVID-19 management in peri-urban, rural, and tribal areas. A few key strategies stated were training ASHA, utilizing women’s self-help groups, and setting up a 3-tier structure for managing COVID-19 cases.[2] However, there are challenges that rural India faced. It has less access to healthcare facilities, shortages in qualified and trained manpower, poor testing facilities and disease surveillance activities, food insecurity, economic crisis, jobless young youth due to lockdown, villagers falling prey to quacks, etc.[3]
The existing manpower such as ASHA workers, Anganwadi workers, etc., was involved in the COVID-19 duty in early detection of cases, COVID-19 vaccination program, etc., However, additional COVID-19 duties were jeopardizing their work. Thus, there was a dire need for community mobilization to fight COVID-19 and to assist these public healthcare workers in controlling COVID-19 in their villages.
To address this crisis, the “CoviSainik Program” was implemented in various rural districts of eight states of India to create a cadre of volunteers who will be trained in basic primary COVID-19 management in crisis time as a support system to the health system, hospitals, and their own villages if required to manage COVID-19 isolation centers, etc.
For such a program to be implemented on a massive scale, there was also a need for collaboration as this program had two main components – training and community-level engagement with the public health department. Hence, to find a sustainable solution to this, the training of master trainers was undertaken by the resource person of the Community Medicine (CM) Department of Medical College and field-level training and engagement of volunteers in the public health system were undertaken by the Ambuja Cement Foundation (ACF) personnel.
The aim of the present paper is to describe this program and evaluate its effectiveness in terms of
Short-term outcomes viz. – Gain in the basic knowledge of COVID-19 among master trainers after the training program and their feedback.
Output viz. – Proportion of volunteers in each selected state, study volunteers’ profile, and assess the population covered.
Explore the motivational factors and experiences of volunteers and the outcomes of their work that contributed to the control of COVID-19 in their respective villages.
SUBJECTS AND METHODS
After the approval from the Joint Ethics Committee NSF – SBF (JEC/NSF-SBF/2021/07 dated 15-2-22), a cross-sectional, mixed-method – concurrent study design was adopted to evaluate the program.
Brief about CoviSainik Program
Activities undertaken were -
Development of the course content [Table 1] for the training of the master trainers and volunteers was done in the month of May–June 2021.
The training program schedule and certificate design were prepared with the consensus of ACF and CM departments.
Master trainers were identified by ACF. The inclusion criteria were – ability to deliver training and interest in training volunteers. Most of them were working as general duty assistants, project coordinator, or facilitators with a qualification in Bachelor or Masters in Social Work.
One of the authors from the CM department published the book titled “Basics of COVID-19” which was freely distributed to all master trainers as a resource book.
Volunteers were identified by ACF. The inclusion criteria were – age ≥18 years, self-interested, no desire to get any monetary benefit, and should know basic writing and reading skills.
Three-day, half-day (4 hours) online training programs for master trainers were conducted in three batches in July–August 2021 by a resource person from Community Medicine. Pre- and post-tests were done on the first and last of the training program, respectively. Those who attended all the sessions and scored at least 50% were certified as master trainers. Feedback was taken on the last day.
As the first batch of master trainers got trained, training of volunteers was initiated from July 2021 and continued till December 2021. Depending on the COVID-19 situation, training was conducted online or offline for a period of 3 days (full day) to 6 days (half day).
-
Trained volunteers then work for the control of COVID-19 in their village. Major work done by them was
- Local Health Team Assistance: Visited health sub-centers daily, discussed the duties with ANMs and ASHA workers, and volunteered in assigned villages
- Regular Follow-ups: Door-to-door visits capturing temperature and oxygen readings and creating awareness
- Community Meetings: Participated in Gram Sabha, farmers’ meetings, Self-help Group meetings; sensitizing about various aspects of COVID-19 and its management
- Vaccination Drives: Coordinated with Gram Panchayat to organize vaccination drives at village levels and also mobilized people during vaccination
- Overall support: Extended support to ANMs, ASHA workers, and Sakhis (Health volunteers of ACF) as and when required.
Table 1.
Course content for the training of master trainers and volunteers under “CoviSainik Program” (Year 2021)
| Course points | Theory pointers | Practical pointers |
|---|---|---|
| Basics of COVID-19 | Introduction of COVID-19, etiology, sign and symptoms, COVID-19 appropriate behaviors | Hand wash, Use of mask, How to make a mask from cotton cloth material Sign and symptoms of COVID-19, High-risk identification |
| Diagnosis of COVID-19 | Various lab tests available in COVID-19 | Use of PPE kit, identification of test kit |
| Recording of vitals | Vital signs and its method of measurement | Blood pressure, Temperature, Respiratory rate, Pulse recording, Thermal scanning, Pulse oximeter recording |
| COVID-19 vaccination | Types of vaccines available, registration process in COVIN-App, cold chain equipment | Reading vaccine vial, handling cold boxes and vaccine carriers, COWIN-platform registration and procedure at vaccination site |
| COVID-19 Biomedical waste (BMW) | Types of BMW and its disposal | Different color-coded bags, needle cutter and burner, and disposal process |
| COVID-19 isolation center | Concept of institutional isolation, the difference between quarantine and isolation, precaution during home and hospital isolation, and managing village-level isolation center | Identification of danger sign for referrals, home isolation guidelines |
| Oxygen therapy | What is oxygen therapy Methods of oxygen therapy Handling of oxygen cylinder, oxygen concentrators | Identify different capacity cylinder, functioning of oxygen concentrators cleaning of tubes, humidifier bottle with water level |
| Communication skill | Types of communication, and its importance | |
| Mucormycosis | Etiology, risk groups, sign and symptoms, and its prevention |
To evaluate the program, for the quantitative component, a census sampling technique was used to assess the gain in the basic knowledge of COVID-19 among master trainers. For the qualitative component, purposive sampling was adopted to explore the motivational factors, experiences of volunteers, and outcomes of the program it had in volunteers’ villages. In-depth interviews (IDI) of 62 volunteers were done telephonically. We selected at least one volunteer from each district who worked as a volunteer for at least 1 month. Data collection continued till at least one volunteer from each district was interviewed. To get maximum diversity sampling, we purposively selected volunteers of different age groups and sex. IDI lasted for 20 to 30 minutes. For seven volunteers, the interviews were done in two parts due to interview fatigue. We also conducted online FGDs with volunteers from each state. For the selection of volunteers for FGD, we purposively selected volunteers from different districts per state. Eight online FGDs were conducted with six to eight volunteers per FGD. IDIs and FGDs were conducted by one of the authors who is specialized in Community Medicine and is trained in qualitative research. One of the authors from ACF was always part of online FGDs to initiate the discussion. FGDs lasted for 60 to 70 minutes. Prior to IDIs and FDGs, district coordinators were given the list of volunteers selected for IDIs and FGDs. They briefed those selected volunteers about the aim of IDIs and FGDs and then scheduled IDIs according to the volunteers’ convenience time. None of the selected volunteers refused to IDIs or FGDs. Telephonic calls were made by an interviewer and verbal consent was taken. All IDIs were audio recorded by the interviewer. For FGDs, the Zoom link was shared by a designated ACF Program manager with district coordinators who ensured that all the selected volunteers were present for FGDs. All IDIs and FGDs were conducted using an interview guide in the Hindi language except in Maharashtra which was conducted in the Marathi language. In some states, the district coordinator also played the role of Hindi translator in IDIs and FGDs when some volunteers were speaking in their local dialect which was difficult to comprehend.
Quantitative data were analyzed in Microsoft Excel version 2021. Verbatims of IDIs and FGDs were transcribed by independent transcribers and back-translated into English. All quotes were encoded using the qualitative software program Atlasti. software version 9 trial package. An inductive thematic analysis approach was utilized to analyze the data. During the first stage, we carefully identified the systematic recurrence of codes throughout the data series and grouped them together by means of thematic analysis and generating open codes. Subsequently, axial coding was followed, and more similar-looking open codes were grouped under a subtheme. Following the constant comparison analysis among the various subthemes, we ultimately generated the major themes.
RESULTS
A total of 122 participants (mean age 34.9 ± 8.3 years) attended the Master’s training, of which 87 (mean age 36.2 ± 9.0 years) were certified as master trainers. Table 2 shows the description of master trainers who participated and those who got certified. There was a statistically significant difference in the pre-test (12.8 ± 5.6) and post-test (25.9 ± 9.3) scores of the Master Training Program evaluation test (P value < 0.05). Overall, there was positive feedback from master trainers on the training program. All master trainers gained the confidence to train volunteers.
Table 2.
Description of master trainers who participated in the online program and those who got certified under CoviSainik Program (Year 2021)
| Participants who attended the online Masters’ Training Program (n=122) | Participants who got certified as master trainers (n=87) | |||
|---|---|---|---|---|
|
|
|
|||
| Frequency | % | Frequency | % | |
| Age | ||||
| 18–24 | 8 | 6.6 | 8 | 9.2 |
| 25–30 | 37 | 30.3 | 22 | 25.3 |
| 31–36 | 29 | 23.8 | 13 | 14.9 |
| 37–42 | 23 | 18.9 | 20 | 23.0 |
| 43–48 | 18 | 14.8 | 17 | 19.5 |
| 48+ | 7 | 5.7 | 7 | 8.0 |
| Sex | ||||
| Female | 48 | 39.3 | 41 | 47.1 |
| Male | 74 | 60.7 | 46 | 52.9 |
| State | ||||
| Chhattisgarh | 10 | 8.2 | 7 | 8.0 |
| Gujarat | 12 | 9.8 | 9 | 10.3 |
| Himachal Pradesh | 15 | 12.3 | 15 | 17.2 |
| Maharashtra | 29 | 23.8 | 15 | 17.2 |
| Punjab | 12 | 9.8 | 11 | 12.6 |
| Rajasthan | 26 | 21.3 | 14 | 16.1 |
| Uttarakhand/Uttar Pradesh | 12 | 9.8 | 12 | 13.8 |
| West Bengal | 6 | 4.9 | 4 | 4.6 |
| Education | ||||
| Bachelor’s degree | 37 | 30.3 | 22 | 25.3 |
| Diploma degree | 26 | 21.3 | 18 | 20.7 |
| Junior college completed | 3 | 2.5 | 0 | 0.0 |
| Master’s degree | 56 | 45.9 | 47 | 54.0 |
| Medical background | ||||
| Yes | 36 | 29.5 | 29 | 33.3 |
| No | 86 | 70.5 | 58 | 66.7 |
| Years of experience in ACF | ||||
| Below 1 year | 1 | 0.8 | 0 | 0.0 |
| 1 to 5 years | 41 | 33.6 | 27 | 31.0 |
| 5 to 10 years | 32 | 26.2 | 18 | 20.7 |
| >10 years | 48 | 39.3 | 42 | 48.3 |
One master trainer trained 75 volunteers (1:75), and a total of 6534 volunteers were trained and out of those, 5,901 worked as volunteers. The mean age of trained volunteers was 31 ± 9.5 years. Maximum of volunteers were 10th or 12th passed. Most trained volunteers were males (3,961; 60.6%) and in the age group of 18 to 24 years (1983; 31.3%) [Table 3].
Table 3.
Description of participants trained as volunteers under the CoviSainik Program (2021) and those who worked as a volunteer
| Total trained volunteers (N-6534) | Total – worked as volunteer (N-5901) | |||
|---|---|---|---|---|
|
|
|
|||
| Frequency | % | Frequency | % | |
| Age (in years) | ||||
| 18 | 17 | 0.3 | 12 | 0.2 |
| 19–24 | 1973 | 31.3 | 1695 | 29.9 |
| 25–30 | 1333 | 21.1 | 1204 | 21.2 |
| 31–36 | 1178 | 18.7 | 1093 | 19.3 |
| 37–42 | 924 | 14.6 | 853 | 15.0 |
| 43–48 | 588 | 9.3 | 542 | 9.6 |
| 48+ | 295 | 4.7 | 276 | 4.9 |
| Total | 6308 | 100.0 | 5675 | 100.0 |
| Sex | ||||
| Female | 2573 | 39.4 | 2124 | 36.0 |
| Male | 3961 | 60.6 | 3777 | 64.0 |
| Total | 6534 | 100.0 | 5901 | 100.0 |
| State | ||||
| Chhattisgarh | 288 | 4.4 | 288 | 4.9 |
| Gujarat | 1029 | 15.7 | 912 | 15.5 |
| Himachal Pradesh | 257 | 3.9 | 256 | 4.3 |
| Maharashtra | 841 | 12.9 | 841 | 14.3 |
| Punjab | 2348 | 35.9 | 2341 | 39.7 |
| Rajasthan | 626 | 9.6 | 466 | 7.9 |
| Uttarakhand/Uttar Pradesh | 790 | 12.1 | 442 | 7.5 |
| West Bengal | 355 | 5.4 | 355 | 6.0 |
| Total | 6534 | 100.0 | 5901 | 100.0 |
| Education | ||||
| Below 10th | 131 | 2.0 | 117 | 2.0 |
| X | 2175 | 33.9 | 2009 | 34.4 |
| XI–XII | 2312 | 36.0 | 2069 | 35.4 |
| Diploma degree | 145 | 2.3 | 1274 | 21.8 |
| Bachelor’s degree | 1355 | 21.1 | 256 | 4.4 |
| Post Graduation | 279 | 4.4 | 104 | 1.8 |
| Other | 18 | 0.3 | 18 | 0.3 |
| Total | 6415 | 100.0 | 5847 | 100.0 |
*For variables other than sex variable, n varies due to missing data. Percentages calculated on available data
Out of 5,901 volunteers, 2,779 (47.1%), 2,071 (35.1%), and 1,051 (17.8%) worked for ≤3 months, 3 to 6 months, and ≥6 months, respectively. 2,555 volunteers (43.3%) worked with the Public Health System either with a Medical Officer, ANM, ASHA, or Gram Panchayat or at ACF field. The rest 3,346 (56.7%) worked individually in their villages to control COVID-19.
The number of districts and villages covered in other states is shown in Table 4. A total of 2343 villages in India were covered. Considering the average size of a village as 1,000, around 23,43,000 population benefited from this program. Each village had an average of two trained volunteers.
Table 4.
Coverage of the CoviSainik Program (2021) w.r.t. creation of volunteers and population covered
| State | Districts covered | Total districts | Percentage of districts covered | Villages covered | Average number of trained volunteers per village |
|---|---|---|---|---|---|
| Gujarat | 19 | 33 | 58 | 397 | 3 |
| Himachal Pradesh | 5 | 12 | 42 | 219 | 1 |
| Maharashtra | 2 | 36 | 6 | 344 | 2 |
| Punjab | 8 | 23 | 35 | 381 | 6 |
| Rajasthan | 27 | 33 | 82 | 465 | 1 |
| Uttarakhand/Uttar Pradesh | 26 | 75 | 35 | 336 | 2 |
| West Bengal | 6 | 23 | 26 | 66 | 5 |
| Chhattisgarh | 24 | 33 | 72 | 135 | 2 |
| Total | 126 | 766 | 16 | 2343 |
Motivational factors and experiences of the volunteers
Through IDIs and FDGs, the major themes generated to join the CoviSainik Program were altruism, savior nature, generating awareness, and concern for others.
Volunteers said, “It’s my habit to help others.” “It’s my duty to help others.” This showed their altruistic behavior. Others’ responses were, “I want to save my family.” “I want to save village from Corona.” This savior nature made them join the program. Some volunteers thought that the only way to control COVID-19 in their village was by generating awareness of the preventive measures, and each one should have correct information about COVID-19. They said, “Knowledge about Corona will only save us.” “I want to create awareness of Corona in my village.” As COVID-19 was spreading in their village, volunteers had concerns for their families or village, which motivated them to join the program.
There were varied experiences of volunteers when they started working in their village. Some of them received objections. Comments that they got from their parents, husbands, their friends, other family members, and/or villagers were – “Don’t do this work.” “Our family will get destroyed.” “You will only get Corona in our home.” “What if something happens to you?” “Do not touch Corona patients. Do not do this work. Why do you go out of your home?” However, they were determined to do COVID-19-related work in their village. Their response to an objection was either by persuading or ignoring it. One of the volunteers said, “I explained to my villagers, someone should come out of the house to help others.” Another said, “It didn’t bother me. I knew what I am doing.” It was observed that in spite of determination, volunteers were apprehensive but they continued to work. They had fear of getting COVID-19 (“I had feared since in nearby villages, people were getting CORONA.”). Some feared that their family or other villagers get COVID-19. Some were anxious (“I had feared what should I do if people in my village get CORONA.”) Some volunteers got support from their parents or husbands. One volunteer commented, “Mummy Pappa said – “Do whatever you feel like to do. We support your decision.” Another said, “My biggest support was of my husband. He took care of my children in my absence.” It was observed that volunteers were satisfied with their work since it was appreciated by others. They said, “Felt nice when villagers used to listen to us.”, “If someone is learning from us, then what can be bigger happiness than this?”, “You are doing great work. You are helping villagers.”
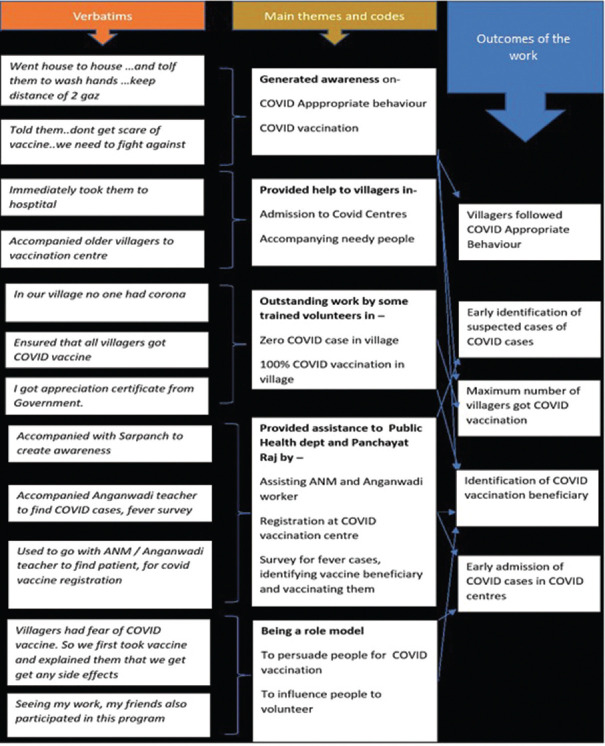
Major outcomes of trained volunteers’ work were in COVID-19 vaccination, raising awareness on COVID-19 appropriate behavior, and early identification of COVID-19 cases in their villages [Figure 1].
Figure 1.
Outcomes of the work done by CoviSainiks
DISCUSSION
The world of work has been profoundly affected by the COVID-19 pandemic. Countries have suffered from severe staff shortages and/or maldistribution of health personnel.[4] There is a universal challenge in staffing health services in remote rural areas.[5] The need to expand and sustain essential health system functions calls for a broader range of health cadres. However, the mere availability of health workers is not sufficient. They should be equitably distributed and accessible by the population. They should possess the required competency and should be motivated and empowered to deliver quality care that is appropriate and acceptable to society.[6]
In rural India, during the 2nd wave of COVID-19, there was a need for trained manpower that would be a helping hand to the existing crunching public health system. Thus, the strategic intervention was planned in the rural areas of selected states in India. CoviSainiks were basically community-based volunteers who could provide support to primary healthcare centers in the fight against COVID-19. There is growing interest in the use of volunteers to assist in the provision of essential PHC services across Low middle-income countries. The term volunteer is used too broadly in denoting unsalaried service. They are defined as people who contribute time, effort, or talent to a cause without monetary rewards.[7] We too used this definition in the selection of volunteers. Through IDIs and FGDs, we found out that the major reasons to participate and work for the control of COVID-19 in their village were altruism and/or savior personality, need to generate awareness, and concern for others.
In the review done by M Woldie et al.,[8] the most common role played by the volunteers was awareness raising by informing and educating about communicable diseases and maternal and child health problems. This is in congruence with our findings. Almost 50% of the volunteers were working individually to raise awareness of COVID-19 appropriate behavior, vaccination, the importance of quarantine, etc., Van Ginneken et al.[9] noted how the selection of volunteers is underpinned by the “cultural, political and social contexts of the programme area” with volunteers usually being “those that are most acceptable to the community”. Hall et al.[10] reviewed 11 studies and concluded that “lay health workers provided excellent health education and counseling and outreach activities, and their involvement was acceptable to most patients.” We too got similar observations. Most of the volunteers were the ones, whom the community was receptive to listening to them. They could trust them. In some villages, we observed that tribals got convinced of vaccinations when these volunteers approached them.
Volunteers are sometimes seen as lesser-trained health workers. But they may represent a different and sometimes preferred type of health worker. The close relationship between them and recipients is a program strength.[11] In our program, the criteria for volunteers were those who were adults and had reading and writing skills. However, almost 70% of the volunteers were 10th to 12th pass. Thus, their educational background was on par with grassroots level workers, viz., ASHA (Accredited Social Health Activist) and Anganwadi workers. Being educated was one of the strengths of our program. They could assist the ANM and Anganwadi workers in registration at COVID-19 vaccination centers, do a fever survey to identify suspected cases of COVID-19, use a pulse oximeter and thermal gun, and assist in reporting and keeping records of those vaccinated and not vaccinated. They worked in liaison with Gram Panchayat and public health department. Some of the volunteers also got appreciation certificates from the Public Health Department for their exemplary work in COVID-19 control in their villages. Volunteers do face challenges that community health workers do not. They may face disapproval from family members as their voluntary activity brings no income to the family, thereby adversely influencing retention.[10] In the CoviSainik Program, volunteers got resistance from family members, not because it did not bring income but because they had concerns and fear about COVID-19. They feared death due to COVID-19.
Volunteers have played an important role in the control of other infectious diseases.[12] According to National and Community Service (2009), volunteers play a very important part mostly during disaster times.[13] As per our review of the literature, ours is the only program in the creation of cadres of volunteers at such a massive scale in eight states during the COVID-19 pandemic. Especially in the 2nd wave, there was an acute emergency of trained manpower in rural areas. Through our novel program which is similar to the PPP model – involving Corporate Social Responsibility (CSR) division of ACF and the Community Medicine (CM) Department of Government Teaching Institute, we were successful in providing trained manpower at the grassroots level. This model can be experimented with for control of other communicable or noncommunicable, maternal, or child-related problems. Each CM department has faculty members who are experts in imparting quality training and moreover, they have field-level experience which is an added advantage. The CSR divisions can partner with CM departments of Medical Institutions for training, knowledge sharing, strategic planning, etc.
United Nations has recognized the role of volunteers and seeks to integrate it into the “Decade of Action” to achieve sustainable development goals by 2030. Most recently, the UN framework for the immediate socio-economic response to COVID-19 takes note that “volunteer groups often play an indispensable leadership role in the response, notably in reaching out to vulnerable people, and in getting to remote places.[14] They can amplify responses.” They have been stepping up to help during the pandemic and have been a beacon of selflessness and optimism. They have demonstrated an exceptional display of solidarity across the world.[15]
As a strategic response to the COVID-19 pandemic, MyGov India, in collaboration with the National Disaster Management Authority (NDMA) and the Ministry of Health and Family Welfare has also called upon individuals and organizations to volunteer or donate.[16]
During the COVID-19 pandemic, multiple strategies were undertaken in each state to control the disease. Due to feasibility issues, we could not compare it with other districts, to provide stronger evidence of program effectiveness.
CONCLUSION
The “CoviSainik Program” was successful in creating cadres of trained volunteers and assisting the public health department to control COVID-19 in their villages.
Financial support and sponsorship
The program was fully funded by the Ambuja Cement Foundation.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We express our gratitude to all master trainers and volunteers for participating in the program. We are thankful to the Program Manager and district coordinators for their assistance in coordinating with volunteers to schedule IDIs and FGDs.
REFERENCES
- 1.World Bank Data. [[Last accessed on 2023 Mar 05]]. Available from: https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS?locations=IN .
- 2.Government of India. Ministry of Health and Family Welfare. SOP on COVID-19 Containment and Management in Peri-urban, Rural and Tribal areas. [[Last accessed on 2023 Mar 05]]. Available from: https://www.mohfw.gov.in/pdf/SOPonCOVID19Containment&ManagementinPeriurbanRural&tribalareas.pdf .
- 3.Chintakula BS. Problems of rural system in India, need for addressing them in rural development planning. Int J Eng Res Technol. 2020;9:255–62. [Google Scholar]
- 4.Workforce in COVID. [[Last accessed on 2023 Mar 05]]. Available from: https://www.ilo.org/global/topics/coronavirus/lang--en/index.htm .
- 5.Lehmann U, Dieleman M, Martineau T. Staffing remote rural areas in middle- and low-income countries: A literature review of attraction and retention. BMC Health Serv Res. 2008;8:19. doi: 10.1186/1472-6963-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Assembly, 69. (2016). Global strategy on human resources for health: Workforce 2030. World Health Organization. [[Last accessed on 2023 Mar 05]]. Available from: https://apps.who.int/iris/handle/10665/252799 .
- 7.Cnaan RA, Handy F, Wadsworth M. Defining who is a volunteer: Conceptual and empirical considerations. Nonprofit Volunt Sect Q. 1996;25:264–383. [Google Scholar]
- 8.Woldie M, Feyissa GT, Admasu B, Hassen K, Mitchell K, Mayhew S, et al. Community health volunteers could help improve access to and use of essential health services by communities in LMICs: An umbrella review. Health Policy Plan. 2018;33:1128–43. doi: 10.1093/heapol/czy094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Ginneken N, Tharyan P, Lewin S, Rao G, Meera S, Pian J, et al. Non-specialist health worker interventions for the care of mental, neurological, and substance-abuse disorders in low- and middle-income countries. Cochrane Database Syst Rev. 2013;11:CD009149. doi: 10.1002/14651858.CD009149.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Hall BJ, Sou KL, Beanland R, Lacky M, Tso LS, Ma Q, et al. Barriers and facilitators to interventions improving retention in HIV care: A qualitative evidence meta-synthesis. AIDS Behav. 2017;21:1755–67. doi: 10.1007/s10461-016-1537-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glenton C, Colvin CJ, Carlsen B, Swartz A, Lewin S, Noyes J, et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health:qualitative evidence synthesis. Cochrane Database Syst Rev. 2013;2013:CD010414. doi: 10.1002/14651858.CD010414.pub2. doi:10.1002/14651858. CD010414.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barogui YT, Sopoh GE, Johnson RC, de Zeeuw J, Dossou AD, Houezo JG, et al. Contribution of the community health volunteers in the control of Buruli ulcer in Bénin. PLoS Negl Trop Dis. 2014;8:e3200. doi: 10.1371/journal.pntd.0003200. doi:10.1371/journal.pntd. 0003200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bureau of Labour Statistics. Volunteering in the United States, USA. [[Last accessed on 2023 Mar 05]]. Available from: https://www.bls.gov/news.release/archives/volun_01262010.pdf .
- 14.Building back better: Why volunteering matters for the post-COVID world. Press release. [[Last accessed on 2023 Mar 05]]. Available from: https://jordan.un.org/en/53636-building-back-better-why-volunteering-matters-post-covidworld .
- 15.COVID – 19 drives global surge in volunteering. [[Last accessed on 2023 Mar 05]]. Available from: https://www.un.org/en/coronavirus/covid-19-drives-global-surgevolunteering .
- 16.Volunteer or donate for fight against Corona. [[Last accessed on 2023 Mar 05]]. Available from: https://self4society.mygov.in/