Abstract
Background:
The Indian government launched national teleconsultation services (eSanjeevani OPD) to provide safe doctor-to-patient consultations. This study aimed to determine the awareness and willingness to seek services from eSanjeevani OPDs.
Material and Methods:
This is a cross-sectional descriptive study conducted in Nandigudi village, Karnataka. The total sample size was 273, and participants were recruited using a systematic sampling technique.
Results:
The prevalence of awareness about teleconsultations was 2.2% (n = 6, 95% CI: 0.8–4.7%). None of the participants utilized eSanjeevani services in the last year. Approximately 56.0% (n = 153, 95% CI: 49.9–62.0%) were willing to use eSanjeevani OPD. “Not being familiar” (n = 99, 82.5%) with eSanjeevani OPD was the major reason for unwillingness to use teleconsultation, and 73.8% (n = 113) preferred video calls as the mode of communication.
Conclusion:
The majority of the participants were not aware of and were unwilling to use eSanjeevani OPD. Therefore, healthcare professionals should focus more on creating awareness of teleconsultations.
Keywords: Digital health, COVID-19, primary care
INTRODUCTION
Telemedicine refers to the utilization of information and communication technology (ICT), such as interactive video conferencing tools, to remotely diagnose, treat, and monitor patients, as well as consult with fellow medical professionals, revolutionizing healthcare delivery by bridging geographical gaps and enhancing accessibility to expert medical advice.[1,2] Telemedicine is time- and money-efficient, especially in nations such as India with poor healthcare infrastructure and a shortage of medical experts.[3,4] The main purpose of telemedicine is to give standard or quality healthcare services in every place in India, including easing access to healthcare to both privileged and non-privileged populations; providing quick, inexpensive, and finer communication for medical care; and follow-up by specialists. It helps eliminate the geographical walls to healthcare, especially by reaching distant areas inadequately connected by any means of transport. The field of telemedicine is growing fleetly.[5]
In 2018, under the Ayushman Bharath scheme, the Government of India committed to modifying existing primary health centers and subcenters into 1,55,000 health and wellness centers (HWCs) in India, where eSanjeevani outpatient department (OPD) (stay-home OPD) service is available in all HWCs.[6] Ministry of Health and Family Welfare (MoHFW), India and the National Institution for Transforming India (NITI-Aayog) jointly developed the Telemedicine Practice Guidelines in March 2020[7] as telemedicine has been considered an ideal tool to face emergencies such as the COVID-19 pandemic.[7-9] The MoHFW’s national teleconsultation service stands as the government’s inaugural online outpatient service, aiming to provide healthcare services directly to patients’ homes through secure and well-organized video-based clinical consultations.[10] eSanjeevani OPD has been established by the Center for the Development of Advanced Computing (C-DAC) in Mohali.[2]
The eSanjeevani OPD aims to enhance the health status of the rural population. Therefore, understanding the awareness and utilization of eSanjeevani OPD by the rural population will help to understand the reach of these services. Hence, this study aimed to determine the awareness, utilization, and willingness to seek services from eSanjeevani OPDs among individuals residing in rural South India.
METHODS
Study design and setting
A cross-sectional analytical study was conducted among individuals aged 18 years and above at the catchment areas of a selected HWC Nandigudi, Harihara taluk, Davanagere district, and Karnataka, India between April 2021 and July 2022.
Sample size calculation
A study conducted by Meher SK et al. in New Delhi, India, determined that 20% of the patients were aware of telemedicine.[11] The study’s final sample size of 273 was determined with a 5% absolute precision and accounting for a 10% non-response rate, as calculated using OpenEpi version 3.01.
Sampling technique
The sampling technique is described in Figure 1. There are ten primary health centers in Harihara, and the HWC of Nandigudi was selected by simple random sampling. There are nine villages under the HCW of Nandigudi. Using simple random sampling, K N Halli and Vasana villages were selected for the study. Households for the samples were drawn using systematic random sampling with a sampling interval of four, and one participant from the selected household was interviewed.
Figure 1.
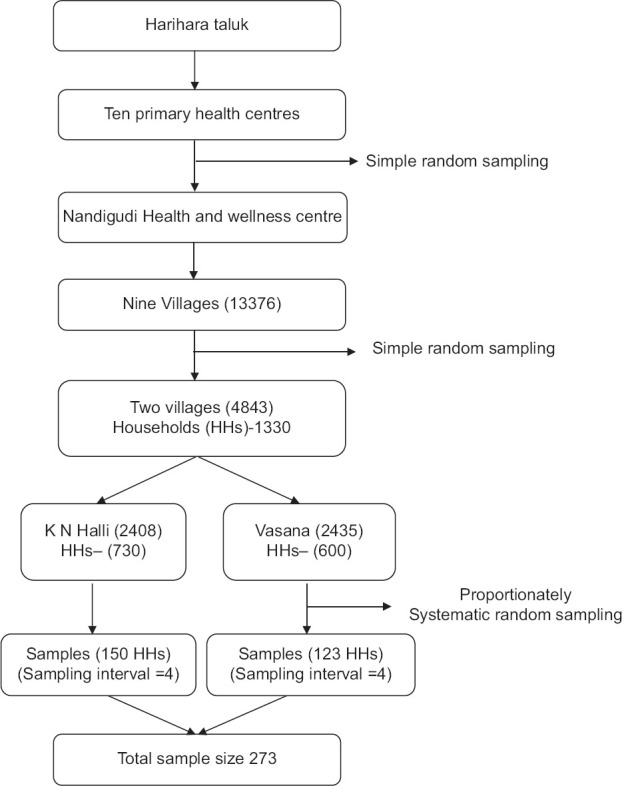
Selection of participants from households among individuals residing in rural areas of Harihara Taluk, Karnataka, India during April–May 2022 (N = 273)
Method of data collection
Three subject experts performed the content validity of the questionnaire. Based on the guidelines and suggestions from the experts, the final version of the questionnaire was prepared. The student investigator, along with the secretory/peon of the gram panchayath, visited the participants’ houses for the study. A validated semi-structured questionnaire was administered to the participants at their houses. Confidentiality and privacy were maintained throughout the interview.
Ethical considerations
The study protocol was reviewed and approved by the institute’s ethics committee, and appropriate permission from the local bodies (Grama Panchayath) was taken for the study.
Operational definitions
Teleconsultation: The services provided through eSanjeevani OPD were considered teleconsultation.
Awareness: Awareness is the state of being conscious of eSanjeevani OPD.
Willingness: If an individual is willing to try the eSanjeevani OPD service, they are fairly happy about trying it and can roll in if asked or required to try it.
Statistical analysis
Data collected through paper-based forms were entered into the EpiCollect 5 mobile application, and subsequent data analysis was conducted using STATA version 14. Categorical variables, including gender, education, occupation, monthly family income, family type, possession of laptop/smartphone and home internet access, type of ration card, presence of morbidity, family history of morbidity, and preferred healthcare service location, were summarized in terms of frequencies and percentages. The outcome variables such as awareness, willingness, and preferred digital healthcare tools were summarized as percentages with a 95% confidence interval (CI). This study examined the relationship between sociodemographic factors and reluctance to use eSanjeevani OPD through a Chi-squared test by calculating unadjusted prevalence ratios (UPRs). Variables with a P value of <0.2 were subjected to a log-binomial regression analysis, generating adjusted prevalence ratios (APRs) with a 95% confidence interval. Statistical significance was set at a P value of <0.05.
RESULTS
The response rate was 100%. The mean (SD) age of the participants was 38.7 (13.9) years. Among 273 participants, 36% (n = 96) belonged to the age group of 30–44 years, and more than half (52%, n = 142) were females. The majority (72%, n = 195) were married, and 38% (n = 104) were having a monthly family income of more than INR 10,000. Approximately 17% (n = 47) had any kind of morbidity, 34% (n = 94) had a family history of any morbidities, and 61% (n = 166) preferred a private hospital for healthcare needs. The majority (88%, n = 240) had a laptop/smartphone and internet facility at home.
Prevalence of awareness and willingness to use eSanjeevani OPD and preferred modes of communication are depicted in Table 1. Approximately 98% (n = 267, 95% CI: 95.3–99.2%) of the participants were not aware of eSanjeevani OPD. Among those who were aware, most of them reported healthcare workers as their source of information on eSanjeevani OPD. None of the participants utilized eSanjeevani services in the last year. Approximately 44% (n = 120, 95% CI: 37.9–50.1%) were unwilling to use eSanjeevani OPD; 83% (n = 99) of them reported “not familiar” as the reason. The majority (92%, n = 251) preferred social media as the platform to use eSanjeevani OPD; among them, 73% (n = 113) preferred video calls (95% CI: 66.0–80.0%).
Table 1.
Proportion of awareness, willingness, and preferred mode of communication to use eSanjeevani OPD among individuals residing in rural areas of Harihara Taluk, Karnataka, during April–May 2022 (n=273)
| Variables | n | % | 95% CI |
|---|---|---|---|
| Awareness | |||
| Yes | 6 | 2.2 | 0.8–4.7 |
| No | 267 | 97.8 | 95.3–99.2 |
| Willingness to use eSanjeevani OPD | |||
| Yes | 153 | 56.0 | 49.9–62.0 |
| No | 120 | 44.0 | 37.9–50.1 |
| Preferred mode of teleconsultation | |||
| Video call | 113 | 73.8 | 66.0–80.0 |
| Audio call | 35 | 22.8 | 16.5–30.3 |
| Message | 27 | 17.6 | 11.9–24.6 |
CI - confidence interval, OPD - Outpatient department
Factors associated with unwillingness to use eSanjeevani OPD are depicted in Table 2. After adjusting the covariates, compared to individuals whose family monthly income was more than INR 10,000, the individuals whose family monthly income was less than INR 5000 had a 22% less chance of being unwilling to use eSanjeevani OPD (95% CI: 0.67–0.92, P = 0.004). Individuals without formal education had a higher chance of being unwilling to use eSanjeevani OPD (APR = 2.89, 95% CI: 1.44–5.80, P = 0.003) as compared to individuals educated with graduation and above. Similarly, not having a laptop/smartphone at home (APR = 1.42, 95% CI: 1.25–1.62, P < 0.001) and no family history of morbidities (APR = 1.01, 95% CI: 1.01–1.02, P < 0.001) were significantly associated with unwilling to use eSanjeevani OPD.
Table 2.
Factors associated with unwillingness to use eSanjeevani OPD from HWC among individuals residing in rural areas of Harihara Taluk, Karnataka, during April–May 2022 (n=273)
| Variables | n | Unwilling n (%) | UPR (95% CI) | APR (95% CI) | P |
|---|---|---|---|---|---|
| Age in years | |||||
| ≥60 | 27 | 17 (63.0) | 2.64 (1.63–4.27) | 1.25 (0.81–1.92) | 0.309 |
| 45–59 | 66 | 36 (54.5) | 2.29 (1.47–3.56) | 1.23 (0.80–1.90) | 0.333 |
| 31–44 | 96 | 47 (49.0) | 2.05 (1.33–3.17) | 1.29 (0.84–1.95) | 0.244 |
| ≤30 | 84 | 20 (23.8) | Reference | Reference | - |
| Gender | |||||
| Female | 142 | 67 (47.2) | 1.17 (0.89–1.52) | - | - |
| Male | 131 | 53 (40.5) | Reference | - | - |
| Marital status | |||||
| Married | 195 | 98 (50.3) | 2.37 (1.45–3.85) | 0.99 (0.59–1.66) | 0.987 |
| Widowed | 12 | 8 (66.7) | 3.14 (1.70–5.80) | 1.12 (0.63–1.97) | 0.688 |
| Single | 66 | 14 (21.2) | Reference | Reference | - |
| Monthly Family income in Indian rupees | |||||
| <5000 | 68 | 42 (61.8) | 1.69 (1.23–2.31) | 0.78 (0.67–0.92) | 0.004 |
| 5000-9999 | 101 | 40 (39.6) | 1.08 (0.76–1.53) | 0.79 (0.68–0.94) | 0.007 |
| ≥10000 | 104 | 38 (36.5) | Reference | Reference | - |
| Educational qualification | |||||
| No formal education | 38 | 29 (76.3) | 4.42 (2.45–7.99) | 2.89 (1.44–5.80) | 0.003 |
| Class 1-7 | 53 | 31 (58.5) | 3.39 (1.84–6.22) | 2.27 (1.16–4.48) | 0.017 |
| Class 8-10 | 74 | 38 (51.4) | 2.98 (1.62–5.46) | 1.99 (1.00–3.94) | 0.047 |
| Class 11-12 | 50 | 12 (24.0) | 1.39 (0.65–2.94) | 1.20 (0.56–2.60) | 0.629 |
| Graduate & above | 58 | 10 (17.2) | Reference | Reference | - |
| Type of ration card | |||||
| BPL | 248 | 116 (46.8) | 1.63 (0.70–3.79) | - | - |
| Not a ration card user | 11 | 0 (0.0) | - | - | - |
| APL | 14 | 4 (28.6) | Reference | - | - |
| Occupation | |||||
| Monthly salaried | 33 | 7 (21.2) | 2.54 (0.58–11.19) | 1.42 (0.30–6.69) | 0.656 |
| Daily waged | 131 | 75 (57.3) | 6.87 (1.80–26.10) | 2.85 (0.65–12.38) | 0.163 |
| Unemployed | 15 | 4 (26.7) | 3.2 (0.67–15.38) | 1.88 (0.37–9.54) | 0.447 |
| Homemaker | 70 | 32 (45.7) | 5.4 (1.42–21.18) | 2.50 (0.57–10.53) | 0.222 |
| Student | 24 | 2 (8.3) | Reference | Reference | - |
| Type of family | |||||
| Nuclear | 192 | 86 (44.8) | 1.06 (0.79–1.44) | - | - |
| Joint | 81 | 34 (42.0) | Reference | - | - |
| Having a laptop/smartphone at home | |||||
| No | 33 | 25 (75.8) | 1.91 (1.49–2.45) | 1.42 (1.25–1.62) | <0.001 |
| Yes | 240 | 95 (39.6) | Reference | Reference | - |
| Using internet facility at home | |||||
| No | 33 | 25 (75.8) | 1.91 (1.49–2.45) | - | - |
| Yes | 240 | 95 (39.6) | Reference | - | - |
| Presence of morbidity | |||||
| Yes | 47 | 24 (51.1) | 1.20 (0.87–1.65) | - | - |
| No | 226 | 96 (42.5) | Reference | - | - |
| Family history of morbidities | |||||
| No | 179 | 85 (47.5) | 1.27 (0.94–1.72) | 1.00 (1.00–1.00) | <0.001 |
| Yes | 94 | 35 (37.2) | Reference | Reference | - |
| Preferred place for healthcare services | |||||
| Government hospital | 107 | 51 (47.7) | 1.14 (0.87–1.49) | - | - |
| Private hospital | 166 | 69 (41.6) | Reference | - | - |
| Awareness of eSanjeevani OPD | |||||
| No | 267 | 119 (44.6) | - | - | - |
| Yes | 6 | 1 (16.7) | - | - | - |
UPR=unadjusted prevalence ratios, APR=adjusted prevalence ratios, APL=above poverty line, BPL=below poverty line, OPD=Outpatient department
DISCUSSION
The present study was conducted on 273 community participants aged 18 years and above residing in rural areas of Harihara Taluk, Karnataka. We found that 97.8% of the participants were unaware of eSanjeevani OPD. Similarly, a study conducted in Uttarakhand found that 45%–50% of the respondents reported a lack of awareness about telemedicine apps among students.[12] A study conducted in New Delhi found that 100 out of 121 patients were not aware of telemedicine.[13] Similarly, a study conducted in Puducherry among health professional faculty also found that they had inadequate (24%) awareness of telemedicine.[14] In our study population, only 40% of the participants preferred government hospitals for healthcare services which play as the main source of information about eSanjeevani OPD. Studies reported that telehealth can be equivalent to or more clinically effective when compared to the usual care.[15] However, adopting telemedicine is challenging due to a number of health-policy consequences and obstacles.[16]
The present study also found that 44% of the participants were unwilling to use eSanjeevani OPD; most of them reported “not familiar” as the reason for unwillingness to use eSanjeevani OPD. A similar study found that 28% were unsure and 19% were unwilling to use telemedicine.[11] It was also reported that the preference was for direct consultation with a doctor. Another reason for unwillingness was the difficulty in operating software to use telemedicine. The present study reports that 92% of the participants preferred social media as the mode of teleconsultation, and almost all preferred WhatsApp as the first option. In a pilot study conducted on teleconsultation, 86.6% of the participants preferred WhatsApp.[17] The ease of using the WhatsApp mobile app might be the reason for this. In the present study, the majority (65%) of the participants reported video calls as their preferred mode of communication for the use of eSanjeevani OPD. It was already established that video conferencing offers more effective and reliable communication for healthcare needs; this could have influenced people’s perception of video calls as the preferred mode of communication.
The current study shows that family monthly income was associated with unwillingness to use eSanjeevani OPD; individuals having a lesser family income had higher chances of unwillingness. As telemedicine requires high-speed internet, the data recharge rates might have influenced the willingness of poor individuals. In our study, educational qualification was associated with unwillingness to use eSanjeevani OPD. Individuals who had no formal education had a higher chance of unwillingness to use eSanjeevani OPD. Lack of knowledge on smartphone use might be the reason for unwillingness to use eSanjeevani OPD. There was an association between individuals who did not have a laptop/smartphone at home and unwillingness to use eSanjeevani OPD. This is expected as the eSanjeevani OPD can be accessed only through a website. Family history of morbidities was also statistically significant with the unwillingness. Individuals having a family history of morbidities might prefer in-person consultation as they accompany their relatives/family members.
To the best of our knowledge, this is the first study that assessed the awareness, utilization, and willingness to use eSanjeevani OPD among the Indian population. This study adds evidence to people’s preference for digital healthcare tools. As only one researcher carried out all the interviews, interviewer bias is limited. However, there are a few limitations. As only the rural population was selected for the study, the generalizability of the findings is limited to the rural population. As the interviewer was from the same community, social desirability bias cannot be ruled out.
CONCLUSION
Most of the participants were not aware of eSanjeevani OPD, and 44% were unwilling to use eSanjeevani OPD. Among the individuals who were willing to use eSanjeevani OPD, 92% of them preferred social media as the mode of teleconsultation. Therefore, healthcare professionals should focus more on creating awareness of teleconsultations. Interventions to improve the awareness of telemedicine in the community are important.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wijesooriya NR, Mishra V, Brand PLP, Rubin BK. COVID-19 and telehealth, education, and research adaptations. Paediatr Respir Rev. 2020;35:38–42. doi: 10.1016/j.prrv.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhaskar S, Bradley S, Chattu VK, Adisesh A, Nurtazina A, Kyrykbayeva S, et al. Telemedicine across the globe-position paper from the COVID-19 pandemic health system resilience PROGRAM (REPROGRAM) international consortium (Part 1) Front Public Heal. 2020;8:556720. doi: 10.3389/fpubh.2020.556720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seguí FL, Walsh S, Solans O, Mas CA, Ferraro G, García-Altés A, et al. Teleconsultation between patients and health care professionals in the catalan primary care service: Message annotation analysis in a retrospective cross-sectional study. J Med Internet Res. 2020;22:e19149. doi: 10.2196/19149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Verhoeven F, Van Gemert-Pijnen L, Dijkstra K, Nijland N, Seydel E, Steehouder M. The contribution of teleconsultation and videoconferencing to diabetes care: A systematic literature review. J Med Internet Res. 2007;9:e37. doi: 10.2196/jmir.9.5.e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ateriya N, Saraf A, Meshram VP, Setia P. Telemedicine and virtual consultation: The Indian perspective. Natl Med J India. 2018;31:215–8. doi: 10.4103/0970-258X.258220. [DOI] [PubMed] [Google Scholar]
- 6.Guidelines for Telemedicine services in AYUSHMAN BHARAT. National Health Mission (NHM) Ministry of Health and Family Welfare (MoHFW) 2019:1–22. [Google Scholar]
- 7.Hincapié MA, Gallego JC, Gempeler A, Piñeros JA, Nasner D, Escobar MF. Implementation and usefulness of telemedicine during the COVID-19 pandemic: A scoping review. J Prim Care Community Health. 2020;11:2150132720980612. doi: 10.1177/2150132720980612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cui F, Ma Q, He X, Zhai Y, Zhao J, Chen B, et al. Implementation and application of telemedicine in china: Cross-sectional Study. JMIR mHealth uHealth. 2020;8:e18426. doi: 10.2196/18426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dorsey ER, Topol EJ. Telemedicine 2020 and the next decade. Lancet. 2020;395:859. doi: 10.1016/S0140-6736(20)30424-4. [DOI] [PubMed] [Google Scholar]
- 10.Sarwal R, Prasad U, Madangopal K, Kalal S, Kaur D, Kumar A, et al. Investment Opportunities in India's Healthcare Sector. NITI Aayog. 2021:1–44. [Google Scholar]
- 11.Meher SK, Tyagi RS, Chaudhry T. Awareness and attitudes to telemedicine among doctors and patients in India. J Telemed Telecare. 2009;15:139–41. doi: 10.1258/jtt.2009.003011. [DOI] [PubMed] [Google Scholar]
- 12.Malhotra RK, Ojha MK, Gupta S, Rupa M, Malhotra K. A study of assessment of knowledge, perception and attitude of using tele health services among college going students of Uttarakhand. J Med Pharm Allied Sci. 2020;10:113–6. [Google Scholar]
- 13.Mukhopadhyay S, Banerjee D. Relevance of the Indian telemedicine guidelines 2020 in psychogeriatric care: A critical appraisal. J Geriatr Ment Health. 2021;8:3–10. [Google Scholar]
- 14.Zayapragassarazan Z, Kumar S. Awareness, knowledge, attitude and skills of telemedicine among health professional faculty working in teaching hospitals. J Clin Diagn Res. 2016;10:JC01–4. doi: 10.7860/JCDR/2016/19080.7431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goharinejad S, Hajesmaeel-Gohari S, Jannati N, Goharinejad S, Bahaadinbeigy K. Review of systematic reviews in the field of telemedicine. Med J Islam Repub Iran. 2021;35:184. doi: 10.47176/mjiri.35.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kruse CS, Williams K, Bohls J, Shamsi W. Telemedicine and health policy: A systematic review. Heal Policy Technol. 2021;10:209–29. [Google Scholar]
- 17.Pandey N, Srivastava R, Kumar G, Katiyar V, Agrawal S. Teleconsultation at a tertiary care government medical university during COVID-19 Lockdown in India-A pilot study. Indian J Ophthalmol. 2020;68:1381–4. doi: 10.4103/ijo.IJO_1658_20. [DOI] [PMC free article] [PubMed] [Google Scholar]


