Abstract
More than three million nursing home residents are currently diagnosed with Alzheimer’s disease and related dementias (ADRD). This number is expected to increase as the population ages and ADRD prevalence increases. People with ADRD require specialized care from trained staff. This study raises two questions: Are residents with ADRD concentrated in nursing homes where they are the majority? If not, what are the implications for their quality of care and life? We answer the first question by determining the ADRD census for all nursing homes nationally during 2017–19. We compare characteristics of nursing homes with high and low ADRD census along several dimensions, including staffing, resident outcomes, and resident characteristics. Data include the Minimum Data Set and Medicare claims. We find that residents with ADRD are dispersed through all nursing homes, with fewer than 50 percent in nursing homes, where they account for 60–90 percent of the census. Furthermore, only facilities exceeding 90 percent residents with ADRD seem to offer better care. These findings raise concerns about the quality of care and life for the majority of residents with ADRD, suggesting that current National Institutes of Health dementia research initiatives and the Biden administration’s policies to improve nursing home care should be coordinated.
The prevalence of Alzheimer’s disease and related dementias (ADRD) is expected to continue to grow in the coming decades,1 and with it the need for specialized nursing home care. Assessment and management of complex medical conditions2 and behavioral symptoms3 require nursing home staff to have enhanced knowledge and training in recognizing and managing the needs of persons with ADRD.4 Relatedly, persons with severe cognitive impairment who have not been diagnosed with ADRD require similar specialized skills. Persons with ADRD are known to be easily agitated by changes in their environment, and high staff turnover5 is likely to be detrimental to their quality of life and care.6
Yet information about whether residents with ADRD or cognitive impairment are offered specialized care is limited. Fewer than 5 percent of nursing home beds are in dementia special care units),1 and the evidence about the quality of care they provide is inconclusive.7 Studies comparing residents with ADRD in dementia special care units with those in general care show that dementia special care units are associated with better outcomes by some metrics, and worse by others.8–10
We seek to answer two questions that are not fully addressed in the literature to date: Are residents with ADRD concentrated in nursing homes where the majority of residents have ADRD, or are they “sprinkled” among all nursing homes? If the latter, what are the implications for the quality of care they receive, their quality of life, and their health outcomes? It is unlikely that nursing homes would invest in staffing and training for specialized ADRD care unless residents with ADRD are a large majority of their census.
In this study we address the first question and discuss the potential implications for the second. Toward that end, we provide a snapshot of the nursing home sector in the US stratified by its pre-COVID-19 (2017–19) census of residents with ADRD or cognitive impairment. As a starting point for answering the second question, we present the distribution of residents with ADRD or cognitive impairment across US nursing homes, along with several important outcomes, staffing, and other nursing home characteristics.
Study Data And Methods
Sample
Our initial sample included all 15,718 nursing homes certified by the Centers for Medicare and Medicaid Services (CMS) during 2017–19. We excluded facilities that were hospital based, not operational for a full year, or had more than 70 percent of their residents younger than sixty-five. The final sample of 13,909 facilities served a total of 7.6 million unique residents during this period, 3.2 million (42 percent) of whom had ADRD or cognitive impairment.
Data And Variables
Data from several sources were merged using the facility Medicare provider number.
We used the Minimum Data Set data to calculate the average facility daily percentage of patients with ADRD or cognitive impairment, percentage residents receiving hospice, percentage of short- and long-stay residents, and daily average age, sex, race, and case-mix index based on the Resource Utilization Groups-IV score. The case-mix index reflects the average acuity, functional, and cognitive impairment levels of the residents in the nursing home and, therefore, the resources required to care for them.11 It determines Medicare payment and, in some states, Medicaid payment. The Minimum Data Set is a resident-level assessment mandated by CMS for all nursing homes. It reports age, sex, health status, and treatments, as well as other resident characteristics. CMS uses these data to determine the case-mix index and quality measures for quality reporting in Nursing Home Care Compare.
We based the ADRD determination on Alzheimer’s disease or dementia diagnoses. Cognitive impairment was based on the resident either having a score of 7 or less on the Brief Interview for Mental Status or having a reported memory problem that moderately or severely impaired the ability to make decisions about daily tasks. The Brief Interview for Mental Status is a nine-question tool used to monitor cognitive decline.12 It ranges from 0 to 15, with 0–7 indicating severe cognitive impairment. It is mandated for nursing home residents quarterly and is reported in the Minimum Data Set.
Following the CMS definition, we considered short-term residents to be those with a stay of less than or equal to 100 days.13
We obtained all other variables directly from the Minimum Data Set and combined them with the residents’ admission and discharge dates to calculate percentages or rates for the study period. We assumed that their daily values did not change until the next Minimum Data Set assessment. For short-stay residents the time between assessments could have been as short as eleven days; for long-stay residents it was typically ninety days.
The Minimum Data Set was also used to calculate the number of residents discharged to the hospital and the number of deaths in the facility, both per 1,000 resident-days. We used Minimum Data Set data merged with Medicare outpatient claims to calculate the number of emergency department (ED) visits not followed by a hospitalization per 1,000 resident-days.
CMS reports facility nurse staffing hours in Nursing Home Care Compare based on facilities’ submission of the Payroll-Based Journal, which provides daily payroll information by staffing types. We used the Payroll-Based Journal data to calculate average hours per resident-day and staffing instability for nonadministrative registered nurses (RNs), licensed practical or vocational nurses (LPNs), and certified nurse aides (CNAs). Staffing instability is a new staffing measure that has been shown to be associated with health outcomes.14,15 Average hours per resident-day was defined as the number of hours worked by each staff type divided by the number of residents in the nursing home averaged over the study period. Staffing instability by type was defined as the percentage of facility days in which staffing hours per resident-day were 20 percent below the facility average hours per resident-day for the period.
The five-star quality rankings are summary statistics calculated by the CMS based on individual quality measures and published in Nursing Home Care Compare. These measures range from 1 (quality much below average) to 5 (quality much above average). There are separate five-star rankings for staffing, survey, and quality measures. CMS differentially weights these separate five-star rankings to create an overall five-star ranking. We obtained the values from archived files in the CMS data catalog and averaged the rankings for each nursing home for the study period.
We obtained other nursing home characteristics, including whether the facility had a dementia special care unit, facility bed size, occupancy percent, ownership, and payer mix from the Long-Term Care Focus website. Rural location was measured by census report of the percentage of the rural population in the county in which the nursing home was located.
Analyses
We first examined the distribution of nursing homes based on the percentage of residents with ADRD only and those with ADRD and cognitive impairment. The two distributions were similar. Because it is unclear how best to identify nursing home residents with ADRD and it is likely that residents with severe cognitive impairment have many of the same care requirements as residents with ADRD diagnoses, we chose an expansive definition and defined the dementia cohort for this study as those with ADRD or cognitive impairment.
We divided the distribution into deciles—for example, the first decile includes all nursing homes having 0–10 percent residents with ADRD or cognitive impairment diagnoses, the second includes those with 11–20 percent residents with ADRD or cognitive impairment diagnoses, and so on. Then, we calculated the averages for all variables described above, across all nursing homes within the same decile.
Limitations
We note several limitations. The most important is the lower sensitivity of diagnosis data to accurately identify residents with ADRD. We addressed this by including residents whose direct Minimum Data Set assessment revealed a likelihood of severe cognitive impairment,16 which may have overestimated the population with dementia.
Second, these cross-sectional descriptive data cannot be interpreted as causal. We offer a first look at the nursing home industry with respect to where patients with ADRD or cognitive impairment receive care and raise questions and directions for future policy and research directions.
Third, the hospitalization and ED admission outcomes we present have not been risk adjusted. Hence, our suggestion that these measures might indicate better outcomes for nursing homes with ADRD or cognitive impairment census in excess of 90 percent, based on comparison to nursing homes at the 41–90 percent deciles, should be further examined in future studies. However, we note that other indicators, and in particular the CMS overall five-star quality measure that is risk adjusted, do suggest better care in this decile.
Finally, our data end in 2019, the last pre-COVID-19 year, and hence we cannot directly assess the impact of the pandemic.
Study Results
Distribution Of Nursing Homes By Their ADRD Census
Exhibit 1 presents the distribution of nursing homes by their ADRD or cognitive impairment census deciles. Few facilities (332, 2.4 percent) cared for a low census (0–30 percent) of residents with ADRD or cognitive impairment; these facilities probably specialized in postacute care, as most of the postacute patients are not likely to have ADRD or cognitive impairment. This assumption is further borne out by the high percentage of short-stay rather than long-stay patients in these deciles, as discussed further below. The majority of nursing homes (12,999, 93.5 percent) had a census ranging from 31percent to 80 percent of residents with ADRD or cognitive impairment. Only 578 (4.1 percent) nursing homes cared almost exclusively for residents with ADRD or cognitive impairment above 80 percent of census. These data suggest that with the exception of those at the top of the distribution, most nursing homes might not be highly specialized in dementia care. Online appendix exhibit A1 presents the distribution of nursing homes based on the ADRD-only definition.17 This distribution is similar to the distribution of nursing homes based on ADRD or cognitive impairment presented in Exhibit 1.
Exhibit 1.
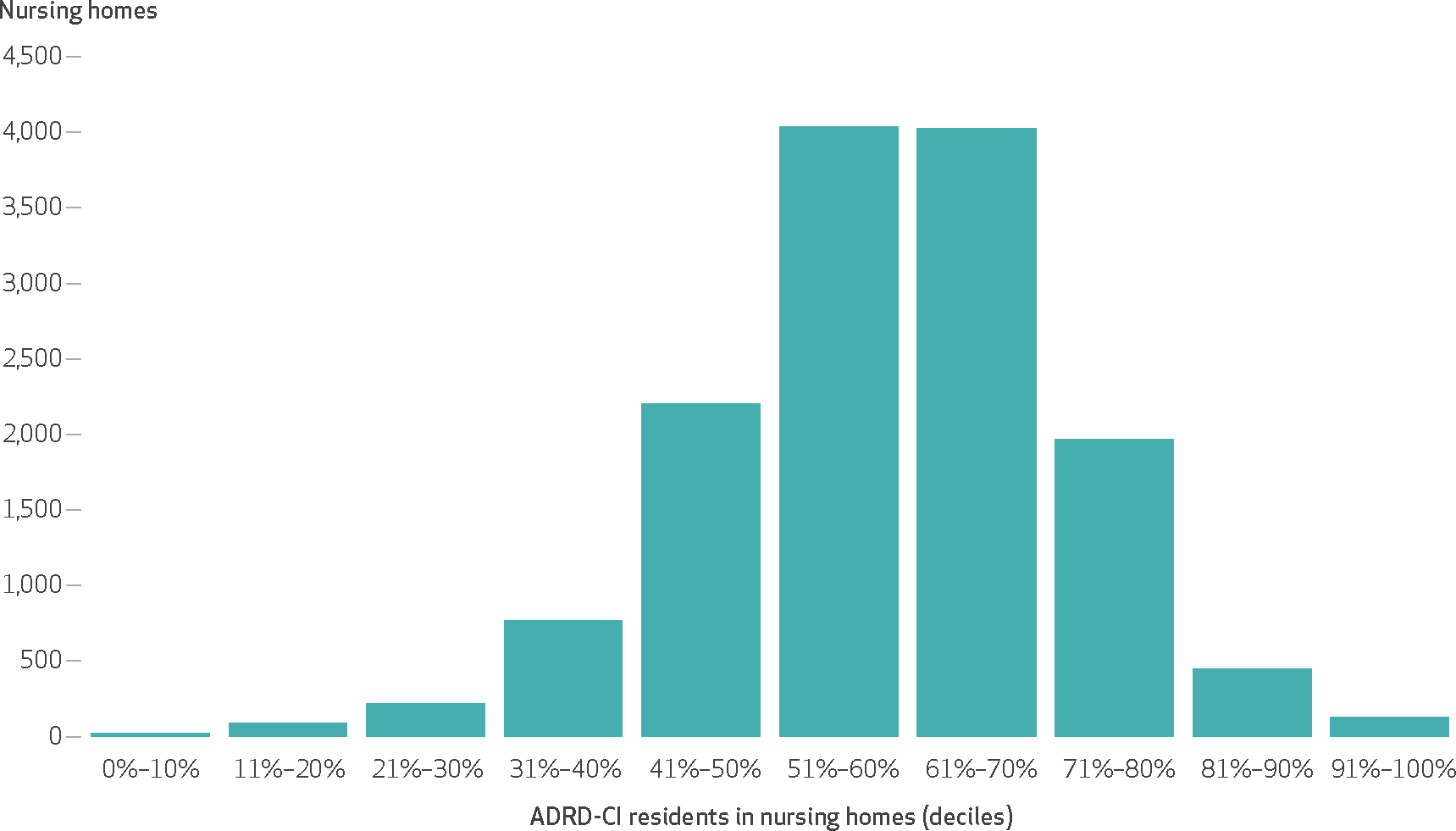
Distribution of US nursing homes by Alzheimer’s disease and related dementias (ADRD) or cognitive impairment (CI) deciles, 2017–19
SOURCE Authors’ analysis of national Minimum Data Set 2017–19 data.
Resident Outcomes By Nursing Home Deciles
Exhibit 2 presents three important resident outcomes—mortality, hospital admissions, and ED admissions—all per 1,000 resident-days. All three outcomes tended to increase initially, when ADRD or cognitive impairment percentages in the nursing home are low (around 20–30 percent), but as ADRD or cognitive impairment percentages increased, hospitalizations declined rapidly, ED visits declined less, and death rates remained stable. For the very two top ADRD or cognitive impairment deciles (above 80 percent), we observed an even greater deceleration, which is particularly pronounced for hospitalization rates.
Exhibit 2.
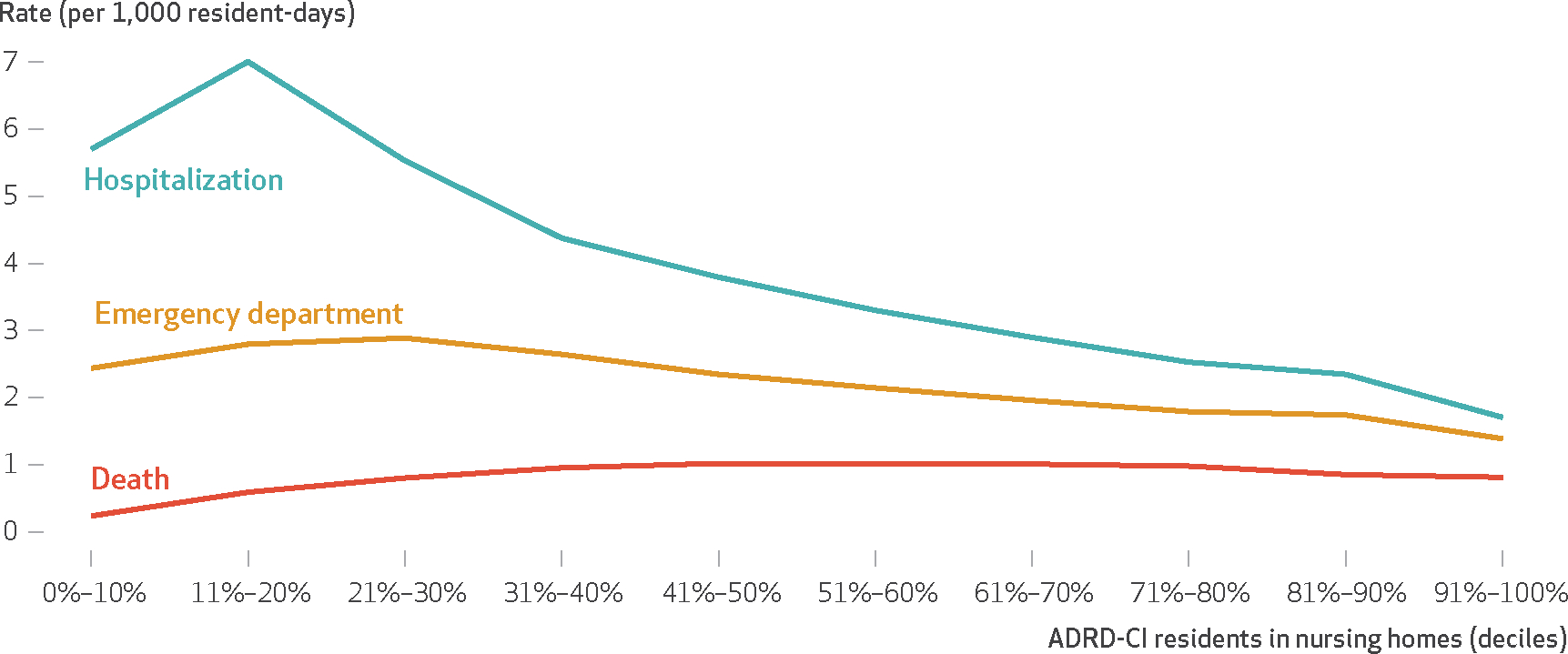
Daily hospitalization, emergency department, and death rates per 1,000 resident-days, US national nursing home residents, 2017–19
SOURCE Authors’ analysis of National Minimum Data Set and Medicare claims 2017–19 data. NOTE Values shown are averages calculated over all nursing homes in each Alzheimer’s disease and related dementias (ADRD) or cognitive impairment (CI) decile.
These outcome trends are parallel to those we observe with the case-mix index and the mix of short-stay and long-stay residents, presented at the top of exhibit 3. The case-mix index increased sharply and was high for the first two deciles of facilities, which also had the highest percentage of short-stay, postacute residents, many of whom were likely to be younger and unlikely to be diagnosed with dementia. Then, as the percentage of ADRD or cognitive impairment increases, case-mix index declined and the number of long-stay residents increased. At around the 51–60 percent ADRD or cognitive impairment decile the rate of decline of the case-mix index decreased as the percentage of residents with ADRD or cognitive impairment continued to increase and the percentage of long-stayers continued to grow, but at a decreasing rate.
Exhibit 3:
Nursing home residents’ characteristics by nursing homes deciles based on Alzheimer’s disease and related dementias (ADRD) or cognitive impairment (CI) distribution, US national nursing home residents, 2017–19
| Characteristics | ADRD-CI residents as percentage of total nursing home census (deciles) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0%–10% (mean) | 11%–20% (mean) | 21%–30% (mean) | 31%–40% (mean) | 41%–50% (mean) | 51%–60% (mean) | 61%–70% (mean) | 71%–80% (mean) | 81%–90% (mean) | 91%–100% (mean) | |
| Number of unique residents with ADRD-CI during the study period | 1,429 | 20,017 | 47,680 | 162,403 | 484,938 | 920,425 | 967,281 | 466,614 | 91,361 | 24,725 |
| Unique ADRD-CI residents out of total ADRD-CI during the study period (%) | 0.0 | 0.6 | 1.5 | 5.1 | 15.2 | 28.9 | 30.4 | 14.6 | 2.9 | 0.8 |
| Average case mix index (resource utilization groups IV) | 2.43 | 2.56 | 2.09 | 1.77 | 1.64 | 1.58 | 1.53 | 1.49 | 1.44 | 1.37 |
| Care type (%) | ||||||||||
| Long stay | 26.3 | 22.2 | 54.6 | 76.0 | 83.8 | 87.7 | 90.3 | 92.4 | 94.8 | 96 |
| Short stay | 73.7 | 77.8 | 45.4 | 24.0 | 16.2 | 12.3 | 9.7 | 7.6 | 5.2 | 4.0 |
| Hospice care | 0.6 | 0.9 | 3.2 | 5.8 | 7.2 | 7.4 | 7.7 | 8.1 | 8.7 | 9.2 |
| Race (%) | ||||||||||
| White | 89.0 | 79.7 | 77.7 | 77.3 | 78.4 | 79.2 | 79.7 | 77.4 | 69 | 72.2 |
| Black | 6.5 | 9.1 | 10.9 | 12.4 | 12.6 | 13.0 | 12.3 | 11.4 | 11.5 | 8.7 |
| Hispanic | 1.2 | 5.2 | 4.3 | 3.9 | 3.9 | 3.4 | 3.9 | 6.5 | 12.2 | 11.2 |
| Other | 3.4 | 6.1 | 7.1 | 6.4 | 5.1 | 4.4 | 4.1 | 4.8 | 7.3 | 7.9 |
| Resident by payer (%) | ||||||||||
| Medicaid | 15.2 | 12.0 | 38.9 | 53.7 | 58.0 | 60.6 | 62.3 | 63.5 | 69.2 | 70.8 |
| Medicare | 59.6 | 55.5 | 34.2 | 19.8 | 15.6 | 13.0 | 10.9 | 9.1 | 7.7 | 4.9 |
| County population (%) | ||||||||||
| Rural | 13.2 | 11.3 | 15.8 | 21.2 | 28.4 | 32.4 | 34.8 | 33.5 | 31.2 | 22.1 |
SOURCE Authors’ analysis of 2017–19 national Minimum Data Set and Long-Term Care Focus data. NOTES All numbers are means by decile except in the rows indicated as “number.” Case-mix index reflects the average acuity and physical and mental impairment levels of the residents in the nursing home. The case-mix index determines the resources required for residents’ care and payment.
Resident Characteristics By Nursing Home Deciles
Exhibit 3 presents additional resident characteristics for all residents in the nursing home by their deciles. The total number of unique residents with ADRD or cognitive impairment during the study period was close to 3.2 million. The majority were found in the middle deciles, with about 30 percent of the ADRD or cognitive impairment total population each in the deciles between 51 percent and 70 percent of the ADRD or cognitive impairment census, and around 15 percent of the total population in each of the deciles flanking them, the 41–50 percent and the 71–80 percent. These are also the deciles with the largest number of beds, accounting for 12,234 out of the total of 13,909, or 88 percent. The percentages of residents with ADRD or cognitive impairment in all other deciles were mostly below 5 percent in each decile.
The payer distribution, as expected, mimicked to a large degree the pattern exhibited by the short-stay and long-stay resident distributions. Medicare pays only for postacute, short-stay patients, which follows a hospital stay and its payment ends on day 100. Medicaid pays for those of low income and assets, with no time limits on their stay. Thus, Medicaid is typically the payor for long-stay, custodial residents. Residents with ADRD would qualify for Medicare payment only if they qualify for postacute care, and even then only for the first 100 days of their stay. Medicare was the dominant payer, with more than 50 percent of residents, for the first two deciles, for which both the case-mix index and short-stay percentages were the highest and declined to their lowest levels at the last decile, with short stay at 4.0 percent. Conversely, Medicaid was the lowest in the first two deciles and the highest in the last decile.
Although very few residents were enrolled in hospice, the percentage increased as the percentage of residents with ADRD or cognitive impairment increased, ranging from 0.6 percent in the first decile to 9.2 percent for the last decile. The racial distribution did not reveal much of a trend. The percentage of the county’s rural population generally increased with the ADRD or cognitive impairment decile, except for the last two deciles, which showed a decline, particularly at the last decile, going from more than 30 percent to 22.1 percent.
Nursing Home Characteristics By Nursing Home Deciles
Exhibit 4 presents facility characteristics. The percentage of nursing homes with dementia special care units increased with the percentage of residents with ADRD or cognitive impairment. Of those with 61–90 percent residents with ADRD or cognitive impairment, about 20 percent had special care units. This percentage increased to 35 percent for the top decile.
Exhibit 4:
Nursing home characteristics by nursing homes deciles based on Alzheimer’s disease and related dementias (ADRD) or cognitive impairment (CI) distribution, US national nursing home residents, 2017–19
| Characteristics | ADRD-CI residents as percentage of total nursing home census (deciles) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0%–10% (mean) | 11%–20% (mean) | 21%–30% (mean) | 31%–40% (mean) | 41%–50% (mean) | 51%–60% (mean) | 61%–70% (mean) | 71%–80% (mean) | 81%–90% (mean) | 91%–100% (mean) | |
| Number of nursing homes in the decile | 22 | 89 | 221 | 765 | 2,203 | 4,035 | 4,029 | 1,967 | 448 | 130 |
| Ownership (%) | ||||||||||
| For profit | 63.6 | 66.3 | 79.2 | 82.4 | 78.8 | 75.2 | 68.3 | 64.5 | 74.1 | 78.5 |
| Part of a chain | 59.1 | 58.4 | 60.2 | 68.5 | 68.0 | 60.9 | 56.7 | 52.4 | 51.8 | 65.4 |
| Nursing homes with dementia special care units | 0.00 | 0.00 | 0.45 | 1.44 | 6.04 | 11.6 | 20.7 | 24.1 | 20.5 | 34.6 |
| Staffing hours per resident-day | ||||||||||
| RNs | 1.43 | 1.23 | 0.80 | 0.53 | 0.45 | 0.40 | 0.38 | 0.35 | 0.31 | 0.35 |
| LPNs | 0.91 | 0.90 | 0.87 | 0.82 | 0.80 | 0.79 | 0.78 | 0.78 | 0.77 | 0.71 |
| CNAs | 2.44 | 2.49 | 2.26 | 2.13 | 2.12 | 2.14 | 2.18 | 2.18 | 2.19 | 2.37 |
| Staffing instability a | ||||||||||
| RNs | 28.8 | 25.4 | 30.2 | 30.2 | 30.5 | 31.6 | 31.8 | 33.1 | 35.8 | 35.5 |
| LPNs | 31.7 | 26.8 | 24.8 | 20.3 | 18.4 | 17.2 | 16.4 | 16.2 | 15.9 | 17.8 |
| CNAs | 13.7 | 10.3 | 9.2 | 7.2 | 6.2 | 6.0 | 5.6 | 5.9 | 6.1 | 5.9 |
| Beds and occupancy | ||||||||||
| Average number of beds | 37.4 | 64.4 | 84.3 | 98.1 | 104.7 | 109.7 | 116.5 | 115.3 | 103.6 | 81.8 |
| Occupancy (%) | 74.2 | 76.6 | 72.3 | 76.3 | 78.5 | 80.3 | 81.2 | 81.5 | 81.8 | 86.6 |
| Quality a | ||||||||||
| Average 5-star overall | 4.28 | 4.29 | 3.63 | 3.30 | 3.24 | 3.19 | 3.29 | 3.33 | 3.23 | 3.57 |
| Average 5-star quality measures | 3.95 | 3.94 | 4.01 | 3.99 | 3.89 | 3.78 | 3.77 | 3.80 | 3.71 | 3.96 |
| Average 5-star survey | 3.96 | 3.70 | 3.05 | 2.67 | 2.68 | 2.72 | 2.87 | 2.93 | 2.93 | 3.10 |
| Average 5-star staffing | 4.21 | 4.06 | 3.48 | 3.24 | 3.17 | 3.06 | 3.03 | 2.98 | 2.81 | 3.03 |
SOURCE Authors’ analysis of 2017–19 National Nursing Homes Payroll Based Journal Data, Long-Term Care Focus data, and the Centers for Medicare and Medicaid Services data catalog. NOTES All numbers are means by decile except in the rows indicated as “number.” RN is registered nurse. LPN is licensed practical or vocational nurse. CNA is certified nurse aide.
Number of nursing homes with data for these categories were somewhat smaller from the other categories and are available from the lead author on request.
The nursing homes at the extremes tended to be small. Those with more than 91 percent residents with ADRD or cognitive impairment averaged 82 beds, those with between 11 and 30percent residents with ADRD or cognitive impairment averaged 64–84 beds, and those with less than 10 percent averaged thirty-seven beds. The nursing homes with 31–90 percent residents with ADRD or cognitive impairment had around 100–115 beds, with size increasing with ADRD or cognitive impairment percentage. Occupancies ranged from a low of 74.2 percent to a high of 86.6 percent and tended to increase as the percentage of residents with ADRD or cognitive impairment increased.
For-profit ownership ranged from a low of 63.6 percent for the first decile to a high of 82.4 percent for the 31–40 percent decile, but there was no particular trend between for-profit ownership and percentage of residents with ADRD or cognitive impairment. Similarly, chain affiliation, which ranged from 51.8 percent in the ninth decile to 68.0 percent in the fifth decile was not associated with ADRD or cognitive impairment census.
All staffing hours per resident-day started at high levels at low ADRD or cognitive impairment deciles and declined, particularly among RNs, as percentage ADRD or cognitive impairment increased. RN staffing hours per resident-day continued to decline while LPNs and CNAs levels stabilized at the 40 percent decile and above. The only exception is the very last decile, in which both RN and CNA staffing increased by 13 percent and 8 percent, respectively, relative to the prior decile.
Staffing instability, which is inversely associated with quality,14,15 increased for RNs as ADRD or cognitive impairment percentages increased, but decreased for LPNs and CNAs, with CNA instability being the lowest throughout.
Quality, as measured by the risk-adjusted overall five-star ratings published by CMS in Nursing Home Care Compare18 and ranging from 1 (worst) to 5 (best), averaged 4.28 for nursing homes in the first decile. Ratings declined as the percentage of residents with ADRD or cognitive impairment increased, suggesting that overall quality, as measured by these rankings, drops as the percentage of residents with ADRD or cognitive impairment increases. The only exception is the highest decile, in which quality ranking increased to 3.57 from 3.23 in the prior decile and was the highest by far compared with all deciles except the first three (0–30 percent), which likely represent the short-stay, postacute nursing homes.
Discussion
This study provides a snapshot of the nursing home sector, focusing on residents with ADRD or cognitive impairment during the pre-COVID-19 era, 2017–19. For nursing homes in which residents with ADRD or cognitive impairment accounted for more than 90 percent of the census, several indicators of quality seemed to suggest better care for residents with ADRD or cognitive impairment when compared with deciles with the 41–90 percent ADRD or cognitive impairment census (that is, the deciles that are not likely to be dominated by postacute patients): better outcomes, particularly lower hospitalization and ED rates (although they are not risk adjusted) and a higher overall five-star ranking, which is based on risk-adjusted quality indicators; higher RN and CNA hours per resident-day; and less CNA staffing instability. This decile also has the largest percentage of facilities with dementia special care units, at 34.6 percent, compared with the next highest, at 24.1 percent, in the 71–80 percent decile. Notably, there are only 130 facilities in this decile caring for only 0.8 percent of the total ADRD or cognitive impairment population.
The vast majority of people with ADRD or cognitive impairment are in nursing homes that also care for many residents without ADRD or cognitive impairment diagnoses. Although the evidence shows that residents with ADRD or cognitive impairment require specialized care from staff with specialized training,4,9,10 they may be less likely to receive this care in facilities with heterogeneous populations. Some of these facilities have dementia special care units, but their percentages are low, and they are not likely to be available to most residents who may benefit from them.
These statistics and the literature suggesting that residents with ADRD or cognitive impairment require more staff with specialized training raise concerns about whether the majority of the residents with ADRD or cognitive impairment in nursing homes receive the care they need.4,8,9 They raise policy questions on two levels: on the research level and on the care delivery level.
On the research level, many of the studies about care for residents with ADRD or cognitive impairment are dated,19 although this might be changing. After the enactment of the 2011 National Alzheimer’s Project Act, the National Institute on Aging has been investing heavily in Alzheimer’s research. The fruits of these efforts should inform questions related to the optimal care of residents with ADRD or cognitive impairment in nursing homes, what staffing complement is required, and the training that such staff needs. Some of the research should also address health outcomes specific to residents with ADRD or cognitive impairment. New statistical methods, taking advantage of large data and clinical insights, should be explored to inform the field.
On the care delivery front, the Biden administration launched a new policy in early 2022 aimed at improving nursing home care through staffing standards.20 Although these efforts are not focused on residents with ADRD or cognitive impairment specifically (except for mentioning continued efforts to reduce use of antipsychotic drugs), the targeted enhancements to staffing levels, staff training, and improvement to Nursing Home Care Compare will benefit residents with ADRD or cognitive impairment who reside in all nursing homes. Note, however, that fewer than 20 percent of patients with ADRD or cognitive impairment are in nursing homes in which they account for more than 70 percent of the census, and fewer than 50 percent are in nursing homes in which their census exceeds 60 percent, yet the staffing standards to be established by the new policy do not mention anything about adjusting these standards to the resident mix in the facility. This raises the question of whether one minimum standard suffices, and particularly whether the envisioned staffing minimums will ensure quality and safety in nursing homes serving residents with ADRD or cognitive impairment for these residents as well.
Finally, how might COVID-19 have affected our findings? Our data did not cover the COVID-19 period. It is documented that persons with ADRD were at high risk for COVID-19 and mortality from COVID-19, particularly before vaccine availability. 21 Comparing persons with dementia who are enrolled in Medicare Parts A and B and living in the community with those living in nursing homes, one study found that people with ADRD in nursing homes were at higher risk for death from COVID-19 than their counterparts living in the community. 22 Although prior research suggests that nursing home size and community prevalence of COVID-19 were key factors driving COVID-19 outbreaks and deaths, 23 it is unclear what role the concentration of residents with ADRD or cognitive impairment in the facility played in the spread of COVID-19. It also remains to be seen if and how the overwhelming experience of nursing homes with COVID-19 will change admission patterns or the organization of nursing home care, training, and staffing as we emerge from this public health emergency.
Conclusion
The most important finding from this snapshot is that residents with ADRD or cognitive impairment receive care across most nursing homes but are the majority in only a handful. This raises two questions for further study: “What are the implications for quality of care, quality of life, and health outcomes of having the majority of nursing home residents with ADRD or cognitive impairment in nursing homes where they are not the dominant resident population?” And “What, if any, changes in staff training, facility environment, and policies are needed to improve the care of this population?” Addressing these questions will require investments and advancements in research approaches, as well as ongoing policy enhancements and innovations. The current focused investments in ADRD research by the National Institute on Aging and the new policy initiated by the Biden administration are an excellent beginning. They need to continue in a coordinated fashion to move the agenda forward.
Supplementary Material
Acknowledgment
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health (Award No. R01AG066742). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Debra Saliba is an employee of the Department of Veterans Affairs. The views presented here do not represent those of the Department of Veterans Affairs. The authors thank Jonathan Bor for his excellent editorial contributions that have improved the manuscript.
Contributor Information
Dana B. Mukamel, Department of Medicine, Division of General Internal Medicine; University of California, Irvine; 100 Theory, Suite 120, Irvine, CA 92617-3056.
Debra Saliba, University of California, Los Angeles Borun Center at David Geffen School of Medicine, 10945 Le Conte Ave., Suite 2339, Los Angeles, CA 90095-1687; Veterans Administration GRECC, Los Angeles, CA; RAND Health, Santa Monica, CA.
Heather Ladd, Department of Medicine, Division of General Internal Medicine; iTEQC Research Program; University of California, Irvine; 100 Theory, Suite 120, Irvine, CA 92617-3056.
R. Tamara Konetzka, Department of Medicine, Section of Geriatrics and Palliative Medicine; The University of Chicago, 5841 South Maryland Ave MC2000, Chicago, IL 60637–1447.
Notes
- 1.2022 Alzheimer’s disease facts and figures. Alzheimers Dement. 2022;18(4):700–89. [DOI] [PubMed] [Google Scholar]
- 2.Bunn F, Burn AM, Goodman C, Rait G, Norton S, Robinson L, et al. Comorbidity and dementia: a scoping review of the literature. BMC Med. 2014;12:192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ishii S, Streim JE, Saliba D. A conceptual framework for rejection of care behaviors: review of literature and analysis of role of dementia severity. J Am Med Dir Assoc. 2012;13(1):11–23.e1–2. [DOI] [PubMed] [Google Scholar]
- 4.Ballard C, Corbett A, Orrell M, Williams G, Moniz-Cook E, Romeo R, et al. Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: a cluster-randomised controlled trial. PLoS Med. 2018;15(2):e1002500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Castle NG, Engberg J. Staff turnover and quality of care in nursing homes. Med Care. 2005;43(6):616–26. [DOI] [PubMed] [Google Scholar]
- 6.Bishop CE, Weinberg DB, Leutz W, Dossa A, Pfefferle SG, Zincavage RM. Nursing assistants’ job commitment: effect of nursing home organizational factors and impact on resident well-being. Gerontologist. 2008;48(Spec No 1):36–45. [DOI] [PubMed] [Google Scholar]
- 7.Lai CK, Yeung JH, Mok V, Chi I. Special care units for dementia individuals with behavioural problems. Cochrane Database Syst Rev. 2009;(4):CD006470. [DOI] [PubMed] [Google Scholar]
- 8.Joyce NR, McGuire TG, Bartels SJ, Mitchell SL, Grabowski DC. The impact of dementia special care units on quality of care: an instrumental variables analysis. Health Serv Res. 2018;53(5):3657–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cadigan RO, Grabowski DC, Givens JL, Mitchell SL. The quality of advanced dementia care in the nursing home: the role of special care units. Med Care. 2012;50(10):856–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gruneir A, Lapane KL, Miller SC, Mor V. Is dementia special care really special? A new look at an old question. J Am Geriatr Soc. 2008;56(2):199–205. [DOI] [PubMed] [Google Scholar]
- 11.Nursing Home Help. RUG-IV Classification System (66 group) with Medicare case mix indices for 10/1/ 2011 [Internet]. Columbia (MO): University of Missouri, Sinclair School of Nursing; [cited 2023 May 15]. Available from: https://nursinghomehelp.org/wp-content/uploads/2017/11/RUG-IVMedicareSNFPPSCMIs100111.pdf [Google Scholar]
- 12.Heerema E BIMS score role in identifying dementia. Verywell Health [serial on the Internet]. [last updated 2020 Feb 2; cited 2023 Mar 27]. Available from: https://www.verywellhealth.com/bims-identifying-dementia-98637
- 13.Centers for Medicare and Medicaid Services. MDS 3.0 quality measures user’s manual (v12.1) [Internet]. Baltimore (MD): CMS; 2019. Oct 1 [cited 2023 Mar 27]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/MDS-30-QM-USERS-MANUAL-v121.pdf [Google Scholar]
- 14.Mukamel DB, Saliba D, Ladd H, Konetzka RT. Association of staffing instability with quality of nursing home care. JAMA Netw Open. 2023;6(1):e2250389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mukamel DB, Saliba D, Ladd H, Konetzka RT. Daily variation in nursing home staffing and its association with quality measures. JAMA Netw Open. 2022;5(3):e222051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bynum JPW, Dorr DA, Lima J, McCarthy EP, McCreedy E, Platt R, et al. Using healthcare data in embedded pragmatic clinical trials among people living with dementia and their caregivers: state of the art. J Am Geriat Soc. 2020;68 Suppl 2(Suppl 2):S49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.To access the appendix, click on the Details tab of the article online. [Google Scholar]
- 18.Medicare.gov. Find & compare providers near you: find nursing homes including rehab services near me [Internet]. Baltimore (MD): Centers for Medicare and Medicaid Services; [cited 2023 Mar 27]. Available from: https://www.medicare.gov/care-compare/?providerType=NursingHome&redirect=true#search [Google Scholar]
- 19.Watt JA, Goodarzi Z, Veroniki AA, Nincic V, Khan PA, Ghassemi M, et al. Comparative efficacy of interventions for aggressive and agitated behaviors in dementia: a systematic review and network meta-analysis. Ann Intern Med. 2019;171(9):633–42. [DOI] [PubMed] [Google Scholar]
- 20.The White House. Fact sheet: protecting seniors by improving safety and quality of care in the nation’s nursing homes [Internet]. Washington (DC): White House; 2022. Feb 28 [cited 2023 Mar 27]. Available from: https://www.whitehouse.gov/briefing-room/statements-releases/2022/02/28/fact-sheet-protecting-seniors-and-people-with-disabilities-by-improving-safety-and-quality-of-care-in-the-nations-nursing-homes/ [Google Scholar]
- 21.Liu N, Sun J, Wang X, Zhao M, Huang Q, Li H. The impact of dementia on the clinical outcome of COVID-19: a systematic review and meta-analysis. J Alzheimers Dis. 2020;78(4):1775–82. [DOI] [PubMed] [Google Scholar]
- 22.Gilstrap L, Zhou W, Alsan M, Nanda A, Skinner JS. Trends in mortality rates among Medicare enrollees with Alzheimer disease and related dementias before and during the early phase of the COVID-19 pandemic. JAMA Neurol. 2022;79(4):342–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Konetzka RT, White EM, Pralea A, Grabowski DC, Mor V. A systematic review of long-term care facility characteristics associated with COVID-19 outcomes. J Am Geriatr Soc. 2021;69(10):2766–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


